Abstract
Objectives:
On December 1, 2015, the Japanese government launched the Stress Check Program, a new occupational health policy to screen employees for high psychosocial stress in the workplace. As only weak evidence exists for the effectiveness of the program, we sought to estimate the risk of stress-associated long-term sickness absence as defined in the program manual.
Methods:
Participants were 7356 male and 7362 female employees in a financial service company who completed the Brief Job Stress Questionnaire (BJSQ). We followed them for 1 year and used company records to identify employees with sickness absence of 1 month or longer. We defined high-risk employees using the BJSQ and criteria recommended by the program manual. We used the Cox proportional regression model to evaluate the prospective association between stress and long-term sickness absence.
Results:
During the follow-up period, we identified 34 male and 35 female employees who took long-term sickness absence. After adjustment for age, length of service, job type, position, and post-examination interview, hazard ratios (95% confidence intervals) for incident long-term sickness absence in high-stress employees were 6.59 (3.04-14.25) for men and 2.77 (1.32-5.83) for women. The corresponding population attributable risks for high stress were 23.8% (10.3-42.6) for men and 21.0% (4.6-42.1) for women.
Conclusions:
During the 1-year follow-up, employees identified as high stress (as defined by the Stress Check Program manual) had significantly elevated risks for long-term sickness absence.
Keywords: Cox proportional hazard regression analysis, Incidence, Kaplan-Meier analysis, Mental health, Psychosocial work environment
Introduction
On December 1, 2015, the Japanese Industrial Safety and Health Law was extended to include a Stress Check Program that makes regular yearly screenings for high psychosocial stress in the workplace mandatory for enterprises with 50 or more employees1). The program requires an employer to (1) provide a survey of employee psychosocial stress, (2) inform each employee of their results, (3) arrange an interview with a physician for high-stress employees (at the employee's request), and (4) follow the physician's recommendations for improving of adverse working conditions. However, only weak evidence exists for the effectiveness of these measures2).
The Stress Check Program manual recommends using the Brief Job Stress Questionnaire (BJSQ)3) and proposes criteria for defining "high-stress" employees1). Although screening of employees with apparent mental health disorders is not the program's primary objective, practitioners need to know how valid the instrument is, since the screening process does detect some employees who need special care from mental health experts.
We recently reported that screening of high-stress employees as per the Stress Check Program manual's recommendation is informative4). However, evidence of the predictive validity of the BJSQ is lacking. The stress response measured by the BJSQ was associated with the onset of depression in a previous cohort study of 1810 Japanese employees5), but this study did not evaluate whether the program manual criteria were predictive. To our knowledge, no reports have demonstrated a prospective association between employees' health outcomes and BJSQ stress profiles (based on the program manual criteria).
Sickness absence is a major cause of lost productivity and a relevant health outcome in occupational health practice, as the cost of sickness absence and disability benefits is a substantial challenge for many workplaces and for society6). Long-term sickness absence, in particular, is associated with deterioration of employee health and work disability. Therefore, its prevention should be an important part of occupational health policy, not only to reduce costs related to sickness absence but also to improve employee health and prevent work disability7). We conducted a prospective cohort study to investigate whether the Stress Check Program's recommended criteria, and the use of the BJSQ, could identify non-sick listed employees at risk of long-term sickness absence during a 1-year follow-up.
Subjects and Methods
Setting
We conducted the study in a company in the financial services industry listed on the major stock exchanges. This company introduced the BJSQ to protect employees health and safety.
Participants
A total of 7356 male and 7362 female employees completed the BJSQ between July-August 2015 (response rate: 94%). At baseline, 32 employees were excluded because of their disease history according to past sick pay records (mental health disorder, 22; musculoskeletal disorder, 6; cardiovascular diseases, 3; and cerebrovascular diseases, 1). Thus, 14686 participants (7341 men, 7345 women; aged 20-66 years) were tracked to July 2016 using sick pay records (Fig. 1). There was no significant difference between the non-response group and the response group in terms of age. However, non-response group compared with response group had higher proportions of men (p < 0.001), those who worked in the company for less time (p < 0.05), those worked in the administrative sector (p < 0.001), and temporary employees (p < 0.01). The company provided anonymous data. Informed consent was obtained from participants using the opt-out method.
Fig. 1.
