ABSTRACT
Francisella tularensis subsp. holarctica is found in North America and much of Europe and causes the disease tularemia in humans and animals. An aquatic cycle has been described for this subspecies, which has caused waterborne outbreaks of tularemia in at least 10 countries. In this study, we sought to identify the mechanosensitive channel(s) required for the bacterium to survive the transition from mammalian hosts to freshwater, which is likely essential for the transmission of the bacterium between susceptible hosts. A single 165-amino-acid MscS-type mechanosensitive channel (FtMscS) was found to protect F. tularensis subsp. holarctica from hypoosmotic shock, despite lacking much of the cytoplasmic vestibule domain found in well-characterized MscS proteins from other organisms. The deletion of this channel did not affect virulence within the mammalian host; however, FtMscS was required to survive the transition from the host niche to freshwater. The deletion of FtMscS did not alter the sensitivity of F. tularensis subsp. holarctica to detergents, H2O2, or antibiotics, suggesting that the role of FtMscS is specific to protection from hypoosmotic shock. The deletion of FtMscS also led to a reduced average cell size without altering gross cell morphology. The mechanosensitive channel identified and characterized in this study likely contributes to the transmission of tularemia between hosts by allowing the bacterium to survive the transition from mammalian hosts to freshwater.
IMPORTANCE The contamination of freshwater by Francisella tularensis subsp. holarctica has resulted in a number of outbreaks of tularemia. Invariably, the contamination originates from the carcasses or excreta of infected animals and thus involves an abrupt osmotic downshock as the bacteria enter freshwater. How F. tularensis survives this drastic change in osmolarity has not been clear, but here we report that a single mechanosensitive channel protects the bacterium from osmotic downshock. This channel is functional despite lacking much of the cytoplasmic vestibule domain that is present in better-studied organisms such as Escherichia coli; this report builds on previous studies that have suggested that parts of this domain are dispensable for downshock protection. These findings extend our understanding of the aquatic cycle and ecological persistence of F. tularensis, with further implications for mechanosensitive channel biology.
KEYWORDS: Francisella tularensis, adaptation to water, mechanosensitive channel, osmotic stress
INTRODUCTION
Francisella tularensis is a Gram-negative bacterium responsible for the disease tularemia in humans and a wide range of animal species. Two subspecies of F. tularensis are of clinical significance for humans, namely, subsp. tularensis and subsp. holarctica (1). F. tularensis subsp. tularensis is considered more virulent and is primarily confined to Northern America. On the other hand, F. tularensis subsp. holarctica is broadly distributed throughout the Northern Hemisphere and has also been found in Australia (2). The manifestations of tularemia are varied depending upon the route of exposure. The ulceroglandular and glandular forms of tularemia are more frequent and are associated with exposure via arthropod bites or direct contact with infected animals, leading to localized lymphadenopathy with or without the formation of an ulcer at the inoculation site (1, 3, 4). Another common manifestation is oropharyngeal tularemia, where the ingestion of contaminated water leads to pharyngitis and swelling of the cervical lymph nodes (1). Rare presentations include oculoglandular tularemia, involving conjunctivitis resulting from inoculation of the eye, as well as typhoidal and pneumonic tularemia, which are both severe systemic diseases resulting from the inhalation of F. tularensis (pneumonic) or with no obvious route of exposure (typhoidal) (3).
Tularemia is considered a zoonotic disease that is rarely if ever transmitted by human-to-human contact (3). Hence, understanding how the bacterium persists and spreads in the environment is important. While long-term reservoirs and transmission cycles of F. tularensis are not well understood (5), the role of freshwater is of particular interest in the ecology of the broadly distributed F. tularensis subsp. holarctica, for which an aquatic cycle has been described (1). Many large outbreaks of tularemia are of the oropharyngeal form and are linked to the direct ingestion of water contaminated with F. tularensis subsp. holarctica. Outbreaks of tularemia from contaminated drinking water have been reported in at least 10 countries, totaling thousands of cases. Such outbreaks have been reported in Turkey (6–8), Sweden (9), Germany (10), Norway (11–13), Russia (14, 15), Bulgaria (16, 17), Kosovo (18, 19), the Czech Republic (20), Italy (21, 22), and the Republic of Georgia (23). Isolated cases of tularemia associated with infection from freshwater have also been described in France (24, 25) and the United States (26). In many of these cases, F. tularensis was detected by PCR (10–13, 20) or was cultured (8, 9, 15–17, 23, 26) from water from the affected area.
As the presence of viable F. tularensis subsp. holarctica in freshwater is directly responsible for many naturally occurring cases of oropharyngeal tularemia, it is important to understand how the bacterium adapts and survives in water. F. tularensis subsp. holarctica has been shown to survive in otherwise sterile freshwater for 7 to 40 days (27, 28). Persistence may be enhanced by the presence of amoebae or ciliates (29, 30), but the bacterium is not able to persist in freshwater indefinitely (27, 28) and is often only seasonally recovered from natural bodies of water (7, 31). This suggests that F. tularensis is introduced to bodies of water shortly before outbreaks, and indeed, almost all cases of water contamination are attributed to the carcasses or excreta of infected animals, including hares, rodents, voles, lemmings, muskrats, and beavers (6–8, 10–12, 16, 17, 19, 22, 26, 31–33). The shift from an animal to a freshwater niche involves an abrupt decrease in extracellular osmolarity, producing a hypoosmotic shock (or osmotic “downshock”).
Downshock results in a rapid influx of water into the cytoplasm, increasing tension on the membrane and potentially leading to lysis of the cell (34). To prevent this outcome, bacteria rely on mechanosensitive channels of small (MscS) and large (MscL) conductances, which open in response to the physical stretch of the membrane and jettison osmolytes (35). By doing so, mechanosensitive channels relieve pressure, restore isotonicity, and enable survival from hypoosmotic shock (36). This is the best-established function of mechanosensitive channels; however, the broader MscS-type protein family is structurally and functionally diverse (34, 37). Members of the family share highly conserved cores but display a broad array of N- and C-terminal modifications (34, 38, 39). The net result is that many bacteria possess multiple genes that code for MscS-family proteins (34, 37), but some of these have lost their role in protecting from abrupt osmotic downshock and gained other functions, for instance, for gating in response to cyclic nucleotide ligands (40).
In this study, we sought to identify the mechanosensitive channel(s) that protects F. tularensis subsp. holarctica from hypoosmotic shock, enabling it to survive the transition from a host to freshwater. We show that a single MscS-family channel in F. tularensis (FtMscS) is required for surviving the transition from mammalian cells to freshwater.
RESULTS
F. tularensis LVS mechanosensitive channels closely resemble those found in clinical and environmental strains.
We first sought to compare putative mechanosensitive channels in various F. tularensis subsp. holarctica strains to determine whether the live vaccine strain (LVS) was an accurate representation of other members of the subspecies. We compared the LVS to a human clinical isolate (FSC200), an isolate from a beaver (OSU18), and an isolate from drinking water (R13-38). Candidate mechanosensitive channel genes were identified using the conserved domain architecture retrieval tool (41). Our search yielded no hits when Escherichia coli MscL was used as a template but yielded four hits for MscS in each genome (FTL_1753, FTL_0945, FTL_1588, and FTL_1209 in the LVS). Two genes (FTL_1753 and FTL_0945) were identical in all four strains of F. tularensis subsp. holarctica (see Fig. S1 and S2 in the supplemental material). When we performed our initial bioinformatics comparison, FTL_1588 was annotated as a pseudogene in RefSeq (8-12-2015, annotation with NCBI software revision 3.0). Nevertheless, our analysis of FTL_1588 revealed that it was identical between the LVS and FSC200 and displayed a small N-terminal deletion in OSU18 (see Fig. S3). A gap in the whole-genome sequencing (WGS) assembly of R13-38 precluded this strain from comparison. The final hit (FTL_1209) was annotated as a pseudogene due to frameshifts in all four strains. Taken together, these data show that the live vaccine strain codes for mechanosensitive channels that accurately represent those found in clinical and environmental F. tularensis subsp. holarctica strains.
A single mechanosensitive channel protects F. tularensis subsp. holarctica from hypoosmotic shock.
