Abstract
Although inherited hematopoietic malignancies have been reported clinically since the early twentieth century, the molecular basis for these diseases has only recently begun to be elucidated. Growing utilization of next-generation sequencing technologies has facilitated the rapid discovery of an increasing number of recognizable heritable hematopoietic malignancy syndromes while also deepening the field’s understanding of the molecular mechanisms that underlie these syndromes. Because individuals with inherited hematopoietic malignancies continue to be underdiagnosed and are increasingly likely to be encountered in clinical practice, clinicians need to have a high index of suspicion and be aware of the described syndromes. Here, we present the methods we use to identify, test, and manage individuals and families suspected of having a hereditary myeloid malignancy syndrome. Finally, we address the areas of ongoing research in the field and encourage clinicians and researchers to contribute and collaborate.
Introduction
Astute clinicians have reported familial clustering of myelodysplastic syndrome (MDS) and acute leukemia (AL; MDS/AL) for decades.1 These physicians often described phenotypic features that are now known to be associated with specific genetically defined hereditary myeloid malignancy syndromes (HMMSs).2 Why, then, is the diagnosis of HMMS only now starting to be considered in the evaluation of the average adult patient with MDS/AL?
The reasons are likely several. Historically, the HMMSs, including inherited bone marrow (BM) failure syndromes (IBMFSs) like Fanconi anemia (FA), have often been part of a syndrome with features that are readily recognized in childhood.3 Thus, traditional hematology training focused on HMMS as mainly a pediatric issue. The lack of genetically defined adult-onset HMMS also limited the utility of recognizing a family history of MDS/AL for adults in most clinical scenarios. Furthermore, MDS/AL cases with usual onset in late adulthood seemed unlikely candidates for the discovery of novel hereditary cancer syndromes, which are expected to cause early-onset disease.4 Moreover, with MDS only incorporated into the National Cancer Institute’s Surveillance, Epidemiology, and End Results program in 2001 and limited literature on the yield of family cancer history in adult MDS/AL patients, the extent of clustering of adult MDS/AL cases has been underappreciated.5 These issues have led to a general resistance to the idea that inherited genetic factors contribute to a significant proportion of adult MDS/AL cases. This sentiment is changing as an increasing number of genetically defined HMMSs are discovered.
Familial platelet disorder (FPD) with associated myeloid malignancy (FPD/acute myeloid leukemia [AML]) due to inherited mutations in RUNX1 was the first HMMS to be genetically defined in 1999,6 followed by familial AML with CEBPA mutation in 2004.7 Expanding use of next-generation sequencing (NGS) contributed to the rapid discovery of 6 additional HMMSs: familial MDS/AML with GATA2 mutation,8,9 thrombocytopenia 2 (ANKRD26),10,11 myeloid neoplasms with germ line predisposition (ATG2B/GSKIP),12 familial MDS/AML with mutated DDX41,13-16 thrombocytopenia 5 (ETV6),17-19 and familial aplastic anemia (AA)/MDS with SRP72 mutation.20 Adult-onset presentations of IBMFSs such as autosomal-dominant telomere syndromes with familial MDS/AL presentation (TERC/TERT) have also been described.21-23 Furthermore, germ line mutations in genes traditionally thought of as solid tumor predisposition genes are increasingly identified in patients with hematopoietic malignancy (HM).24,25
Recognition of HMMSs in clinical care is imperative. First, a molecular diagnosis provides a precise explanation for the conditions present within an affected individual and family, which can help patients understand their specific disorder and avoid inappropriate treatments (eg, splenectomy for misdiagnosed immune thrombocytopenia [ITP] in HMMS featuring thrombocytopenia). Second, a genetic diagnosis can help avoid the use of hematopoietic stem cells (HSCs) from an asymptomatic HMMS mutation carrier.26-31 Finally, routine clinical care now requires knowledge of HMMSs. For example, the National Comprehensive Cancer Network (NCCN) recommends surveillance for HMMSs in patients at high risk for Li-Fraumeni syndrome,32 and clinicians ordering genetic testing of malignant cells (eg, CEBPA for AML prognosis) will encounter reports suggesting that an identified mutation may be germ line. Furthermore, the 2016 World Health Organization (WHO) classification of HMs incorporated a provisional diagnostic category for hereditary myeloid malignancies, such as AML with mutated RUNX1, prompting pathologists and clinicians to consider HMMSs when rendering diagnoses.33 Thus, clinicians will increasingly need to identify, diagnose, and manage individuals with HMMSs.
