Abstract
Background
Several studies have put an effort to minimize the tourniquet pain and complications after conventional double tourniquet intravenous regional anesthesia (IVRA). We expressed in our hypothesis that an upper arm single wide tourniquet (ST) may serve a better clinical efficacy rather than the conventional upper arm double tourniquet (DT) in distal upper extremity surgeries.
Methods
In this randomized controlled trial, 80 patients undergoing upper limb orthopedic surgeries were randomized into two groups. IVRA was administered using lidocaine in both groups. Tourniquet pain was recorded based on visual analogue scale (VAS). In case of pain (VAS>3) in the DT group, the proximal tourniquet was replaced with a distal tourniquet while fentanyl 50µg was injected in the ST group. The onset time of tourniquet pain, time to reach to maximum tourniquet pain and the amount of fentanyl consumption were compared between the two groups.
Results
No significant difference was seen in demographic characteristics. The onset time of tourniquet pain (VAS=1) in the ST group (26.9±13.2 min) was longer than that of the DT group (13.8±4.8 min) (P<0.0001). The median of time to reach to maximum tourniquet pain (VAS>3) in DT and ST groups were 25 and 40 minutes, respectively; indicating that the patients in ST group reached to pain level at a significantly later time (P<0.0001). The total opioid consumption in the DT group (61 µg) was significantly lower than the ST group (102 µg) (P<0.0001); however, both groups were similar regarding fentanyl consumption before 40 minutes of surgeries.
Conclusion
It seems that in upper limb orthopedic surgeries with less than 40-minute duration, a single tourniquet may serve as a proper alternative opposed to the conventional double tourniquet technique.
Level of evidence: II
Keywords: Bier block, Opioid consumption, Orthopedic surgery, Regional anesthesia, Tourniquet pain
Introduction
August Bier, a German surgeon, introduced intravenous regional anesthesia (IVRA), known as the Bier block, in 1908 (1, 2). The method involves the injection of a local anesthetic into the venous system in the upper or lower extremities, which is isolated from the blood circulation by a double tourniquet (1, 3). Few studies suggest that intravenous injection of a retrograde local anesthetic may cause high tissue concentrations of the local anesthetic by increasing the filtration and permeation (4). Some advantages of this technique could be convenience and speed of analgesia, feasibility to perform in various operation theatres, and hindering the operative site from bleeding (5-11).
Several studies have modified this technique; each one attempted to find a way to postpone the onset of tourniquet pain, decrease the local anesthetic dose to nontoxic levels, and improve the quality of anesthesia (1, 3-7, 12-14). Application of an additional forearm tourniquet in several studies have resulted in need for smaller amounts of local anesthetic as well as faster onset of sensory and motor block; However, the additional forearm tourniquet may disturb and obstruct the surgical field especially in wrist surgeries (1, 9, 12, 15-17).
Almost all studies on modified cuff techniques and IVRA were attributed to placing an additional or temporary forearm cuff while few studies were performed on cuff size and double- vs single- arm tourniquet (1, 3, 4, 6, 12, 13, 15, 20, 22). Estebe et al. examined a wide (14 cm) and a narrow cuff (7 cm) tourniquet with regards to the occlusion pressure and the resulting pain (23). They found that pain was developed later and slower in all cases using wide tourniquet, and that the wide cuffs were much more effective than the narrow cuffs with respect to occlusion pressure. The rationale was that as the cuff provides compression (sagittal forces) and stretching (axial forces), it may damage the soft tissue including nerves and vessels by mechanical pressure. On the other hand, it was also suggested that a narrower tourniquet cuff results in more pain (21, 23). We have aimed to compare the single upper arm tourniquet with double one for open reduction and internal fixation of distal radius fracture. We hypothesized that in such surgeries, a single arm tourniquet may have more effective pain control rather than the double tourniquet technique.
