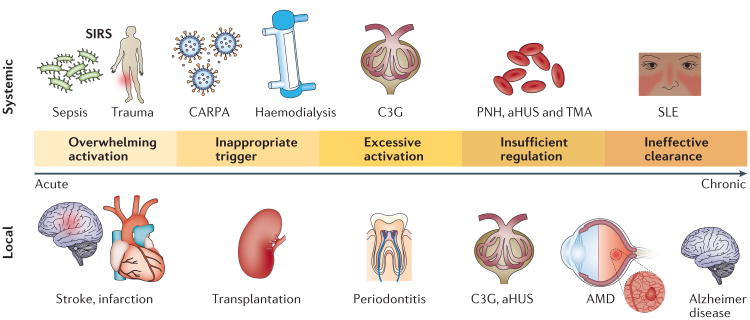
Figure 2. Major mechanisms of the pathogenic involvement of complement in systemic and local disorders.
Even when the complement system is operating normally, adverse activation can be triggered after exposure to massive amounts of pathogen, damage-associated stimuli or foreign surfaces such as transplanted organs or biomaterials. In many chronic disorders, genetic alterations lead to a systemic or local imbalance of complement that can contribute to inflammation, thrombosis and tissue damage. Ineffective removal of apoptotic cells, debris or immune complexes owing to the clearing capacity of the complement system being exceeded or deficiencies in complement components can induce or exacerbate autoimmune and neurodegenerative diseases. aHUS, atypical haemolytic uraemic syndrome; AMD, age-related macular degeneration; C3G, C3 glomerulopathy; CARPA, complement activation-related pseudo allergy; PNH, paroxysmal nocturnal haemoglobinuria; SIRS, systemic inflammatory response syndrome; SLE, systemic lupus erythematosus; TMA, thrombotic microangiopathy.