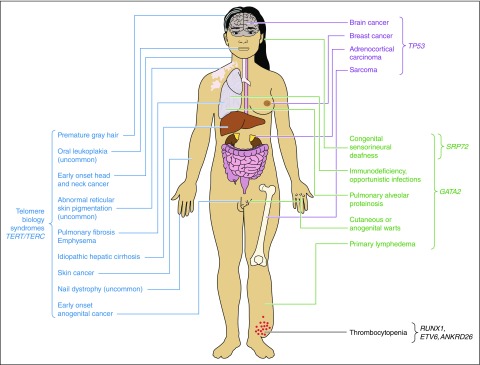
HMMSs encompass familial MDS/AL predisposition syndromes, IBMFSs, familial myeloproliferative neoplasms (MPNs), and, more broadly, traditional hereditary cancer predisposition syndromes. A review of each HMMS is beyond the scope of this article, but the features of each syndrome are summarized in Table 134,35 and Figure 136 and have been reviewed in detail elsewhere.37-40 In this review, we provide a practical outline for identifying and diagnosing HMMSs in hematology clinical care. We review the current evidence, or lack thereof, on how to care for individuals with known HMMS. Lastly, we outline areas of active investigation to detail the current state of the HMMS field and encourage clinicians and researchers to contribute and collaborate.
Table 1.
The known hereditary myeloid malignancy syndromes
| Class | Hematologic malignancy risk | Gene | Disorder | Hematologic phenotype | Other phenotype | Inheritance | OMIM no. | Key |
|---|---|---|---|---|---|---|---|---|
| Familial MDS/AL syndrome | MDS AML ALL NHL CML |
ANKRD26 | Thrombocytopenia 2 | Chronic thrombocytopenia with normal platelet size, easy bruising, increased plasma thrombopoietin, platelet dysfunction | NA | AD* | 188 000 | A |
| ETV6 | Thrombocytopenia 5 | Chronic thrombocytopenia with normal platelet size is present in nearly all mutation carriers, macrocytosis, easy bleeding/bruising | Esophageal dysmotility? Colon cancer? | AD | 616 216 | B | ||
| RUNX1 | FPD/AML | Mild to moderate chronic thrombocytopenia with normal platelet size, easy bleeding/bruising, epistaxis; platelet function may be abnormal on platelet aggregation studies | Eczema | AD | 601 399601 626 | C | ||
| DDX41 | Familial MDS/AML with mutated DDX41 | None until development of hematologic malignancy; MDS/AML often hypocellular with prominent erythroid dysplasia or erythroleukemia morphology | Autoimmune disorders? | AD | 153 550616 871 | D | ||
| CEBPA | Familial AML with CEBPA mutation | None until development of AML | NA | AD | 601 626 | E | ||
| GATA2 | Familial MDS/AML with GATA2 mutation | Mild cytopenias including chronic neutropenia, B-/NK-cell lymphopenia, monocytopenia are common | Anogenital or cutaneous warts, congenital sensorineural deafness, lymphedema, opportunistic infections (eg, atypical mycobacterial infections), pulmonary alveolar proteinosis immunodeficiency | AD | 614 038 | F | ||
| ATG2B/GSKIP | Myeloid neoplasms with germ line predisposition | Primary myelofibrosis, essential thrombocythemia | NA | AD | 601 626 | G | ||
| TERC/TERT | Telomere syndromes with familial MDS/AL presentation | Mild asymptomatic cytopenias, especially thrombocytopenia or macrocytosis, are common; if cytopenias are progressive or severe, AA or hematologic malignancy likely | Early-onset anogenital cancer, early onset head and neck cancer, esophageal stricture, hepatic cirrhosis, hepatopulmonary syndrome, osteoporosis, premature gray hair, pulmonary fibrosis or emphysema; lymphocyte subset telomere lengths <1st percentile for age. The classical triad of reticulated pigmentation, leukoplakia, and nail dystrophy less likely | AD, AR* | 601 626613 989614 742615 134 | H | ||
| SRP72 | Familial aplastic anemia/MDS with SRP72 mutation | None until development of MDS or aplastic anemia | Congenital sensorineural deafness | AD | 614 675 | I | ||
| IBMFSs | MDS AML ALL* Other* |
