Abstract
Anterior cervical corpectomy and fusion (ACCF) is an effective surgical technique for cervical spondylotic myelopathy (CSM). However, no data exist regarding long-term outcomes after ACCF with the dynamic cervical plate for CSM. This study aimed to provide minimum 5-year clinical and radiographic outcomes of anterior corpectomy and reconstruction using dynamic cervical plate and titanium mesh cage (TMC) for CSM.
Thirty-five patients who underwent single- or 2-level ACCF with dynamic cervical plate and TMC for the treatment of CSM were retrospectively investigated. The Japanese Orthopedic Association (JOA) score was used to assess the clinical outcome. Radiographic evaluations included TMC subsidence, fusion status, cervical lordosis, segmental angle, and segmental height.
Twenty-eight patients underwent single-level and 7 patients underwent 2-level corpectomy with a mean follow-up period of 69.5 months. The average preoperative JOA score was 11.3 ± 3.0 and improved significantly to 14.2 ± 2.0 at the last follow-up (P < .001). Both cervical lordosis (P = .013) and segmental angle (P = .001) were significantly increased toward lordosis at the last follow-up. The TMC subsidence rate was 31.4% (n = 11) at the last follow-up. There was no significant difference in JOA recovery rate between subsidence and no subsidence group (P = .43). All patients obtained solid fusion at 1-year follow-up.
Anterior corpectomy and reconstruction with dynamic cervical plate and TMC might be an effective method for the treatment of CSM at a minimum 5-year follow-up. It can maintain or restore cervical sagittal alignment. Subsidence of the TMC did not influence the clinical outcome.
Keywords: anterior cervical corpectomy and fusion, cervical spondylotic myelopathy, dynamic cervical plate, 5-year follow-up, titanium mesh cage
1. Introduction
Cervical spondylotic myelopathy (CSM) is the most common cause of spinal cord impairment especially in elderly.[1] Patients with CSM typically manifest signs and symptoms including motor weakness, gait instability, hand clumsiness, and bowel and bladder incontinence. Surgery is generally recommended, as patients will deteriorate neurologically over time without surgical intervention.[2] Among various anterior and posterior surgical procedure, anterior cervical corpectomy and fusion (ACCF) is one of the efficient methods of treating CSM with satisfactory results.[3–6] Anterior corpectomy can directly remove the spinal cord compressions including osteophytes, herniated discs, and ossified posterior longitudinal ligament, without damaging the posterior neck muscles.[3]
Reconstruction after cervical corpectomy was initially used by autogenous iliac bone which is considered as the ‘golden standard’ strut graft for its high fusion rates and good clinical outcomes.[7] However, harvesting of autogenous iliac crest bone may lead to donor-site complications which include chronic donor site pain, blood loss, infection, and hematoma.[8,9] Autogenous fibula strut graft are a substitute but have been reported to be associated with prolonged incisional pain, tibial stress fractures, ankle instability, and superficial peroneal neuromas.[10] Though allografts were used to avoid donor-site complications, the allografts were associated with lower fusion rates and higher incidence of graft collapses.[11]
Titanium mesh cages (TMC) with anterior cervical plate had been widely used in anterior cervical surgery. Rigid cervical plate with TMC had obtained high fusion rate, provided rigid immobilization, and avoided donor site complications.[12] Unfortunately, the rigid cervical plate was reported to be associated with stress shielding and may lead to failure of plate and TMC construct.[13] Dynamic cervical plate was designed to increase load sharing and had demonstrated equal or superior clinical and radiologic outcomes compared with rigid cervical plates.[14–18] However, to the best of our knowledge, there is no long-term outcome regarding dynamic cervical plate for ACCF so far. In the present study, we used dynamic translational cervical plate with TMC for reconstruction after anterior cervical corpectomy. This dynamic translational cervical plate allows for a maximum of 4 and 5-mm axial translation in single- and 2-level coprectomy, respectively. The present study was designed to investigate the minimum 5-year follow-up clinical and radiographic outcomes of anterior corpectomy and reconstruction using dynamic cervical plate and TMC for CSM.
