Abstract
Background
Stroke is becoming an increasingly serious public health issue in Ethiopia and the paucity of data specific to the Ethiopian setting is limiting the formulation of an appropriate response.
Objective
This study aimed to describe types, risk factors, management patterns, and outcomes among stroke patients treated at a tertiary teaching hospital in northern Ethiopia from 2012 to 2014.
Design
Medical record review with a standardized abstraction tool was used to obtain all data for this retrospective case study. Data was entered in EpiInfo Version 7 and analyzed using STATA12. Descriptive statistics were used to explore differences among stroke subtypes and compare with other sub-Saharan African countries.
Results
Among 142 stroke patients (mean age 62.8 ± 15.6 years, 54.2% male), ischemic stroke was the most frequent subtype (55.6%) followed by intracerebral hemorrhage (32.4%) and subarachnoid hemorrhage (5.6%). 38.0% of patients had pre-existing hypertension and 4.9% had pre-existing diabetes, and most were not on any treatment. 66.2% of patients were hypertensive at hospital arrival and nearly all presented with focal neurological deficit. Less than 10% arrived at the hospital within 3 h of stroke; nearly half (47.9%) were delayed over 24 h. 76.1% received CT Scan. We observed 12.0% in-hospital mortality.
Conclusions
Ischemic stroke was the predominant form of stroke, although to a lesser degree than in studies from developed countries. Under-diagnosing of hypertension and other risk factors and delayed presentation at the hospital are the major challenges to address.
Keywords: Cerebrovascular accident, Ethiopia, Stroke, Epidemiology, Hospital, Medical record review
Highlights
-
•
Low ischemic to hemorrhagic stroke ratio compared with developed countries
-
•
Hypertension and other stroke risk factors were under-identified and under-treated.
-
•
Less than 10% of patients reached the hospital within 3 h of stroke symptoms.
-
•
Financial and social barriers to accessing CT Scan affected quality of stroke care.
1. Introduction
Recent studies have revealed that Ethiopia is beginning to enter the epidemiologic shift, where the burden of non-communicable diseases (NCDs) such as cardiovascular disease (CVD), cancers, diabetes, chronic respiratory diseases, and injury is increasing while communicable diseases simultaneously remain highly prevalent [1]. According to the WHO, NCDs are estimated to account for 30% of all deaths in Ethiopia [2], with stroke being one of the most prominent of the NCDs. The Global Burden of Disease Project stated that in 2010 stroke caused 642,000 years of life lost (YLL) due to premature mortality, a 31% increase in stroke-attributable YLL since 1990. Compared with other causes of burden, stroke ranked as the most burdensome NCD and the 13th highest overall cause of YLL in Ethiopia in 2010 [3]. A 2012 surveillance study done on adult deaths in Addis Ababa showed that NCDs accounted for 51% of all mortality, with cerebrovascular accident or stroke accounting for 11% of all-cause mortality and 37% of NCD mortality [1].
It has been estimated that 68% of adult Ethiopians in the country's capital city, Addis Ababa, have one or more of the following CVD risk factors: daily smoking, regular khat chewing, binge drinking, obesity, abdominal obesity, physical inactivity, or high blood pressure [4]. Although currently there exists a pronounced urban–rural gradient in the prevalence of these risk factors, the differential is narrowing as the population urbanizes [4]. Well-established cohort studies in the United States have demonstrated that stroke risk varies by race and ethnicity [5], so Ethiopians may also experience different risk factors from those associated with stroke in other populations, or at least the risk factors might occur at a different magnitude or relative importance. For example, a study done by Ethiopian-born physicians residing in the United States found that the average body mass index (BMI) at which most Ethiopians develop type-2 diabetes mellitus is 25 kg/m2 (Dr Elias S. Siraj MD, FACP, FACE, Professor of Medicine; Director, Diabetes Program; Program Director, Endocrinology Fellowship Temple University School of Medicine and Hospital, 2010). However, two national surveys conducted in the United States found that more than 75% of diabetes, hypertension, and dyslipidemia patients had a BMI greater than 25 kg/m2 [6]. This comparison suggests that Ethiopians may develop type-2 diabetes mellitus at a lower than typical BMI. The WHO 2014 Africa Regional Health Report states that risk factors like obesity, hypertension, diabetes mellitus, dyslipidemia, and chronic rheumatic heart disease tend to occur at younger ages in the African Region than in many developed countries [7], [8]. In addition, several prior hospital based studies conducted in Ethiopia reported unusually high proportions of hemorrhagic stroke [9], [10], [11], suggesting that there may be distinctive factors affecting the dynamics of stroke in the Ethiopian population.
