Abstract
Background
Fall rates among adults with multiple sclerosis are consistently greater than 50%, but near-falls (i.e. a trip or stumble) are often undocumented. Furthermore, little is known about the circumstances surrounding fall and near-fall events. The purpose of this study was to examine the similarities and differences among non-fallers, near-fallers and fallers with multiple sclerosis, including the circumstances that surround falls and near-falls.
Methods
In a single visit, 135 multiple sclerosis participants completed the Hopkins Falls Grading Scale, a custom questionnaire investigating circumstances surrounding falls and near-falls, and performed the Timed Up and Go and Timed 25-Foot Walk tests. Mann-Whitney tests were used to examine differences between fallers, near-fallers and non-fallers. Multiple logistic regression with AIC criterion was used to examine associations of circumstances with the odds of falling vs. near-falling. Cumulative odds ordinal logistic regression was used to analyze the association between each of the walking tests and the susceptibility of the individual for falls or near-falls.
Results
30% of individuals reported falls, while 44% reported near-falls over a 1-year period. Non-fallers completed the walking tests more quickly than near-fallers (p<0.0045), and fallers (p<0.0001); near-fallers and fallers demonstrated similar motor profiles. Individuals were more likely to sustain a fall rather than a near-fall under the following circumstances: transferring outside the home (p=0.015) and tripping over an obstacle (p=0.025). Performing 1-second slower on the walking tests increased the odds of a history of a fall by 6–20%.
Conclusion
Near-falls occur commonly in individuals with MS; near-fallers and fallers reported similar circumstances surrounding fall events and demonstrated similar performance on standard timed walking tests. Clinicians monitoring individuals with MS should consider evaluation of the circumstances surrounding falls in combination with quantitative walking measures to improve determination of fall risk and appropriate rehabilitation interventions.
Keywords: Multiple Sclerosis, Accidental Falls, Falls, Near-Falls, Walking
1. Introduction
The prevalence of falls among adults with multiple sclerosis (MS) is consistently >50% [1], resulting in more injuries than age-matched controls [2–3]. Many factors have been linked with increased odds of falling including longer disease duration [4], progressive disease [4–6], use of assistive devices [4–8], greater overall disability as measured by the Expanded Disability Status Score (EDSS) [4,9], poorer cognition [1, 5–6, 10], bladder dysfunction [1], slower walking speed or poorer gait performance and endurance [4], and worse performance on balance tests [4–5, 9–10]. Despite the identification of factors related to falls, less is known about the circumstances surrounding fall events and their relationship to measures of walking.
Anecdotally, individuals with MS often report particular circumstances when describing fall-events, such as transfers, stair-climbing, tripping or obstacle avoidance during walking. Knowledge of the circumstances surrounding fall events may direct rehabilitation efforts and improve fall prevention. Information on the circumstances surrounding fall events are growing. One study shows that over a 3-month period, 28% of falls occurred during mobility activities of walking, turning or transferring and 11% of falls resulted in injuries requiring medical attention [11]. Additionally, 72% of falls occurred during the day and 62% occurred indoors [11]. More than half of the individuals in this sample had an EDSS >5.5 [11]; making it challenging to generalize these results to individuals with lower disability levels. Others have shown that >45% of falls occurred because of a slip or trip, >45% of falls occurred when the individual was tired or fatigued, approximately 30% of falls were due to the individual not paying attention and 20–25% of falls occurred when the individual was rushing or not using a needed walking aid [6]. A recent prospective meta-analysis of individuals with MS in four countries with EDSS levels ranging from 0–6.5 reported that 65% of falls occurred indoors while 75% occurred during between 6am and 6pm [12]. Although they noted associations between falls and EDSS score, no other measures of walking were included in this study.