2. Materials and methods
2.1. Patient population
This retrospective study enrolled 35 patients with CSM between May 2009 and February 2012 at a single academic institution. The study was initiated after obtaining approval from the Ethical Committee of West China Hospital of Sichuan University. All patients signed an informed consent and agreed to participate in the study. All patients underwent single- or 2-level anterior corpectomy and reconstruction using dynamic cervical plate (Vectra-T, DePuy Synthes, West Chester, PA) and TMC with a minimum 5-year follow-up. Include criteria were patients presented with both clinical and radiographic evidence of CSM and were refractory to conservative treatment. Exclude criteria included previous cervical spine surgery, cervical spine trauma, active infection, rheumatoid arthritis, severe osteoporosis (T scores<−2.5) and neoplasm. Information about patients, surgery, and associated perioperative complications were obtained from medical records.
2.2. Surgical procedure
All the operations were performed by a single surgeon (HL). After general anesthesia, the patient was maintained in supine position with a pillow underneath the shoulders. A classic right-side Smith–Robinson approach was performed through a transverse incision.[19] The Caspar cervical retractor was used for soft tissue retraction in exposure. The Caspar vertebral body distractor was used for distraction. After adequate distraction, complete discectomy was performed followed by a single- or 2- level corpectomy. The vertebral body piecemeal was collected to fill the TMC. Then remove the posterior longitudinal ligament and posterior osteophytes; and carefully prepare the endplate. After thorough decompression, a vernier caliper was used to measure the distance between the lower endplate of the superior vertebrae body and the upper endplate of the inferior vertebrae body. The length of TMC was selected in accordance with the lengths of vernier caliper. After that, insert the TMC that filled with local bone. Finally, the Vectra-T anterior cervical dynamic plate was implant for stabilization. A drainage catheter was placed and incisions were sutured.
2.3. Outcome assessment
Clinical and radiographic data were collected preoperatively, immediately after operation, at 3, 6, 12, months after surgery and then annually thereafter. The evaluation of TMC subsidence, fusion status, cervical lordosis, segmental angle, and segmental height were conducted using anteroposterior, lateral, and flexion/extension plain radiographic.
The Japanese Orthopedic Association (JOA) scoring system was used to assess the neurologic status. And the neurological recovery rate was calculated by the formula: recovery rate = (JOA score − preoperative JOA score)/(17-preoperative JOA score) × 100%.[20]
Cervical lordosis was defined as the Cob angle formed by the inferior endplates of C2 and C7 (Fig. 1). Segmental angle was defined as the Cob angle formed by the superior and inferior endplate of fused segment (Fig. 1). Segmental height was measured by the distance between the mid-point of the superior and inferior endplate of fused segment (Fig. 1). TMC subsidence was defined as change of ≥3 mm of fused segmental height. Solid fusion was defined as interspinous process motion <1 mm on flexion/extension plain radiographs.[21] If indeterminate radiographic evaluations were present, we used CT for further assessments. Symptomatic adjacent segment degeneration (ASD) was defined as the presence of clinical symptoms and homologous degeneration changes on Magnetic Resonance Imaging (MRI) examination. A single independent orthopedic surgeon performed these analyses using Canvas X16 software (ACD Systems, Seattle, Washington)
Figure 1.
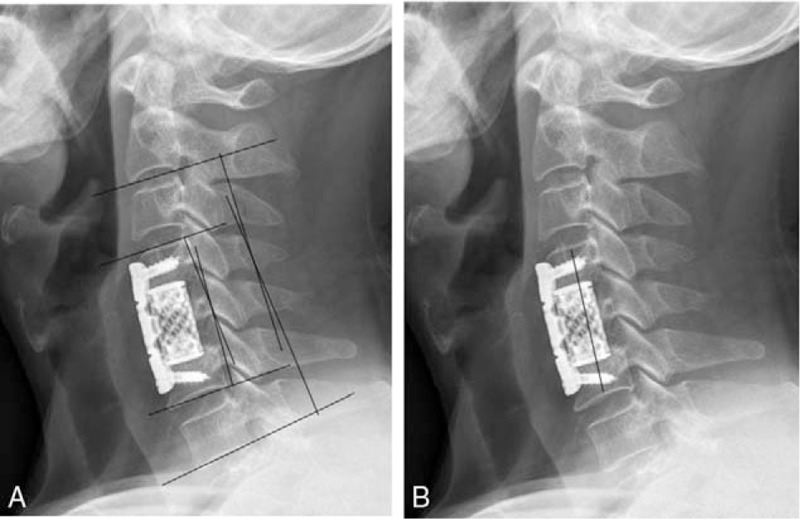
(A) Measurements of cervical lordosis and segmental angle; (B) Segmental height was measured by the distance between the midpoint of the superior and inferior endplate of fused segment.