Thus, this study was conducted to further build the evidence based on stroke in the Ethiopian population through studying the types of stroke, the demographic characteristics, and the treatment outcomes among stroke patients treated in Mekelle University Ayder Referral Hospital.
2. Materials and methods
2.1. Study design
This retrospective medical record review study was conducted in Mekelle University Ayder Referral Hospital, a tertiary level hospital located in northern Ethiopia with an estimated catchment area of 5 million people. The study used convenience sampling, selecting all consecutive patients above the age of 18 years with a diagnosis of stroke or transient ischemic attack (TIA) during a two year period (March 2012–February 2014) [12]. The study period was bound by the date when the hospital acquired a computed tomography (CT) scan machine in March 2012. However, patients diagnosed without neuro-imaging were still included in the study because not all suspected stroke patients get CT Scans due to economic or other reasons.
2.2. Data collection
Stroke and TIA cases were identified through review of hand-written admission and discharge logbooks from the adult Intensive Care Unit and Medical Wards. Each medical record number with a recorded admission diagnosis of “stroke”, “hemiparesis”, or “transient ischemic attack” was submitted to the medical record room for chart retrieval.
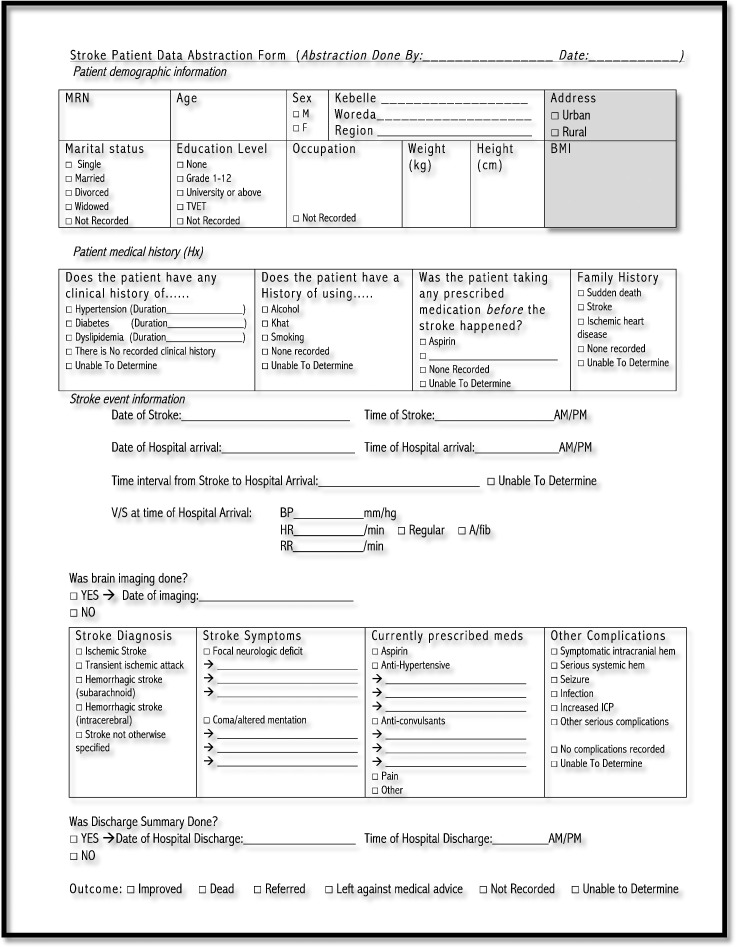
Data was abstracted from the patient's medical records by seven trained final year medical students blinded to the study hypothesis using a standardized, pre-developed paper data abstraction instrument in English, based on the study's data abstraction procedural guideline which clearly defined the inclusion and exclusion criteria, the variables' locations in the medical record, variable definitions, and treatment of missing data [13]. Each event was classified as being the patient's first-ever-in-a-lifetime clinically evident stroke or TIA, as confirmed through CT Scan findings or a neurological evaluation during hospitalization. The data abstraction tool was first piloted on 30 cases to check the consistency and understandability of the format. This was based on the assumption that we would find approximately 300 cases, using 10% for the pilot study [12]. Modifications were made to the abstraction format based on data quality checks. The final version of the data abstraction tool is included in Appendix A. Data abstractors were randomly checked for interrater reliability of their abstraction using weighted kappa statistics calculated on selected variables [12].
2.3. Data processing and analysis
All data were entered using EpiInfo Version 7 and analyzed using STATA 12. Statistics such as means, standard deviations, medians, and interquartile ranges were calculated to describe the typology of stroke, demographic characteristics, prevalence of risk factors, and treatment outcomes among stroke patients at Ayder Referral Hospital.