As opposed to a fall, in which the individual comes to rest on a lower surface, a near-fall occurs when the individual has a trip or stumble, but is able to recover balance. Very few studies examine near-fallers and the circumstances surrounding near-falls are unknown. There are established relationships among reported numbers of near-falls and falls [13] and among near-falls and the Timed 25 Foot Walk (T25FW) score in ambulatory individuals with MS [14]. Although balance, gait and other motor measures may distinguish between MS fallers and non-fallers [15–17], the usefulness of these measures is unclear in individuals with near-falls. Validation of accurate, clinically accessible assessment tools for distinguishing fallers and near-fallers from non-fallers are an important step toward minimizing fall risk and directing individuals into appropriate rehabilitation programs. Individuals who experience near-falls may represent an important target group that has yet to experience a catastrophic fall and could benefit from fall avoidance interventions [11]. One way to improve fall risk may be to link measures that are commonly used in the clinic with circumstances known to surround fall events.
Therefore, our objectives were to utilize survey information to a) identify the circumstances surrounding fall or near-fall events; b) identify the prevalence of near-falls in our clinic; and c) examine clinical walking performance in self-identified non-fallers, near-fallers and fallers. We hypothesized that fallers and near-fallers would report similar circumstances leading to falls, which may be amenable to education and rehabilitation; near-fallers would be prevalent in our clinical population, thus identifying an underserved population that should be addressed clinically to prevent injurious falls; and clinical walking performance would distinguish fallers from non-fallers and near-fallers.
2. Patients and Methods
A convenience sample of participants diagnosed with MS by the 2010 McDonald Criteria [18] were included in this observational, cross-sectional quality improvement study. This study was reviewed by the Johns Hopkins Medicine Institutional Review Board and was determined to be a quality improvement project for which informed consent was not required. All data were collected from current patients at the Johns Hopkins Medical Institute MS Center between December 19, 2012 and May 1, 2013. All participants who were ambulatory with or without an assistive device, lacked orthopedic or other neurologic disorders that would interfere with their walking or their ability to understand survey questions, and able to follow study-related commands were included in this quality improvement study. In a single session, participants completed clinical testing and questionnaires.
2.1 Fall Questionnaires
The Hopkins Falls Grading Scale divides falls into grades 1–4 by the severity of the fall event, and has established face validity, content validity and excellent interrater reliability [19]. Grade 1 indicates near-falls, Grade 2 indicates a fall without injury, Grade 3 indicates a fall requiring medical attention, and Grade 4 indicates a fall requiring a hospital admission (Appendix A). An individual was considered a non-faller if they had no falls or near-falls in the past year, a near-faller if they had no falls in the past year but at least one near-fall (Grade 1), and a faller if they had at least one fall (Grade 2–4) within the last year.
A custom survey (Appendix A) that aimed to identify the number and circumstances surrounding fall events was created by two of the study authors based on clinical expertise and administered to all participants. The survey was completed in a single visit without longitudinal monitoring.
2.2 Clinical Testing
Two standard clinical tests of walking, the T25FW and Timed Up and Go (TUG) were chosen because they are considered gold standards for mobility function in clinical trials of MS [20, 21].
The T25FW [22] requires individuals to ambulate at their quickest, safe speed over 25 feet for two trials. The T25FW has excellent intra (ICC=0.99) and interrater (ICC=1.0) reliability [23]. Although no cut-off scores have been established, a recent meta-analysis suggested that MS fallers perform worse than non-fallers on the T25FW [4].
The TUG requires individuals to stand from a chair, walk 10 feet, turn, walk back, and return to a seated position in the chair. The TUG is reliable and valid in persons with MS [24]; while there is marginal evidence to suggest that TUG scores differ between MS fallers and non-fallers [4], cut-off scores have been reported only for the TUG-cognitive version of this test [24].
2.3 Statistical Analysis
All statistical analyses were performed in R (version 3.0.2; The R Foundation for Statistical Computing). Subjects were subdivided utilizing The Hopkins Fall Grading Scale to separate non-fallers from near-fallers (Grade 1) and fallers (Grades 2–4).
To examine associations of circumstances with the odds of falling vs. near-falling, we considered only individuals reporting at least one fall or near-fall in the past year, as non-fallers could not provide this information. We examined the circumstances surrounding fall-events with descriptive statistics and then a multiple logistic regression was used to model the association of log-odds of falling with the covariates in the model and the circumstances. Due to the large number of predictors in the model, we first used a variable selection procedure, forward selection using the Akaike Information Criterion (AIC) criterion [25] to identify a subset of predictors used in the final model. AIC assesses the goodness-of-fit of nested models with different numbers of predictors.