2.4. Statistical analysis
Statistical analysis was performed using SPSS version 22.0 software (SPSS Inc., Chicago, Illinois). Quantitative data are presented as the mean ± SD. The nonparametric Wilcoxon signed-rank test was applied for comparison of pre- and postoperative results. The nonparametric Mann–Whitney U test was used to compare results between independent groups. Fisher exact test was used to compare binary data between independent groups. Statistical significance is assumed at a P value of <0.05.
3. Results
3.1. General data
This retrospective study included 35 patients (19 men and 16 women) with a mean age of 54.4 (range, 32–78) years. The mean follow-up duration was 69.5 (range, 60–87) months. A single-level cervical corpectomy was performed in 28 patients and a 2-level cervical corpectomy in 7 patients. The average operative time was 137.4 ± 20.3 minutes. The mean blood loss was 93.4 ± 24.9 mL. There was no significant difference regarding sex (P > .99), age (P = .51), or duration of follow-up (P = .92) between single- and 2-level corpectomy. General results are summarized in Table 1 and Table 2.
Table 1.
Summary of patients general data.
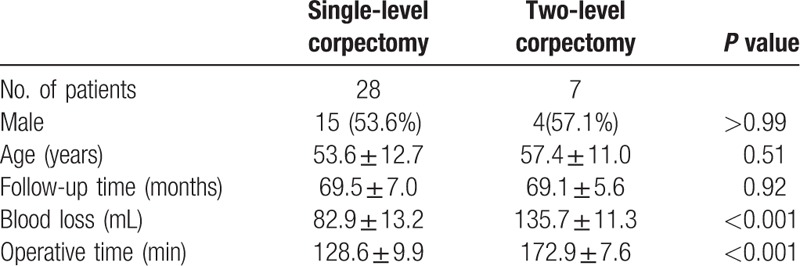
Table 2.
Summary of the involved segments.
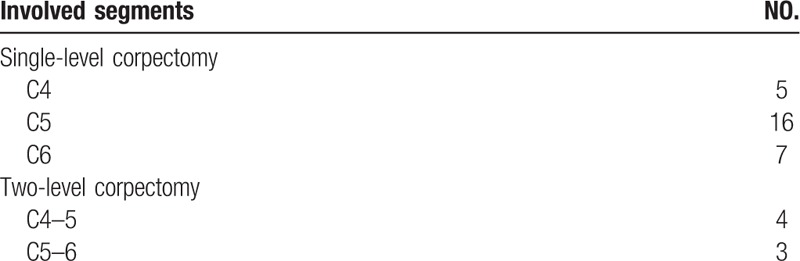
3.2. Clinical outcome
The average preoperative JOA score was 11.3 ± 3.0. The JOA score improved significantly to 14.3 ± 2.1 points 3 months after surgery (P < .001) and was maintained at 14.2 ± 2.0 points at the last follow-up (P < .001). There was no significant difference between JOA score at 3 months postoperatively and the last follow-up (P = .62). There was no significant difference regarding JOA score between single- and 2-level corpectomy preoperatively (P = .45), 3month postoperatively (P = .73), or at the last follow-up (P = .61). The JOA recovery rate was 56.1 ± 22.3% 3 months postoperatively and 54.6 ± 19.3% at the last follow-up. No significant difference was detected in JOA recovery rate between subsidence and no subsidence group (P = .43). Clinical outcome results are summarized in Table 3.