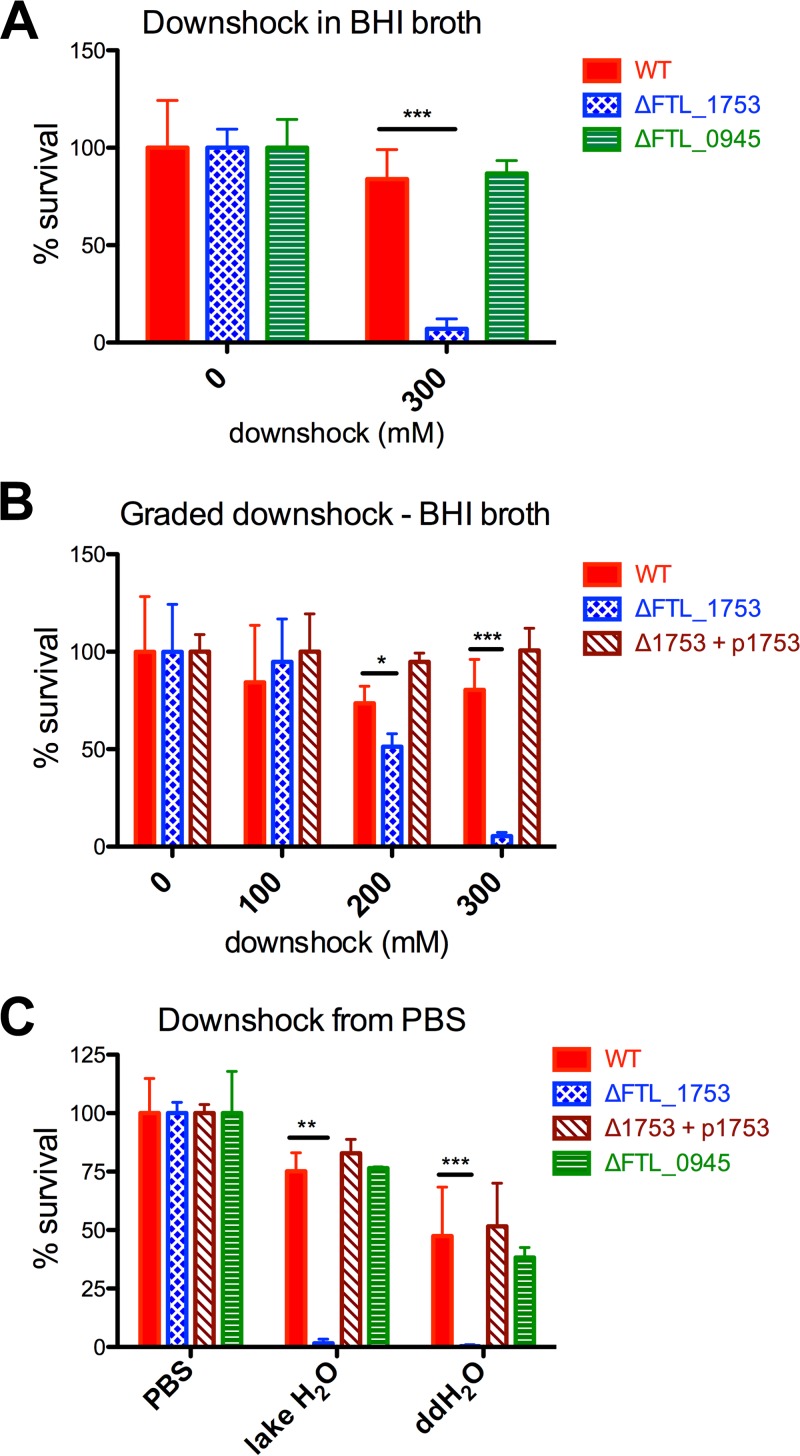
We next sought to determine which of the predicted mechanosensitive channels conferred protection from hypoosmotic shock/downshock. Because FTL_1753 and FTL_0945 were found in all four strains of F. tularensis subspecies holarctica, markerless in-frame deletions of these two genes were generated in the live vaccine strain (see Fig. S4). A hypoosmotic shock of 300 mM had little impact on the viability of the wild-type (WT) or ΔFTL_0945 strains but killed >90% of ΔFTL_1753 cells, indicating this gene is required for bacterial survival following osmotic downshock (Fig. 1A). To determine the magnitude of osmotic shock required to kill ΔFTL_1753 cells in medium, we measured their survival after graded downshocks of 100, 200, or 300 mM. The downshock of 300 mM killed the vast majority of ΔFTL_1753 cells as before; a 200 mM downshock caused a moderate but significant loss of viability, and a 100 mM downshock did not result in any loss of viability (Fig. 1B). These data for the ΔFTL_1753 strain are similar to prior observations for E. coli strains lacking two mechanosensitive channel genes, mscS and mscL (36). Trans-complementation with an expression plasmid for FTL_1753 completely restored the ability of ΔFTL_1753 cells to survive all three graded downshocks (Fig. 1B). Finally, we tested whether the observed phenotype was relevant to surviving the transition from a mammalian host to freshwater by equilibrating bacteria in phosphate-buffered saline (PBS) and then diluting them in double-distilled water (ddH2O) or filtered water obtained from a freshwater lake. While the ΔFTL_1753 strain was unable to survive in lake water and distilled water, the wild type, the ΔFTL_0945 strain, and the trans-complemented strain of ΔFTL_1753 were able to survive under both conditions (Fig. 1C). These data demonstrate that FTL_1753 encodes a functional mechanosensitive channel that is required by F. tularensis subsp. holarctica to survive hypoosmotic shock, including that encountered when the bacterium transitions from a mammalian host to freshwater. Here, we will refer to the product of FTL_1753 as FtMscS, consistent with the nomenclature used for MscS from other organisms (34, 42). In contrast, FTL_0945 appears to be not essential for osmotic downshock from a high-NaCl environment to a low-NaCl environment. However, our results do not rule out the possibilities that FTL_0945 may be involved in the adaptation of the bacteria to other osmotic shifts nor that the functions of FTL_0945 may be compensated for by FtMscS. Nevertheless, our data clearly indicate that FtMscS is essential and sufficient for F. tularensis subsp. holarctica to survive osmotic downshock.
FIG 1.
FTL_1753 is required for F. tularensis subsp. holarctica to survive hypoosmotic shock. (A and B) Survival data from downshock experiments performed in BHI broth. Bacteria were grown in BHI broth plus 300 mM NaCl, and then diluted in BHI broth plus 300, 200, 100, or 0 mM NaCl, producing hypoosmotic shocks of 0, 100, 200, and 300 mM, respectively. (C) Survival data for PBS-equilibrated bacteria diluted in water retrieved from a freshwater lake or double-distilled H2O. Statistical differences were determined by one-way analyses of variance (ANOVAs) with Dunnett's posttests. *, P < 0.05; **, P < 0.01; ***, P < 0.001. Each experiment was performed a minimum of three times.
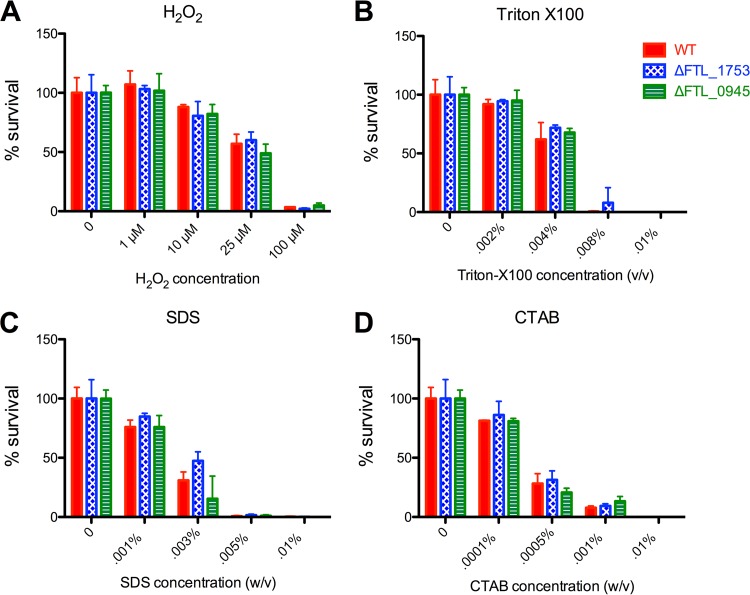
ΔFTL_1753 bacteria are not more sensitive to detergents, H2O2, or antibiotics.
To establish whether the deletion of FTL_1753 (FtMscS) or FTL_0945 resulted in a more generalized vulnerability to stressors, we tested these strains for sensitivity to three detergents and H2O2. The three detergents included an anionic detergent (SDS), a cationic detergent (cetyltrimethylammonium bromide [CTAB]), and a nonionic detergent (Triton X-100). In contrast to the large differences observed in the survival from downshock, all strains displayed similar sensitivity profiles to these stressors (Fig. 2). As mechanosensitive channels have been associated with antibiotic sensitivity in some contexts (43–45), we determined the MICs of 9 antibiotics for these strains. The knockout strains displayed sensitivities identical to that of the wild type, with the exception of the ΔFTL_1753 strain, which appeared slightly more resistant to kanamycin (see Table S1). These data support a specific role for FtMscS in survival from hypoosmotic shock rather than a more general role in the resistance to physical or chemical stressors.
FIG 2.
Sensitivity profiles of the wild-type, ΔFTL_1753, and ΔFTL_0945 strains to detergents and H2O2. Early-log-phase bacteria were exposed to the indicated concentrations of H2O2 (A), Triton X-100 (B), SDS (C), or CTAB (D) in medium for 1 h before dilution and plating to enumerate viable CFU. Representative results shown are from a minimum of four repeats. No statistically significant differences were found by one-way ANOVAs with Dunnett's posttests.