Recruitment and follow-up flow diagram
Variables and data source/measurement
(1) Outcome
We measured two types of sickness absence based on the company human resources records: paid leave of absence and applications for invalidity benefit with medical certification. For both types, sickness absence for 1 month or longer was recorded. Japanese employees commonly register absences owing to ill-health as paid leave of absence before applying for invalidity benefit. As described below, we identified 69 participants who took sickness absence and invalidity benefits. They included all the participants who took paid leave of absence (n = 60); thus, we analyzed data based on records of sickness absence for invalidity benefits.
(2) Assessment of stress profile
The BJSQ consists of 57 items used to assess job stressors, psychological and physical stress responses, and buffering factors3). The development of the BJSQ was based on the job stress model proposed by researchers from the US National Institute for Occupational Safety and Health8). The BJSQ measures the following job stressors: quantitative job overload (3 items), qualitative job overload (3 items), physical demands (1 item), job control (3 items), skill utilization (1 item), interpersonal conflict (3 items), poor physical environment (1 item), suitable jobs (1 item), and intrinsic rewards (1 item). An 18-item scale measures five aspects of psychological response: lassitude (3 items), irritation (3 items), fatigue (3 items), anxiety (3 items), and depression (6 items). An 11-item scale measures physical stress responses. In addition, the scale measures the following buffering factors: supervisor support (3 items), coworker support (3 items), and support from family and friends (3 items). The BJSQ also measures job satisfaction and life satisfaction (1 item for each). All BJSQ scales have demonstrated acceptable or high levels of internal consistency reliability and factor-based validity3). Item responses are measured on a four-point Likert-type scale [for the full questionnaire, see 9].
The program manual proposes criteria for defining high-stress employees based on the BJSQ1). High stress is defined as the highest level of stress response (criterion A) or having a moderate or higher level of stress response, together with having the highest job stressors (or lowest social support in the workplace) (criterion B). The criteria were established based on expert consensus, and criterion B was included because the program aims to improve the psychosocial work environment and reduce psychosocial stress among high-stress employees.
To calculate stress response and job stressor scores, we simply summed the item scores of the 4-point Likert scale (1 = low stress to 4 = high stress). The scores for stress response and job stressors ranged from 29 to 116, and 26 to 104, respectively. Cronbach's α coefficients were 0.78, 0.66, 0.92, and 0.94 for the job demand, job control, workplace support, and stress response scale, respectively. The proposed cutoff points were 77 for the stress response score for criterion A, 76 for the job stressor score, and 63 for the stress response score for criterion B.
(3) Demographic variables
We measured gender, age, job type (sales, claims service, administrative, or others), position (staff, manager, senior employee, temporary employee, or others), and whether participants had an interview with occupational health staff after the Stress Check examination as confounding variables. We obtained these data from the company records of the human resources department and occupational health division and combined them.
Bias
The study was conducted in a single company in a financial service. Although the response rate was high, we found differences between the non-response group and the response group in gender, length of service, job type, and position. The Stress Check Program is supposed to be conducted at yearly intervals. For this reason, we used a short follow-up period (1 year) to ensure minimal dropout. We expected that this would ensure minimal dropout. We consider the selection bias of this study in the discussion section. Regarding information bias, measurements of the studied variables (except for the self-report independent variable) were obtained from the company human resources department; the outcome measure (sickness absence records) was based on physician diagnoses, which reduced the likelihood of measurement errors. Finally, the effects of psychosocial factors at work on health outcome can vary according to participants' sociodemographic backgrounds and gender. We measured potential confounders with the help of the company and adjusted for them in the statistical analyses. We also analyzed data separately for men and women.
Statistics
Analysis was based on the sickness absence incidence rate during the 1-year follow-up, calculated separately for men and women. The participants were divided into high-stress employees and others according to the program manual and using the BJSQ at baseline (Table 1). For each participant, person-months of follow-up were allocated according to the dates of Stress Check examinations until the start date of sickness absence, the date of leaving the company (mainly age-limited retirement), or July 1, 2016, whichever occurred first. Data for leaving the company were obtained from the human resources department. A total of 517 subjects (3.5% of the analytic cohort) retired during the study period and were treated as censored cases. The total observed person-months was 172,329. Cox's proportional hazard regression analysis was used to investigate the association between stress profiles and onset of long-term sickness absence. Hazard ratios (HRs) were estimated first after adjusting for age, and then after adjusting for age, length of service, job type, position, and post-examination interview. Ordinal variables were represented by dummy variables. All probability values were 2-tailed, and values of p < 0.05 were considered statistically significant. We calculated population-attributable risk (PAR) for high stress with accompanying 95% confidence intervals (CIs). This risk is the proportion of all cases of sickness absence attributable to high stress, assuming a causal association. We calculated this as (HR-1) *p/[1+ (HR-1) *p], in which p is the prevalence of high stress in the total population at baseline and HR is the hazard ratio for incident sickness absence for high stress versus others. We adjusted the PAR estimates for covariates in a similar way to the corresponding Cox models for HRs10). We also ran subsidiary analyses to separately test the stress profiles defined by criteria A and B.