Materials and Methods
The IRB and ethics committee approved the conduct of this randomized parallel controlled trial and the study was registered in the Iranian registry of clinical trials (IRCT2013041111898N4). The study was conducted during June 2013-November 2014 in accordance with ethical standards of Helsinki and the patients were briefed about the study design and signed the informed consent forms prior to enrolment. The inclusion criteria comprised of patients between 20-50 years old; ASA physical status I; and orthopedic surgery times between 40 to 60 minutes. Obesity (BMI>30); peripheral vascular disease; Reynaud’s phenomenon; scleroderma; epilepsy; sickle cell anemia; met-hemoglubinemia; history of drug allergies; underlying diseases such as cardiovascular disease; hypertension; coagulopathy disorders; renal failure; drug abuse; lack of patient’s cooperation; and skin infections in axillary region were defined as the exclusion criteria. Patients would be excluded if high doses of opioids (>3µg/kg fentanyl) were needed while blocking the limb or during the operation. Patients were randomized using random block method into the Single Tourniquet (ST) and Double Tourniquet (DT) groups. An anesthesiologist who was blinded to the patient allocation performed the block and concealed the tourniquet site with a sterile drape.
In accordance with a previous study and considering the clinical differences in VAS scores, the sample size was calculated as 40 patients in each treatment group with a power of 90% and confidence interval of 95%. In this per-protocol study among 113 eligible patients, 12 patients were excluded from the study and 21 patients were disqualified during the surgeries; therefore, a total of 80 patients were randomized into the DT (Double Tourniquet) or ST (Single Tourniquet) groups [Figure 3].
Figure 3.
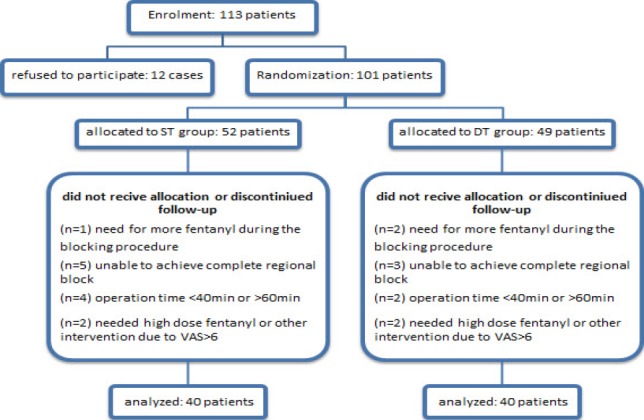
Patients’ flow diagram.
Two peripheral i.v. lines were placed on both operative and non-operative hands in the operating room. ECG, NIBP and pulse oximeter monitoring were established for all patients. All patients underwent monitoring for vital signs, blood pressure, heart rate and respiration throughout the whole operation. Patients’ MBP (Mean Blood Pressure) and HR (Heart Rate) were recorded pre-operatively, and then every 5 minutes until the end of the procedure.
Intravenous midazolam (2 mg) and fentanyl (50 μg) were injected prior to commencing the IVRA. The hand was placed above the heart and blood was allowed to drain using an Esmarch bandage in order to prepare the patient for the block. A 12cm-width tourniquet in the ST group and two tourniquets (6cm each) in the DT group were placed in the arm zone [Figures 1; 2]. The tourniquets were inflated until the radial artery pulse as well as the pulsed oxy-meter waves were both faded. This was symptomatic for proper tourniquet pressure. Lidocaine 3mg/kg (~40cc Lidocaine 0.5% for an average 70 kg person) was injected in both groups in order to perform the block. Patients were monitored during the infusion for signs and symptoms of local anesthetic toxicity. The time when a complete block was achieved after the injection was considered as time zero. Patients with hemodynamic instability and/or changes in consciousness or those who failed to achieve a complete sensory block after 5 minutes were excluded from the study. Also, patients with operation times less than 40 minutes or more than 60 minutes were excluded from the study. The anesthesiologist assistant recorded the vital signs and level of tourniquet pain (based on visual analogue scale: VAS) every 5 minutes by asking the patient to point out the severity of their pain on a 10-centimeter ruler based on a 0-10 score. VAS is an 11-point numeric scale with zero representing no pain and 10 representing the worst imaginable pain.
Figure 1.

Single tourniquet.
Figure 2.

Double tourniquet.