2.4. Ethics statement
This study did not involve human or animal subjects. All data was deidentified and assigned identification numbers during the process of data computerization. Ethical clearance was obtained from the Institutional Review Board of Mekelle University, College of Health Sciences. This study was approved by the Institutional Review Board of Mekelle University, College of Health Sciences.
3. Results
The hospital's Health Management Information System (HMIS) reported 291 stroke cases during the two year study period from March 2012 to February 2014 (Ayder Hospital HMIS Office). A total of 236 unique stroke cases were identified by reviewing the hospital's admission log books, with 160 admissions to the Adult ICU and 76 to the Medical Wards. From these, about one quarter (26.6%, N = 63) of the medical records were missing from the medical record room and 31 (13.1%) were not stroke patients upon review of the chart. Finally, 142 stroke patients treated in Ayder Referral Hospital during the two year study period were included in the study, or 49.1% of the 291 strokes originally reported by HMIS for the study period.
3.1. Demographic characteristics
The mean age of stroke patients was 62.8 ± 15.6 years, ranging from 19 to 93 years. Stroke in the young, defined by age less than 45 years, accounted for 12% of the total patients, while nearly half (45.1%) of the total patients were below 65 years of age. The majority of stroke patients were male (54.2%) and from urban areas (59.2%). Data was unavailable for several basic demographic characteristics of interest. For example, educational level (98.6%, N = 140) and occupation (87.3%, N = 124) were unrecorded for nearly all patients in the study. Table 1 shows the demographic characteristics of the stroke patients in the study by stroke subtype.
Table 1.
Demographic characteristics and risk factor profile by stroke subtype.
| All patients (n = 142) | Ischemic (n = 79) | Transient ischemic attack (n = 2) | Sub-arachnoid hemorrhage (n = 8) | Intra-cerebral hemorrhage (n = 46) | Other stroke (n = 7) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age group (years) | ||||||||||||
| < 25 | 3 | 2.1% | 2 | 2.5% | 0 | 0 | 1 | 2.2% | 0 | |||
| 25–44 | 14 | 9.9% | 5 | 6.3% | 1 | 50.0% | 1 | 12.5% | 6 | 13.0% | 1 | 14.3% |
| 45–64 | 47 | 33.1% | 24 | 30.4% | 0 | 4 | 50.0% | 17 | 37.0% | 2 | 28.6% | |
| 65–84 | 71 | 50.0% | 42 | 53.2% | 1 | 50.0% | 3 | 37.5% | 21 | 45.6% | 4 | 57.1% |
| > 85 | 7 | 4.9% | 6 | 7.6% | 0 | 0 | 1 | 2.2% | 0 | |||
| Sex | ||||||||||||
| Male | 77 | 54.2% | 44 | 55.7% | 1 | 50.0% | 4 | 50.0% | 16 | 34.8% | 0 | |
| Female | 65 | 45.8% | 35 | 44.3% | 1 | 50.0% | 4 | 50.0% | 30 | 65.2% | 7 | 100% |
| Address | ||||||||||||
| Urban | 84 | 59.2% | 46 | 58.2% | 2 | 100% | 8 | 100% | 23 | 50.0% | 5 | 71.4% |
| Rural | 58 | 40.8% | 33 | 41.8% | 0 | 0 | 23 | 50.0% | 2 | 28.6% | ||
| Clinical history | ||||||||||||
| Hypertension only | 49 | 34.5% | 16 | 20.3% | 1 | 50.0% | 6 | 75.0% | 20 | 43.5% | 6 | 85.7% |
| Diabetes only | 2 | 1.4% | 2 | 2.5% | 0 | 0 | 0 | 0 | ||||
| HTN & diabetes | 5 | 3.5% | 2 | 2.5% | 0 | 0 | 3 | 6.5% | 0 | |||
| Unable to determine | 86 | 60.6% | 59 | 74.7% | 1 | 50.0% | 2 | 25.0% | 23 | 50.0% | 1 | 14.3% |
3.2. Stroke subtypes
Ischemic stroke was the most frequent stroke subtype (55.6%, N = 79) followed by intracerebral hemorrhage (32.4%, N = 46), subarachnoid hemorrhage (5.6%, N = 8), other types of stroke (4.9%, N = 57), and transient ischemic attack (1.4%, N = 2).