Table 1.
Baseline characteristics by gender and stress profile as defined by the Brief Job Stress Questionnaire
| Men (n=7341) | Women (n=7345) | ||||||
|---|---|---|---|---|---|---|---|
| High stress | Others | p-value | High stress | Others | p-value | ||
| No. of participants | 411 | 6930 | 1105 | 6240 | |||
| Mean age, y | 48.5 | 47.5 | .06 | 36.9 | 35.3 | <.001 | |
| Mean length of service, y | 12.6 | 14.0 | <.01 | 12.2 | 10.9 | <.001 | |
| Job type, n (%) | |||||||
| Sales | 144 (35.0) | 2924 (42.2) | <.01 | 583 (52.8) | 3383 (54.2) | <.001 | |
| Claims Service | 196 (47.7) | 2753 (39.7) | 403 (36.5) | 1903 (30.5) | |||
| Administrative | 71 (17.3) | 1244 (18.0) | 119 (10.8) | 950 (15.2) | |||
| Others | 0 (0.0) | 9 (0.1) | 0 (0.0) | 4 (0.1) | |||
| Position, n (%) | |||||||
| Staff | 156 (38.0) | 2342 (33.8) | <.001 | 1005 (91.0) | 5543 (88.8) | <.01 | |
| Manager | 80 (19.5) | 2117 (30.5) | 8 (0.7) | 138 (2.2) | |||
| Senior employee | 14 (3.4) | 443 (6.4) | 7 (0.6) | 93 (1.5) | |||
| Temporary employee | 161 (39.2) | 2019 (29.1) | 85 (7.7) | 462 (7.4) | |||
| Others | 0 (0.0) | 9 (0.1) | 0 (0.0) | 4 (0.1) | |||
| Post-examination interview by occupational health staff, n (%) | |||||||
| Had the interview | 49 (11.9) | 6 (0.1) | <.001 | 116 (10.5) | 6 (0.1) | <.001 | |
| Did not have the interview | 362 (88.1) | 6924 (99.9) | 989 (89.5) | 6234 (99.9) | |||
| Comparisons among variables were conducted by t-tests for mean age and mean length of service and by chi-square tests for job type, position, and post-examination interview by occupational health staff. | |||||||
As there is ample evidence that adverse psychosocial job characteristics cause physical disorders (such as cardiovascular, cerebrovascular,11,12) and musculoskeletal disorders or accidents13) as well as psychological distress14), we collapsed sickness absence from all the etiologies. However, to focus on social needs and the primary objective of the Stress Check system, we separately analyzed sickness absence owing to mental health disorder.
The program manual recommends that the post-examination physician interview should be conducted within 2 months of the Stress Check examination. The timing is usually determined by logistics; it takes a month to feed back the examination results to the participants, and then the employer is required to ask participants whether they wish to have an interview with a physician. A Kaplan-Meier plot was generated to show how rapidly sickness absences occurred after the Stress Check examination. IBM SPSS Statistics for Windows, Version 23 (IBM Corp., Armonk, NY, USA) was used for the statistical analyses.
The study aims and protocol were approved by the Research Ethics Committee of the Kitasato University Medical Ethics Organization (No. B15-113).
Results
Table 1 shows the relationships between stress profiles and studied variables at baseline. The prevalence of high-risk employees, defined using the recommended criteria, was 5.6% for men. Men defined as high stress were slightly older but had worked in the company for less time than those not defined as high stress. The high-stress group was more likely to work in the sales and claims service sectors. Staff members and temporary employees were more prevalent among the high-stress group. Almost 12% of the high-stress group had an interview with occupational health staff.
The prevalence of high-risk employees was 15.0% for women. Women with high stress were older and had worked for the company for longer than women without high stress. The relationship between stress profiles and employment status for women was similar to that for men. High-stress employees were more likely to work in the sales and claims service sectors and they were almost all staff members. Of high-stress women, almost 11% had an interview with occupational health staff.