Table 3.
Summary of JOA scores and JOA recovery rate at follow-ups.
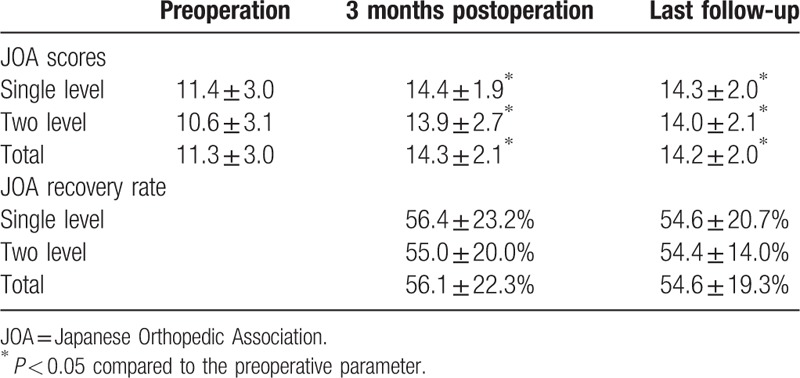
3.3. Radiographic outcome
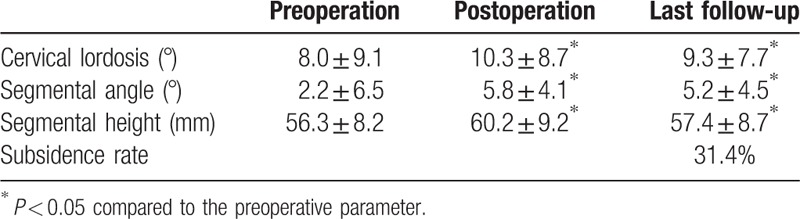
The mean cervical lordosis was 8.0 ± 9.1° preoperatively, significantly increased to 10.3 ± 8.7° immediately after operation (P = .003), and was maintained at 9.3 ± 7.7° at the last follow-up (P = .013). The average segmental angle significant improved from 2.2 ± 6.5° preoperatively to 5.8 ± 4.1° immediately postoperatively (P < .001) and was maintained at 5.2 ± 4.5° at the last follow-up (P = .001). Both cervical lordosis (P = .013) and segmental angle (P = .001) were significantly increased toward lordosis at the last follow-up compared with that of preoperatively. The mean segment height was 56.3 ± 8.2 mm preoperatively and significantly increased to 60.2 ± 9.2 mm immediately after surgery (P < .001). But segmental height significantly decreased to 57.4 ± 8.7 mm at the last follow-up compared with that of immediately after surgery, which represented a mean 2.8 ± 1.3 mm decrease (P < .001). The TMC subsidence rate was 31.4% (n = 11) at the last follow-up. No significant difference was found regarding subsidence rate between single- and 2-level corpectomy (P = .65). The fusion rate at 3- and 6-month follow-up was 74.3% (26/35) and 88.6% (31/35), respectively. Solid fusion was observed in all patients at the 1-year follow-up. Radiographic outcome results are summarized in Table 4.
Table 4.
Summary of cervical lordosis, segmental angle and subsidence at follow-ups.
3.4. Complications
No hardware-related complication including plate fracture, screw broken, or TMC dislodgement occurred. One patient experienced the upper screw slightly back out and did not complain any discomfort (Fig. 2). Dural tears occurred in 2 patients; both patients were successfully treated by drainage. No patients showed postoperative wound infection, esophageal laceration, epidural hematoma, or vertebral artery rupture. Three patients (8.6%) were diagnosed with symptomatic ASD which were confirmed by clinical symptoms and MRI examination (Fig. 3). Two patients complained arm and neck pain and 1 patient complained sensory defects. All 3 patients were treated conservatively and symptoms were resolved within 6 weeks. Two patients suffered dysphagia that persisted for more than 6 weeks; symptoms of both patients spontaneously resolved within 12 months.
Figure 2.

