Abstract
Background:
Imaging has a big role in tuberculosis (TB) diagnosis and chest X-ray is preferable because it is available in primary health care and can point out the location, area, and morphology of lesions, such as cavity, consolidation, pleural effusions, and fibrosis. We aimed to compare the chest X-ray findings in multi-drug resistant TB (MDR-TB) and in drug-sensitive TB (DS-TB) cases.
Methods:
This is a retrospective cross-sectional study which compares chest X-ray findings of two groups of patients, involving 183 DS-TB patients and 183 MDR-TB patients. Radiologic findings that we analyzed were infiltrate, consolidation, cavity, ground glass opacity, fibrosis, bronchiectasis, calcification, node, atelectasis, bullae, emphysema, and other nonlung parenchymal findings.
Results:
MDR-TB group have 177 (96%) patients with large lesions, 6 (4%) with medium lesions, and no small lesions. DS-TB group have 55 (30%) patients with small lesions, 78 (43%) with medium lesions, and 50 (27%) with large lesions. Active TB lesions in the forms of infiltrate and ground-glass opacity were more dominant in DS-TB group, whereas consolidation, cavity, fibrosis, bronchiectasis, calcification, node, atelectasis, bullae, emphysema, and other nonlung parenchymal findings, were more dominant in MDR-TB.
Conclusions:
There were significant differences in chest X-ray findings between MDR-TB and DS-TB in terms of lesion size and morphology. Recognition of chest X-ray findings could help the physician to differentiate patient with suspected MDR-TB.
Keywords: Chest X-ray, drug-sensitive tuberculosis, multi-drug resistant tuberculosis
INTRODUCTION
Tuberculosis (TB) is a chronic granulomatous disease caused by Mycobacterium tuberculosis (MTB) that has been announced as a global health emergency by the World Health Organization (WHO). TB has infected approximately a third of world population with estimated 1.6 million mortality yearly.[1,2,3] Among those infected, 3.5% of new cases and 20.5% of old cases are infected with multi-drug resistant TB (MDR-TB).[4,5] Indonesia is the 8th country with the most MDR-TB cases in the world, with estimated 6900 cases or 1.9% from new cases and 12.5% of old cases.[1,5] MDR-TB diagnosis is made by performing the drug-sensitivity test of MTB and supported by physical examination, microbiology, and radiology.
Imaging has a big role in TB diagnosis due to the limitations of microbiology examinations in Indonesia. Radiologic examinations that can be used to diagnose TB and evaluate therapy in Indonesia are computed tomography and chest X-ray. Chest X-ray is preferable because it is available in primary health care and can point out the location, area, and morphology of lesions, such as cavity, consolidation, pleural effusions, and fibrosis.[3,4] These findings are very important considering the increasing number of MDR-TB cases, either new or old ones because chest X-ray evaluates the response of the therapy so that early diagnosis of MDR-TB can be achieved.[2,5,6]
To have a better early diagnosis for TB, a basic knowledge to differentiate chest X-ray findings between drug-sensitive TB (DS-TB) and MDR-TB are needed.[2,5,6] Until now, there are not many studies that elaborate the comparison of chest X-ray findings in MDR-TB and DS-TB cases.
METHODS
This study is carried out retrospectively with a comparative cross-sectional study design that compares two groups of patients, one with DS-TB and the other with MDR-TB. This study was conducted in the Department of Radiology, Persahabatan Hospital, Jakarta, using secondary data that were acquired from the medical record of patients from January 2013 to December 2015. The study protocol was approved by the Ethical Committee of Persahabatan Hospital, Jakarta, Indonesia (Ethical Clearance Number: 74/KEPK-RSP/I/2016). A total of patients in this study was 183 MDR-TB patients (96 men and 87 women; mean 39.87 and median age 56 years) and 183 DS-TB patients (127 men and 56 women; mean 41.03 and median age 42 years). TB diagnosis is confirmed from the chest X-ray results, sputum smear, and culture results from the medical record.