3.3. Antecedent risk factors
Table 1 shows the frequency of identified antecedent risk factors by stroke subtype. History of hypertension was the most common antecedent risk factor identified in a total of 54 (38.0%) patients. History of diabetes was identified in a total of 7 (4.9%) patients. From these, 5 (3.5%) had a comorbid history of diabetes and hypertension. It is worth noting that the remaining 86 (60.6%) patients' medical records did not definitively confirm or deny the presence of hypertension or diabetes prior to the cerebrovascular accident occurrence. Among the patients with recorded history of hypertension and/or diabetes, the mean duration of hypertension prior to stroke was 4.4 years and 4.1 years for diabetes. Of the 54 patients with pre-existing hypertension, 20 (37.0%) had been prescribed anti-hypertensive medication prior to the stroke occurrence, but the level of medication adherence was unclear from the information in the medical records.
History of substance use was not definitively recorded for the majority of patients, though there were 7 (4.9%) reported alcohol users and one case each using cigarettes (0.7%) and khat (0.7%). In addition, data about lipid profile was not available in any of the medical records and only 2 (1.4%) patients had recorded data on BMI. None of the medical records contained information about family history of sudden death, stroke, or ischemic heart disease. Therefore, these variables were completely excluded from analysis.
3.4. Admission interval
The specific time (in HH:MM format) of stroke symptom onset (79.6%, N = 113) or hospital arrival (69.7%, N = 99) was not recorded in the majority of cases. Using only dates to calculate the interval from symptom onset to hospital arrival, the estimated median time for urban residents was 17.0 h (6.0–72.0 IQR) and for rural residents 60.0 h (23.0–144.0 IQR). Cumulatively, only 9.9% of patients were admitted to the hospital within the first 3 h of stroke symptom onset. 19.7% were admitted within 6 h, and 31.7% were admitted within 12 h. Nearly half (47.9%) of the patients were delayed more than 1 day for hospital admission, and 9.8% were delayed more than 7 days.
3.5. Clinical presentation
Table 2 shows various aspects of the patients' clinical presentation at the time of hospital arrival according to stroke subtype. Almost all (92.3%, N = 131) of the patients presented suffering from focal nuerological deficit while about one-third (31.7%, N = 45) presented with coma or altered mentation. From these, about one quarter (26.6%, N = 37) had both types of symptoms.
Table 2.
Clinical presentation at hospital arrival by stroke subtype.
| All patients (n = 142) | Ischemic (n = 79) | Transient ischemic attack (n = 2) | Sub-arachnoid hemorrhage (n = 8) | Intra-cerebral hemorrhage (n = 46) | Other stroke (n = 7) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Stroke symptoms | ||||||||||||
| Focal neurologic deficit | 94 | 67.6% | 56 | 70.9% | 1 | 50.0% | 6 | 75.0% | 26 | 56.5% | 5 | 71.4% |
| Coma or altered mentation | 8 | 5.8% | 1 | 1.3% | 0 | 0 | 7 | 15.2% | ||||
| Both FND and CAM | 37 | 26.6% | 21 | 26.6% | 1 | 50.0% | 1 | 12.5% | 12 | 26.1% | 2 | 28.6% |
| No symptoms recorded | 3 | 2.1% | 1 | 1.3% | 0 | 1 | 12.5% | 1 | 2.2% | |||
| Systolic BP at hospital arrival | ||||||||||||
| ≤ 89 mm Hg | 1 | 0.7% | 1 | 1.3% | 0 | 0 | 0 | 0 | ||||
| Normal range 90–120 mm Hg | 37 | 26.1% | 31 | 39.3% | 1 | 50.0% | 0 | 4 | 8.7% | 1 | 14.3% | |
| 121–139 mm Hg | 8 | 5.6% | 5 | 6.3% | 0 | 0 | 3 | 6.5% | 0 | |||
| ≥ 140 mm Hg | 94 | 66.2% | 40 | 50.6 | 1 | 50.0% | 8 | 100% | 39 | 84.8% | 6 | 85.7% |
| Unable to determine | 2 | 1.4% | 2 | 2.5% | 0 | 0 | 0 | 0 | ||||
| Heart rate at hospital arrival | ||||||||||||
| ≤ 59 bpm | 6 | 4.2% | 3 | 3.8% | 0 | 0 | 3 | 6.5% | 0 | |||
| Normal 60–100 bpm | 117 | 82.4% | 63 | 79.8% | 2 | 100% | 8 | 100% | 38 | 82.6% | 6 | 85.7% |
| 101–129 bpm | 16 | 11.3% | 11 | 13.9% | 0 | 0 | 4 | 8.7% | 1 | 14.3% | ||
| Unable to determine | 3 | 2.1% | 2 | 2.5% | 0 | 0 | 1 | 2.2% | 0 | |||
| Respiratory rate at hospital arrival | ||||||||||||
