Figure 2.
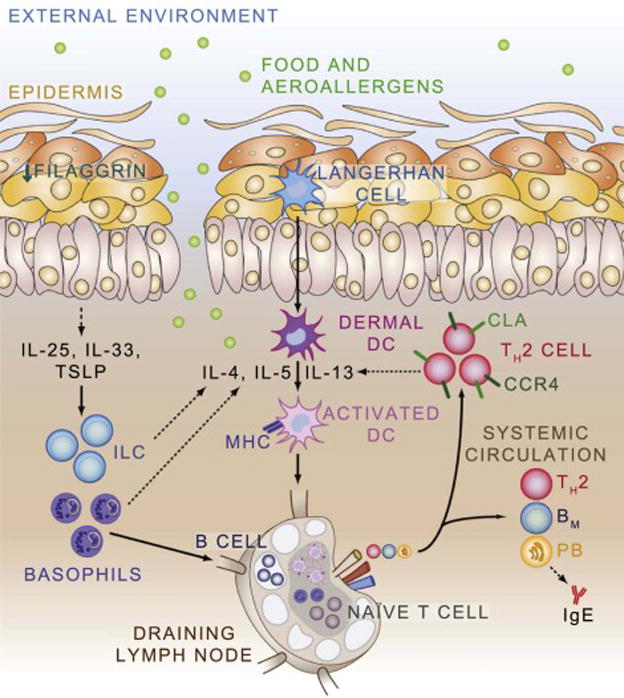
Model of the Atopic March. Deficiencies in epithelial proteins such as filaggrin, in conjunction with atopic predisposition, result in skin inflammation. Epithelial-derived cytokines such as Il-25, Il-33, and TSLP recruit and activate innate cell types including innate lymphoid cells (ILC) and basophils which produce cytokines that promote the activation of dendritic cells. Activated dendritic cells process allergen, upregulate MHC, and circulate to draining lymph nodes where they can interact with naïve T and B cells to promote the development of allergen-specific T and B cell responses. Allergen-specific T helper type 2 (TH2) cells home back to the skin through expression of C-C chemokine receptor type 4 (CCR4), cutaneous lymphocyte antigen (CLA), and other molecules. TH2 cells also enter the systemic circulation where they can exert effector response at distant tissue sites. Memory B cells (BM) recirculate in the blood and lymph, while plasmablasts (PB) home to the bone marrow where they differentiate in to plasma cells and produce allergen-specific IgE.