The time was recorded for all patients in both groups, when the intensity of the tourniquet pain reached one (VAS=1). When the intensity of tourniquet pain reached more than three (VAS>3) in the DT group, the distal tourniquet was inflated and the proximal tourniquet was deflated; however if the pain was persistent, Fentanyl 50µg was re-administered. In cases of pain with VAS>3 in the ST group Fentanyl 50µg was also administered intravenously. Additional Fentanyl was subsequently given if necessary when the VAS score remained >3. Fentanyl consumption rates were recorded and compared in both groups. The time to reach VAS>3 was considered as the primary outcome and Fentanyl consumption as the secondary outcome. Vital signs, time of tourniquet pain, rate of opioid consumption and local anesthetic toxicity were measured in all patients in both groups.
SPSS software version 21 (Chicago, IL) was used for statistical analysis. The response variables were evaluated for normal distribution according to the Kolmogorov-Smirnov test before comparing the two groups. Independent t-test was used to compare the opioid consumption between the two groups. The Kaplan Meier Survival Analysis as well as the Tarone-Ware test were used to evaluate and compare the “time to reach to VAS>3” and the opioid consumption between the two groups. The significance level was set two-sided at P<0.05.
Results
The demographic characteristics including age, gender, BMI and duration of surgery were homogeneous in both groups (P>0.05) [Table 1]. The time to reach to the tourniquet pain level (VAS=1) in the ST group (26.9±13.2 min) was significantly longer than that of the DT group (13.8±4.8 min) (P<0.0001). The median of the time to reach to (VAS>3) was shorter in the DT group, since it reached at 25 minute postoperatively and it declined after switching the proximal tourniquet with the distal one; while it was longer in ST group and reached to VAS>3 after 40 minutes [Figure 4]. According to repeated measure analysis and the Greenhouse-Geisser Test, the trend of VAS changes was significantly different between the two groups (P<0.0001). The Kaplan Meier diagram illustrated that the survival of reaching to VAS>3 (Critical Pain Point) was longer in the ST group compared with the DT group (42.0±1.7 vs 26.8±1.0, P<0.001) [Figure 5; Table 2].
Table 1.
Demographic characteristics
| DT | ST | P-value | |
|---|---|---|---|
| Gender: Male/Female (n) | 32/8 | 30/10 | 0.59 |
| Surgery Duration: Mean±SD (min) | 57.2±3.2 | 56.3±4.1 | 0.14 |
| Weight: Mean±SD (kg) | 73.2±9.6 | 71.6 | 0.46 |
| BMI: Mean±SD | 24.9±3 | 24.4±2.9 | 0.45 |
| Tourniquet pneumatic pressure | 258±35 | 207±42 | .0001 |
| Age: Mean± SD | 42.85±8.71 | 41.42±8.69 | 0.46 |
| Block onset: Mean± SD(min) | 4.18±0.42 | 4.35±0.44 | 0.76 |
DT: double tourniquet; ST: single tourniquet; Std Dev: standard deviation; BMI: body mass index
Figure 4.
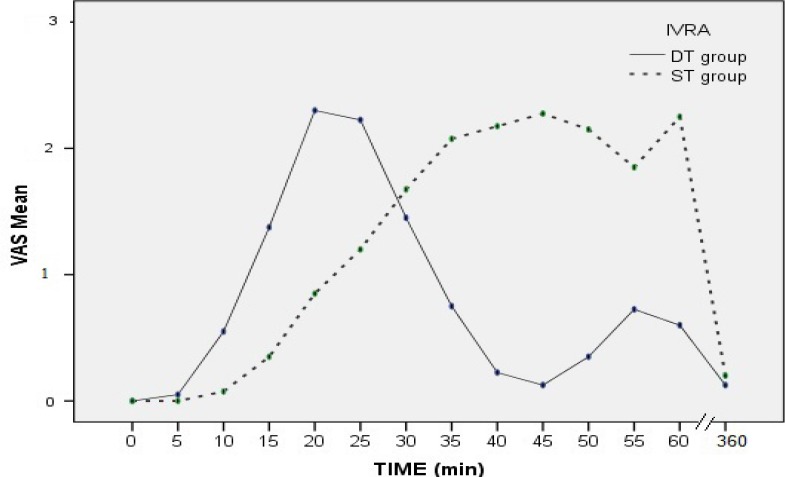
Changes in pain intensity (VAS) in both groups.
