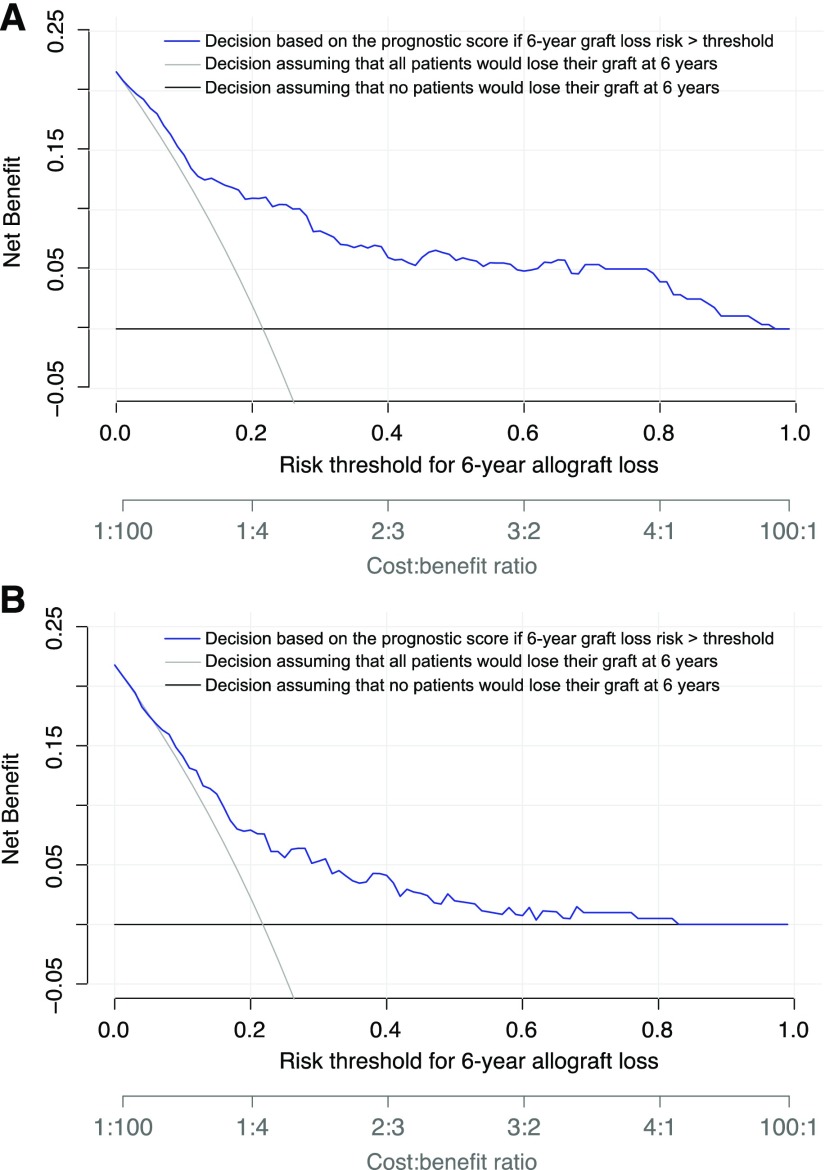
Figure 5.
Decision making after standard management of ABMR on the basis of the ABMR prognostic score provided greater net clinical benefit to patients than considering all patients to have the same level of risk of allograft loss at 6 years after the diagnosis of ABMR. Decision curve analysis shows the net benefit achieved by making clinical decisions on the basis of the predictions at 6 years after ABMR diagnosis computed by the prognostic score (A) in the development cohort and (B) in the external validation cohort. The decision curve analysis shows the net benefit of the prognostic score in regard to decision making for potential intervention across all of the thresholds of risk of allograft loss at 6 years as defined by clinician judgement and patient preference (blue), compared with considering patients with ABMR at the same level of risk of allograft loss: all patients at risk (gray) or no patients at risk (black). If the decision is defined by the performance of additional therapy to standard treatment, the expected benefit is represented by the number of patients who would lose their allograft and who would undergo clinical intervention (true positives) using the proposed decision rule. The expected harm is represented by the number of patients without allograft loss who would undergo clinical intervention in error (false positives) multiplied by a weighting factor on the basis of the risk threshold. The highest curve at any given risk threshold is the optimal strategy for decision-making in order to maximize net benefit. Overall, the net benefit for decisions on the basis of the prognostic score is higher than that for decisions on the basis of the same level of risk for thresholds from 1% to 96%.