ACD CTC1 DKC1 NHP2 NOP10 PARN RTEL1 TERC TERT TINF2 WRAP53 |
Telomere syndromes | Cytopenias, macrocytosis, elevated hemoglobin F; if cytopenias are progressive or severe, AA or hematologic malignancy likely | Abnormal dentition, cerebellar hypoplasia, dental caries, developmental delay, early-onset head and neck cancer, esophageal stenosis, liver fibrosis, epiphora, intrauterine growth retardation, microcephaly, osteoporosis, premature gray hair, pulmonary fibrosis, testicular atrophy. The classical triad of reticulated pigmentation, leukoplakia, and nail dystrophy; lymphocyte subset telomere lengths <1st percentile for age | AD AR X-linked | 224 230268 130606 471608 833612 661613 987613 988613 990615 190616 353616 371616 373616 553 | J |
|
FANCA FANCB FANCC FANCD1/BRCA2 FANCD2 FANCE FANCF FANCG FANCI FANCJ FANCL FANCM FANCN FANCS/BRCA1 |
Fanconi anemia | Cytopenias, macrocytosis, elevated hemoglobin F; if cytopenias are progressive or severe, AA or hematologic malignancy likely | Anal atresia, absent kidney, cafe-au-lait spots, cleft palate, congenital heart defects, cryptorchidism, developmental delay, duplicated kidney, esophageal atresia, horseshoe kidney, hypergonadotrophic hypogonadism, kidney malformation, limb anomalies, microcephaly, nail dystrophy, radial ray anomalies, short neck, skin pigmentation abnormalities, small stature, strabismus, tracheoesophageal fistula, severe toxicity with cytotoxic exposures. Spontaneous and induced chromosomal instability | AR, X-linked | 227 645227 646227 650300 514600 901603 467605 724609 053609 054610 832614 082614 083 | K | ||
| Cancer predisposition syndromes | MDS AML ALL NHL HL MM |
TP53 | Li-Fraumeni syndrome | None until development of hematologic malignancy; 6% of tumors in individuals with Li-Fraumeni syndrome are hematologic malignancies; therapy-related leukemias possible34,35 | Adrenocortical carcinoma, brain cancer, breast cancer, choroid plexus carcinoma, colon cancer, lung carcinoma, sarcoma, any tumor possible | AD | 137 800151 623601 626 | L |
|
BRCA1 BRCA2 |
Hereditary breast and ovarian cancer syndrome | None until development of hematologic malignancy.34,35 Therapy-related leukemias possible | Breast cancer, ovarian cancer, pancreatic cancer, primary peritoneal carcinoma, prostate cancer, male breast cancer, melanoma | AD | 604 370612 555 | M | ||
|
EPCAM MLH1 MSH2 MSH6 PMS2 |
Lynch syndrome | None until development of hematologic malignancy | Colorectal cancer, endometrial cancer, gastric cancer, glioblastoma, hepatobiliary cancers, microsatellite instability of tumor cells, ovarian cancer, sebaceous adenomas, sebaceous carcinoma, sebaceous epitheliomas, small bowel cancer, transitional cell carcinoma; also cafe-au-lait lesions and early-onset hematologic malignancies or brain tumors in MMR deficiency | AD AR (MMR deficiency) | 114 500120 435158 320276 300609 310613 244614 337614 350 | N | ||
| Familial MPNs | CML AML |
ATG2B/GSKIP | Myeloid neoplasms with germ line predisposition | Primary myelofibrosis, essential thrombocythemia | NA | AD | 601 626 | O |
| RBBP6 | MPNs with germ line RBBP6 mutation | Primary myelofibrosis, essential thrombocythemia | Glioma | AD | 601 626 |
AD, autosomal dominant; AR, autosomal recessive; MMR, mismatch repair; NA, not applicable; NK, natural killer.
Indicates that association is less established and is an area of ongoing investigation.
Figure 1.