Figure 5.
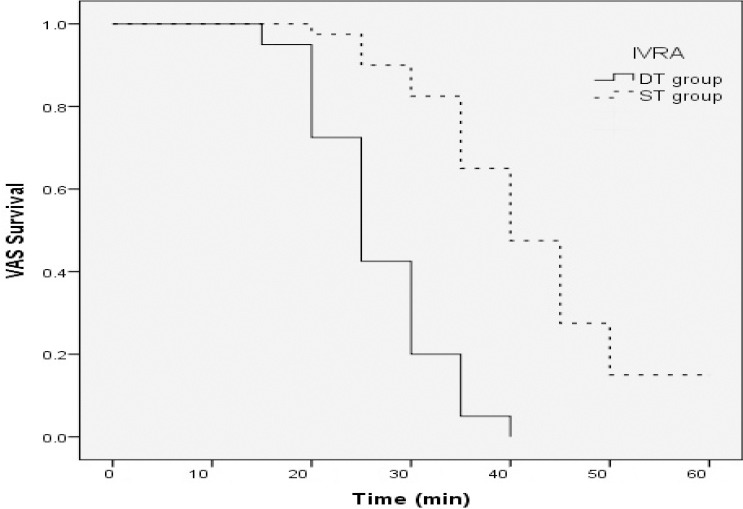
Kaplan Meier Diagram of the survival time of reaching VAS>3 (Critical Pain Point).
Table 2.
Comparing the survival of reaching to VAS>3 (Critical Pain Point) in the two studied groups
| Mean | Median | |||||
|---|---|---|---|---|---|---|
| Estimate | Std Err | CI-95% | Estimate | Std Err | CI-95% | |
| DT | 26.8 | 1.0 | 24.7 - 28.7 | 25 | 1.3 | 22.4 - 27.6 |
| ST | 42 | 1.7 | 38.7 - 45.3 | 40 | 2.1 | 35.9 - 44.1 |
| Total | 34.4 | 1.3 | 31.8 - 36.9 | 35 | 1.7 | 31.7 - 38.3 |
DT: double tourniquet; ST: single tourniquet; Std Err: standard error; CI-95%: confidence interval 95%
The total Fentanyl consumption in the DT group (61 µg) was significantly lower than the ST group (102 µg) (P<0.0001), indicating a lower need for pain control medication in patients in ST group (P<0.001). The mean arterial pressure showed no significant difference between the two groups until 40 minutes [Table 3].
Table 3.
Intra-operative opioid (fentanyl) consumption (µg)
| Total fentanyl | Before 40min fentanyl | |||
|---|---|---|---|---|
| Mean± SD | P | Mean± SD | P | |
| DT (n=40) | 61±18 | <0.0001 | 53±13 | >0.05 |
| ST (n=40) | 102±23 | 59±16 | ||
DT: double tourniquet; ST: single tourniquet; Std Dev: standard deviation
Discussion
The mechanism of tourniquet pain is still poorly understood, but is probably multifactorial. Cole suggested that tourniquet pain had both a superficial and a deep component and maybe caused by compression or possibly ischemia of large nerves (24). Nerve compression was classically thought to be mediated by unmyelinated slow-conducting C fibres normally inhibited by earlier arriving fast impulses conducted by myelinated A-δ fibers. Mechanical compression would block the large A-δ fibers, leaving uninhibited C fibers still functioning (25, 26). Pressure-related injuries to the underlying skin, nerve, muscle and blood vessels are dependent on both the duration and pressure of tourniquet inflation. These result from tissue compression under the tourniquet and from ischaemia beneath and distal to the device (27).
In our study, surgeries with durations between 40 to 60 minutes were analyzed. The results of our study showed that the median time to reach tourniquet pain (VAS>3) in the ST group was longer than the DT group. It shows that the single tourniquet can be a more proper alternative for upper limb surgeries that span less than 40 minutes. One may suggest that if the orthopedic surgeon estimates the operation duration to be less than 40 minutes, the anesthetist could prefer the single tourniquet rather than double one.