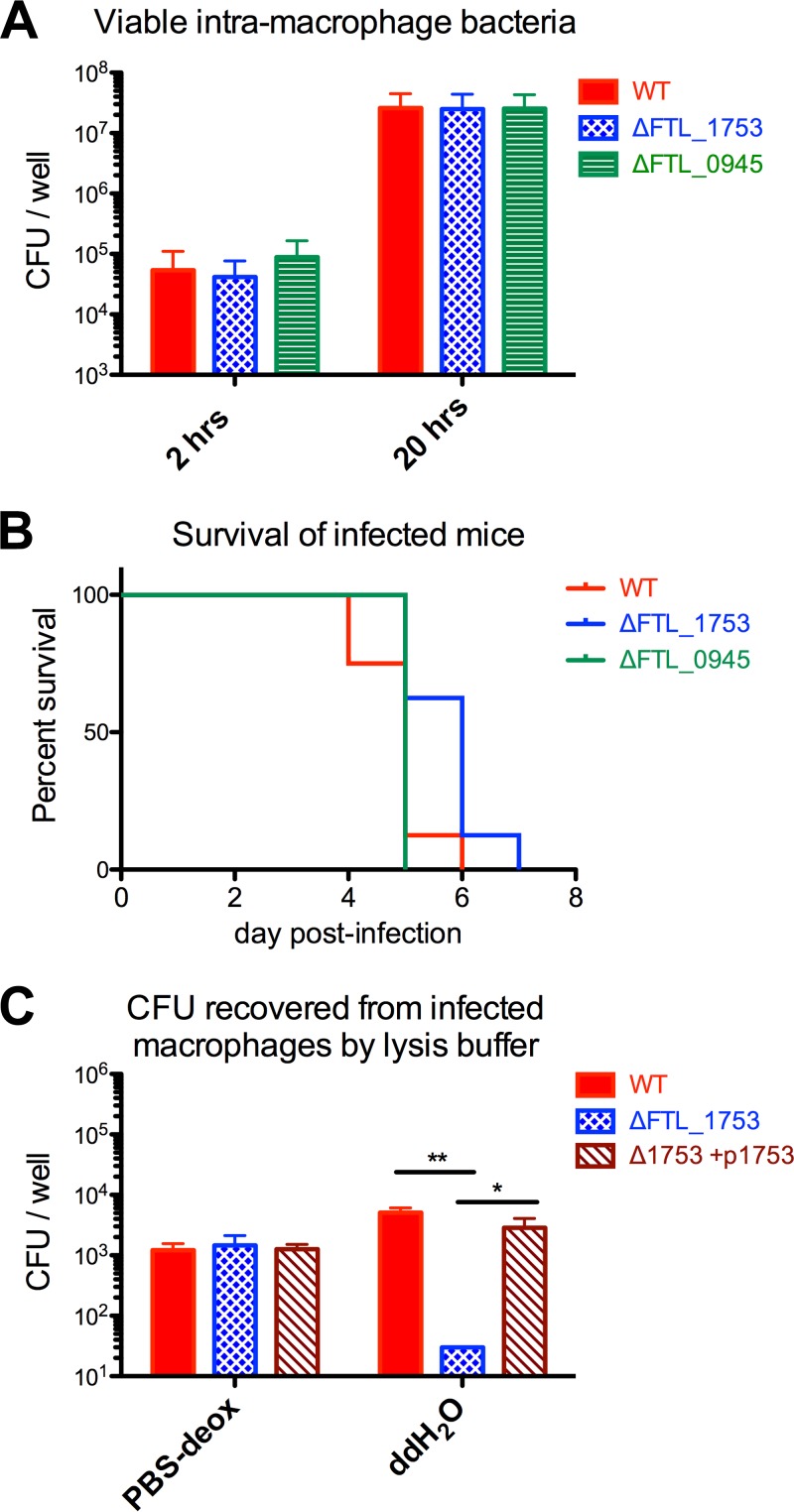
FtMscS does not contribute to virulence in the host niche but is required to survive the transition from that niche to freshwater.
We next sought to determine the roles of FtMscS and FTL_0945 in the context of the mammalian host niche. As F. tularensis is an intracellular pathogen that predominantly targets macrophages, we tested the ability of these strains to proliferate in macrophages using gentamicin protection assays. Similar amounts of intramacrophage growth were observed for all strains, suggesting that these genes do not contribute to F. tularensis replication within host cells (Fig. 3A). For the most part, mammalian tissues are maintained at similar osmolarities. However, some large osmotic gradients are found in mammals, most notably in the kidneys and liver. To determine whether FTL_1753 and FTL_0945 contribute to the pathogenesis of F. tularensis in the mammalian host, we tested strains lacking these genes in a mouse model of pneumonic tularemia. Mice infected with each of the strains displayed similar survival profiles, suggesting that these genes do not contribute to virulence within a host (Fig. 3B). Finally, we tested whether FtMscS is required for surviving the transition from a mammalian cell niche to freshwater using a modified gentamicin protection assay. After eliminating extracellular bacteria, infected macrophages were lysed either with detergent in PBS or with ddH2O. Similar numbers of viable bacteria were recovered using the PBS-detergent lysis buffer. In contrast, FtMscS was required for bacteria to survive macrophage lysis with ddH2O (Fig. 3C). Collectively, these data suggest that FtMscS is not required for virulence within the mammalian host niche but is required to survive the transition from this niche to freshwater.
FIG 3.
FTL_1753 (FtMscS) does not contribute to virulence in the host niche but is required to survive the transition from that niche to freshwater. (A) Viable CFU of indicated F. tularensis strains recovered from RAW 264.7 macrophages in a gentamicin protection assay at 2 and 20 h postinfection; pooled data from three repeats. (B) Survival curves of C57BL/6J mice (n = 8 per group) infected with 104 CFU of the indicated strains of F. tularensis LVS. (C) Viable CFU of indicated F. tularensis strains recovered from infected RAW 264.7 macrophages based on lysis buffer used. PBS-deox, 0.1% (wt/vol) sodium deoxycholate in PBS. One-way ANOVA with Tukey's posttest: *, P < 0.05; **, P < 0.01.
FtMscS lacks the C-terminal α-β domain and axial β-barrel found in prototypical MscS structures.
At 165 amino acids, FtMscS is notably smaller than the MscS protein found in E. coli (EcMscS; 286 amino acids [aa]) (46) and other species for which crystal structures have been determined (Helicobacter pylori, 274 aa; Thermoanaerobacter tengcongensis, 282 aa) (42, 47). The size difference suggested that FtMscS may lack structural components found in prototypical versions of the channel. The MscS crystal structures solved thus far are comprised of homoheptamers, with three transmembrane α-helices per subunit, and large hollow cytoplasmic “vestibules” (Fig. 4) (42, 46, 48). The vestibule consists of a middle β domain, followed by a C-terminal α-β domain, and finally an axial β-barrel. We used SWISS-MODEL (49) to compare the predicted structure of FtMscS to the known structure of EcMscS (46). FtMscS closely resembles the N-terminal portion of EcMscS, with three transmembrane helices and a cytoplasmic β domain (Fig. 4A). However, the C-terminal α-β domain and the axial β-barrel are missing from the FtMscS structure (Fig. 4). These data suggest that FtMscS lacks the C-terminal part of the cytoplasmic vestibule found in the most heavily studied MscS channels.
FIG 4.
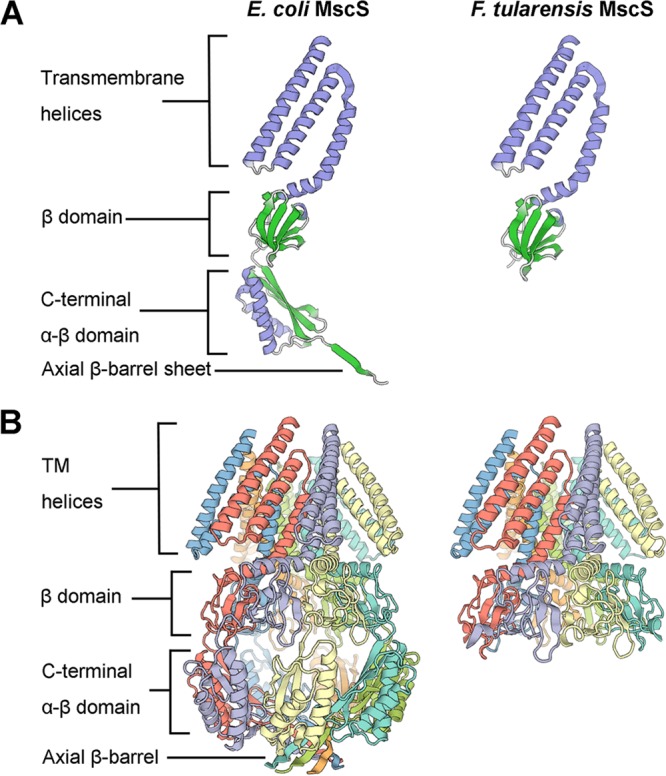
FtMscS lacks the C-terminal α-β domain and axial β-barrel found in prototypical MscS structures. (A) Structures of individual subunits of E. coli MscS (left) and FtMscS (right), colored according to secondary structure. (B) Structures of assembled homoheptamers of E. coli MscS (left) and FtMscS (right), colored by subunit. Images were generated using SWISS-MODEL (49) using PDB entry 2OAU as the structure template (63).
