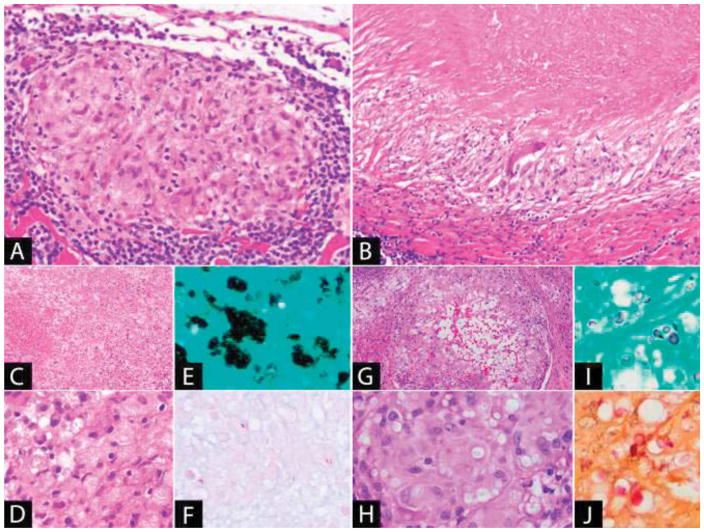
Figure 4. Granulomatous Inflammation.
(A) Non-necrotizing granuloma: The granuloma is well-demarcated and composed of epithelioid histiocytes with a peripheral lymphoid cuff. (B) Necrotizing granuloma: There is a large area of necrosis surrounded by a peripheral rim of epithelioid histiocytes. A giant cell is also present. (C–E) Disseminated histoplasmosis: (C) The lymph node is effaced by sheets of macrophages with extensive necrosis. (D) The yeast is present in clusters within the cytoplasm of the macrophages and is positive with (E) GMS stain. (F) Acid-fast bacilli (Fite): Mycobacteria, a cause of necrotizing granulomatous lymphadenitis, may be few in number and difficult to identify. (G–J): Cryptococcal lymphadenitis: (G) Granulomatous inflammation with central cystic spaces. (H) The yeast is visible within the cytoplasm of the histiocytes as faintly staining structures within clear spaces. It is positive with (I) GMS and (J) mucicarmine stains.