Our study demonstrated that in distal upper extremity surgeries, single tourniquet patients tolerated the tourniquet pain for a longer duration rather that double tourniquet group; however, the mean total Fentanyl consumption was significantly higher in the single tourniquet group. If we categorize the surgeries by the time duration, in less than 40min operations, single tourniquet not only provided a longer time to reach to tourniquet pain but also the opioid consumption was similar to the double tourniquet group. Longer time of tourniquet tolerance may provide anesthesiologist with better post-op pain management and better patient recovery. To our knowledge, there has been no similar study comparing single with double tourniquet in the IVRA setting for distal upper extremity orthopedic surgeries and it could be considered as a pilot study for further ones.
Using a forearm single tourniquet instead of an arm double tourniquet in previous studies was attributed to less intraoperative pain (1-3). In a study by Hutchinson and McClinton, it was shown that the time of tourniquet analgesia in the single forearm tourniquet was 45% longer than the upper arm tourniquet technique (28). Applying forearm single tourniquet instead of forearm double tourniquet may induce less pain (1, 4-7, 12-14, 18). However, there are some studies with controversial opinions (17, 19). We applied the tourniquets in the upper arm instead of forearm; hence, operations in the proximal forearm could be performed. In the forearm tourniquet technique there is a less possibility of blockade in anterior and posterior intra-osseous arteries and consequently lesser leakage of local anesthetic into the blood circulation (1, 29). Since we needed to change the tourniquets in the conventional double tourniquet technique, the leakage of local anesthetic into the blood flow and creating symptoms of poisoning was probable. However, in the single tourniquet technique the possibility of local anesthetic leakage into blood flow was less than that of the previous techniques.
The inflation pressure of the pneumatic tourniquets is disputable (30). Some studies advocate a standard increase of 100mmHg above thesystolic pressure. In Estebe et al. study, fading the radial pulse was considered as the sign of maximum tourniquet insufflation (instead of inflating tourniquet at 100mmHg above the systolic pressure) and it provided less pain and longer tourniquet tolerating time (23). We applied the same protocol in our study in both groups as well. Also, mechanical trauma under the cuff can be minimized by reducing the pressure per unit area. The force required to occlude the artery is a product of the inflation pressure and the area under the cuff. Therefore, a wider cuff enables a lower inflation pressure to be used to achieve arterial occlusion (29). The optimal dose of lidocaine for IVRA is not clearly defined; however, it should not exceed 300mg (31). We injected the lidocaine dose based on references of 3mg/kg (0.5% solution) in both groups (28) and we did not detect any signs of local anesthetic toxicity in either of both groups.
There are several limitations in this study. Firstly, we ought to inform patients in both groups about both single and double tourniquet techniques so the patients were aware of the group allocation and the blindness of the study was compromised; so we could not set a blinded study design. However, we did what we could to blind the assessor anesthesiologist (by concealing the tourniquet site with a drape) and the statistical analyzer. To perform a randomized clinical trial, we suggest patient sedation prior to fixing the tourniquets. In this study, we only used lidocaine as a blocking agent; this could be another limitation of our study since by adding benzodiazepines and other additive sedatives, we may reduce local anesthetic complications.
It seems that the use of single tourniquets in surgeries on upper limb orthopedics that span a time of less than 40 minutes could be a good alternative to the conventional double tourniquet technique.
All named authors hereby declare that they have no conflicts of interest to disclose.
All above-mentioned authors state that they cooperate in conducting the manuscript. They also state that they had substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data; drafting the article or revising it critically for important intellectual content and final approval of the version to be published.