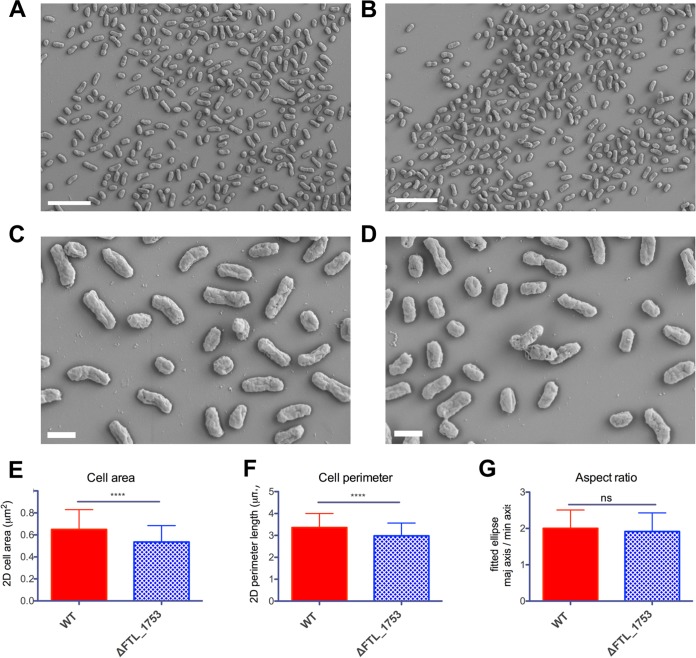
ΔFTL_1753 cells are smaller in size on average than the wild type.
As we observed that bacteria lacking FtMscS often formed smaller colonies than the wild type and a mutant form of EcMscS (lacking the C-terminal β-barrel) causes abnormal filamentation of E. coli cells (43), we used electron microscopy to determine whether cells lacking FtMscS displayed an aberrant morphology. ΔFTL_1753 cells were of a smaller average size than the wild type; two-dimensional (2D) outline traces revealed significantly smaller areas and perimeters than those of the wild type (Fig. 5A to F). Although smaller in size on average, ΔFTL_1753 cells had an overall morphology similar to that of the wild type, and there was no difference in the aspect ratio of fitted elliptical axes (Fig. 5G). These data show that the absence of FTL_1753 leads to smaller average bacterial cell sizes but does not lead to other gross morphological changes compared to the wild-type F. tularensis LVS.
FIG 5.
ΔFTL_1753 cells are smaller in size on average than the wild type. SEM images of wild-type (A) and ΔFTL_1753 (B) cells at ×3,000 magnification. Scale bars, 5 μm. SEM images of wild-type (C) and ΔFTL_1753 (D) cells at ×10,000 magnification. Scale bars, 1 μm. Cells (n > 180 per group) were traced in ImageJ and subjected to the indicated analyses. (E) Two-dimensional areas of cell traces. (F) Perimeter lengths of cell traces. (G) Aspect ratios of ellipses fitted to cell traces. ****, P < 0.0001 by a two-tailed unpaired t test. Negative-staining experiments with uranyl acetate and phosphotungstic acid followed by transmission electron microscopy (TEM) yielded similar results.
Comparative bioinformatics reveal conservation of FtMscS but heterogeneity in the other mechanosensitive channels encoded by F. tularensis subspecies.
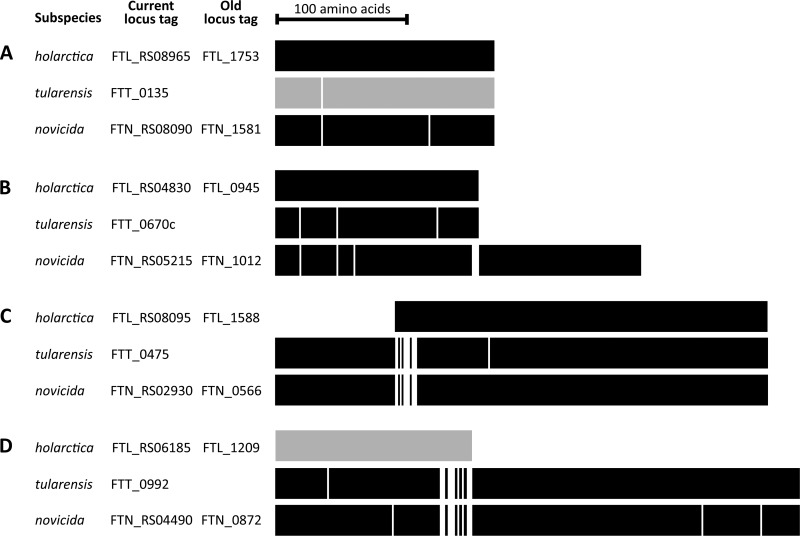
We chose to focus our study on the holarctica subspecies of F. tularensis, as this is the subspecies for which an aquatic cycle has been described and that is responsible for outbreaks of tularemia from contaminated water. Nonetheless, as there is great interest in the highly virulent F. tularensis subsp. tularensis and also subsp. novicida, we compared the loci predicted to code for mechanosensitive channels in these subspecies to the loci present in F. tularensis subsp. holarctica. Of the four loci, the one corresponding to FtMscS (FTL_1753) was the most highly conserved among the three subspecies, with only 1 to 2 amino acid substitutions between them (Fig. 6A; see also Fig. S5). The equivalent of FTL_1753 in the prototypical F. tularensis subsp. tularensis (strain SCHU S4) genome is currently annotated as a pseudogene. However, our data and analyses suggest this is erroneous and should be corrected as explained in Discussion. The remaining three loci display marked heterogeneity among the F. tularensis subspecies. In the set of genes equivalent to FTL_0945, the C-terminal 44% of the protein is lacking in both F. tularensis subsp. holarctica and F. tularensis subsp. tularensis relative to F. tularensis subsp. novicida (Fig. 6B; see also Fig. S6). In another set, the N-terminal ∼25% is absent in F. tularensis subsp. holarctica relative to the others (Fig. 6C; see also Fig. S7). In the final set, a frameshift has resulted in a premature stop codon and pseudogene annotation in F. tularensis subsp. holarctica (Fig. 6D; see also Fig. S8). Overall, these data suggest that (i) the mechanosensitive channel found to protect F. tularensis subsp. holarctica from hypoosmotic shock in this study is conserved among the F. tularensis subspecies and (ii) the other loci predicted to code for mechanosensitive channels exhibit considerable heterogeneity between the subspecies.
FIG 6.
Summary of comparative alignments of loci predicted to encode mechanosensitive channels in F. tularensis subspecies. White lines represent amino acid substitutions relative to F. tularensis subsp. holarctica except where no F. tularensis subsp. holarctica sequence is aligned. Gray shading signifies a current pseudogene annotation in RefSeq. For alignment detail, see Fig. S5 to S8 in the supplemental material.
DISCUSSION
The contamination of freshwater by F. tularensis subsp. holarctica is relevant to the bacterium's ecological persistence and transmission to hosts, including humans. F. tularensis can persist in freshwater for only a limited time (27, 28) and is seasonally recovered from natural bodies of water, suggesting recurrent cycles of contamination (7, 31). To survive an osmotic downshock, such as that encountered when going from a mammalian host to freshwater, bacteria rely on mechanosensitive channels which act as “pressure relief valves.” In this study, we have identified a mechanosensitive channel which protects F. tularensis subsp. holarctica from hypoosmotic shock (FtMscS, encoded by FTL_1753). The survival profile of the ΔFTL_1753 strain upon downshocks of 100 to 300 mM (Fig. 1B) closely resembles that of E. coli lacking both mscL and mscS (36) and is consistent with the notion that this is the only mechanosensitive channel that protects the subspecies from abrupt downshock. We demonstrated that the results of this study are applicable to clinical and environmental strains of F. tularensis subsp. holarctica (see Fig. S1 to S3 in the supplemental material) and that bacteria lacking FTL_1753 are unable to survive the transition from the osmolarity of the mammalian host to freshwater (Fig. 1C and 3C). Notably, FTL_1753 has been found to be upregulated within the intracellular growth niche (50); speculatively, this may be to increase the chances of survival in the event of a shift to a freshwater niche.