To analyze the association between each of the walking tests and the susceptibility of the individual for falls, we modeled fall status as a function of the specific walking test while controlling for the effects of age and MS type using a cumulative odds ordinal logistic regression [26]. In this model, the outcome can have more than two categories that can be ordered in terms of severity (i.e., falls are worse than near-falls and near-falls are worse than non-falls). Finally, we utilized Mann-Whitney tests to examine differences among fallers and near-fallers on questions 6–11 from our custom survey.
3. Results
3.1 Participants
One hundred and thirty-five individuals participated in this study; 112 with relapsing-remitting MS and 23 with progressive MS. Our cohort had a mean ± SD age: 45.7 ± 13.3 years; EDSS level was <6.5 for all participants. Participants were sub-grouped by fall status and baseline characteristics (table 1).
Table 1.
Participant Demographics
| N | Age | Disease Type | Assistive Device Use | Near-Falls per Year | Falls per Year | ||
|---|---|---|---|---|---|---|---|
| Non-Fallers | 69 | 42.1 (12.9) | 62 R; 7 P | Not collected | 0 | 0 | |
| Near-Fallers 1 | Grade | 25 | 49.9 (13.1) | 20 R; 5 P | 6/19 | 4.2 (3.7) | 0 |
| Fallers 2 | Grade | 32 | 48.9 (12.8) | 22 R; 10 P | 13/30 | 39.0 (82.7) | 9.5 (22.2) |
| Grade 3–4 | 9 | 49.8 (13.2) | 8 R; 1 P | 2/8 | 89.8 (157.2) | 5.4 (4.0) |
All values listed mean(SD); Relapsing (R); Progressive (P); grades determined by the Hopkins Falls Grading Scale [19]; Grade 1 indicates near-falls, Grade 2 indicates a fall without injury, Grade 3 indicates a fall requiring medical attention, and Grade 4 indicates a fall requiring a hospital admission; Nine individuals had missing data for assistive device use. If individuals recorded no falls, the survey stopped at this point and did not report assistive device data.
3.2 Frequency of Falls and Near-Falls
30.4% of individuals in our cohort reported falls in the past year, while 43.7% of individuals reported one or more near-falls in the past year. As expected, fallers also commonly experienced near-falls; with 82.9% of fallers also reporting near-falls (table 1). To be included in the near-falls group 1, individuals could only have experienced near-falls, but to be in the faller groups 2–4, individuals could have experienced both falls and near-falls.
3.3 Demographics and Fall Status
To assess the role of demographics on fall category, individuals were divided into three categories: non-fallers, near-fallers, and fallers. The results of ordinal regression indicate that the probability of reporting a fall increases significantly with age (p=0.04), but type of MS did not significantly affect the probability of being a faller or a non-faller. It is notable that only 11% of non-fallers had progressive MS compared to 25% of near-fallers and 37% of fallers in this cohort.
3.4 Circumstances Surrounding Falls
Subjects reporting falls or near-falls were prompted to describe the circumstances surrounding fall events with a series of qualifiers. These included such situations as stair climbing, transferring inside and outside the home, negotiating obstacles, and walking on slippery surfaces, as well as various other factors such as poor vision, incontinence, and alcohol intake (see Appendix A).
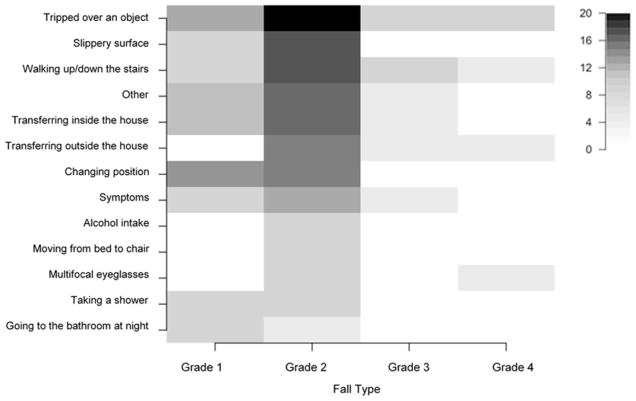
The circumstances were assessed individually against the fall categories; after adjustment for age and disease type, five tasks were associated with the odds of reporting a fall as opposed to the odds of a reporting a near-fall: changing position, climbing stairs, tripping over an obstacle, transferring outside the home, and alcohol consumption. In the final model, the odds of a fall compared to a near-fall were 31 times more likely for transferring outside the home (p=0.015), 5 times more likely for tripping over an obstacle (p=0.025) and 0.2 times more likely for changing position (p=0.046). An exploratory analysis was used to describe the rates of different circumstances that result in the different grades of falls (figure 1).
