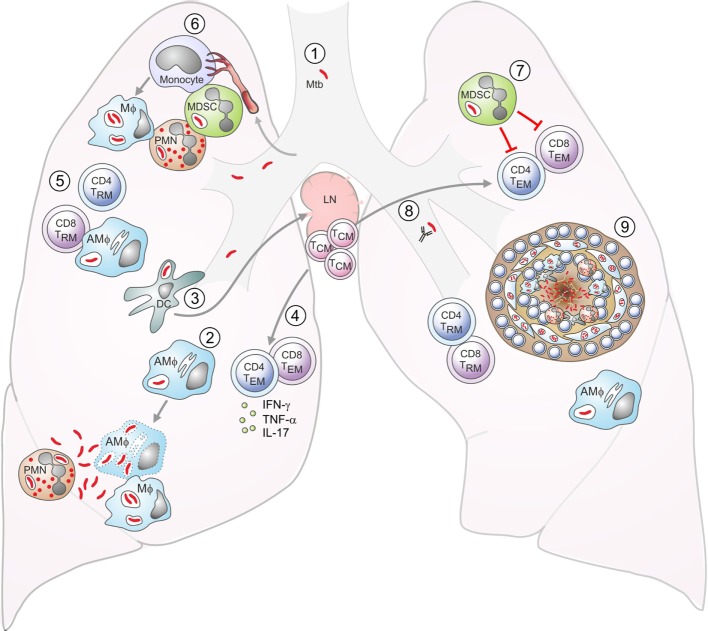
Figure 1.
Aspects of tuberculosis (TB) immunology. DC: dendritic cell; Mϕ: macrophage; AMϕ: alveolar macrophage; TEM: effector memory T cell; TCM: central memory T cell; TRM: resident memory T cell; MDSC: myeloid-derived suppressor cell; PMN: neutrophil. (1) Exposure to Mycobacterium tuberculosis (Mtb) is by the inhalation of infected aerosol droplets generated by coughing. (2) Mtb bacilli primarily live in host macrophages. Alveolar macrophages and other myeloid cells such as DCs can take up bacteria from the airways. If macrophages do not control infection, the bacteria can replicate and kill the cell. Bacteria can also infect neutrophils, which die and can be taken up by macrophages, which subsequently become infected themselves. (3) Infected DCs have delayed migration to the lymph nodes and impaired antigen presentation. In the lymph nodes, they transfer antigens to uninfected bystander DCs, which present the antigens to T cells. (4) Effector CD4+ and CD8+ T cells generated from naive T cells or from memory T cells are recruited to the lungs. (5) Effector CD4+ T cells produce cytokines such as IFN-γ, interleukin (IL)-17, and TNF-α, while CD8+ T cells can lyse infected macrophages. IFN-γ can activate bacterial killing. (6) Neutrophils, monocytes, or immature myeloid cells with suppressive functions, known as MDSCs are recruited to the lungs. Monocytes can differentiate into inflammatory macrophages or inflammatory DCs. (7) MDSCs aim to limit excessive inflammation by inhibiting T-cell proliferation and function, but they can act as a reservoir for Mtb. (8) Antibodies may also play a role in controlling infection. (9) Eventually, the immune cells form a granuloma around Mtb in an attempt to contain the bacteria. These are the typical lesions observed in the Mtb-infected lung, most commonly in the upper lobes.