The presence of F. tularensis subsp. holarctica in freshwater has led to outbreaks of mostly oropharyngeal tularemia in at least 10 countries, as described earlier. Oropharyngeal tularemia is often initially misdiagnosed, and without appropriate treatment, it can become a chronic debilitating disease with the risk of serious complications (23). In addition, the aquatic cycle of F. tularensis subsp. holarctica can be implicated in many cases of ulceroglandular tularemia; water is thought to facilitate the spread of bacteria between animals and to mosquito vectors. In cases where humans develop ulceroglandular tularemia from mosquito bites, mosquitos may acquire the bacterium from water during their development. In Sweden, where most cases of tularemia are associated with mosquito bites (3, 51), a strong association has been found between infection and recreational areas near water (52). Furthermore, mosquito larvae reared in pond water from areas where the bacterium is endemic or that were experimentally exposed to F. tularensis during development have been shown to harbor F. tularensis as adults (53, 54). In cases where humans develop ulceroglandular tularemia from handling infected animals, F. tularensis can often be found in water within the animals' habitat (26, 33, 55); the presence of viable bacteria in the water is thought to contribute to the spread and persistence of infection among animal populations (26, 33). Thus, the mechanosensitive channel identified here is likely to be important to the overall ecological persistence of F. tularensis and its transmission to humans and other susceptible hosts.
In a bioinformatics analysis, we identified four loci predicted to contain mechanosensitive channel domains in each F. tularensis genome surveyed, including in F. tularensis subsp. tularensis and F. tularensis subsp. novicida (Fig. 6; see also Fig. S1 to S3 and S5 to S8). Notably, FtMscS was the most conserved among the subspecies, with only one amino acid substitution between F. tularensis subsp. holarctica and F. tularensis subsp. tularensis (Fig. 6A; see also Fig. S5). A predictive structural analysis indicates that FtMscS lacks much of the cytoplasmic vestibule found in prototypical versions of MscS with crystal structures (Fig. 4). Specifically, it lacks the C-terminal α-β domain and axial β-barrel, which are required for stable membrane incorporation of EcMscS (56). This has led to a “partial” annotation in the nonredundant protein record for FtMscS (WP_003017262.1) and a pseudogene annotation in the manually curated F. tularensis subsp. tularensis strain SCHU S4 genome (FTT_0135). Our data demonstrate that this gene does indeed code for an active mechanosensitive channel that protects from downshock. Our findings support previous reports that parts of the cytoplasmic vestibule of MscS are dispensable for downshock protection. First, EcMscS with a targeted deletion of the axial β-barrel retained the ability to protect from downshock (56). Second, the expression of MscS from the archaeon Nitrosopumilus maritimus, similar in structure to FtMscS, partially protected E. coli lacking other mechanosensitive channels from osmotic downshock (57). Functions beyond survival from downshock have been reported for the cytoplasmic vestibule, including roles in ion selectivity (42, 58), channel inactivation (59), and as a sensor for cytoplasmic crowding (60). How these functions are affected by the absence of the α-β domain and axial β-barrel remain interesting open questions to be addressed by future studies. In conclusion, we have identified a 165-amino-acid mechanosensitive channel that protects F. tularensis subsp. holarctica from downshock. This channel is required for the bacterium to survive the transition from mammalian hosts to freshwater and likely contributes to the ecological persistence of F. tularensis and transmission between hosts.
MATERIALS AND METHODS
Bioinformatics analysis of mechanosensitive channel domain-containing genes in F. tularensis.
The amino acid sequences of mechanosensitive channels (MscS and MscL) that protect E. coli from downshock (36) were retrieved from UniProtKB and input into the conserved domain architecture retrieval tool (CDART) (41). Results were filtered to the Francisella genus using the NCBI taxonomy tree to identify genes containing MscS or MscL domains in the strains of interest. Open reading frame (ORF) and gene sequences were retrieved from RefSeq genomes, compared using standard protein BLAST and Needleman-Wunsch global alignment, and visualized using Multiple Align Show (http://www.bioinformatics.org/sms/multi_align.html).
Bacterial strains and growth conditions.
The Francisella tularensis subsp. holarctica live vaccine strain (LVS) was obtained from Albany Medical College and was grown on MH chocolate agar (Mueller-Hinton II agar [BD BBL] supplemented with 1% hemoglobin [Remel] and 1% Isovitalex [BD BBL]). Liquid cultures of F. tularensis were routinely grown in modified brain heart infusion (BHI) broth (299070; BD BBL) at pH 6.4 to 6.8. Cloning procedures were performed using DH5α E. coli grown in LB broth (Miller formulation; BD Difco) or LB agar (Miller formulation; EMD Chemicals). Liquid cultures were incubated at 37°C in an orbital shaker operating at 200 rpm. Agar plates were incubated at 37°C under 5% CO2 for 48 to 72 h.
Primers, plasmids, and DNA manipulation.
All primers used in this study are shown in Table 1. The pMP812 sacB suicide vector (61) was used to generate targeted, markerless in-frame deletions of desired genes. Briefly, 700- to 900-bp PCR products flanking the sequence to be removed were amplified, digested, and ligated together and then reamplified as one unit and cloned into the multiple-cloning site (MCS) of pMP812. A complementation plasmid for FTL_1753 was generated by modifying the pKK214-GFP plasmid (29). First, the GroEL promoter and green fluorescent protein (GFP) gene were removed by digestion with XbaI and EcoRI. A multiple cloning site with four restriction sites was then added by annealed oligonucleotide cloning, with phosphorylated MCS4_1 and MCS4_2 oligonucleotides, to generate pKK214-MCS4. The bacterioferritin promoter and FTL_1753 were amplified, digested, and ligated together and then reamplified as one unit and cloned into pKK214-MCS4 with EcoRI. The resulting plasmid is referred to as p-1753. All oligonucleotides were synthesized by Integrated DNA Technologies or the Penn State Genomics Core Facility. All enzymes were from New England BioLabs. Vent DNA polymerase was used for cloning, and Taq DNA polymerase was used for screening. Genomic DNA was isolated from F. tularensis using an E.Z.N.A. bacterial DNA kit (Omega Bio-Tek) and plasmid DNA was isolated using an E.Z.N.A. plasmid DNA minikit I (Omega Bio-Tek).
TABLE 1.
Primers and plasmids used in this study
| Name | Sequence (5′→3′)a | Description |
|---|---|---|
| 1753_UP_F | TATTAAGCGGCCGCAATGTGTGAAATAACTTTTATACCACTTTTAGCAGAT | For upstream flank in FTL_1753 deletion construct |
| 1753_UP_R | GAAGCGGAATTCACTATTGCCTAATTGATCGAACATCGC | For upstream flank in FTL_1753 deletion construct |
| 1753_DOWN_F | TCCCCGGAATTCTAATGCAAAAACGTTACTTTCTTCAGATGAAATCC | For downstream flank in FTL_1753 deletion construct |
| 1753_DOWN_R | AATCTTGTCGACTGCTCACGGAACTCCTCATTTGAGTC | For downstream flank in FTL_1753 deletion construct |
| 0945_UP_F | TATTAAGTCGACCTTTCAGGTAAGACATCAGCAG | For upstream flank in FTL_0945 deletion construct |
| 0945_UP_R | TATTAAGGATCCAACGTTGATATTATGTTGAAAAGCATTTCATT | For upstream flank in FTL_0945 deletion construct |
| 0945_DOWN_F | TATTAAGGATCCTAGGATGTATGAAACTATTGAGCATGG | For downstream flank in FTL_0945 deletion construct |
| 0945_DOWN_R | ATTATGCGGCCGCTGGCATTATTGCTATTGATATATTCACTG | For downstream flank in FTL_0945 deletion construct |
| 0945_SCREEN_F | AGCAAATACCAAACAACGATAACTGCT | For screening for FTL_0945 deletion |
| 0945_SCREEN_R | TCTTTTAATTAATTGCTCAAGCTTTTGGGCA | For screening for FTL_0945 deletion |
| pBFR_F | GCTCGTCTAGAGATCCATACCCATGATGGTTACTATTG | Bacterioferritin promoter for plasmid complementation |
| pBFR_R | GCCGCGGGATCCTATTGTTACCTCCATTATTTAAAACTCTAATCA | Bacterioferritin promoter for plasmid complementation |
| 1753_COMP_F | TCATCAGGATCCATGTTCGATCAATTAGGCAATAGTGG | For FTL_1753 plasmid complementation |
| 1753_COMP_R | GCTCCGAATTCACCTGATAATAAAAAATAACGCTCATCACT | For FTL_1753 plasmid complementation |
| MCS4_1 | CTAGAGAATTCGGATCCG | Phosphorylated oligonucleotide for generation of pKK214-MCS4 via annealed oligonucleotide cloning |
| MCS4_2 | AATTCGGATCCGAATTCT | Phosphorylated oligonucleotide for generation of pKK214-MCS4 via annealed oligonucleotide cloning |
| pMP812 | sacB allelic exchange vector (61) | |
| pKK214 | Expression/complementation plasmid (29) |
Restriction sites are underlined.
Generation of in-frame deletions via allelic exchange and trans-complementation.
