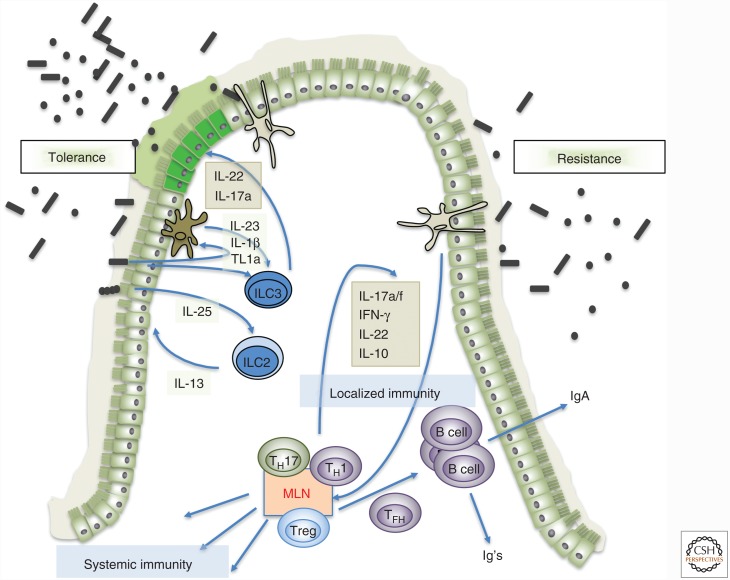
Figure 1.
Microbiota-mediated strategies for host-mediated protection from pathogens. (Left) Tolerance induced by microbiota by way of innate signals mediated by epithelial cells, myeloid cells, and innate lymphoid cells. Cytokines and growth factors produced by cells such as ILC3 result in more robust epithelial barrier function and modifications in the mucin layer (e.g., allowing pathogenic bacteria to forage fucose, precluding invasion of host tissues despite high bacterial load). ILC2 may also participate in promoting tolerance, by responding to microbe-induced epithelial tuft cell–produced interleukin (IL)-25 with secretion of IL-13, which promotes epithelial robustness. (Right) Resistance to pathogenic bacteria through induction of microbiota-specific T- and B-cell responses. Myeloid cells (macrophages/dendritic cells) take up microbial products, transport them to draining lymph nodes (mesenteric lymph node [MLN]), and present microbiota antigen to naïve T cells, activating them and polarizing them (CD8 T cells are not depicted, but are likely also primed). The T cells then distribute throughout the body, including the intestinal lamina propria, and limit microbial growth through production of cytokines and recruitment of neutrophils and other phagocytic cells. The T cells also differentiate into follicular helper T cells (TFH), which promote B-cell affinity maturation and isotype class switching, with production of secreted IgA and other classes of antibody (Ig) that can function systemically. IFN, Interferon.