During 172,329 person-months (mean: 329 days; min.: 2 days; max.: 343 days), 34 men and 35 women who took long-term sickness absence were identified. The age-adjusted HR for incident long-term sickness absence in high-stress men showed a 6-fold higher risk. After adjustment for age, length of service, job type, position, and post-examination interview, the risk for men increased to 6.6-fold (HR: 6.59). The age-adjusted HR for high-stress women was 3.11. After adjustment for age, length of service, job type, position, and post-examination interview, the HR for women was 2.77 (Table 2). The corresponding PAR for high stress was 23.8% (95% CI: 10.3-42.6) for men and 21.0% (95% CI: 4.6-42.1) for women.
Table 2.
Associations between stress profiles as defined by the Brief Job Stress Questionnaire and incident long-term sickness absence
| Person- months | No. of events | Rate/1000 person-months | Rate ratio (95% confidence interval) | ||
|---|---|---|---|---|---|
| Adjusted for age | Adjusted for age, length of service, job type, position and post-examination interview | ||||
| Men (n=7341) | |||||
| High stress | 4,681 | 9 | 1.92 | 6.13 (2.86, 13.13) | 6.59 (3.04, 14.25) |
| Others | 81,092 | 25 | 0.31 | 1 (Reference) | 1 (Reference) |
| Women (n=7345) | |||||
| High stress | 12,946 | 12 | 0.93 | 3.11 (1.54, 6.26) | 2.77 (1.32, 5.83) |
| Others | 73,610 | 23 | 0.31 | 1 (Reference) | 1 (Reference) |
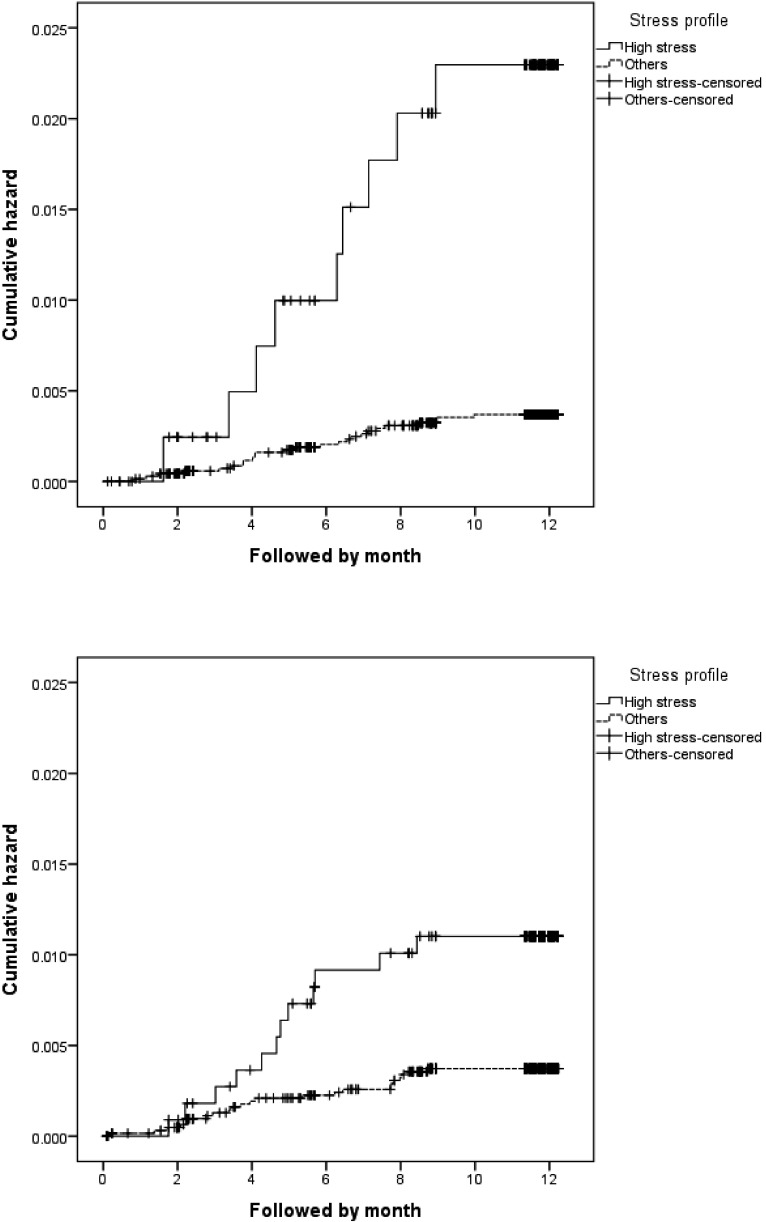
The Kaplan-Meier plots showed significant group differences for both men and women (Fig. 2). The plots indicated that the HRs started to acutely increase approximately 2 months after the Stress Check examinations and then plateaued 9 months after the examination. Most of the increase in sick absence took place during the first 6 months among women, whereas the progression was slower among men.