Physical manifestations of the known HMMSs. It is vital that the personal and family history include details regarding nonhematopoietic processes as HMMSs can present in a syndromic manner with multiple organ systems involved. Adapted from Churpek and Godley36 with permission.
Case 1
A 54-year-old woman presents to the emergency room with fever and petechiae. Her peripheral blood smear reveals a white blood cell count of 45.0 × 109/L with a blast count of 15.8 × 109. AML is diagnosed. An NGS panel sent for prognostication identifies 1 deleterious mutation in RUNX1 and 2 in TP53. How should this patient be evaluated for an HMMS?
How we screen for hereditary myeloid malignancy syndromes
We favor a stepwise, team-based screening approach. Hematologists in our practice gather a significant portion of the history needed to identify individuals with personal or family histories concerning for HMMSs during their usual histories and physical examinations. Our colleagues flag any patient with a suggestive history (Figure 2) and have a low threshold for referral to our HMMS genetics team for further evaluation. Patient-specific characteristics warranting referral include: personal or family history of longstanding cytopenias or organ-system manifestations consistent with known HMMS (Table 1; Figure 1), personal or family history of multiple HMs or other cancers, or the identification of a known or possibly deleterious mutation in an HMMS-predisposing gene on tumor testing.
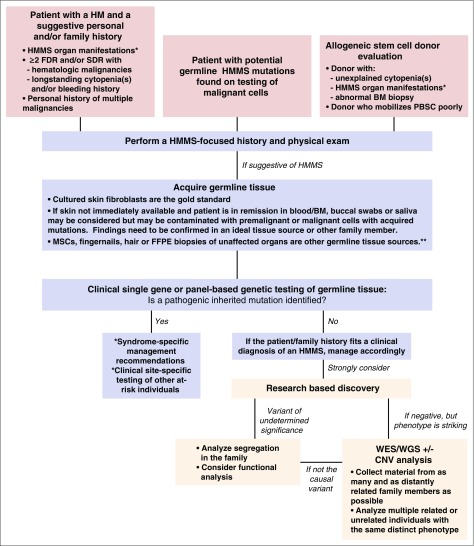
Figure 2.
The schema used to clinically screen patients for HMMSs based on their personal and family histories. This schema captures the general principles we use in our institution to evaluate all HM patients for HMMSs. *See Table 3. **These samples may not be accepted by some clinical laboratories. CNV, copy number variation; FDR, first-degree relatives; FFPE, formalin-fixed, paraffin-embedded; MSC, mesenchymal stem cell; PBSC, peripheral blood stem cell; SDR, second-degree relatives; WES, whole-exome sequencing; WGS, whole-genome sequencing.
Patient subgroups warranting special attention include:
Healthy HSC donors.
Inadvertent use of HSCs from donors carrying an HMMS germ line mutation may result in poor engraftment and/or donor-derived MDS/AL.26-31 Therefore, it is vital that all related and unrelated donors are screened for HMMSs.41 Further evaluation of the potential donor and/or recipient is warranted if a donor notes a personal or family history suggestive of an HMMS, has unexplained cytopenias, or mobilizes peripheral blood HSCs poorly.31
Patients with an HMMS gene mutation identified in their leukemia cells.
Molecular diagnostic testing is increasingly being used to analyze malignancies for mutations in genes, such as CEBPA, FLT3, and NPM1 in AML, to determine prognosis, guide clinical decision making, and inform therapeutic options.42-54 Whether analyzed by classic Sanger sequencing using a gene-by-gene approach or by NGS panels, mutations identified in some genes, like CEBPA, may represent pathogenic germ line mutations.55-57 The challenge is determining which patients with a potentially pathogenic mutation in an HMMS gene should have follow-up germ line genetic testing performed. How many of these mutations are germ line, and what are the clinical predictors that should prompt germ line analysis? The answers to these questions are not yet known but are being addressed on a research basis. For now, we recommend further evaluation using an HMMS-focused personal and family history for any patient with a somatic mutation in an HMMS-associated gene (Table 2). We perform germ line genetic testing if a pattern suggestive of an HMMS is identified and/or based on the specific gene mutated (see “Whom to test” below).
Table 2.