Chest X-ray results that were obtained from the medical record was re-evaluated by one radiologist who specializes in thoracic radiologist and one senior radiology resident. Assessment of the chest X-ray results is performed according to thoracic assessment form. Chest X-ray characteristics that were assessed were 14 types of morphology lesions, area, and location of the lesion (s). The obtained data were edited and coded, then goes through validation. After validation, the data were tabulated and calculated using IBM SPSS Statistics for Windows, Version 20.0. (Armonk, NY: IBM Corp). For quantitative data, mean, standard deviation, and 95% confidence interval were calculated.
RESULTS
Participants and patients
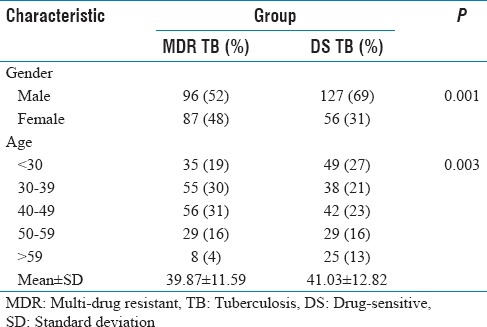
The sample for this research was gathered from the medical records of MDR-TB and DS-TB patients from Persahabatan Hospital, Jakarta. Using this collecting method, 183 patients from MDR-TB group and 183 patients from DS-TB group were gathered and analyzed statistically. Genders of the patients were mostly male (54% for MDR-TB and 69% for DS-TB). Age distributions were mostly 40–49-year-old in MDR-TB and DS-TB (31% and 23%, respectively). The mean age was 39.87-year-old with 11.59 standard deviation for MDR-TB and 41.03-year-old with 12.82 standard deviations for DS-TB. Details for demographic distributions are presented in Table 1.
Table 1.
Demographic characteristic between multi-drug resistant tuberculosis and drug-sensitive tuberculosis groups
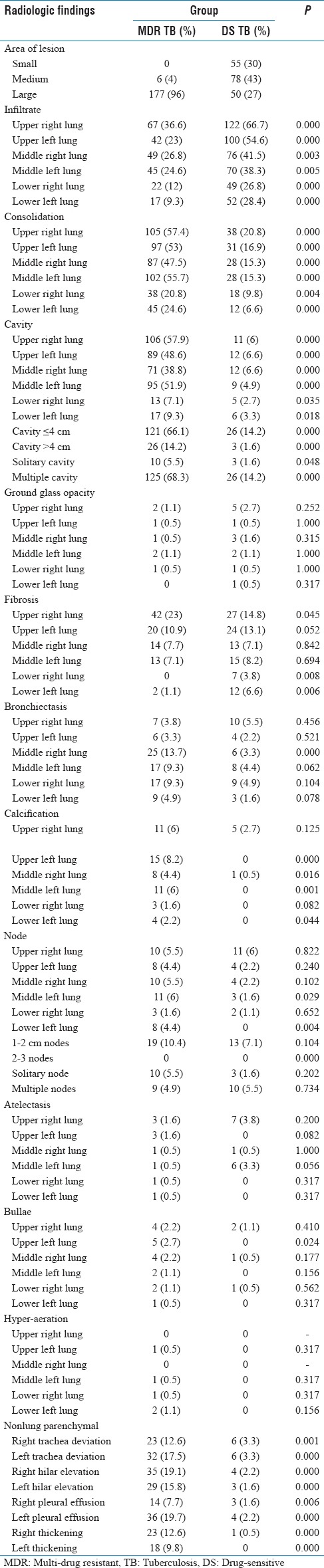
Radiologic findings
The MDR-TB group has 177 (96%) patients with large lesions, 6 (4%) with medium lesions, and no small lesions. DS-TB group have 55 (30%) patients with small lesions, 78 (43%) with medium lesions, and 50 (27%) with large lesions. Radiologic findings that we analyzed were infiltration, consolidation, cavity, ground glass opacity, fibrosis, bronchiectasis, calcification, node, atelectasis, bullae, emphysema, and other nonlung parenchymal findings.