Fig. 2.
Cumulative hazard risks for sickness absence during 1-year follow-up in high-stress men (upper) and high-stress women (lower) according to the Stress Check Program manual
The high-stress prevalences, as defined by criterion A, were 4.5% for men and 13.2% for women. High-stress prevalences, as defined by criterion B, were 2.3% for men and 5.5% for women. We found almost the same level of HRs for each criterion as for high stress defined by a combination of criteria A and B. Reflecting the low prevalence for each criterion, the corresponding PARs were lower than those for high stress as defined by a combination of criteria A and B (Table 3).
Table 3.
Associations between stress profiles based on the respective criteria according to the Stress Check Program manual and incident long-term sickness absence
| Rate ratio (95% confidence interval) | Population- attributable risk based on full adjustment (%) | ||
|---|---|---|---|
| Adjusted for age | Adjusted for age, length of service, job type, position, and post-examination interview | ||
| Men | |||
| High stress based on criterion A | 6.54 (2.96, 14.44) | 7.17 (3.22, 15.96) | 21.9 (9.2-40.5) |
| Others | 1 (Reference) | 1 (Reference) | |
| Women | |||
| High stress based on criterion A | 3.15 (1.54, 6.45) | 2.84 (1.32, 6.08) | 19.5 (4.0-40.5) |
| Others | 1 (Reference) | 1 (Reference) | |
| Men | |||
| High stress based on criterion B | 5.89 (2.08, 16.72) | 6.28 (2.19, 18.03) | 10.7 (2.6-27.9) |
| Others | 1 (Reference) | 1 (Reference) | |
| Women | |||
| High stress based on criterion B | 3.18 (1.22, 8.28) | 2.60 (0.94, 7.22) | 8.1 (-0.3-25.6) |
| Others | 1 (Reference) | 1 (Reference) | |
| Criterion A is defined as the highest level of stress response as measured by the Brief Job Stress Questionnaire (cutoff 77) and criterion B is defined as a moderate or higher level of stress response (cutoff 63), along with having the highest job stressors (or lowest social support in the workplace) (cutoff 76), according to the Stress Check Program manual. It should be noted that there is overlap in the distribution of criteria A and B. | |||
When we restricted the analyses to only mental health disorder cases, the estimated risks increased for both men and women. The age-adjusted HR for long-term sickness absence for mental health disorder in high-stress men was 8.69 (3.72-20.32) and the fully adjusted HR was 8.68 (3.67-20.53). For high-stress women, the age-adjusted HR was 3.67 (1.79-7.54) and the fully adjusted HR was 3.29 (1.53-7.04). The corresponding PAR for high-stress men was 30.1% (13.0-52.2) and 25.6% (7.4-47.6) for high-stress women.
Discussion
During 1-year follow-up, we found that both male and female employees who identified as high stress by the Stress Check Program manual had a significantly higher risk of taking long-term sickness absence. Male high-stress employees had a 6.6-times higher risk and female high-stress employees had a 2.8-times higher risk of sickness absence compared with their respective counterparts. For both men and women, more than 20% of all cases of sickness absence were estimated to be attributable to high stress. The risk of sickness absence accelerated 2 or 3 months after the Stress Check examination. This study showed predictive validity of sickness absence for the criteria defined by the program manual using the BJSQ. These findings provide a basis for examining the effectiveness of the program in future studies. The findings also provide practical information about how quickly occupational health staff must obtain post-examination measures after the Stress Check examination.
Perceived stress was more prevalent among women than men, but stress affected sickness more for men. The findings are in line with previous occupational stress research15,16). Comparison of male and female Kaplan-Meier plots also suggested a prolonged effect of high stress on sickness absence among men. Although the magnitude of the risk for women was less than half that for men, the impact of high stress in this population (i.e., PARs) was almost the same between genders, because the prevalence of high-stress employees was higher among women (15.0%) than among men (5.6%). Eliminating high stress from this population could reduce long-term sickness absence by seven to eight persons for both men and women.