The University of Chicago Hereditary Hematopoietic Malignancies Screening Form
| Hereditary Hematologic Malignancies Screening Form | |
|---|---|
| Step 1 | |
| Draw the family pedigree using standard symbols | |
| Step 2 | |
| Use screening questions to guide workup (see Table 1 for specific syndromes corresponding to letter designations) | Consider: |
| Do you/does anyone in your family have chronic low blood cell counts, including low numbers of red blood cells (anemia), low platelet counts, (thrombocytopenia or ITP), low numbers of white blood cells (leukopenia, monocytopenia, lymphopenia)? | A, B, C, F, H, J, K |
| Has anyone required a transfusion for a low blood count? | |
| Did you/does anyone in your family bleed or bruise easily? | A, B, C |
| If yes, have they required transfusions for bleeding? | |
| Do you/does anyone in your family have or have had warts (genital, hands, feet, or any other site)? | F |
| If yes, where and for how many years? | |
| Do you/does anyone in your family get infections easily or severe or unusual types of infections? | F, J, K |
| If yes, how many infections and what type? (e.g., pneumonia, meningitis) and at what age(s)? | |
| Did they require hospitalization or antibiotics? | |
| Does anyone in the family have swelling of one limb larger than the others (also known as lymphedema)? | F |
| If yes, what limb and is there a known reason why that limb is swollen? | |
| Do you/does anyone in your family have deafness? | F, I, J |
| If yes, at what age did it occur and is there a known reason for why that person cannot hear? | |
| Do you/does anyone in your family have abnormal nails (e.g. misshapen or missing not due to injury)? | H, J, K |
| Did you/does anyone in your family get gray hair in their 20s or earlier? Whom and at what age? | H, J |
| Have you or anyone in your family had skin cancer or abnormal coloration of the skin, especially around the neck region? | H, J, K, N |
| Have you/anyone in your family had a specific skin problem called eczema? | C |
| Do you or anyone in your family have lung disease, including pulmonary fibrosis, IPF, or early onset emphysema? | H, J |
| Do you or anyone in your family have a lung disease called pulmonary alveolar proteinosis? | F |
| Do you/does anyone in your family have a liver disease called cirrhosis? | H, J |
| If yes, at what age and is there a known reason why you/they have cirrhosis (for example, heavy alcohol use)? | |
| Have you or other family members had other types of cancer, such as head and neck cancer? | H, J, K, L, M |
| Have you or other family members had other types of cancer, such as cervical or anal cancer? | H, J, K, L |
| Have you or other family members had other types of cancer, such as early onset breast cancer, sarcoma, or brain or colon cancers? | L, M, N |
| Step 3 | |
| Determine exposure history | |
| Do you smoke? If yes, how many packs per day? | |
| Do you drink alcohol? If yes, how many drinks per day? | |
| Have you been exposed to pesticides? If yes, for what career, what agents, and for how many years? | |
| Have you been exposed to radiation and/or chemotherapy? If yes, what drugs or type of radiation were you exposed to and for what reason? | |
| Have you been exposed to other chemicals such as benzene? If yes, what chemicals, why, and for how long? | |
IPF, idiopathic pulmonary fibrosis.
Upon referral to our inherited HM clinic, our HMMS-trained genetic counselors and physicians construct a formal 3-generation family pedigree noting the number of affected individuals, their relationships, ages at diagnosis, and specific diagnoses. We ask specific history questions (Table 2) and perform a focused physical examination to assess for the classic signs/symptoms of HMMSs, recognizing that many patients with HMMS lack the classic, most severe phenotypes. Obtaining accurate information about specific HM diagnoses, a history of mild cytopenias, or reasons for specific organ-system dysfunction, especially from family members, is challenging but critically important. Thus, we often assist in gathering laboratory records, pathology reports, and death certificates for confirmation. Finally, we assess for environmental factors or other exposures that may contribute to patient or family phenotypes.
Based on this evaluation, our team makes a formal recommendation to the referring clinician, who remains the primary hematologist directing the day-to-day hematologic care of the patient, regarding degree of suspicion for an HMMS, plan for further evaluation and/or genetic testing, and any immediate impact on usual care for the patient’s HM (eg, related HSC donor selection must await results of genetic testing). Other practices may find referral to genetic counselors, specialized clinicians, or academic centers more appropriate for their practice needs. Table 2 can be used as a screening tool to guide the genetic workup for HMMSs in any clinical setting.