A 59-year-old woman who underwent a C4–5 2-level corpectomy. (A) Immediate postoperative lateral radiograph; (B) Lateral radiograph at 1-year follow-up shown the upper screw was slightly back out (the arrow). The patient did not complain any discomfort.
Figure 3.
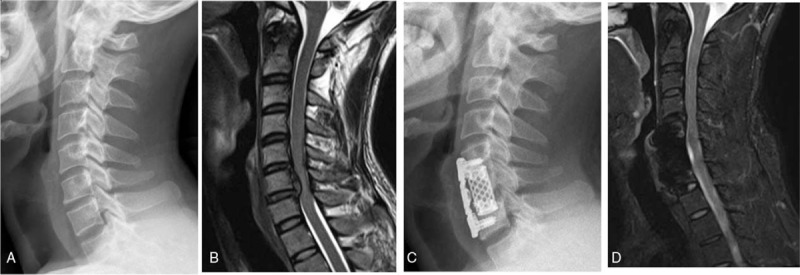
A 32-year-old man who underwent a C6 corpectomy. (A) Preoperative lateral radiograph; (B) Preoperative sagittal T2-weigh MRI showing the cervical disc degeneration at C5/6 and C6/7; (C) Lateral radiograph at 5-year follow-up; (D) Sagittal T2-weigh MRI showing the adjacent level degeneration (C4/5) at 5-year follow-up. This patient complained arm and neck pain and was treated conservatively. These symptoms were re resolved within 6 weeks. MRI = magnetic resonance imaging.
4. Discussion
There are several established surgical methods of treating CSM in terms of anterior and posterior approaches. Although optimal surgical treatment option for CSM remains controversial, ACCF have advantages in directly removing the pathogenic structures, maintaining or restoring cervical lordosis, and no damage of posterior neck muscles.[22] Autogenous iliac bone graft has been the ‘golden standard’ struts for reconstruction after anterior cervical corpectomy. However, the reported high incidence of donor site complications cannot be overlooked.[8,9] TMCs has been used to reduce donor-site complications and achieved satisfactory fusion rates; and rigid anterior cervical plate can offer immediate stabilization, reduce graft dislodgement, and provide rigid internal fixation.[12] However, because rigid plates also decrease compression forces across the intervertebral grafts, dynamic plates were designed to minimize stress shielding and enhance fusion rates. Previous biomechanical studies have supported that dynamic plates allowed more load transmission by the intervertebral graft.[14,15] Previous studies also indicated that dynamic plates had superior or at least equal clinical outcome compared with rigid plates.[16–18]
In the present study, the reliefs of myelopathic symptoms in the 35 patients were supported by an overall increase of 3.0 points in the JOA scores. The JOA score was improved significantly after surgery and maintained to the minimum 5-year follow-up. And satisfactory JOA recovery rate (54.6%) was observed at the last follow-up. Several investigators have reported the long-term follow-up outcomes of ACCF for patients diagnosed with CSM. Andaluz et al[5] performed a retrospective study and found an overall almost 3-point improvement in the Chiles modified Japanese Orthopedic Association scores in 130 patients undergoing a single- or 2-level ACCF. Similarly, Gao et al[6] conducted a retrospective study of 145 patients and found a 3.8 points increase in JOA scores and the overall recovery rate was 62.5%. All these previous studies used rigid cervical plate with TMC or other graft material for reconstruction after cervical corpectomy. We used dynamic cervical plate and TMC for ACCF, and obtained the same successful results. We hold that thorough decompression plays an important role in the relief of myelopathic symptoms after cervical surgery.
Postoperative kyphotic in segment angle and the whole spine curvature has been reported after uninstrumented corpectomy in several studies.[23,24] Andaluz et al[5] reported an overall progressive postoperative kyphotic increase in focal lordosis, but a lordotic increase in regional cervical sagittal alignment. In the present study, cervical lordosis and segmental angle were increased toward lordosis postoperatively compared with that of preoperatively. Similar results were reported by Zhang et al[4] and Gao et al[6] Our data demonstrated that dynamic cervical plate with TMC can maintain and restore cervical lordosis after cervical corpectomy.