Active TB lesions, infiltrate in this case, were more dominant in DS-TB group compared to MDR-TB, especially the ones in the upper right lung. Consolidation finding is more dominant in MDR-TB in both lungs and can be found in more than one part of each lung. Consolidation was founded most at the upper left lung (57.4%), middle left lung (55.7%), and upper left lung (57.4%). In DS-TB, 20.8% was found in the upper right lung, 15.3% middle left lung, and 16.9% in the upper left lung.
Consolidations at both lungs in MDR-TB group were more dominant compared to DS-TB group. These consolidation findings can be found in more than one part of the lung, either right or left lung. Most MDR-TB consolidations were found in the upper right lung (57.4%), middle left lung (55.7%), and upper left lung (53%). In DS-TB group, most consolidations were also found in the upper right lung (20.8%), middle left lung (15.3%), and upper left lung (16.9%).
Most other radiologic findings, such as cavity, fibrosis, bronchiectasis, calcification, node, atelectasis, bullae, emphysema, and other nonlung parenchymal findings, were found more in MDR-TB group. The only exception was ground glass opacity that was found more in DS-TB group. The details of radiologic findings are shown in Table 2.
Table 2.
Radiologic finding between multi-drug resistant tuberculosis and drug-sensitive tuberculosis groups
DISCUSSION
This study shows the comparison of chest X-ray findings of MDR-TB and DS-TB in adult patients with the competent immune system. The population of the MDR-TB and DS-TB samples that were recorded in Persahabatan Hospital from January 2013 to December 2015 were 230 and 240 samples, respectively, and only 183 samples from each group that fulfills the inclusion criteria. Some of the samples are also excluded due to some of the data, such as chest X-ray, laboratory examination, and drug resistance, are incomplete in the medical record.[3,4]
Demographic characteristic distribution of gender in both groups showed that there are more male than female, 52% male compared to 48% female in MDR-TB and 69% male to 31% female in DS-TB group. Yoon et al. also had similar findings and concluded that male is more likely to be infected due to the higher exposure and having a higher risk of infection. Delay in diagnosis and early detection of pulmonary TB is a serious problem in Vietnam because female patients were afraid to be excommunicated by family and friends if they suffered from pulmonary TB.[2,4]
Both MDR-TB and DS-TB group had most patients with age range from 40 to 49, 31% and 23%, respectively, with a mean age of 39.87 for MDR-TB and 41.03 for DS-TB. In other studies, patients' age results were not much different.[3,4,7] The WHO in 2013 stated that most TB patients are in their productive age. High level of mobility and social interaction in productive ages supports the higher prevalence of TB due to the increased risk of exposure.[3,4]
The large lesion was found in both MDR and DS-TB group (69% vs. 27%) and showed a significant difference. Extensive tissue damage caused by the long duration of disease is suspected to be the reason why a lot of large lesions were found in MDR-TB group. A significant difference in the degree of lesions in both groups is caused by the difference in disease progression, except in primary MDR-TB that was caused by contaminated environment or previous interaction with the MDR-TB patient without any protection.[3,4,8,9]