Figure 1.
Frequency of circumstances associated with grades of fallers; n=25 Grade 1; n=32 Grade 2; n=5 Grade 3; n=4 Grade 4.
3.5 Differences among Near-Fallers and Fallers
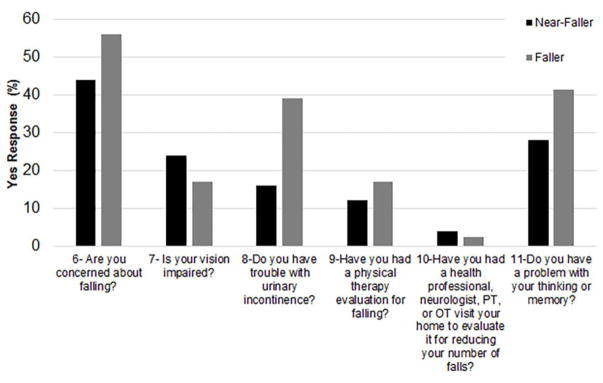
To further understand differences among near-fallers and fallers, we examined the responses to questions 6–11 on our custom survey (Appendix A). Fifty-six percent of fallers and 44% of near-fallers reported that they were concerned about falling, yet only 17% of fallers and 12% of near-fallers had experienced a rehabilitation evaluation for fall-related issues, and only 2% of fallers and 4% of near-fallers reported having a home safety evaluation to reduce the number of falls in the home (figure 2). On questions related to impairments, 39% of fallers and 16% of near-fallers reported having trouble with urinary incontinence, while 41% of fallers and 28% of near-fallers reported problems with thinking or memory, and 17% of fallers and 24% of near-fallers reported vision impairments. Despite these subtle differences, near-fallers and fallers were not significantly different in their responses to questions 6–11 (p<0.07 for all). On walking tests, non-fallers completed the TUG and T25FW more quickly than near-fallers (p=0.0018 and p=0.0045, respectively), and fallers (p<0.0001 and p<0.0001, respectively); near-fallers walked more quickly than fallers, but this difference was not significant (p=0.26 and p=0.16, respectively) (table 2).
Figure 2.
Comparison of self-reported impairment measures (Questions 6–11 on Appendix A) in individuals reporting falls and near-falls. Values on the y-axis represent the percent endorsing a “Yes” response to each question. Occupational Therapy (OT); Physical Therapy (PT).
Table 2.
Non-fallers walk significantly faster than near-fallers and fallers, but there is no significant difference in walking performance among near-fallers and fallers.
| N | TUG(s) | T25FW(s) | |
|---|---|---|---|
| Non-Fallers | 69 | 6.4 (3.5) | 4.5 (1.6) |
| Near-Fallers | 25 | 10.5 (10.4)** | 8.3 (12.9)* |
| Fallers | 41 | 11.5 (10.0)*** | 7.2 (4.9)*** |
All values listed mean(SD);
significantly different from non-fallers, p<0.0001;
significantly different from non-fallers, p=0.0018;
significantly different from non-fallers, p=0.0045.
Timed Up and Go (TUG); Timed 25 Foot Walk (T25FW).
3.6 Association of Walking Tests to Fall Status
Timed Up and Go
A one-second increase in TUG increased odds of reporting a fall by 6% (p=0.057). Not surprisingly, a one-year increase in age results in marginally increased odds of experiencing a worse (i.e., higher grade) fall by 2% (p=0.085). For any given person in this cohort, controlling for age, MS type and TUG speed, the likelihood of near-falls was 5.75 times higher than the individual having had no falls at all (p=0.019), while the likelihood of falls was 14.19 times higher than the likelihood of having had near-falls (p=0.001).