Sickness absences were defined as work absences that required a medical certification and that had an associated income replacement benefit. Long-term sickness absence has a very detrimental impact on the mental health and wellbeing of employees17). We were not able to examine shorter periods of sick leave, which might have reduced the risk estimation. Nonetheless, as sickness absence can be considered a coping strategy18), a conservative risk estimation for the association between high stress (as defined by the BJSQ) and sickness absence is probably appropriate.
It is reasonable to assume a strong association between psychosocial stress as measured by the BJSQ and sickness absence from mental health disorders, because the BJSQ was developed to measure psychosocial work environment and stress responses. There is ample evidence that psychosocial job characteristics cause cardiovascular disease, musculoskeletal disorders, accidents, and other problems. However, to predict the risk of physical disorders, longer follow-up is necessary.
Our findings provided practical information about the implementation of the Stress Check Program, which is conducted at yearly intervals. It is clear that the post-examination measures should be conducted fairly soon after the Stress Check examination. The Kaplan-Meier analyses showed that the risk of sickness absence accelerated 2 or 3 months after the Stress Check examination and the cumulative risk increased up to 9 months after the examination. It should be noted that most absentees (60 of 69) took paid leave of absence before applying for invalidity benefit and the leave period was at least 1 month.
The effectiveness of the post-examination measures should be explored in future studies. There is no convincing evidence that non-psychiatrist physician interviews and advice are effective in preventing mental health problems among employees2). In this study, there was no difference in onset of sickness absence between those who had and those who did not have the post-examination interview by occupational health staff (data not shown). Although employers should arrange for a physician interview when requested to do so by an employee with high stress, few high-stress employees (11-12%) had such interviews. The Stress Check Program also proposes following physicians' recommendations for improvement of adverse working conditions. As the concept of high stress as defined by the BJSQ combines job stressors and stress responses, the examination results could help practitioners take measures to improve workplace environment and care for employees suffering from psychological distress. The effectiveness of the measure should be evaluated using appropriate study designs and valid implementations.
We did not measure working hours in this study. Because our aim was to investigate the predictive validity of the BJSQ, we did not investigate the effect of the BJSQ and sickness absence independent of work hours, or the mechanisms by which work stress leads to sickness absence. However, information about work hours is practically very useful. Work hours are closely related to work stress and long working hours constitute a relevant background factor in work stress19); therefore, they are primary intervention targets of the post-examination physician interview. Furthermore, a combination of work hours and the BJSQ measure may improve the screening performance to detect high-stress employees.
The present study is the largest of its kind and provides reliable information about the studied variables (except for the exposure variable) using company data. However, the study has several limitations. Although the sample was large, we could not perform stratified analyses or outcome-specific analyses other than for mental health disorder; such analyses may provide additional practical information. The generalizability of our findings is limited because the study was conducted in a single company and most of the employees were white-collar employees. The relatively large proportion of men who were temporary employees was not representative. Under-representation of men and temporary employees in this study might have underestimated the effect of high stress, while under-representation of those working in administrative jobs may have had a reverse effect. Further studies are necessary to confirm the predictive validity of the BJSQ for working populations in other industries or companies. We measured as many potentially confounding variables as the company data permitted, but residual cofounding variables may exist, such as work-family conflicts.
In conclusion, using a 1-year follow-up study, we demonstrated predictive validity for the criteria defined by the program manual using the BJSQ. The next steps are to confirm the effectiveness of the program components: (1) decreasing the risk of employee mental health problems through periodic surveys and feedback about stress to employees, (2) prevention of mental health problems by screening high-risk employees and offering them a physician interview, and (3) reducing psychological distress among employees by improving the psychosocial work environment, which includes education and training of managers, in conjunction with the program.
Acknowledgments: The present study was supported by a Health and Labour Sciences Research Grant 2015-2017 (H27-Rodo-Ippan-004) from the Ministry of Health, Labour and Welfare, Japan. We thank Diane Williams, PhD, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Conflicts of interest: The authors declare that there are no conflicts of interest.