Active lesion of lung parenchymal was found more in MDR-TB compared to DS-TB and dominated by multiple consolidation and multiple cavities. Active lesion morphologies in MDR-TB were consolidation (57.4%), cavity (57.9%), infiltrate (36.6%), and ground glass opacity (1.1%). These active lesions were found mostly in right upper lung. Most of the lung parenchymal active lesions in DS-TB were also found in the upper right lung. Active lesions for DS-TB group were infiltrate (66.7%), consolidation (20.8%), the cavity (6%), and ground glass opacity (2.7%). Cavity with ≤4 cm in MDR-TB was found most on upper right lung (66.1%) and had a significant difference compared to DS-TB (14.2%) group (P < 0.005). Multiple cavities were found on 68.3% MDR-TB group and had a significant difference compared to 14.2% of DS-TB group (P < 0.005). Deesuwan et al. and Cha et al. stated that active lesions that were mostly found in thorax X-ray for MDR-TB patients are multiple consolidations and multiple cavities. Multiple reticulonodular infiltrate, ground glass opacity, and multiple or solitary cavities are the dominant X-ray findings for DS-TB patients.[7,10,11] These studies support the hypothesis that the dominant characteristic lesions in MDR-TB are multiple consolidations and multiple cavities (P < 0.005). All active lung parenchymal lesions in MDR-TB and DS-TB were mostly found in the upper region of the lung. Some references stated that the dominant consolidations and cavities in MDR-TB were caused by failed treatment on a postprimary TB or mutation of MTB that caused the bacteria to be resistant to anti-TB drugs. These resistant bacteria might cause TB reactivation and spreads to the right and left lung, forming consolidation and infiltrate at early stages that develop to the cavity, through the lymphatic system, blood, or endobronchial. Unhealed cavity might cause new consolidations and in turn, make new cavities. Other study stated that cavities are a predisposing factor for TB treatment failure and reoccurrence.[4,7,11,12]
Some nonlung parenchymal morphologies in the lung for MDR-TB and DS-TB had a significant difference (P < 0.005), such as bronchiectasis in middle right lung. Node and tuberculoma on lower left lung also had a significant difference (P < 0.005%) in MDR-TB (4.4%) compared to DS-TB (0). A study by Deesuwan et al. stated that nonactive lesion found in MDR-TB was multiple bronchiectases. On contrary, this study did not found a significant difference in multiple bronchiectasis finding between MDR-TB and DS-TB group.
Bronchiectasis is a diffuse dilatation of multiple bronchi resulting from the course of active lesion of postprimary pulmonary TB which affects surrounding structures, for example, traction or impaction of bronchus, bronchioles, and their branches due to recurrent reactivation. Similar to the pathogenesis of cavity formation, nodules, or tuberculoma which do not recover will become cavity contain new pneumonia focus.[4,7,11,13]
There was no significant difference in morphology of nonactive pulmonary lesion between MDR-TB and DS-TB. For example, fibrosis in MDR-TB and DS-TB (23% vs. 14.8%) commonly shown in upper lobe of right lung, calcification (8.2% vs. 0%) most found in mid lobe of left lung, atelectasis (1.6% vs. 3.8%) in upper lobe of left lung, bulla (2.2% vs. 1,1%) most found in upper lobe of right lung, and hyper-aeration or emphysema (1.1% vs. 0%) in left lower lobe of left lung. Nonactive lesion in this study has shown the possibility of reactivation.[4,7,10] Fibrosis and calcification are also chronic processes leading to recovery.[3,4,11]
There were some abnormalities outside pulmonary parenchyma that significantly different between MDR-TB and DS-TB group. Those are left pulmonary effusion (19.7% vs. 2.2%), right pleural effusion (7.7% vs. 1.6%), right hilum elevation (19.1% vs. 2.2%), left hilum elevation (15.8% vs. 1.6%), left deviation of trachea (17.5% vs. 3.3%), right deviation of trachea (12% vs. 3.3%), right pleural thickening (12.6% vs. 0.5%), and left pleural thickening (9.8% vs. 0%). Pleural effusion found in this study is also accompanied by an active lesion in pulmonary parenchyma, which similar result already is shown from the previous study in Persahabatan Hospital. Hilum elevation, tracheal deviation, and pleural thickening can occur as result of fibrosis in pulmonary parenchyma and pleura. These pleural thickening usually are the results of previous pleural effusion.[3,4,7,10,14,15]
The limitations of this study are the using of manual medical record and retrospective data. Therefore, many patients being excluded as their data were incomplete.