References
- 1.Chiao FB, Chen J, Lesser JB, Resta-Flarer F, Bennett H. Single-cuff forearm tourniquet in intravenous regional anaesthesia results in less pain and fewer sedation requirements than upper arm tourniquet. Br J Anaesth. 2013;111(2):271–5. doi: 10.1093/bja/aet032. [DOI] [PubMed] [Google Scholar]
- 2.Choyce A, Peng P. A systematic review of adjuncts for intravenous regional anesthesia for surgical procedures. Can J Anaesth. 2002;49(1):32–45. doi: 10.1007/BF03020416. [DOI] [PubMed] [Google Scholar]
- 3.Frank R, Cowan BJ, Lang S, Harrop AR, Magi E. Modification of the forearm tourniquet techniques of intravenous regional anaesthesia for operations on the distal forearm and hand. Scand J Plast Reconstr Surg Hand Surg. 2009;43(2):102–8. doi: 10.1080/02844310802576420. [DOI] [PubMed] [Google Scholar]
- 4.Davis R, Keenan J, Meza A, Danaher P, Vacchiano C, Olson RL, et al. Use of a simple forearm tourniquet as an adjunct to an intravenous regional block. AANA J. 2002;70(4):295–8. [PubMed] [Google Scholar]
- 5.Farrell RG, Swanson SL, Walter JR. Safe and effective IV regional anesthesia for use in the emergency department. Ann Emerg Med. 1985;14(4):288–92. doi: 10.1016/s0196-0644(85)80088-3. [DOI] [PubMed] [Google Scholar]
- 6.Johnson CN. Intravenous regional anesthesia: new approaches to an old technique. CRNA. 2000;11(2):57–61. [PubMed] [Google Scholar]
- 7.Tham CH, Lim BH. A modification of the technique for intravenous regional blockade for hand surgery. J Hand Surg Br. 2000;25(6):575–7. doi: 10.1054/jhsb.2000.0423. [DOI] [PubMed] [Google Scholar]
- 8.Soleimanha M, Sedighinejad A, Haghighi M, Nabi BN, Mirbolook AR, Mardani-Kivi M. Hemodynamic and arterial blood gas parameters during cemented hip hemiarthroplasty in elderly patients. Arch Bone Jt Surg. 2014;2(3):163–7. [PMC free article] [PubMed] [Google Scholar]
- 9.Haghighi M, Sedighinejad A, Mirbolook A, Naderi Nabi B, Farahmand M, Kazemnezhad Leili E, et al. Effect of intravenous intraoperative esmolol on pain management following lower limb orthopedic surgery. Korean J Pain. 2015;28(3):198–202. doi: 10.3344/kjp.2015.28.3.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Soleimanha M, Haghighi M, Mirbolook A, Sedighinejad A, Mardani-Kivi M, Naderi-Nabi B, et al. A survey on transfusion status in orthopedic surgery at a trauma center. Arch Bone Jt Surg. 2016;4(1):70–4. [PMC free article] [PubMed] [Google Scholar]
- 11.Sedighinejad A, Haghighi M, Naderi Nabi B, Rahimzadeh P, Mirbolook A, Mardani-Kivi M, et al. Magnesium sulfate and sufentanil for patient-controlled analgesia in orthopedic surgery. Anesth Pain Med. 2014;4(1):e11334–9. doi: 10.5812/aapm.11334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chong AK, Tan DM, Ooi BS, Mahadevan M, Lim AY, Lim BH. Comparison of forearm and conventional Bier's blocks for manipulation and reduction of distal radius fractures. J Hand Surg Eur Vol. 2007;32(1):57–9. doi: 10.1016/j.jhsb.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 13.Karalezli N, Karalezli K, Iltar S, Cimen O, Aydogan N. Results of intravenous regional anaesthesia with distal forearm application. Acta Orthop Belg. 2004;70(5):401–5. [PubMed] [Google Scholar]
- 14.Perlas A, Peng PW, Plaza MB, Middleton WJ, Chan VW, Sanandaji K. Forearm rescue cuff improves tourniquet tolerance during intravenous regional anesthesia. Reg Anesth Pain Med. 2003;28(2):98–102. doi: 10.1053/rapm.2003.50036. [DOI] [PubMed] [Google Scholar]