Markerless in-frame deletions of FTL_1753 (new locus tag FTL_RS08965) and FTL_0945 (new locus tag FTL_RS04830) were generated using the pMP812 sacB suicide vectors as previously described (61). PCR was used to screen for secondary recombinants with deletions, as outlined in Fig. S4 in the supplemental material. Trans-complementation of FTL_1753 was achieved by introducing the p-1753 plasmid into a confirmed ΔFTL_1753 strain. Electrocompetent F. tularensis cells were prepared as previously described (62), except that electroporations were done using 0.1-cm gap cuvettes (VWR) and a Bio-Rad Micropulser using Ec1 settings (1.8 kV, 10 μF, and 600 Ω).
Hypoosmotic shock assays.
For downshock experiments conducted in medium, single colonies of each strain were picked from MH chocolate agar plates and grown in BHI broth supplemented with 300 mM NaCl (EMD Chemicals). Mid-log-phase cultures were diluted (in BHI broth plus 300 mM NaCl) to a concentration of approximately 5 × 105 CFU/ml, and then 20 μl of each culture was added to 980 μl of BHI broth plus 300, 200, 100, or 0 mM NaCl to produce hypoosmotic shocks of 0, 100, 200, or 300 mM, respectively. The resulting cultures were vortexed and incubated for 1 h at room temperature before plating on MH chocolate agar with the same concentrations of NaCl added to prevent further osmotic shock. The percent survival was calculated by comparing viable counts from cultures subject to downshock to cultures maintained with 300 mM NaCl throughout the experiment. For downshock experiments from PBS to freshwater, a similar method was used, except that no NaCl was added to growth medium, and cells were equilibrated in PBS for 30 min before dilution into freshwater for 10 min. To test a source of water more naturally relevant than double-distilled H2O, water was retrieved from a freshwater lake in Pennsylvania and passed through a 0.2-μm filter.
H2O2 and detergent sensitivity assays.
Single colonies of each strain were picked from MH chocolate agar plates and grown in BHI broth. Early-log-phase cultures were diluted to a concentration of approximately 4 × 104 CFU/ml and added 1:1 to plain medium or medium with 2× the final desired concentration of detergent or H2O2. All dilutions and challenges were performed in identical media, such that the only variable would be the detergent or H2O2. These cultures were vortexed and incubated for 1 h at room temperature before being diluted 1/10 in BHI broth, and 100 μl was plated to enumerate viable CFU. The percent survival was calculated relative to the negative-control plates for the same strain (which yielded ∼200 CFU).
Determination of antibiotic MICs.
Twofold serial dilutions of each antibiotic were prepared and added to 96-well plates. Bacterial cultures were grown overnight, diluted to an optical density at 600 nm (OD600) of 0.050, and added 1:1 to plate wells containing medium and antibiotics in triplicates. Plates were incubated overnight (∼18 h), and bacterial growth was determined by measuring the optical density at 600 nm. The MIC was defined as the lowest final concentration of antibiotic for which cultures did not grow beyond an OD600 of 0.1.
Intramacrophage replication and macrophage-to-freshwater downshock assays.
RAW 264.7 macrophages were maintained in complete Dulbecco's modified Eagle medium (DMEM) (DMEM plus 10% fetal bovine serum [FBS], 1 mM sodium pyruvate, 2 mM l-glutamine, 10 mM HEPES, 1× nonessential amino acids). For intramacrophage replication assays, RAW 264.7 macrophages were seeded at a concentration of 3 × 105 cells per well in 24-well tissue culture plates (Greiner Bio-One) the evening before the assay. Macrophages were infected with early-log-phase BHI broth-grown F. tularensis cells at a multiplicity of infection of 100 bacteria per macrophage. Plates were centrifuged to facilitate synchronized infections (10 min, 300 × g, room temperature [RT]). After a 1-h incubation to allow for bacterial uptake, the medium was aspirated and replaced with medium containing 100 μg/ml gentamicin (Gibco) to kill extracellular bacteria. Following an additional 1-h incubation, the cells were washed twice with PBS. For wells designated for later time points, fresh medium (without antibiotic) was added. Cells in other wells were lysed by the addition of 100 μl/well of 0.1% (wt/vol) sodium deoxycholate (Sigma) in PBS. After lysis was observed, 900 μl of PBS was added to each well, and serial dilutions were plated on MH chocolate agar to determine the number of bacteria that had been taken up by macrophages. At 20 h postinfection, cells were similarly lysed and plated to determine the number of bacteria present. Macrophage-to-freshwater downshock assays were conducted in a similar fashion but with the following alterations: 5 × 104 cells were seeded per well to minimize the contribution of intracellular salt carryover during lysis, and cells were lysed at the 2-h time point only using 200 μl/well of either ddH2O or PBS plus 0.1% (wt/vol) sodium deoxycholate.
Mouse infections.
C57BL/6J mice were maintained under specific-pathogen-free conditions at the Pennsylvania State University animal care facilities. Isoflurane-anesthetized mice (n = 8 per group) were infected intranasally with 10,000 CFU of bacteria in 50 μl of PBS. Serial dilutions of the inoculum were plated on MH chocolate agar to confirm the correct dose was administered. Body weights were measured daily, and mice that lost 20% or more of their starting body weights were euthanized and counted as having succumbed to infection, per the Institutional Animal Care and Use Committee (IACUC) guidelines. Experimental groups were age and sex matched.
Predictive structural modeling.
The amino acid sequence of FTL_1753 was submitted to the SWISS-MODEL server (49), and a model was built using the structure of E. coli MscS as a template (PDB entry 2OAU [63]). The E. coli MscS protein sequence was similarly input to generate the corresponding images of E. coli MscS.
Electron microscopy.
Five-milliliter bacterial cultures were grown to an OD600 of approximately 0.5 and rinsed twice by centrifuging at 1,500 × g for 4 min and then resuspending in prewarmed medium. Cells were fixed by resuspending in 2% glutaraldehyde (Electron Microscopy Sciences) in PBS for 30 min at room temperature and then overnight at 4°C. The cell suspension was applied to poly-l-lysine-coated coverslips for 10 min at 4°C and subjected to critical point drying in the chamber of a Leica EM CPD300 (Leica Microsystems, Buffalo Grove, IL) critical point dryer using an automatic program. The coverslips were then mounted onto double-sided carbon tape on a single-pin aluminum scanning electron microscopy (SEM) stab (Ted Pella, Redding, CA) and sputter coated with iridium on a rotation stage of a Leica ACE600 (Leica Microsystems, Buffalo Grove, IL). The bacterial samples were examined and imaged in a Zeiss Sigma FE-SEM instrument (Carl Zeiss Microscopy, Thornwood, NY) at 2 kV. Cell two-dimensional (2D) areas, perimeter lengths, and the aspect ratios of fitted ellipses were determined using ImageJ v1.50i (64).
Statistics.
Statistical differences were determined as indicated in the figure legends using GraphPad Prism 5.0.
Ethics statement.
All animal experiments were carried out by following recommendations and approval from the Pennsylvania State University Animal Care and Use Committee (protocol 46070) with great care taken to minimize the suffering of animals.
Supplementary Material
ACKNOWLEDGMENTS
We thank Martin Pavelka, University of Rochester, for providing the pMP812 plasmid and Karl Klose, University of Texas at San Antonio, for providing the pKK214-GFP plasmid. We also thank The Huck Institutes of the Life Sciences for the facilities and technical support.
This study was supported by a T32 training grant AI 074551 (NIAID/NIH) to D.R.W. and AI077917 (NIAID/NIH), AES4605 (USDA), and startup funds from Penn State University and The Huck Institutes of the Life Sciences to G.S.K.
The funders had no role in the study design, data collection and interpretation, or the decision to submit the work for publication.
Footnotes
Supplemental material for this article may be found at https://doi.org/10.1128/AEM.02203-17.