References
- 1). Ministry of Health, Labour and Welfare, Japan. [Online]. 2015[cited 2016 Dec. 23]; Available from: URL: http://www.mhlw.go.jp/bunya/roudoukijun/anzeneisei12/
- 2). Kawakami N, Tsutsumi A. The Stress Check Program: a new national policy for monitoring and screening psychosocial stress in the workplace in Japan. J Occup Health 2016; 58: 1-6. [DOI] [PubMed] [Google Scholar]
- 3). Shimomitsu T, Haratani T, Nakamura K, et al. Final development of the Brief Job Stress Questionnaire mainly used for assessment of the individuals. In: Kato M. The Ministry of Labor sponsored grant for the prevention of work-related illness. Tokyo: Tokyo Medical University; 2000. p. 126-164 (in Japanese). [Google Scholar]
- 4). Tsutsumi A, Inoue A, Eguchi H. How accurately does the Brief Job Stress Questionnaire identify with or without potential psychological distress? J Occup Health 2017; 59: 356-360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5). Wada K, Sairenchi T, Haruyama Y, et al. Relationship between the onset of depression and stress response measured by the Brief Job Stress Questionnaire among Japanese employees: a cohort study. PLoS One 2013; 8 (2): e56319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6). Lund T, Kivimäki M, Labriola M, et al. Using administrative sickness absence data as a marker of future disability pension: the prospective DREAM study of Danish private sector employees. Occup Environ Med 2008; 65: 28-31. [DOI] [PubMed] [Google Scholar]
- 7).van Amelsvoort LG, Jansen NW, Kant I. Addressing long-term sickness absence: moving beyond disease, illness and work-related factors for effective prevention. Scand J Work Environ Health 2017; 43 (1): 1-4. doi: 10.5271/sjweh.3605. Epub 2016 Dec 2. [DOI] [PubMed] [Google Scholar]
- 8). Hurrell JJ, McLaney M. Exposure to job stress: a new psychometric instrument. Scand J Work Environ Health 1988; 14 (Supple 1): 27-28. [PubMed] [Google Scholar]
- 9). Ministry of Health, Labour and Welfare, Japan. [Online]. 2015[cited 2017 Jul. 30]; Available from: URL: http://www.mhlw.go.jp/bunya/roudoukijun/anzeneisei12/dl/160621-1.pdf
- 10). Day LE. Confidence limits made easy: interval estimation using a substitution method. Am J Epidemiol 1998; 147 (8): 783-790. [DOI] [PubMed] [Google Scholar]
- 11). Theorell T, Jood K, Jarvholm LS, et al. A systematic review of studies in the contributions of the work environment to ischaemic heart disease development. Eur J Public Health 2016; 26 (3): 470-477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12). Huang Y, Xu S, Hua J, et al. Association between job strain and risk of incident stroke: A meta-analysis. Neurology 2015; 85 (19): 1648-1654. [DOI] [PubMed] [Google Scholar]
- 13).Sommer TG, Svendsen SW, Frost P. Sickness absence and permanent work disability in relation to upper- and lower-body pain and occupational mechanical and psychosocial exposures. Scand J Work Environ Health 2016; 42 (6): 481-489. doi: 10.5271/sjweh.3600. Epub 2016 Oct 13. [DOI] [PubMed] [Google Scholar]
- 14). Theorell T, Hammarstrom A, Aronsson G, et al. A systematic review including meta-analysis of work environment and depressive symptoms. BMC Public Health 2015; 15: 738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15). Belkić K, Landsbergis PA, Schnall PL, et al. Is job strain a major source of cardiovascular disease risk? Scand J Work Environ Health 2004; 30 (4): 85-128. [DOI] [PubMed] [Google Scholar]
- 16). Tsutsumi A, Kayaba K, Tsutsumi K, et al. Association between job strain and prevalence of hypertension: a cross sectional analysis in a Japanese working population with a wide range of occupations: the Jichi Medical School Cohort Study. Occup Environ Med 2001; 58 (6): 367-373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17). OECD. Sick on the Job? Myths and Realities about Mental Health and Work, Mental Health and Work, OECD Publishing; 2011. [Online]. doi: https://doi.org/10.1787/9789264124523-en
- 18). Kristensen TS. Sickness absence and work strain among Danish slaughterhouse workers: an analysis of absence from work regarded as coping behaviour. Soc Sci Med 1991; 32 (1): 15-27. [DOI] [PubMed] [Google Scholar]
- 19). Härmä M. Workhours in relation to work stress, recovery and health. Scand J Work Environ Health 2006; 32 (6): 502-514. [DOI] [PubMed] [Google Scholar]