- 15.Arslanian B, Mehrzad R, Kramer T, Kim DC. Forearm Bier block: a new regional anesthetic technique for upper extremity surgery. Ann Plast Surg. 2014;73(2):156–7. doi: 10.1097/SAP.0b013e318276da4c. [DOI] [PubMed] [Google Scholar]
- 16.Haghighi M, Soleymanha M, Sedighinejad A, Mirbolook A, Naderi Nabi B, Rahmati M, et al. The effect of magnesium sulfate on motor and sensory axillary plexus blockade. Anesth Pain Med. 2015;5(1):e21943–8. doi: 10.5812/aapm.21943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Odinsson A, Finsen V. The position of the tourniquet on the upper limb. J Bone Joint Surg Br. 2002;84(2):202–4. doi: 10.1302/0301-620x.84b2.12777. [DOI] [PubMed] [Google Scholar]
- 18.Chan CS, Pun WK, Chan YM, Chow SP. Intravenous regional analgesia with a forearm tourniquet. Can J Anaesth. 1987;34(1):21–5. doi: 10.1007/BF03007677. [DOI] [PubMed] [Google Scholar]
- 19.Edwards SA, Harper GD, Giddins GE. Efficacy of forearm versus upper arm tourniquet for local anaesthetic surgery of the hand. J Hand Surg Br. 2000;25(6):573–4. doi: 10.1054/jhsb.2000.0420. [DOI] [PubMed] [Google Scholar]
- 20.Graham B, Breault MJ, McEwen JA, McGraw RW. Occlusion of arterial flow in the extremities at subsystolic pressures through the use of wide tourniquet cuffs. Clin Orthop Relat Res. 1993;286:257–61. [PubMed] [Google Scholar]
- 21.Pedowitz RA, Gershuni DH, Botte MJ, Kuiper S, Rydevik BL, Hargens AR. The use of lower tourniquet inflation pressures in extremity surgery facilitated by curved and wide tourniquets and an integrated cuff inflation system. Clin Orthop Relat Res. 1993;287:237–44. [PubMed] [Google Scholar]
- 22.Coleman MM, Peng PW, Regan JM, Chan VW, Hendler AL. Quantitative comparison of leakage under the tourniquet in forearm versus conventional intravenous regional anesthesia. Anesth Analg. 1999;89(6):1482–6. doi: 10.1097/00000539-199912000-00031. [DOI] [PubMed] [Google Scholar]
- 23.Estebe JP, Le Naoures A, Chemaly L, Ecoffey C. Tourniquet pain in a volunteer study: effect of changes in cuff width and pressure. Anaesthesia. 2000;55(1):21–6. doi: 10.1046/j.1365-2044.2000.01128.x. [DOI] [PubMed] [Google Scholar]
- 24.Cole F. Tourniquet pain. Curr Res Anesth Analg. 1952;31(1):63–4. [PubMed] [Google Scholar]
- 25.Gielen MJ, Stienstra R. Tourniquet hypertension and its prevention: a review. Reg Anesth. 1991;16(4):191–4. [PubMed] [Google Scholar]
- 26.Hodgson AJ. A proposed etiology for tourniquet-induced neuropathies. J Biomech Eng. 1994;116(2):224–7. doi: 10.1115/1.2895723. [DOI] [PubMed] [Google Scholar]
- 27.Kam PC, Kavanaugh R, Yoong FF. The arterial tourniquet: pathophysiological consequences and anaesthetic implications. Anaesthesia. 2001;56(6):534–45. doi: 10.1046/j.1365-2044.2001.01982.x. [DOI] [PubMed] [Google Scholar]
- 28.Hutchinson DT, McClinton MA. Upper extremity tourniquet tolerance. J Hand Surg Am. 1993;18(2):206–10. doi: 10.1016/0363-5023(93)90347-6. [DOI] [PubMed] [Google Scholar]
- 29.Sanders R. The tourniquet. Instrument or weapon? 1973;5(2):119–23. doi: 10.1016/0072-968x(73)90051-x. [DOI] [PubMed] [Google Scholar]
- 30.Barry LA, Balliana SA, Galeppi AC. Intravenous regional anesthesia (Bier block) Techniq Regional Anesthesia Pain Manage. 2006;10(3):123–31. [Google Scholar]
- 31.Rosenberg PH, Veering BT, Urmey WF. Maximum recommended doses of local anesthetics: a multifactorial concept. Reg Anesth Pain Med. 2004;29(6):564–75. doi: 10.1016/j.rapm.2004.08.003. [DOI] [PubMed] [Google Scholar]