REFERENCES
- 1.Maurin M, Gyuranecz M. 2016. Tularaemia: clinical aspects in Europe. Lancet Infect Dis 16:113–124. doi: 10.1016/S1473-3099(15)00355-2. [DOI] [PubMed] [Google Scholar]
- 2.Jackson J, McGregor A, Cooley L, Ng J, Brown M, Ong CW, Darcy C, Sintchenko V. 2012. Francisella tularensis subspecies holarctica, Tasmania, Australia, 2011. Emerg Infect Dis 18:1484–1486. doi: 10.3201/eid1809.111856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sjöstedt A. 2007. Tularemia: history, epidemiology, pathogen physiology, and clinical manifestations. Ann N Y Acad Sci 1105:1–29. doi: 10.1196/annals.1409.009. [DOI] [PubMed] [Google Scholar]
- 4.Jones CL, Napier BA, Sampson TR, Llewellyn AC, Schroeder MR, Weiss DS. 2012. Subversion of host recognition and defense systems by Francisella spp. Microbiol Mol Biol Rev 76:383–404. doi: 10.1128/MMBR.05027-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tärnvik A, Priebe H-S, Grunow R. 2004. Tularaemia in Europe: an epidemiological overview. Scand J Infect Dis 36:350–355. doi: 10.1080/00365540410020442. [DOI] [PubMed] [Google Scholar]
- 6.Aktas D, Celebi B, Isik ME, Tutus C, Ozturk H, Temel F, Kizilaslan M, Zhu B-P. 2015. Oropharyngeal tularemia outbreak associated with drinking contaminated tap water, Turkey, July-September 2013. Emerg Infect Dis 21:2194–2196. doi: 10.3201/eid2112.142032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kilic S, Birdsell DN, Karagöz A, Çelebi B, Bakkaloglu Z, Arikan M, Sahl JW, Mitchell C, Rivera A, Maltinsky S, Keim P, Üstek D, Durmaz R, Wagner DM. 2015. Water as source of Francisella tularensis infection in humans, Turkey. Emerg Infect Dis 21:2213–2216. doi: 10.3201/eid2112.150634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Karadenizli A, Forsman M, Şimşek H, Taner M, Öhrman C, Myrtennäs K, Lärkeryd A, Johansson A, Özdemir L, Sjödin A. 2015. Genomic analyses of Francisella tularensis strains confirm disease transmission from drinking water sources, Turkey, 2008, 2009 and 2012. Euro Surveill 20:21136. doi: 10.2807/1560-7917.ES2015.20.21.21136. [DOI] [PubMed] [Google Scholar]
- 9.Alm E, Advani A, Bråve A, Wahab T. 2015. Draft genome sequence of strain R13-38 from a Francisella tularensis outbreak in Sweden. Genome Announc 3:e01517-14. doi: 10.1128/genomeA.01517-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaysser P, Seibold E, Mätz-Rensing K, Pfeffer M, Essbauer S, Splettstoesser WD. 2008. Re-emergence of tularemia in Germany: presence of Francisella tularensis in different rodent species in endemic areas. BMC Infect Dis 8:157. doi: 10.1186/1471-2334-8-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Larssen KW, Afset JE, Heier BT, Krogh T, Handeland K, Vikøren T, Bergh K. 2011. Outbreak of tularaemia in central Norway, January to March 2011. Euro Surveill 16:19828. doi: 10.2807/ese.16.13.19828-en. [DOI] [PubMed] [Google Scholar]
- 12.Brantsaeter AB, Krogh T, Radtke A, Nygard K. 2007. Tularaemia outbreak in northern Norway. Euro Surveill 12:E070329.2. [DOI] [PubMed] [Google Scholar]
- 13.Berdal BP, Mehl R, Haaheim H, Løksa M, Grunow R, Burans J, Morgan C, Meyer H. 2000. Field detection of Francisella tularensis. Scand J Infect Dis 32:287–291. doi: 10.1080/00365540050165938. [DOI] [PubMed] [Google Scholar]
- 14.Rogutskiĭ SV, Khramtsov MM, Avchinikov AV, Gar'kavaia OI, Larchenkova NV, Golovanov AM, Parfenova TA, Rudkovskaia LB. 1997. An epidemiological investigation of a tularemia outbreak in Smolensk Province. Zh Mikrobiol Epidemiol Immunobiol 2:33–37. (In Russian.) [PubMed] [Google Scholar]
- 15.Karpoff SP, Antonoff NI. 1936. The spread of tularemia through water, as a new factor in its epidemiology. J Bacteriol 32:243–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kantardjiev T, Ivanov I, Velinov T, Padeshki P, Popov B, Nenova R, Mincheff M. 2006. Tularemia outbreak, Bulgaria, 1997-2005. Emerg Infect Dis 12:678–680. doi: 10.3201/eid1204.050709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Christova I, Velinov T, Kantardjiev T, Galev A. 2004. Tularaemia outbreak in Bulgaria. Scand J Infect Dis 36:785–789. doi: 10.1080/00365540410021199. [DOI] [PubMed] [Google Scholar]
- 18.Grunow R, Kalaveshi A, Kühn A, Mulliqi-Osmani G, Ramadani N. 2012. Surveillance of tularaemia in Kosovo, 2001 to 2010. Euro Surveill 17:20217. doi: 10.2807/ese.17.28.20217-en. [DOI] [PubMed] [Google Scholar]
- 19.Reintjes R, Dedushaj I, Gjini A, Jorgensen TR, Cotter B, Lieftucht A, D'Ancona F, Dennis DT, Kosoy MA, Mulliqi-Osmani G, Grunow R, Kalaveshi A, Gashi L, Humolli I. 2002. Tularemia outbreak investigation in Kosovo: case control and environmental studies. Emerg Infect Dis 8:69–73. doi: 10.3201/eid0801.010131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pazdiora P, Morávková I, Nocarová D, Velkoborská M, Valecková K. 2002. A water-borne epidemic of tularemia in Chlumcany. Epidemiol Mikrobiol Imunol 51:23–25. (In Czech.) [PubMed] [Google Scholar]
- 21.Mignani E, Palmieri F, Fontana M, Marigo S. 1988. Italian epidemic of waterborne tularaemia. Lancet ii:1423. [DOI] [PubMed] [Google Scholar]
- 22.Greco D, Allegrini G, Tizzi T, Ninu E, Lamanna A, Luzi S. 1987. A waterborne tularemia outbreak. Eur J Epidemiol 3:35–38. doi: 10.1007/BF00145070. [DOI] [PubMed] [Google Scholar]
- 23.Chitadze N, Kuchuloria T, Clark DV, Tsertsvadze E, Chokheli M, Tsertsvadze N, Trapaidze N, Lane A, Bakanidze L, Tsanava S, Hepburn MJ, Imnadze P. 2009. Water-borne outbreak of oropharyngeal and glandular tularemia in Georgia: investigation and follow-up. Infection 37:514–521. doi: 10.1007/s15010-009-8193-5. [DOI] [PubMed] [Google Scholar]
- 24.Guerpillon B, Boibieux A, Guenne C, Ploton C, Ferry T, Maurin M, Forestier E, Dauwalder O, Manipoud P, Ltaïef-Boudrigua A, Gürkov R, Vandenesch F, Bouchiat C. 2016. Keep an ear out for Francisella tularensis: otomastoiditis cases after canyoneering. Front Med (Lausanne) 3:9. doi: 10.3389/fmed.2016.00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ughetto E, Héry-Arnaud G, Cariou M-E, Pelloux I, Maurin M, Caillon J, Moreau P, Ygout J-F, Corvec S. 2015. An original case of Francisella tularensis subsp. holarctica bacteremia after a near-drowning accident. Infect Dis 47:588–590. doi: 10.3109/23744235.2015.1028099. [DOI] [PubMed] [Google Scholar]
- 26.Jellison WL, Epler DC, Kuhns E, Kohls GM. 1950. Tularemia in man from a domestic rural water supply. Public Health Rep 65:1219–1226. doi: 10.2307/4587477. [DOI] [PubMed] [Google Scholar]
- 27.Forsman M, Henningson EW, Larsson E, Johansson T, Sandström G. 2000. Francisella tularensis does not manifest virulence in viable but non-culturable state. FEMS Microbiol Ecol 31:217–224. doi: 10.1111/j.1574-6941.2000.tb00686.x. [DOI] [PubMed] [Google Scholar]
- 28.Berrada ZL, Telford SR III. 2011. Survival of Francisella tularensis type A in brackish-water. Arch Microbiol 193:223–226. doi: 10.1007/s00203-010-0655-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abd H, Johansson T, Golovliov I, Sandström G, Forsman M. 2003. Survival and growth of Francisella tularensis in Acanthamoeba castellanii. Appl Environ Microbiol 69:600–606. doi: 10.1128/AEM.69.1.600-606.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thelaus J, Andersson A, Mathisen P, Forslund A-L, Noppa L, Forsman M. 2009. Influence of nutrient status and grazing pressure on the fate of Francisella tularensis in lake water. FEMS Microbiol Ecol 67:69–80. doi: 10.1111/j.1574-6941.2008.00612.x. [DOI] [PubMed] [Google Scholar]
- 31.Schulze C, Heuner K, Myrtennäs K, Karlsson E, Jacob D, Kutzer P, Große K, Forsman M, Grunow R. 2016. High and novel genetic diversity of Francisella tularensis in Germany and indication of environmental persistence. Epidemiol Infect 144:3025–3036. doi: 10.1017/S0950268816001175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ul'ianova NI, Bessonova MA, Panasik LN, Svimonishvili VN, Grishina LS. 1982. Results of prolonged study of flood plain-swamp endemic foci of tularemia, and its prophylaxis in the Leningrad Region. Zh Mikrobiol Epidemiol Immunobiol 2:104–107. (In Russian.) [PubMed] [Google Scholar]
- 33.Young LS, Bickness DS, Archer BG, Clinton JM, Leavens LJ, Feeley JC, Brachman PS. 1969. Tularemia epidemia: Vermont, 1968. Forty-seven cases linked to contact with muskrats. N Engl J Med 280:1253–1260. [DOI] [PubMed] [Google Scholar]
