Fig. 1.
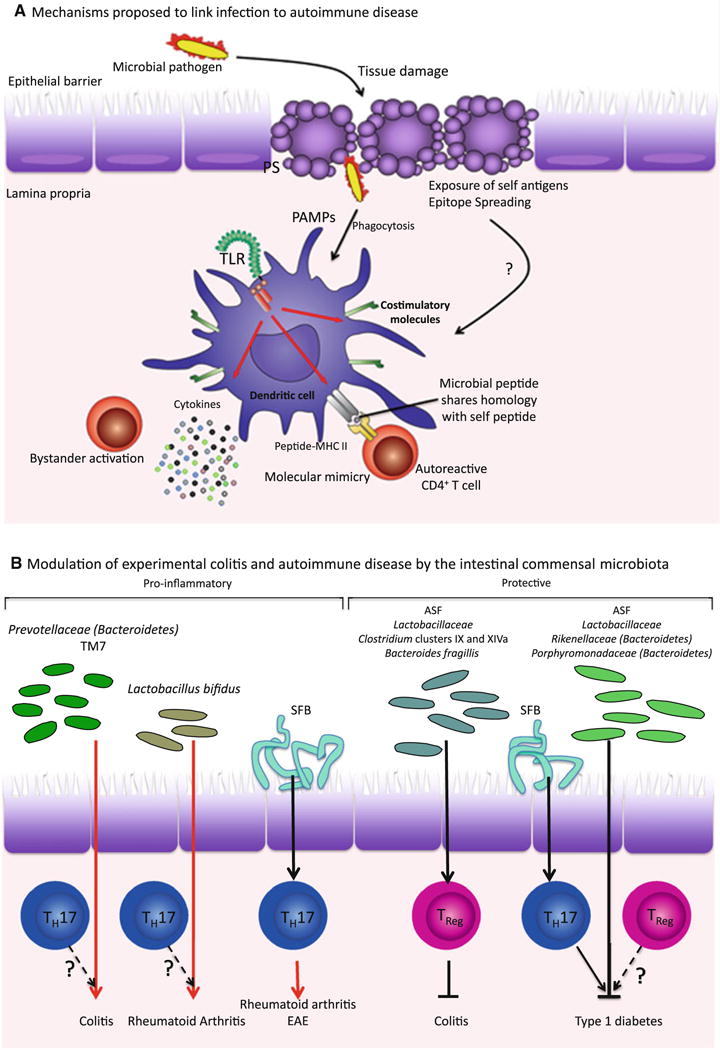
Both pathogenic and commensal microbes can influence development of autoimmunity. a In molecular mimicry, or T cell epitope mimicry, peptides derived from a pathogen share homology with some self-peptides. During infection, autoreactive T cells that have escaped clonal deletion in the thymus, can become activated by antigen-presenting cells (APC) presenting these “mimic” antigens. Pathogens may also contribute to autoimmunity by causing tissue damage and allowing abnormal exposure of self-antigens. Self-antigens presented by APC activated by PAMPs present during infection can then stimulate autoreactive T cells by a process known as epitope spreading. Bystander activation occurs when “bystander” T cells are activated via the pro-inflammatory cytokine milieu surrounding an infection. b In addition to pathogenic bacteria, commensals also influence the development of autoinflammatory conditions, by promoting inflammation in certain cases and preventing it in others. However, the mechanism by which commensals can be pro-inflammatory or protective remains unclear—although TH17 and TReg and the balance in their numbers clearly seem to be involved in autoimmunity, whether protective commensals such as Lactobacillus promote tolerance via Treg activity or otherwise is not known. Some pro-inflammatory commensals such as SFB have been shown to induce TH17 cells, which exacerbate the development of rheumatoid arthritis. However, for the most part, these links and the antigen specificity of the T cells involved, have yet to be fully elucidated. Specific links that have not been tested are indicated with question marks. ASF, Altered Schaedler Flora, SFB, segmented filamentous bacteria
