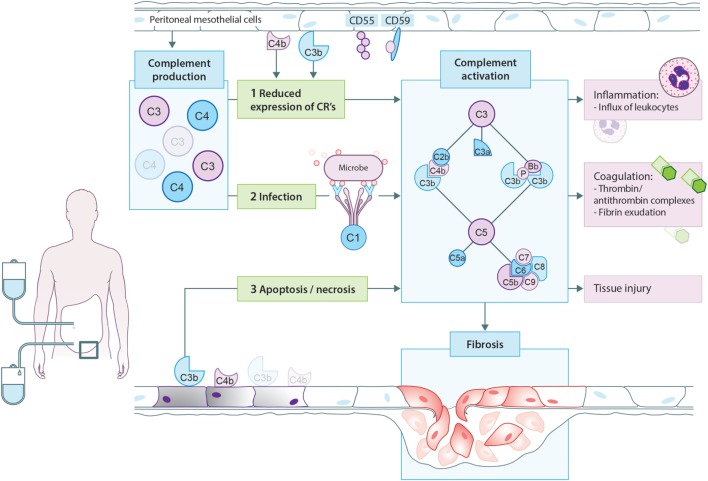
Figure 3.
Proposed model for complement activation in peritoneal dialysis (PD). In PD patients, mesothelial cells produce and secrete different complement factors. One of the proposed mechanisms of complement activation in PD patients is that PD therapy decreases the expression of complement regulators such as CD55 and CD59 on the peritoneal mesothelium, leading to local complement activation. In addition, cellular debris as a result of direct peritoneal damage by bioincompatible PD fluids as well as antibodies against microorganisms could contribute to local complement activation during PD. Complement activation will result in the formation of anaphylatoxins (C3a, C5a), opsonins (C3b, iC3b), and the membrane attack complex (C5b-9). First, complement activation leads to the influx of leukocytes, predominantly neutrophils. Second, complement activation increased the production of thrombin anti-thrombin complexes and fibrin exudation on the surface of the injured peritoneum. Altogether, these events indicate the activation of the coagulation system. Third, complement activation during PD leads to direct damage of the peritoneum. Moreover, recent evidence suggests that complement activation promotes the progression to fibrosis after tissue injury. In PD, complement activation could stimulate mesothelial cells to undergo epithelial-to-mesenchymal transition, resulting in the accumulation of myofibroblasts and consequently peritoneal fibrosis.