Case 1 (continued)
During the HMMS evaluation, the patient denies a history of easy bleeding or blood count abnormalities, but recalls that her mother may have had a low platelet count and required transfusions following childbirth. Her 42-year-old brother has frequent nosebleeds. Records confirm chronic thrombocytopenia in her mother and brother (platelet counts, 115 × 109/L and 145 × 109/L, respectively). FPD/AML is strongly suspected. Urgent single-site germ line testing of the RUNX1 mutation identified on somatic testing is recommended. A skin biopsy is performed at the site of her nadir BM biopsy for fibroblast culture. The primary hematologist is informed of the high suspicion for FPD/AML and recommended to avoid use of family donors unless a familial mutation is confirmed and the donor does not carry it.
How we perform genetic testing for HMMS
Whom to test.
The prevalence of HMMSs in most patient populations is unknown but is the subject of ongoing research. In small case series of children or young adults with MDS/AL or AA or in patients with HM tested for a suspicious personal or family history, the yield of germ line testing via gene panels ranges from 11% to 24%.24,57,58 These yields approach those of solid tumors, such as early-onset breast cancer,59 and justify genetic testing.
At present, we recommend clinical germ line genetic testing in: (1) families with 2 or more cases of MDS/AL; (2) families with MDS/AL and unexplained cytopenias/AA; and (3) individuals or families clustering MDS/AL with organ-system manifestations fitting a HMMS (Figure 1; Table 1). We routinely perform germ line testing for any individual whose tumor possesses mutations in genes associated with HMMSs (Table 1). This testing is performed on a clinical basis whenever possible. Germ line analysis is also imperative for: (1) biallelic CEBPA, as 7% to 11% of these individuals possess germ line CEBPA mutations55,56; (2) a deleterious GATA2 mutation, especially in children/adolescents with MDS, as germ line GATA2 mutations are present in 7% of these cases overall and up to 72% of patients with monosomy 7 (many of these will be de novo germ line mutations with no family history or clinical features [Table 1] of germ line GATA2 deficiency60); and (3) a deleterious RUNX1 mutation. Germ line RUNX1 mutations are associated with early-onset clonal hematopoiesis and cytopenias that may be erroneously treated as ITP, and germ line testing may therefore inform the care of the patient’s family.58
Families clustering mixed myeloid and lymphoid malignancies or lymphoid malignancies alone are more challenging, as the genes responsible for the majority of these families are largely unknown, although a pathogenic germ line variant of the KDR gene is associated with familial Hodgkin lymphoma.61 We consider clinical testing for these families on a case-by-case basis based on specific HMMS patterns. For example, we do not routinely test families with familial chronic lymphocytic leukemia, but we do offer testing for families with AML segregating with T-cell acute lymphoblastic leukemia or follicular lymphoma, as these patterns may reflect HMMS (Table 1).62 These recommendations will evolve as prevalence and yield of testing for HMMSs in different scenarios become available.
How to test.
Given the phenotypic overlap of HMMSs, we often recommend panel-based NGS testing for the known HMMSs and/or IBMFSs, ensuring that all genes relevant for the patient scenario are included. We use panels from The University of Chicago or the University of Washington.63,64 Single-gene and HMMS panels available at other laboratories can be found at www.genetests.org. Comprehensive techniques that detect point mutations and large deletions/duplications are essential, as these mutation types may cause HMMS. Once a familial mutation is identified in an individual, we perform site-specific testing for that particular mutation in other family members who seek testing. We may begin with site-specific testing if a deleterious HMMS mutation is identified on somatic tumor testing, but reflex to a larger panel if the patient scenario warrants. Standard germ line genetic testing clinical practice guidelines performed in other clinical scenarios should be followed, including pretest counseling about the reason for testing, testing alternatives, possible results, and how clinical management would change with or without testing.65,66
Tissue selection.