Graft subsidence was a common phenomenon after ACCF. The impact of subsidence on cervical fusion and clinical outcome remains controversial. Chen et al[25] reported that severe subsidence (>3 mm) occurred in 19.0% of the patients, and these patients has a lower JOA recovery rate. They concluded that severe subsidence was associated with bad clinical results and subsidence-related complications. Karikari et al[26] conduct a systematic review and concluded that subsidence did not have impact on successful fusion or clinical outcomes. Yan et al[27] concluded that cage subsidence did not correlated with clinical outcome, nor sagittal alignment, or fusion rate. In the present study TMC subsidence rate was 31.4% at the last follow-up. We found no significant difference in JOA recovery rate between subsidence and no subsidence group (P = .43). Our study indicated that subsidence of the TMC did not influence the clinical outcome. We speculate that once the TMC subsiding into the vertebra body (Fig. 4), the dynamic plate can translate to a shorter plate to accommodate the subsidence. In case the plate was rigid, the high stress induced by the subsidence could lead to the fracture of the screws and the plate. The dynamic plate can therotically reduce this complication. This may be 1 of the reasons that the subsidence of TMC did no harm to the clinical outcome.
Figure 4.
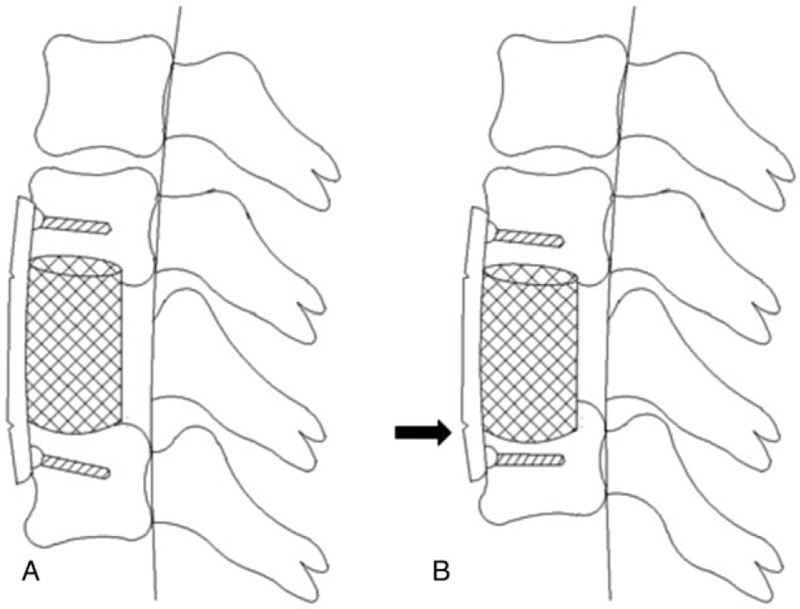
(A)The titanium mesh cage did not subside into the vertebra body; (B) The TMC subsided into the vertebra (the arrow). And the dynamic translational cervical plate shortened to accommodate the subsidence.
Rhee et al[21] conducted a systematic review to find the best radiographic assessment criteria for cervical fusion in 2015. They recommended using interspinous process motion less than 1 mm on flexion/extension plain radiograph as the modality for determining anterior cervical arthrodesis. According to these fusion criteria, we documented a fusion rate of 100% in the current study at 1-year follow-up. Similar fusion results were reported in previous studies.[4–6] The rigid cervical plate fixation can cause the plate to shift load from the graft, resulting in stress shielding. The dynamic cervical plate allowed more load transmission by the graft.[14] Base on Wolff's theory, dynamic cervical plate can theoretically promote bone fusion.
Previous biomechanical and clinical studies suggested that cervical fusion may accelerate the ASD.[28,29] However, it is still not clear whether ASD is a natural progression or the result of cervical fusion. The symptomatic ASD rate was 8.6% in our study. All these 3 patients had different degrees of preoperative disc degeneration at adjacent segments. We believe that preexisting degeneration at the adjacent segment has an important influence on the development of symptomatic ASD.