| Normal (12–20/min) | 54 | 38.0% | 32 | 40.5% | 1 | 50.0% | 2 | 25.0% | 17 | 37.0% | 2 | 28.6% |
| ≥ 21/min | 85 | 59.9% | 45 | 57.0% | 1 | 50.0% | 6 | 75.0% | 28 | 60.8% | 5 | 71.4% |
| Unable to determine | 3 | 2.1% | 2 | 2.5% | 0 | 0 | 1 | 2.2% | 0 | |||
| Cardiac rhythm at hospital arrival | ||||||||||||
| Regular | 41 | 28.9% | 22 | 27.9% | 0 | 5 | 62.5% | 10 | 21.7% | 4 | 57.1% | |
| Atrial fibrillation | 11 | 7.7% | 9 | 11.4% | 0 | 0 | 2 | 4.4% | 0 | |||
| Unable to determine | 90 | 63.4% | 48 | 60.7% | 2 | 100% | 3 | 37.5% | 34 | 73.9% | 3 | 42.9% |
The majority of patients' (66.2%, N = 94) systolic blood pressures (SBP) were highly elevated (140 mm Hg and above) upon hospital arrival. In particular 87% of intracerebral and subarachnoid hemorrhage stroke patients had SBP of 140 mm Hg or above. Most patients (82.4%, N = 117) presented with heart rate within normal range (60–100 bpm) upon hospital arrival. A majority (59.9%) of patients presented with elevated respiratory rate. Cardiac rhythm was not measured in the most (63.4%) cases, while 28.9% presented with regular cardiac rhythm, and 7.8% presented with atrial fibrillation.
3.6. In-hospital treatments and complications
Table 3 shows the medications prescribed for stroke and common in-hospital complications by stroke subtype. CT Scan was performed on 108 (76.1%) of the patients with a mean time from hospital admission to first neuroimaging of 1.6 (± 4.7) days. The most common drugs prescribed for ischemic stroke were Aspirin (93.7%), anti-hypertensives (45.6%), statins, (39.2%) and anti-coagulants (31.7%). Anti-hypertensives were prescribed for 83.3% of hemorrhagic stroke patients. About one quarter of the patients experienced in hospital complications of increased intracranial pressure (26.1%) or infection (21.1%) while intracranial hemorrhage and seizure were slightly less common (Table 3).
Table 3.
Treatments, complications, and prognosis by stroke subtype.
| All patients (n = 142) | Ischemic (n = 79) | Transient ischemic attack (n = 2) | Sub-arachnoid hemorrhage (n = 8) | Intra-cerebral hemorrhage (n = 46) | Other stroke (n = 7) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Medications prescribed for stroke | ||||||||||||
| Aspirin | 84 | 59.2% | 74 | 93.7% | 1 | 50.0% | 1 | 12.5% | 5 | 10.9% | 3 | 42.9% |
| Anti-HTN | 87 | 61.3% | 36 | 45.6% | 2 | 100% | 7 | 87.5% | 38 | 82.6% | 4 | 57.1% |
| Anti-coagulant | 37 | 26.1% | 25 | 31.7% | 1 | 50.0% | 1 | 12.5% | 8 | 17.4% | 2 | 28.6% |
| Anti-convulsant | 22 | 15.5% | 11 | 13.9% | 2 | 25% | 8 | 17.4% | 1 | 14.3% | ||
| Diuretic | 22 | 15.5% | 7 | 8.9% | 1 | 12.5% | 12 | 26.1% | 2 | 28.6% | ||
| Laxative | 8 | 5.6% | 5 | 6.3% | 3 | 6.5% | ||||||
| Statin | 36 | 25.4% | 31 | 39.2% | 1 | 12.5% | 3 | 6.5% | 1 | 14.3% | ||
| Anti-biotic | 32 | 22.5% | 11 | 13.9% | 3 | 37.5% | 15 | 32.6% | 3 | 42.9% | ||
| Pain | 23 | 16.2% | 8 | 10.1% | 2 | 25.0% | 11 | 23.9% | 2 | 28.6% | ||
| Complications | ||||||||||||
| Intracranial hemorrhage | 21 | 14.8% | 2 | 2.5% | 3 | 37.5% | 16 | 34.8% | ||||
| Seizure | 14 | 9.9% | 6 | 7.6% | 1 | 50.0% | 1 | 12.5% | 4 | 8.7% | 2 | 28.6% |
| Infection | 30 | 21.1% | 15 | 19.0% | 1 | 50.0% | 1 | 12.5% | 10 | 21.7% | 3 | 42.9% |
| Increased ICP | 27 | 26.1% | 16 | 20.3% | 1 | 12.5% | 16 | 34.8% | 4 | 57.1% | ||
| Other serious complications | 40 | 28.2% | 21 | 26.6% | 1 | 50.0% | 3 | 37.5% | 12 | 26.1% | 3 | 42.9% |
| Prognosis | ||||||||||||
| Inpatient mortality | 17 | 12.0% | 6 | 7.6% | 2 | 25.0% | 7 | 15.2% | 2 | 28.6% | ||
| Left against medical advice | 29 | 20.4% | 17 | 21.5% | 1 | 12.5% | 11 | 23.9% | ||||
| Improved | 68 | 47.9% | 40 | 50.6% | 2 | 100% | 5 | 62.5% | 20 | 43.5% | 1 | 14.3% |
| Referred | 6 | 4.2% | 4 | 5.1% | 2 | 28.6% | ||||||
| Unable to determine | 22 | 15.5% | 12 | 15.2% | 8 | 17.4% | 2 | 28.6% | ||||
3.7. Outcome
