Abstract
Basal cell adenoma is a rare type of monomorphic salivary adenoma most commonly involving the parotid gland. Cytology of basal cell adenoma closely mimics many other benign and malignant basaloid neoplasms. Cytological features of membranous basal cell adenoma simulate adenoid cystic carcinoma in fine needle aspiration cytology (FNAC) smears. Here, we are presenting a rare case of cytodiagnosis of membranous basal cell adenoma of parotid gland in an elderly lady, which mimicked adenoid cystic carcinoma on FNAC. We discuss the cytomorphology of this rare case with an emphasis on cytological difference between membranous basal cell carcinoma and adenoid cystic carcinoma as well as other basaloid neoplasms.
Keywords: Adenoid cystic carcinoma, basal cell adenoma, cytology, parotid gland
INTRODUCTION
Basal cell adenoma is a rare benign salivary gland tumor accounting for only 1–3% of salivary gland tumors.[1,2,3,4] Although it is most common in the parotid gland (75%), it also occurs in other major and minor salivary glands.[1,2,3] Most cases are found in elderly females clinically presenting as painless mobile swelling.[2,5] Cytological diagnosis of basal cell adenoma is always challenging because it mimics many other basaloid tumors (e.g., cellular pleomorphic adenoma, adenoid cystic carcinoma, basal cell carcinoma and metastatic small cell carcinoma etc.).[2,3] Here, we are presenting the cytology of basal cell adenoma of parotid in an elderly female patient, which mimicked adenoid cystic carcinoma on cytological diagnosis.
CASE HISTORY
A 62-year-old lady presented with gradually increasing painless mass in the left parotid region of 6 months duration. On examination, the swelling was firm and mobile measuring 4 × 3 cm in diameter. She was approached with fine needle aspiration cytology (FNAC) by a 23-gauge needle attached with a 10-ml syringe. The smears were fixed in alcohol and stained by Leishman–Giemsa and hematoxylin and eosin (H and E) stains. The smears were cellular and comprised clusters and sheets of basaloid cells around hyaline globules and acellular dense hyaline material [Figure 1a and b]. The cells were small, monomorphic with scanty cytoplasm, round to oval bland nuclei, fine chromatin, and conspicuous nucleoli. Ribbon of basement membrane material and palisading of tumor cells at the periphery were present in some clusters [Figure 1a–c]. There was no necrosis and pleomorphism in tumor cells and mitosis was absent. We reported the cytology smears as suggestive of basal cell adenoma. However, we advised biopsy and histopathological study to exclude the possibility of adenoid cystic carcinoma.
Figure 1.
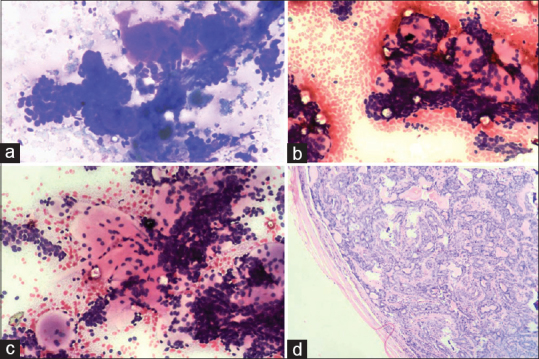
(a-c) Photomicrograph of cytology of basal cell adenoma exhibiting clusters and cords of basaloid cells with variable amount basement membrane like stromal material and palisading of tumor cells at periphery and also in the basement membrane material (a: Leishman and Giemsa stain, ×40 b-c: H and E stain, ×40). (d) Photomicrograph showing histology of basal cell adenoma, the tumor was composed of bland basaloid cells separated by many abundant amorphous hyaline membranous stroma (H and E stain, ×100)
The patient underwent left total parotidectomy and the specimen was sent to our histopathology laboratory. On gross examination, it was a 3.5 × 2× 2 cm solid lobulated mass with a tan cut surface. On histology, the tumor composed basaloid cells separated by amorphous hyaline membranous stroma [Figure 1d]. Tumor cells were arranged in tubulo-trabecular pattern, and peripheral palisading of tumor cells was seen. There was no cytological atypia, necrosis, and mitosis in the cells. Histopathology was diagnosed as basal cell adenoma in a predominantly membranous pattern [Figure 1d].
Her postoperative period was uneventful and no recurrence was noted during 2 years of follow-up.
DISCUSSION
Histologically, there are four types of basal cell adenomas – solid, trabecular, tubular, and membranous type.[1,2,6] FNAC is a common and very useful tool in the diagnosis of salivary gland lesions. Preoperative cytology not only helps in correct diagnosis but also avoids radical surgery in benign and non-neoplastic lesions.[6] However, diagnosis and typing of basaloid tumors are always difficult because differential diagnoses of basaloid tumors include several benign and malignant entities.[1,6] Differential diagnoses of basaloid tumors include cellular pleomorphic adenoma, basal cell adenoma, myoepithelioma, adenoid cystic carcinoma, basal cell adenocarcinoma, basaloid squamous cell carcinoma, and cutaneous cylindroma.[1,3]
Cytology of basal cell adenoma is cellular and comprises small uniform cells in clusters, cords, as well as singly around variable amount eosinophilic basement membrane-like stromal material and hyaline globules.[2,6] Often, there is presence of palisading and peripheral ribbons of acellular matrix surrounding cell clusters. The cells are small basaloid type with scanty pale cytoplasm, round-to-oval bland nuclei, fine chromatin, and indistinct nucleoli. Absence of chondromyxoid stromal matrix, cytological atypia, necrosis, and mitosis are the key features.[1,2,3,6,7] In our case, there was peripheral palisading of basaloid cells around the hyaline globules. Similar features are also found in adenoid cystic carcinoma. Singh et al. reported a similar case of basal cell adenoma misinterpreted as adenoid cystic carcinoma in cytology.[2] They concluded that cell-stromal interface is a very useful differentiating feature.[2] In basal cell adenoma, cells are intermingled [Figures 1a and 1b] with adjacent stroma, whereas in adenoid cystic carcinoma stroma is sharply demarcated.[2,8]
Cytology of membranous subtype closely mimics adenoid cystic carcinoma because in both the cases abundant hyaline membrane material (globule) surrounded by basaloid cells is seen.[1] In cytology of both the tumors, basaloid cells are arranged in sheets, three-dimensional cell clusters, and acinar pattern.[1] Our case was a membranous variant of basal cell adenoma where cytomorphology was closely similar to adenoid cystic carcinoma.