As with all studies, the current study had several limitations. First, the sample size was small and potential selection bias may exist. Second, this was a retrospective study without setting a control group. Last, because of significant difference was detected in blood loss and operative time between single- and 2-level corpectomy, comparison of outcomes between these two groups may be associated with bias. Future prospective, controlled, randomized trials with large sample sizes are warranted to further evaluate efficacy of this surgical technique for CSM.
5. Conclusion
Minimum 5-year follow-up of clinical and radiographic outcomes demonstrates that dynamic cervical plate and TMC for cervical reconstruction after corpectomy might be a safe and efficacy surgical technique for CSM. Cervical sagittal alignment including cervical lordosis and segmental angle were maintained or restored. Satisfactory fusion rate, JOA scores, and JOA recovery rate were obtained. Furthermore, this study revealed that subsidence of the TMC did not influence the clinical outcome. Prospective multicenter controlled study with large sample is needed to further verify our findings in this study.
Footnotes
Abbreviations: ACCF = Anterior cervical corpectomy and fusion, ASD = adjacent segment degeneration, CSM = cervical spondylotic myelopathy, JOA = Japanese Orthopedic Association, TMC = titanium mesh cage.
The authors declare no conflict of interest.
References
- [1].Young WF. Cervical spondylotic myelopathy: a common cause of spinal cord dysfunction in older persons. Am Fam Physician 2000;62:1064-1070, 1073. [PubMed] [Google Scholar]
- [2].Karadimas SK, Erwin WM, Ely CG, et al. Pathophysiology and natural history of cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2013;38(22 Suppl 1):S21–36. [DOI] [PubMed] [Google Scholar]
- [3].Fessler RG, Steck JC, Giovanini MA. Anterior cervical corpectomy for cervical spondylotic myelopathy. Neurosurgery 1998;43:257–65. [DOI] [PubMed] [Google Scholar]
- [4].Zhang Y, Deng X, Jiang D, et al. Long-term results of anterior cervical corpectomy and fusion with nano-hydroxyapatite/polyamide 66 strut for cervical spondylotic myelopathy. Sci Rep 2016;6:26751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Andaluz N, Zuccarello M, Kuntz C. Long-term follow-up of cervical radiographic sagittal spinal alignment after 1- and 2-level cervical corpectomy for the treatment of spondylosis of the subaxial cervical spine causing radiculomyelopathy or myelopathy: a retrospective study. J Neurosurg Spine 2012;16:2–7. [DOI] [PubMed] [Google Scholar]
- [6].Gao R, Yang L, Chen H, et al. Long term results of anterior corpectomy and fusion for cervical spondylotic myelopathy. PloS one 2012;7:e34811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Saunders RL, Bernini PM, Shirreffs TG, Jr, et al. Central corpectomy for cervical spondylotic myelopathy: a consecutive series with long-term follow-up evaluation. J Neurosurg 1991;74:163–70. [DOI] [PubMed] [Google Scholar]
- [8].Kurz LT, Garfin SR, Booth RE., Jr Harvesting autogenous iliac bone grafts. A review of complications and techniques. Spine (Phila Pa 1976) 1989;14:1324–31. [DOI] [PubMed] [Google Scholar]
- [9].Silber JS, Anderson DG, Daffner SD, et al. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2003;28:134–9. [DOI] [PubMed] [Google Scholar]
- [10].Nassr A, Khan MH, Ali MH, et al. Donor-site complications of autogenous nonvascularized fibula strut graft harvest for anterior cervical corpectomy and fusion surgery: experience with 163 consecutive cases. Spine J 2009;9:893–8. [DOI] [PubMed] [Google Scholar]
- [11].Fernyhough JC, White JI, LaRocca H. Fusion rates in multilevel cervical spondylosis comparing allograft fibula with autograft fibula in 126 patients. Spine (Phila Pa 1976) 1991;16(10 Suppl):S561–4. [DOI] [PubMed] [Google Scholar]