The in-hospital case fatality rate was 12.0% with 17 patient deaths. This was slightly lower than that reported by the hospital HMIS of 16.2% (47 deaths from 291 stroke cases). Among the 142 study patients, 68 (47.9%) improved, 29 (20.4%) left the hospital against medical advice, 6 (4.2%) were referred to other facilities, and outcome was unable to be determined for 22 (15.5%) of the patients. An official discharge summary was not found in the medical records of 56 (39.4%) patients. For the 97 (68.3%) patients with a recorded date of discharge or death, the median duration of hospital stay was 11 days (1–47 IQR), with the longest hospital stay of 96 days.
3.8. Data quality
Interrater reliability was calculated using the kappa statistic in order to measure the degree to which results obtained by one data abstractor differed from those obtained by a different abstractor when they both reviewed the same case. For treatment outcome (Weighted Kappa = 0.55) and stroke subtype diagnosis (Weighted Kappa = 0.42), interrater reliability was moderate and for demographic factors such as age (Kappa = 0.87) and sex (Kappa = 1.00) interrater agreement was nearly perfect [14], [15].
4. Discussion
This medical record review study aimed to describe types of stroke, frequency of risk factors, management patterns, and outcomes among stroke patients treated over a 2 year study period at a tertiary teaching hospital in northern Ethiopia.
Several other hospital-based studies conducted in Ethiopia [11], [16], Kenya [17], and Nigeria [18], [19] revealed a slight majority of male patients similar to our study. However, the average age of stroke patients in our study (62.8 years) was higher than in that reported in several other African hospital-based studies [9], [16], [17], [18], [19], although still lower than the typical age of stroke victims in the United States [20].
Our study found an ischemic to hemorrhagic stroke ratio of 1.72, including subarachnoid hemorrhage among the hemorrhagic strokes. Other hospital-based studies in Addis Abeba, Ethiopia found similarly low ischemic to hemorrhagic ratios of 1.58 [16], 0.63 [9], and 1.33 [11] while a study in Gondar, Ethiopia found 2.27 [21]. Furthermore, a hospital-based study in Kenya found an ischemic to hemorrhagic ratio of 1.06 and two hospital-based studies in Nigeria found ratios of 1.78 [18] and 1.62 [19]. This suggests that while ischemic stroke is still generally the most common form of stroke in sub-Saharan Africa, hemorrhagic stroke is relatively more dominant than in other parts of the world. For example, the American Heart Association estimates a ratio of 7.33 among the North American population [20] Dietary, environmental, and genetic factors probably play important roles in these differences, as well as a higher prevalence of untreated hypertension in sub-Saharan African populations. As the health and lifestyle of the Ethiopian population transitions, the pattern of CVD may also shift towards a pattern dominated by ischemic stroke.
Our study, similar to other studies, has shown that hypertension is the most common risk factor in stroke patients. However, the prevalence of hypertension (38.0%) found in our study was very low compared with other hospital-based studies in Ethiopia that found prevalences of hypertension ranging from 50.9%–69.3% [9], [10], [21], in Kenya 80% [17], and in Nigeria ranging from 73%–82.7% [18], [19]. This discrepancy is probably because we measured hypertension based on diagnoses that were clearly recorded in the medical record prior to the occurrence of stroke. When looking at the patients' vital signs that were measured at the time of hospital arrival, 66.2% (N = 94) had highly elevated SBP above 140 mm Hg. From these, however, only half (51.1%, N = 48) had any indication of previously diagnosed hypertension in their medical record. This leads us to believe that hypertension is highly underdiagnosed in our study population due to the lack of an active non-communicable disease screening program, failure to take routine blood pressure measurements, poor medical history taking, poor referral linkages between lower levels of healthcare and the referral hospital, and a general lack of awareness among health practitioners about hypertension, diabetes, high cholesterol and their complications.