Genetic testing to identify germ line HMMS mutations requires careful tissue selection. In the setting of HM, the usual tissue source for germ line genetic testing in most other clinical scenarios, peripheral blood (PB), is an affected, tumor-containing tissue. Clonally skewed hematopoiesis further complicates PB analysis, as ∼1% of healthy patients under 50 years of age and 10% of healthy patients over 65 years of age will accumulate mutations in genes associated with MDS/AL, several of which cause HMMS if inherited in the germ line.67,68 Thus, clinicians should avoid the use of PB, BM, or other tissues frequently contaminated with PB such as saliva, buccal cells, and DNA made directly from skin biopsies without culture. Our preferred source of germ line DNA from individuals with HM is DNA derived from cultured skin fibroblasts, usually obtained from a 3-mm skin-punch biopsy or by removing a skin ellipse at the site of a BM biopsy. The major disadvantage of utilizing cultured skin fibroblasts is the 3 to 6 weeks required to culture a sufficient number of cells for genetic testing.
Results disclosure.
Disclosure of clinical results in which a germ line deleterious mutation has been identified is best performed in person with a physician and/or genetic counselor familiar with HMMSs. These discussions are facilitated greatly by pretest counseling. Occasionally, individuals cannot return to clinic, and telephone/video conferencing is used as is done in other hereditary cancer genetics disclosure scenarios without adverse effects.69,70 We also provide a “Family Letter” written in lay language summarizing our HMMS risk assessment, genetic testing results, recommendations for screening or follow-up care, and potential risk to and/or need for testing of additional family members. This letter is written for distribution to at-risk family members and the patient’s primary care and other physicians.
Case 2
A 42-year-old man is diagnosed with chronic myelomonocytic leukemia-2 with isolated isochromosome 17q. An allogeneic hematopoietic stem cell transplant (HSCT) is recommended in first remission. The patient’s 3 siblings are queried as potential HSC donors, and 1 is an HLA-identical match. The family history reveals that their father died of AML at 53 years of age. How should recipient and donor evaluations proceed?
Genetic testing in urgent clinical scenarios
Waiting up to 12 weeks for a skin fibroblast culture and genetic testing results is not appropriate in urgent clinical scenarios like case 2. For urgent scenarios only, we use buccal swabs, saliva, or DNA made directly from a skin biopsy without culture, but clearly inform the testing laboratory and patient that any findings will need confirmation in their concurrently growing skin fibroblasts before final interpretation.
For time-critical HSCT decisions, our HMMS genetics team performs simultaneous evaluations of the recipient and related donor(s). These paired evaluations provide objective data, including the donor’s blood counts and physical examination, that may result in a clinical HMMS diagnosis. We may then advise directed genetic testing of 1 or more gene(s) by Sanger sequencing, which may have a shorter turnaround time compared with panel/array testing. At the same time, the transplant team performs an expedited matched unrelated donor search. We recommend an unrelated donor HSCT if suspicion for an HMMS is high but a specific germ line mutation cannot be identified in a family. If no HLA-matched unrelated donors are located, a careful discussion of the potential risks and benefits in that family’s unique scenario are revisited with both donor and recipient. Rarely, we have convened a team of ethicists, transplant physicians, hematologists, and geneticists to develop a consensus donor recommendation for a patient.
Case 2 (continued)
HMMS-focused evaluations of both the recipient and his HLA-matched sibling are urgently performed. The recipient has chronic cutaneous warts on the hands and feet and lymphedema in the right lower extremity of unclear etiology. The 35-year-old sibling is healthy, but his complete blood count (CBC) shows mild anemia and leukopenia. A BM biopsy of the sibling/potential donor reveals newly diagnosed MDS with monosomy 7. GATA2 deficiency syndrome is clinically suspected. Expedited panel-based genetic testing is sent from a skin-punch biopsy from the recipient with an additional biopsy sent for fibroblast culture. A germ line GATA2 mutation is confirmed. Unrelated donor HSCT is recommended for the proband and his sibling as no appropriate related donors exist. What are the unique care needs for this family?
How we care for individuals with HMMS
Due to the recent description of these syndromes and the limited number of patients prospectively followed to date, evidence-based clinical surveillance and management recommendations for mutation carriers are not yet available but are the subject of ongoing research efforts.38 Thus, current recommendations are expert opinion-based and modeled after clinical guidelines developed for IBMFSs and other syndromes featuring HM, such as FA and Li-Fraumeni syndrome.3,32,38,71,72 The HMMS features of incomplete penetrance, variable phenotypic presentation, and anticipation all complicate development of clinical management recommendations even within a single syndrome.