Timed 25 Foot Walk
In a second analysis, the T25FW measure was used as a predictor of the cumulative odds of having worse (i.e., higher grade) falls while controlling for age and disease type. A one-second increase in T25FW time results in increased odds of reporting a fall by 20% (p=0.017). Similar to the TUG results, a one-year increase in age results in a 2% increase in the odds of worse (i.e., higher grade) falls (p=0.084). For any given person in this cohort, controlling for age, MS type and T25FW speed, the likelihood of reporting near-falls is 9.48 times higher than the individual having had no falls at all (p=0.004), while the likelihood of reporting falls is 22.77 times higher than the likelihood of having had near-falls (p<0.001).
4. Discussion
Near-falls were highly prevalent, with over 40% of the cohort experiencing near-falls. Both fallers and near-fallers experienced similar circumstances surrounding their fall events (figure 2); these tasks may be modifiable with education and rehabilitation. Our results showed that specific circumstances were associated with increased odds of reporting falls compared to near-falls; strikingly, the odds of falling were up to 31 times that of a near-fall for transferring outside the home.
Fallers and near-fallers performed similarly on TUG and T25FW tests (table 2). Poorer performance on both the TUG and T25FW result in increased odds of reporting near-falls and falls, after controlling for age and disease type. A one-second increase in TUG performance was associated with 6% greater odds of experiencing a worse (i.e., higher grade) fall. Similarly, a one-second increase in T25FW performance was associated with 20% greater odds of experiencing a fall. Our results demonstrate that the TUG and T25FW provide important information that can be used to understand a person’s odds of falling.
Identification of differences among fallers and near-fallers is critical for implementing fall-prevention techniques. However, accuracy for determining near-fallers was quite low due to a large overlap in walking performance with fallers. This is significant, given that the individuals with near-falls have yet to experience an injurious fall. While more complex machine learning algorithms may be utilized to classify participants into three groups, these algorithms are difficult to apply clinically. Therefore, in order to appropriately differentiate among fallers and near-fallers, additional clinical tests may be required. In considering what tools may be most helpful for differentiation, other studies have discussed the importance of muscle tone, proprioception, and continence in relation to MS falls [1, 4–6, 27]. Our data shows that both fallers and near-fallers report issues with incontinence as well as difficulty with memory and thinking (figure 2). Additionally, our previous work shows relationships of walk velocity to quantitative strength and dynamic balance, with greater ability to move toward the limits of stability and greater hip strength associated with faster walking velocity [28–29]. Further examination of balance, strength, incontinence and cognition may improve our ability to differentiate among fallers and near-fallers [30], and participation measures that have been validated for use in MS such as the Community Participation Indicators or the Community Integration Measure, are relevant and meaningful to the lives of individuals with MS and should also be considered [8].
Fall prevention is a significant public health issue. Our data shows that rehabilitation services are underutilized in this cohort, with <20% reporting evaluations for fall-related issues and <5% reporting home safety evaluations (figure 2). With fall rates in individuals with MS >50% annually [1] and injury and fracture rates 2–3 times higher in individuals with MS compared to age-matched controls [2–3], it is clear that improving fall prediction in MS is critically important for early intervention to decrease the risk of injurious and costly falls.
This survey study is limited by accounting for only retrospective falls. In older adults, 12-month fall recall has been shown to be an underestimate, particularly in those who experience 3 or more falls [31]; thus it is possible that some participants misestimated the number of falls or near-falls experienced. Thirty percent of our cohort reported at least one fall in the past year; while this number is lower in comparison to recent prospective falls-reporting studies [10–11, 32], it is in agreement with other retrospective studies [33]. This study has presented near-fallers as individuals at risk for a future fall; however, it is possible that near-fallers may actually be demonstrating good fall-avoidance strategies, and this should be explored in future work. Additionally, previous studies have found progressive disease to be linked with higher risk of falls in individuals with MS. MS type was not related to fall category, but this is likely due to the smaller cohort of progressive subtype in this group of subjects. Finally, with survey data, we were unable to assess additional factors related to falls such as cognition, strength, sensory effects, and community participation. Furthermore, symptom duration, gender, and medications, including those modulating blood pressure, were not included in this survey. Measurement of these factors may improve future studies examining fall risk. EDSS was not specifically measured for individual patients as part of this quality improvement study, but all individuals were ambulatory with an EDSS less than or equal to 6.5. While disease severity may impact fall risk, our data shows that rates of assistive device use between fallers and near-fallers are relatively similar (Table 1; near-fallers: 31.6%; fallers: 39.5%).