We also observed that patients are extremely delayed in coming to the hospital and this was consistent with other studies on stroke in sub-Saharan Africa [9], [18]. It is recommended that stroke patients arrive at the hospital within 3 h of symptom onset in order to receive treatments such as tPA, to minimize long-term effects and even prevent death [20]. Although thrombolytic treatments are currently unavailable in our hospital, the delay of several days creates management difficulties and would make such advanced treatments impossible in the future.
It is also worth noting that Aspirin (11.1%), statins (7.4%), and anti-coagulants (16.7%) were prescribed in a small proportion of hemorrhagic stroke cases (Table 3). This abnormality is due to the fact that brain imaging is often delayed or not done at all if patients or their attendants are not convinced of the benefit of the CT Scan, or they are not willing or able to pay for it. In these cases, physicians sometimes give anticoagulants and anti-platelets if the patient is suspected of having ischemic stroke. When imaging becomes available either through negotiation or when the hospital is convinced to do it for free, these medications are immediately stopped if the patient is found to have intracranial bleeding contrary to the preliminary suspected diagnosis of ischemia. This highlights that despite the availability of the CT Scan, educational level and economic capacity remain as major barriers to utilization of this important diagnostic tool among stroke patients. Similar challenges were reported in Gondar, Ethiopia and Nigeria [18], [21].
The in-hospital case fatality rate of 12% observed in this study was similar to that found in Gondar, Ethiopia [21], but much lower than the 30-day case fatality rate of 30% reported in a systematic review of hospital-based prospective studies in sub-Saharan Africa [22]. The elevated case fatality due to intracerebral hemorrhage (15.2%) compared to ischemic stroke (7.6%) observed in our study is similar to other studies in sub-Saharan Africa [19], [22].
4.1. Limitations
The study has some limitations due to its nature as a retrospective medical record review study. The investigators had no control over the quality or completeness of the data since it was primary clinical data, not originally recorded for research purposes but for patient care. In general, the poor quality of medical recording we observed affected our ability to accurately report demographic characteristics, risk factors of interest, and even treatment outcomes. The challenge of missing data and even absence of entire charts could have introduced random error and non-response bias whereby subjects missing data systematically differ from those with complete data.
The convenience sampling approach restricts the generalizability of the findings and we may also may have observed survival bias or hospital admission bias where some victims died before reaching the hospital, and the patients who made it to the hospital may not be a representative sample. The extended delay in reaching care in combination with the high percentage of patients in our study discharged against medical advice may point to a much higher rate of out of hospital deaths. A study from Switzerland concluded that out-of-hospital deaths account for up to 50% of stroke deaths [23], and in sub-Saharan Africa there are many factors that probably increase the proportion of stroke patients who are not admitted to the hospital [22]. Therefore, a prospective hospital-based study or a large population-based study would be better suited to accurately describe stroke epidemiology in Ethiopia.
5. Conclusion and recommendations
The increasing burden of chronic disease in low-income countries like Ethiopia poses a challenge to the health system, which has until now been oriented to communicable disease characterized by acute episodes of illness. The level of undiagnosed and untreated hypertension accented by the insufficient medical history taking we observed in this study is alarming. As electronic medical recording is scaled up in Ethiopia, NCD risk factors must be strategically incorporated in the routinely collected data. In addition, the health system needs to be reoriented to encourage health education on NCDs for the general public, to promote identification of lifestyle related risk factors through proper history taking, to include regular screening for NCD risk factors at all levels of care, and to facilitate consistent and continuous follow up of chronic conditions.
Acknowledgments
We are very grateful to the seven data abstractors for the time and effort they exerted in conducting this study. The research was funded by a Mekelle University Contract Research and Publication Team Budget.
Contributor Information
Sennay A. Gebremariam, Email: sennay2003@yahoo.com.
Hannah S. Yang, Email: hszmyang@gmail.com.
Appendix A. Data abstraction tool
References
- 1.Misganaw A., Hailemariam D., Araya T. The double mortality burden among adults in Addis Ababa, Ethiopia, 2006–2009. Prev Chronic Dis. 2012;9:110–142. doi: 10.5888/pcd9.110142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization Ethiopia non-communicable diseases (NCD) country profile. 2014. http://www.afro.who.int/en/health-topics/topics/4358-noncommunicable-diseases.html Retrieved May 6, 2015, from.
- 3.Institute for Health Metrics and Evaluation Global burden of disease profile: Ethiopia. 2010. http://www.healthdata.org/sites/default/files/files/country_profiles/GBD/ihme_gbd_country_report_ethiopia.pdf Retrieved Oct 22, 2015, from.