- [12].Majd ME, Vadhva M, Holt RT. Anterior cervical reconstruction using titanium cages with anterior plating. Spine (Phila Pa 1976) 1999;24:1604–10. [DOI] [PubMed] [Google Scholar]
- [13].Hee HT, Majd ME, Holt RT, et al. Complications of multilevel cervical corpectomies and reconstruction with titanium cages and anterior plating. J Spinal Disord Tech 2003;16:1–8. [DOI] [PubMed] [Google Scholar]
- [14].Reidy D, Finkelstein J, Nagpurkar A, et al. Cervical spine loading characteristics in a cadaveric C5 corpectomy model using a static and dynamic plate. J Spinal Disord Tech 2004;17:117–22. [DOI] [PubMed] [Google Scholar]
- [15].Mackiewicz A, Banach M, Denisiewicz A, et al. Comparative studies of cervical spine anterior stabilization systems: finite element analysis. Clin Biomech 2016;32:72–9. [DOI] [PubMed] [Google Scholar]
- [16].Epstein NE. Anterior cervical dynamic ABC plating with single level corpectomy and fusion in forty-two patients. Spinal Cord 2003;41:153–8. [DOI] [PubMed] [Google Scholar]
- [17].Nunley PD, Jawahar A, Kerr EJ, 3rd, et al. Choice of plate may affect outcomes for single versus multilevel ACDF: results of a prospective randomized single-blind trial. Spine J 2009;9:121–7. [DOI] [PubMed] [Google Scholar]
- [18].Schroeder GD, Kepler CK, Hollern DA, et al. The effect of dynamic versus static plating systems on fusion rates and complications in 1-level and/or 2-level anterior cervical discectomy and fusion: a systematic review. Clin Spine Surg 2017;30:20–6. [DOI] [PubMed] [Google Scholar]
- [19].Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 1958;40-A:607–24. [PubMed] [Google Scholar]
- [20].Hirabayashi K, Miyakawa J, Satomi K, et al. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine (Phila Pa 1976) 1981;6:354–64. [DOI] [PubMed] [Google Scholar]
- [21].Rhee JM, Chapman JR, Norvell DC, et al. Radiological determination of postoperative cervical fusion: a systematic review. Spine (Phila Pa 1976) 2015;40:974–91. [DOI] [PubMed] [Google Scholar]
- [22].Luo J, Cao K, Huang S, et al. Comparison of anterior approach versus posterior approach for the treatment of multilevel cervical spondylotic myelopathy. Eur Spine J 2015;24:1621–30. [DOI] [PubMed] [Google Scholar]
- [23].Hughes SS, Pringle T, Phillips F, et al. Settling of fibula strut grafts following multilevel anterior cervical corpectomy: a radiographic evaluation. Spine (Phila Pa 1976) 2006;31:1911–5. [DOI] [PubMed] [Google Scholar]
- [24].Thakar S, Ch M, Vedantam A, et al. Correlation between change in graft height and change in segmental angle following central corpectomy for cervical spondylotic myelopathy. J Neurosurg Spine 2008;9:158–66. [DOI] [PubMed] [Google Scholar]
- [25].Chen Y, Chen D, Guo Y, et al. Subsidence of titanium mesh cage: a study based on 300 cases. J Spinal Disord Tech 2008;21:489–92. [DOI] [PubMed] [Google Scholar]
- [26].Karikari IO, Jain D, Owens TR, et al. Impact of subsidence on clinical outcomes and radiographic fusion rates in anterior cervical discectomy and fusion: a systematic review. J Spinal Disord Tech 2014;27:1–0. [DOI] [PubMed] [Google Scholar]
- [27].Yan D, Wang Z, Deng S, et al. Anterior corpectomy and reconstruction with titanium mesh cage and dynamic cervical plate for cervical spondylotic myelopathy in elderly osteoporosis patients. Arch Orthop Trauma Surg 2011;131:1369–74. [DOI] [PubMed] [Google Scholar]
- [28].Eck JC, Humphreys SC, Lim TH, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976) 2002;27:2431–4. [DOI] [PubMed] [Google Scholar]
- [29].Hilibrand AS, Carlson GD, Palumbo MA, et al. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 1999;81:519–28. [DOI] [PubMed] [Google Scholar]