- 34.Wilson ME, Maksaev G, Haswell ES. 2013. MscS-like mechanosensitive channels in plants and microbes. Biochemistry 52:5708–5722. doi: 10.1021/bi400804z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kung C, Martinac B, Sukharev S. 2010. Mechanosensitive channels in microbes. Annu Rev Microbiol 64:313–329. doi: 10.1146/annurev.micro.112408.134106. [DOI] [PubMed] [Google Scholar]
- 36.Levina N, Tötemeyer S, Stokes NR, Louis P, Jones MA, Booth IR. 1999. Protection of Escherichia coli cells against extreme turgor by activation of MscS and MscL mechanosensitive channels: identification of genes required for MscS activity. EMBO J 18:1730–1737. doi: 10.1093/emboj/18.7.1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cox CD, Nakayama Y, Nomura T, Martinac B. 2015. The evolutionary ‘tinkering’ of MscS-like channels: generation of structural and functional diversity. Pflügers Arch 467:3–13. doi: 10.1007/s00424-014-1522-2. [DOI] [PubMed] [Google Scholar]
- 38.Malcolm HR, Maurer JA. 2012. The mechanosensitive channel of small conductance (MscS) superfamily: not just mechanosensitive channels anymore. Chembiochem 13:2037–2043. doi: 10.1002/cbic.201200410. [DOI] [PubMed] [Google Scholar]
- 39.Booth IR, Miller S, Müller A, Lehtovirta-Morley L. 2015. The evolution of bacterial mechanosensitive channels. Cell Calcium 57:140–150. doi: 10.1016/j.ceca.2014.12.011. [DOI] [PubMed] [Google Scholar]
- 40.Caldwell DB, Malcolm HR, Elmore DE, Maurer JA. 2010. Identification and experimental verification of a novel family of bacterial cyclic nucleotide-gated (bCNG) ion channels. Biochim Biophys Acta 1798:1750–1756. doi: 10.1016/j.bbamem.2010.06.001. [DOI] [PubMed] [Google Scholar]
- 41.Geer LY, Domrachev M, Lipman DJ, Bryant SH. 2002. CDART: protein homology by domain architecture. Genome Res 12:1619–1623. doi: 10.1101/gr.278202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang X, Wang J, Feng Y, Ge J, Li W, Sun W, Iscla I, Yu J, Blount P, Li Y, Yang M. 2012. Structure and molecular mechanism of an anion-selective mechanosensitive channel of small conductance. Proc Natl Acad Sci U S A 109:18180–18185. doi: 10.1073/pnas.1207977109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Koprowski P, Grajkowski W, Balcerzak M, Filipiuk I, Fabczak H, Kubalski A. 2015. Cytoplasmic domain of MscS interacts with cell division protein FtsZ: a possible non-channel function of the mechanosensitive channel in Escherichia coli. PLoS One 10:e0127029. doi: 10.1371/journal.pone.0127029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Iscla I, Wray R, Wei S, Posner B, Blount P. 2014. Streptomycin potency is dependent on MscL channel expression. Nat Commun 5:4891. doi: 10.1038/ncomms5891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jiafeng L, Fu X, Chang Z. 2015. Hypoionic shock treatment enables aminoglycosides antibiotics to eradicate bacterial persisters. Sci Rep 5:14247. doi: 10.1038/srep14247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bass RB, Strop P, Barclay M, Rees DC. 2002. Crystal structure of Escherichia coli MscS, a voltage-modulated and mechanosensitive channel. Science 298:1582–1587. doi: 10.1126/science.1077945. [DOI] [PubMed] [Google Scholar]
- 47.Lai JY, Poon YS, Kaiser JT, Rees DC. 2013. Open and shut: crystal structures of the dodecylmaltoside solubilized mechanosensitive channel of small conductance from Escherichia coli and Helicobacter pylori at 4.4 Å and 4.1 Å resolutions. Protein Sci 22:502–509. doi: 10.1002/pro.2222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang W, Black SS, Edwards MD, Miller S, Morrison EL, Bartlett W, Dong C, Naismith JH, Booth IR. 2008. The structure of an open form of an E. coli mechanosensitive channel at 3.45 Å resolution. Science 321:1179–1183. doi: 10.1126/science.1159262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Biasini M, Bienert S, Waterhouse A, Arnold K, Studer G, Schmidt T, Kiefer F, Gallo Cassarino T, Bertoni M, Bordoli L, Schwede T. 2014. SWISS-MODEL: modelling protein tertiary and quaternary structure using evolutionary information. Nucleic Acids Res 42:W252–W258. doi: 10.1093/nar/gku340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bent ZW, Brazel DM, Tran-Gyamfi MB, Hamblin RY, VanderNoot VA, Branda SS. 2013. Use of a capture-based pathogen transcript enrichment strategy for RNA-seq analysis of the Francisella tularensis LVS transcriptome during infection of murine macrophages. PLoS One 8:e77834. doi: 10.1371/journal.pone.0077834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Eliasson H, Lindbäck J, Nuorti P, Arneborn M, Giesecke J, Tegnell A. 2002. The 2000 tularemia outbreak: a case-control study of risk factors in disease-endemic and emergent areas, Sweden. Emerg Infect Dis 8:956–960. doi: 10.3201/eid0809.020051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Svensson K, Bäck E, Eliasson H, Berglund L, Granberg M, Karlsson L, Larsson P, Forsman M, Johansson A. 2009. Landscape epidemiology of tularemia outbreaks in Sweden. Emerg Infect Dis 15:1937–1947. doi: 10.3201/eid1512.090487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lundström JO, Andersson A-C, Bäckman S, Schäfer ML, Forsman M, Thelaus J. 2011. Transstadial transmission of Francisella tularensis holarctica in mosquitoes, Sweden. Emerg Infect Dis 17:794–799. doi: 10.3201/eid1705.100426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bäckman S, Näslund J, Forsman M, Thelaus J. 2015. Transmission of tularemia from a water source by transstadial maintenance in a mosquito vector. Sci Rep 5:7793. doi: 10.1038/srep07793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Anda P, Segura del Pozo J, Díaz García JM, Escudero R, García Peña FJ, López Velasco MC, Sellek RE, Jiménez Chillarón MR, Sánchez Serrano LP, Martínez Navarro JF. 2001. Waterborne outbreak of tularemia associated with crayfish fishing. Emerg Infect Dis 7(3 Suppl):575–582. doi: 10.3201/eid0707.017740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schumann U, Edwards MD, Li C, Booth IR. 2004. The conserved carboxy-terminus of the MscS mechanosensitive channel is not essential but increases stability and activity. FEBS Lett 572:233–237. doi: 10.1016/j.febslet.2004.07.045. [DOI] [PubMed] [Google Scholar]
- 57.Widderich N, Czech L, Elling FJ, Könneke M, Stöveken N, Pittelkow M, Riclea R, Dickschat JS, Heider J, Bremer E. 2016. Strangers in the archaeal world: osmostress-responsive biosynthesis of ectoine and hydroxyectoine by the marine thaumarchaeon Nitrosopumilus maritimus. Environ Microbiol 18:1227–1248. doi: 10.1111/1462-2920.13156. [DOI] [PubMed] [Google Scholar]
- 58.Cox CD, Nomura T, Ziegler CS, Campbell AK, Wann KT, Martinac B. 2013. Selectivity mechanism of the mechanosensitive channel MscS revealed by probing channel subconducting states. Nat Commun 4:2137. doi: 10.1038/ncomms3137. [DOI] [PubMed] [Google Scholar]
- 59.Nomura T, Sokabe M, Yoshimura K. 2008. Interaction between the cytoplasmic and transmembrane domains of the mechanosensitive channel MscS. Biophys J 94:1638–1645. doi: 10.1529/biophysj.107.114785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rowe I, Anishkin A, Kamaraju K, Yoshimura K, Sukharev S. 2014. The cytoplasmic cage domain of the mechanosensitive channel MscS is a sensor of macromolecular crowding. J Gen Physiol 143:543–557. doi: 10.1085/jgp.201311114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.LoVullo ED, Molins-Schneekloth CR, Schweizer HP, Pavelka MS. 2009. Single-copy chromosomal integration systems for Francisella tularensis. Microbiology 155:1152–1163. doi: 10.1099/mic.0.022491-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.LoVullo ED, Sherrill LA, Perez LL, Pavelka MS. 2006. Genetic tools for highly pathogenic Francisella tularensis subsp. tularensis. Microbiology 152:3425–3435. doi: 10.1099/mic.0.29121-0. [DOI] [PubMed] [Google Scholar]
- 63.Steinbacher S, Bass R, Strop P, Rees DC. 2007. Structures of the prokaryotic mechanosensitive channels MscL and MscS, p 1–24. In Simon S, Benos D (ed), Current topics in membranes. Academic Press, Cambridge, MA. [Google Scholar]
- 64.Schneider CA, Rasband WS, Eliceiri KW. 2012. NIH Image to ImageJ: 25 years of image analysis. Nat Methods 9:671–675. doi: 10.1038/nmeth.2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.