5. Conclusions
Near-falls occur commonly in individuals with MS; near-fallers and fallers reported similar circumstances surrounding fall events and demonstrated similar performance on standard timed walking tests. The outcome of this quality improvement project was the implementation of improved documentation of near-fall events, routine administration of the T25FW and TUG tests, and referral to rehabilitation services when near-falls were reported within the Johns Hopkins Medical Institute MS Center. Clinicians monitoring individuals with MS should consider documentation of near-falls and evaluation of the circumstances surrounding falls in combination with quantitative walking measures to improve determination of fall risk and appropriate rehabilitation interventions. Future studies should examine additional factors that may improve fall prediction, and consider the importance of near-falls for predicting future safety and preventing injurious falls.
Supplementary Material
Highlights.
Near-falls are prevalent in individuals with Multiple Sclerosis
Near-fallers and Fallers report similar circumstances surrounding falls
The circumstances described (transfers, obstacles) are amenable to rehabilitation
Near-fallers and Fallers walk slower than Non-Fallers
Screening for Near-Falls and Falls may improve referrals to rehabilitation
Acknowledgments
The authors gratefully acknowledge Santiago Pardo for assistance with data management and we appreciate the effort of all of our participants. This work was supported by NIH NICHD K01 HD049476-04 (KMZ) and by a National Multiple Sclerosis Society Tissue Repair Grant (KMZ and PAC).
Role of Funding Source:
This work was supported by NIH NICHD K01 HD049476-04 (KMZ) and by a National Multiple Sclerosis Society Tissue Repair Grant (KMZ and PAC). The funding sources had no involvement in study design, collection, analysis and interpretation of data, the writing of the report, or in the decision to submit this article for publication.
Glossary
- EDSS
Expanded Disability Status Score
- MS
Multiple Sclerosis
- T25FW
Timed 25 Foot Walk
- TUG
Timed Up and Go
- AIC
Akaike Information Criterion
Footnotes
Declaration of Interest Statement
Dr. Fritz reports no disclosures.
Dr. Eloyan reports no disclosures.
Ms. Baynes reports no disclosures.
Dr. Newsome reports grants and personal fees from Biogen and Novartis as well as personal fees from Genzyme that are outside the submitted work.
Dr. Calabresi reports grants from Biogen-IDEC, Novartis, and MedImmune, grants and personal fees from Abbvie, personal fees from Vertex, Vaccinex, Merck, and Prothena that are outside the submitted work.