- 4.Tesfaye F. Department of Public Health and Clinical Medicine, Umea University; Sweden: 2008. Epidemiology of Cardivascular Disease Risk Factors in Ethiopia: The urban–rural gradient. (PhD Dissertation) [Google Scholar]
- 5.Go A.S. American Heart Association Statistics Committee and Stroke Statistics Subcommittee; 2014. Heart Disease and Stroke Statistics — 2014 Update: A Report From the American Heart Association. (Circulation) [Google Scholar]
- 6.Bays H., Chapman R., Grandy S. The relationship of body mass index to diabetes mellitus, hypertension, and dyslipidaemia: comparison of data from two national surveys. Inst J Clin Pract. 2007;61(5):737–747. doi: 10.1111/j.1742-1241.2007.01336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mensah G. Epidemiology of stroke and high blood pressure in Africa. Heart. 2008;94:697–705. doi: 10.1136/hrt.2007.127753. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization Regional Office for Africa . World Health Organization; Luxembourg: 2014. The Health of the People — What Works: The Africa Regional Health Report 2014. (World Health Organization) [Google Scholar]
- 9.Alemayehu C., Birhanesilasie S. Assessment of stroke patients: occurrence of unusually high number of haemorrhagic stroke cases in Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. Clin Med Res. 2013;2(5):94–100. [Google Scholar]
- 10.Deresse B., Shaweno D. Epidemiology and in-hospital outcome of stroke in South Ethiopia. J Neurol Sci. 2015;335(1):138–142. doi: 10.1016/j.jns.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 11.Zenebe G., Alemayehu M., Asmera J. Characteristics and outcomes of stroke at Tikur Anbessa Teaching Hospital Ethiopia. Ethiop Med J. 2005;43(4):251–259. [PubMed] [Google Scholar]
- 12.Worster A., Haines T. Advanced statistics: understanding medical record review (MRR) studies. Acad Emerg Med. 2004;11:187–192. [PubMed] [Google Scholar]
- 13.Vassar M., Holzmann M. The retrospective chart review: important methodological considerations. J Educ Eval Health Prof. 2013;10(12) doi: 10.3352/jeehp.2013.10.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Viera A., Garrett J. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37(5):360–363. [PubMed] [Google Scholar]
- 15.Yawn B., Wollan P. Interrater reliability: completing the methods description in medical records review studies. Am J Epidemiol. 2005;161(10):974–977. doi: 10.1093/aje/kwi122. [DOI] [PubMed] [Google Scholar]
- 16.Asefa G., Meseret S. CT and clinical correlation of stroke diagnosis, patternm and clinical outcome among stroke patients visiting Tikur Anbessa Hospital. Ethiop Med J. 2010;48(2):117–122. [PubMed] [Google Scholar]
- 17.Jowi J., Mativo P. Pathological sub-types, risk factors and outcome of stroke at the Nairobi Hospital, Kenya. East Afr Med J. 2008;85(12) doi: 10.4314/eamj.v85i12.43535. [DOI] [PubMed] [Google Scholar]
- 18.Adeyoyin K.M., Oluwole K.E., Femi F. Profile of stroke in Nigerians: a prospective clinical study. Afr J Neurol Sci. 2007;26(1) [Google Scholar]
- 19.Alkali N.H., Bwala S.A., Akano A.O. Stroke risk factors, subtypes, and 30-day case fatality in Abuja, Nigeria. Niger Med J. 2013;54(2):129–135. doi: 10.4103/0300-1652.110051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.American Heart Association About stroke. 2015. http://www.strokeassociation.org/STROKEORG/AboutStroke/About-Stroke_UCM_308529_SubHomePage.jsp Retrieved Sept 1, 2015, from American Stroke Association.
- 21.Greffie E., Mitiku T., Getahun S. Risk factors, clinical pattern and outcome of stroke in a referral hospital, Northwest Ethiopia. Clin Med Res. 2015;4(6):182–188. [Google Scholar]
- 22.Connor M.D., Walker R., Modl G. Burden of stroke in black populations in sub-Saharan Africa. Lancet Neurol. 2007;6:269–278. doi: 10.1016/S1474-4422(07)70002-9. [DOI] [PubMed] [Google Scholar]
- 23.Meyer K., Simmet A., Arnold M. Stroke events and case fatalities in Switzerland based on hospital statistics and cause of death statistics. Swiss Med Wkly. 2009;139(5–6):65–69. doi: 10.4414/smw.2009.12448. [DOI] [PubMed] [Google Scholar]