CONCLUSIONS
In terms of lesion size, MDR-TB group have a majority of patients with large lesions in their chest X-ray, meanwhile, DS-TB group have a dominant small-medium lesion. In terms of morphology, infiltrate and ground-glass opacity were more dominant in DS-TB group, whereas consolidation, cavity, fibrosis, bronchiectasis, calcification, node, atelectasis, bullae, emphysema, and other nonlung parenchymal findings, were more dominant in MDR-TB.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.World Health Organization. Global Tuberculosis Report 2014. USA: World Health Organization; 2014. pp. 1–147. [Google Scholar]
- 2.Center for Tuberculosis Information and Data. Ministry of Health Indonesia. 2015 [Google Scholar]
- 3.Icksan AG, Maryastuti M. Characteristics of chest X-ray lesion in smear-negative TB patient with culture-positive vs. culture-negative in the Persahabatan Hospital, Jakarta. Bul Ilmiah Radiol. 2012;2:80–90. [Indonesian Society of Radiology chapter Yogyakarta and Department of Radiology, University of Gajah Mada Faculty of Medicine, Yogyakarta] [Google Scholar]
- 4.Icksan AG. Doctoral Dissertation of the PhD in Clinical Medicine. Yogyakarta: University of Gajah Mada Faculty of Medicine; 2014. The Accuracy of CT Scan without Contrast Scoring System in the Diagnosis of Adult Pulmonary TB; pp. 1–156. [Google Scholar]
- 5.Technical Guidelines for Multi-drug Resistant Tuberculosis Holistic Control. Directorate General for Disease and Environmental Health Control. Jakarta: Ministry of Health Indonesia; 2014. Technical Guidelines for Multi-drug Resistant Tuberculosis Holistic Control; pp. 1–111. [Google Scholar]
- 6.Reviono, Harsini IJ, Aphridasari J, Sutanto YS. Comparisons of clinical, radiological and smear conversion of multi-drug resistant patients with diabetes and without diabetes at the Dr. Moewardi Hospital, Solo. J Respirol Indones. 2013;2:103–9. [Google Scholar]
- 7.Deesuwan P, Autravisittikul O, Girapongsa L. Chest radiographic findings of multidrug resistant pulmonary tuberculosis in comparisons to drug-sensitive pulmonary tuberculosis in non-HIV patient. Region 4-5 Med J. 2015;34:66–78. [Google Scholar]
- 8.Aditama TY. Directorate General for Disease and Environmental Health Control. Jakarta: Ministry of Health Indonesia; 2011. National Action Plan of Programmatic Management Drug Resistance Tuberculosis Control Indonesia 2011-2014; pp. 1–54. [Google Scholar]
- 9.Soetikno RD, Derry The conformity of chest X-ray and sputum spear findings in the treatment respond evaluation after 6-month course of treatment in Bandung, Indonesia. Majalah Kedokteran Bandung. 2011;43:140–5. [Google Scholar]
- 10.Cha J, Lee HY, Lee KS, Koh WJ, Kwon OJ, Yi CA, et al. Radiological findings of extensively drug-resistant pulmonary tuberculosis in non-AIDS adults: Comparisons with findings of multidrug-resistant and drug-sensitive tuberculosis. Korean J Radiol. 2009;10:207–16. doi: 10.3348/kjr.2009.10.3.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zahirifard S, Amiri MV, Karom MB, Mirsaeidi SM, Ehsanpour A, Masjedi MR. The radiological spectrum of pulmonary multidrug-resistant tuberculosis In HIV-negative patients. Iran J Radiol. 2013;1:161–6. [Google Scholar]
- 12.Ahuja SD, Ashkin D, Avendano M, Banerjee R, Bauer M, Bayona JN, et al. Multidrug resistant pulmonary tuberculosis treatment regimens and patient outcomes: An individual patient data meta-analysis of 9,153 patients. PLoS Med. 2012;9:e1001300. doi: 10.1371/journal.pmed.1001300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prasad R. Multidrug and extensively drug-resistant tuberculosis management: Evidences and controversies. Lung India. 2012;29:154–9. doi: 10.4103/0970-2113.95321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pirina P, Spada V, Arcadu A, Fois AG. Emerging clinical-radiological-pattern of pulmonary tuberculosis in immunocompetent patients. Eur Med J. 2014:1–6. [Google Scholar]
- 15.Thakker H, Shah JR. Multi-drug resistant pulmonary tuberculosis. Indian J Tuberc. 1998;45:131–9. [Google Scholar]