Other cytologic features that help to differentiate basal cell adenoma from adenoid cystic carcinoma are (1) acellular hyaline membrane material in membranous basal cell adenoma is denser than hyaline globules in adenoid cystic carcinoma; (2) fibrous lines and fragments can be seen in basal cell adenoma but not in adenoid cystic carcinoma, where it is mucoid and more homogeneous; (3) absence of mitosis in cytology of basal cell adenoma where as in adenoid cystic carcinoma frequent mitoses are found.[1]
Two close benign cytologic mimickers of basal cell adenoma are cellular pleomorphic salivary adenoma and myoepithelioma.[1,2,6] Absence of chondro-myxoid stroma and myoepithelial cells in cytology smears of basal cell adenoma differentiate basal cell adenoma from Pleomorphic salivary adenoma (PSA). Another two malignant entities which also simulate basal cell adenoma are basal cell adenocarcinoma and basaloid squamous cell carcinoma. Presence of significant cytological atypia, mitosis, and necrosis differentiates these two lesions from basal cell adenoma.[1,9,10] Other rare cytological and histological differential diagnoses of basal cell adenoma are dermal cylindroma, trichoepithelioma, and spiradenoma, where the location of the tumor is a very important distinguishing feature.[1]
In the diagnosis of basaloid neoplasm of salivary gland, cytologists should be careful in identifying basaloid cells, arrangement, presence of other cell and stromal components, cell-stroma interface, and mitosis to avoid cytological misinterpretation. Our case report of cytology of basal cell adenoma of membranous variant exposes close differential diagnoses and pitfalls of cytodiagnosis which may help cytologists in evaluation of basaloid neoplasm of salivary glands.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Jurczyk M, Peevey JF, Vande Haar MA, Lin X. Pitfalls of fine-needle aspiration cytology of parotid membranous basal cell adenoma - A review of pitfalls in FNA cytology of salivary gland neoplasms with basaloid cell features. Diagn Cytopathol. 2015;43:432–7. doi: 10.1002/dc.23234. [DOI] [PubMed] [Google Scholar]
- 2.Singh A, Sharma R, Nema SK. Basal cell adenoma mimicking adenoid cystic carcinoma on FNAC - A case report. Int J Med Rev. 2014;2:166–8. [Google Scholar]
- 3.Gupta N, Bal A, Gupta AK, Rajwanshi A. Basal cell adenoma: A diagnostic dilemma on fine needle aspiration cytology. Diagn Cytopathol. 2011;39:913–6. doi: 10.1002/dc.21576. [DOI] [PubMed] [Google Scholar]
- 4.de Araujo VC. Basal cell adenoma. In: Barnes L, Eveson JW, Reichart P, Sidransky D, editors. World Health Organization Classification of Tumours: Pathology & Genetics-Head and Neck Tumours. Lyon: IARC Press; 2005. pp. 261–2. [Google Scholar]
- 5.Margaritescu C, Mercut V, Mogoanta L, Florescu M, Simionescu C, Cionca L, et al. Salivary gland basal cell adenomas – Immunohistochemical evaluation of four cases and review of the literature. Rom J Morphol Embryol. 2005;46:29–40. [PubMed] [Google Scholar]
- 6.Bhat A, Rao M, Geethamani V, Shetty AC. Basal cell adenoma of the parotid gland: Cytological diagnosis of an uncommon tumor. J Oral Maxillofac Pathol. 2015;19:106. doi: 10.4103/0973-029X.157211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mukunyadzi P. Review of fine-needle aspiration cytology of salivary gland neoplasms, with emphasis on differential diagnosis. Am J Clin Pathol. 2002;118:S100–5. doi: 10.1309/WVVR-30E4-13TW-494D. [DOI] [PubMed] [Google Scholar]
- 8.Hara H, Oyama T, Saku T. Fine needle aspiration cytology of basal cell adenoma of the salivary gland. Acta Cytol. 2007;51:685–91. doi: 10.1159/000325830. [DOI] [PubMed] [Google Scholar]
- 9.Geisinger KR, Stanley MW, Raab SS, Silverman JF, Abati A. Salivary gland masses. In: Geisinger KR, Stanley MW, Raab SS, Silverman JF, Abati A, editors. Modern Cytopathology. Churchill Livingstone: Elsevier Science; 2003. pp. 781–811. [Google Scholar]
- 10.Maradi K, Kaushal V, Asotra S. Basal cell adenocarcinoma of submandibular salivary gland-problems in cytologic diagnosis. J Cytol. 2011;28:203–6. doi: 10.4103/0970-9371.86349. [DOI] [PMC free article] [PubMed] [Google Scholar]