Dr. Zackowski reports grants from National MS Society, Sun Pharmaceuticals, and Acorda Therapeutics that are outside the submitted work.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Finlayson ML, Peterson EW, Cho CC. Risk factors for falling among people aged 45 to 90 years with multiple sclerosis. Arch Phys Med Rehabil. 2006;87:1274–1279. doi: 10.1016/j.apmr.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 2.Cameron MH, Poel AJ, Haselkorn JK, Linke A, Bourdette D. Falls requiring medical attention among veterans with multiple sclerosis: a cohort study. J Rehabil Res Dev. 2011;48:13–20. doi: 10.1682/JRRD.2009.12.0192. [DOI] [PubMed] [Google Scholar]
- 3.Peterson EW, Cho CC, von Koch L, Finlayson ML. Injurious falls among middle aged and older adults with multiple sclerosis. Arch Phys Med Rehabil. 2008;89:1031–1037. doi: 10.1016/j.apmr.2007.10.043. [DOI] [PubMed] [Google Scholar]
- 4.Gianni C, Prosperini L, Jonsdottir J, Cattaneo D. A systematic review of factors associated with accidental falls in people with multiple sclerosis: a meta-analytic approach. Clin Rehabil. 2014;28:704–716. doi: 10.1177/0269215513517575. [DOI] [PubMed] [Google Scholar]
- 5.Gunn HJ, Newell P, Haas B, Marsden JF, Freeman JA. Identification of risk factors for falls in multiple sclerosis: a systematic review and meta-analysis. Phys Ther. 2013;93:504–513. doi: 10.2522/ptj.20120231. [DOI] [PubMed] [Google Scholar]
- 6.Matsuda PN, Shumway-Cook A, Bamer AM, Johnson SL, Amtmann D, Kraft GH. Falls in multiple sclerosis. PM & R. 2011;3:624–632. doi: 10.1016/j.pmrj.2011.04.015. [DOI] [PubMed] [Google Scholar]
- 7.Coote S, Finlayson M, Sosnoff JJ. Level of mobility limitations and falls status in persons with multiple sclerosis. Arch Phys Med Rehabil. 2014;95:862–866. doi: 10.1016/j.apmr.2013.10.018. [DOI] [PubMed] [Google Scholar]
- 8.Finlayson ML, Peterson EW, Asano M. A cross-sectional study examining multiple mobility device use and fall status among middle-aged and older adults with multiple sclerosis. Disabil Rehabil Assist Technol. 2014;9:12–16. doi: 10.3109/17483107.2013.782578. [DOI] [PubMed] [Google Scholar]
- 9.Kasser SL, Jacobs JJ, Foley JT, Cardinal BJ, Maddalozzo GF. A prospective evaluation of balance, gait, and strength to predict falling in women with multiple sclerosis. Arch Phys Med Rehabil. 2011;92:1840–1846. doi: 10.1016/j.apmr.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 10.Hoang PD, Cameron MH, Gandevia SC, Lord SR. Neuropsycholoical, balance, and mobility risk factors for people with multiple sclerosis: a prospective cohort study. Arch Phys Med Rehabil. 2014;95:480–486. doi: 10.1016/j.apmr.2013.09.017. [DOI] [PubMed] [Google Scholar]
- 11.Gunn H, Creanor S, Haas B, Marsden J, Freeman J. Frequency, characteristics and consequences of falls in multiple sclerosis: findings from a cohort study. Arch Phys Med Rehabil. 2014;95:538–545. doi: 10.1016/j.apmr.2013.08.244. [DOI] [PubMed] [Google Scholar]
- 12.Nilsagard Y, Gunn H, Hoang P, Lord S, Mazumder R, Cameron M. Falls in persons with MS-an individual data meta-analysis from studies from Australia, Sweden, United Kingdom and the United States. Mult Scler. 2015;21:92–100. doi: 10.1177/1352458514538884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nilsagard Y, Lundholm C, Denison E, Gunnarsson LG. Predicting accidental falls in people with multiple sclerosis-a longitudinal study. Clin Rehabil. 2009;23:259–269. doi: 10.1177/0269215508095087. [DOI] [PubMed] [Google Scholar]
- 14.Argento O, Incerti CC, Pisani V, et al. Domestic accidents and multiple sclerosis: an exploratory study of occurrence and possible causes. Disabil Rehabil. 2014;36:2205–2209. doi: 10.3109/09638288.2014.895429. [DOI] [PubMed] [Google Scholar]
- 15.Dibble LE, Lopez-Lennon C, Lake W, Hoffmeister C, Gappmaier E. Utility of disease-specific measures and clinical balance tests in prediction of falls in persons with multiple sclerosis. J Neurol Phys Ther. 2013;37:99–104. doi: 10.1097/NPT.0b013e3182a18460. [DOI] [PubMed] [Google Scholar]
- 16.Prosperini L, Fortuna D, Gianni C, Leonardi L, Pozzilli C. The diagnostic accuracy of static posturography in predicting accidental falls in people with multiple sclerosis. Neurorehab Neural Re. 2013;27:45–52. doi: 10.1177/1545968312445638. [DOI] [PubMed] [Google Scholar]
- 17.Cameron MH, Thielman E, Mazumder R, Bourdette D. Predicting falls in people with multiple sclerosis: fall history is as accurate as more complex measures. Mult Scler Int. 2013:496325. doi: 10.1155/2013/496325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Polman CH, Reingold SC, Banwell B, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011;69:292–302. doi: 10.1002/ana.22366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davalos-Bichara M, Lin FR, Carey JP, et al. Development and validation of a falls-grading scale. J Geriatr Phys Ther. 2013;36:63–67. doi: 10.1519/JPT.0b013e31825f6777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kapoor R, Furby J, Hayton, et al. Lamotrigine for neuroprotection in secondary progressive multiple sclerosis: a randomised, double-blind, placebo-controlled, parallel-group trial. Lancet Neuruol. 2010;9:681–688. doi: 10.1016/S1474-4422(10)70131-9. [DOI] [PubMed] [Google Scholar]
- 21.Hupperts R, Lycke J, Short C, et al. Prolonged-release fampridine and walking and balance in MS: randomised controlled MOBILE trial. Mult Scler. 2016;22:212–221. doi: 10.1177/1352458515581436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Polman CH, Rudick RA. The multiple sclerosis functional composite: a clinically meaningful measure of disability. Neurology. 2010;74:S3, S8–S15. doi: 10.1212/WNL.0b013e3181dbb571. [DOI] [PubMed] [Google Scholar]
- 23.Rosti-Otajärvi E, Hämäläinen P, Koivisto K, Hokkanen L. The reliability of the MSFC and its components. Acta Neurol Scand. 2008;117:421–427. doi: 10.1111/j.1600-0404.2007.00972.x. [DOI] [PubMed] [Google Scholar]
- 24.Nilsagard Y, Lundholm C, Gunnarsson LG, Denison E. Clinical relevance using timed walk tests and ‘timed up and go’ testing in persons with multiple sclerosis. Physiother Res Int. 2007;12:105–114. doi: 10.1002/pri. [DOI] [PubMed] [Google Scholar]
- 25.Akaike H. A new look at the statistical model identification. IEEE T Automat Contr. 1974;19:716–723. doi: 10.1109/TAC.1974.1100705. [DOI] [Google Scholar]
- 26.Agresti A. Categorical Data Analysis. Hoboken, NJ: John Wiley & Sons; 2012. [Google Scholar]
- 27.Coote S, Hogan N, Franklin S. Falls in people with multiple sclerosis who use a walking aid: prevalence, factors, and effect of strength and balance interventions. Arch Phys Med Rehabil. 2013;94:616–621. doi: 10.1016/j.apmr.2012.10.020. [DOI] [PubMed] [Google Scholar]
- 28.Fritz NE, Marasigan RE, Calabresi PA, Newsome SD, Zackowski KM. The impact of dynamic balance measures on walking performance in multiple sclerosis. Neurorehabil Neural Re. 2015;29:62–69. doi: 10.1177/1545968314532835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fritz NE, Newsome SD, Eloyan A, Marasigan RE, Calabresi PA, Zackowski KM. Longitudinal relationships among posturography and gait measures in multiple sclerosis. Neurology. 2015;84:2048–2056. doi: 10.1212/WNL.0000000000001580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zelaya JE, Murchison C, Cameron M. Associations between bladder dysfunction and falls in people with multiple sclerosis. Int J MS Care. 2017;19(4):184–190. doi: 10.7224/1537-2073.2016-049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sanders KM, Stuart AL, Scott D, Kotowicz MA, Nicholson GC. Validity of 12-month falls recall in community-dwelling older women participating in a clinical trial. Int J Endocrinol. 2015:210527. doi: 10.1155/2015/210527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mazumder R, Murchison C, Bourdette D, Cameron M. Falls in people with multiple sclerosis compared with falls in healthy controls. PLoS One. 2014;9(9):e107620. doi: 10.1371/journal.pone.0107620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stolze H, Klebe S, Zechlin C, Baecker C, Friege L, Deuschl G. Falls in frequent neurological diseases—prevalence, risk factors and aetiology. J Neurol. 2004;251(1):79–84. doi: 10.1007/s00415-004-0276-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.