Germ line mutation carriers with an active HM.
There are unique considerations involved in the care of individuals with an HM who carry a germ line HMMS gene mutation. First, referral to a multidisciplinary team that includes a physician who is well-versed in HMMS should be considered. This referral facilitates assessment of all potential HMMS-specific organ-system manifestations that may impact the patient’s HM treatment (eg, immunodeficiency in GATA2 deficiency) and expedite referral to appropriate subspecialists. This team may also have knowledge of HMMS-specific treatment options such as decreased efficacy of immunosuppression in AA in patients with telomere syndromes or a potential increased response to lenalidomide in patients with MDS/AML and a DDX41 mutation.13 Furthermore, this team will facilitate genetic testing and/or monitoring of at-risk family members.
For patients with a deleterious mutation in an HMMS-associated gene and an active HM, we advocate performing an allogeneic HSCT, regardless of prognostic markers, using donors who lack the familial mutation in order to eradicate not only the MDS/AL but the HM-predisposed BM as well. This approach is not universal, as certain scenarios warrant induction/consolidation treatment with allogeneic HSCT at relapse/diagnosis of second primary leukemias. For example, patients with germ line CEBPA mutations may warrant initial treatment with only chemotherapy given the long remissions these patients experience.7
HSCT timing, preparative regimen, peritransplant care, and donor selection require special consideration. Preparative regimen selection is critical for some HMMSs, specifically the telomere syndromes, as these individuals may experience excess toxicity with agents such as busulfan or an increased likelihood of graft failure.73-75 Differential outcomes with particular preparative regimens are not known in the other HMMSs at this time. Optimal peritransplant care includes a thorough evaluation for HMMS-specific organ manifestations in order to address presymptomatic organ dysfunction. In GATA2 deficiency, for example, antimicrobial prophylaxis is recommended against atypical mycobacteria.76
Case 2 (continued)
Evaluation does not identify any additional GATA2 deficiency syndrome manifestations. Atypical mycobacterial prophylaxis is incorporated into the peritransplant care plan. Genetic counseling and testing are offered to the parents and siblings. The 40-year-old sister is found to carry the familial mutation. Her baseline clinical evaluation and CBC are normal. How should she be followed?
Germ line mutation carriers without an HM
Surveillance recommendations include uniform recommendations for all mutation carriers, regardless of the specific gene involved, as well as recommendations unique to specific HMMSs (Table 33,10,11,13,14,17-20,28,32,38,39,71-83). These recommendations may be adjusted based on an individual family’s presentation.
Table 3.
Recommendations for the clinical care and surveillance of patients with pathogenic germline hereditary myeloid malignancy syndrome variants
| Syndrome | At diagnosis | At follow-up | Research questions |
|---|---|---|---|
| All inherited MDS and/or AL syndromes | CBC with differential | CBC with differential every 6-12 mo3,38,72,78 | What drives progression from the carrier state to overt malignancy development? |
| Clinical examination | Clinical examination every 6-12 mo | ||
| BM biopsy with aspirate and cytogenetic/molecular analysis3,38,72,78 | BM biopsy with aspirate and cytogenetic/molecular analysis at the time of any significant, persistent change in blood counts3,38,72,78 | What are useful clinical biomarkers of impending malignancy development? | |
| Educate the patient regarding signs and symptoms of MDS/AL and to alert his/her physician promptly for evaluation if any develop | If MDS or AL develops, consider risks and benefits of allogeneic transplant in first remission given risk of future second primary leukemias | ||
| Consider HLA typing patient and all full siblings | |||
| Site-specific testing for pathogenic germ line mutation in potential related donors | |||
| Careful consideration of matched related stem cell donors: avoid donors known to carry pathogenic germ line mutations or those with cytopenia(s) or donors who fail to mobilize well in whom a germ line mutation is not identifiable | |||
| Offer genetic counseling and site-specific testing for the familial mutation to all at-risk individuals | |||
| Familial MDS/AL with mutated DDX41 | How effective is lenalidomide for MDS/AML or other hematologic malignancies in the setting of a germ line DDX41 mutation?13 | ||
| What is the risk of lymphoma development and autoimmunity in those with germ line DDX41 mutations and does it vary by mutation type?14 | |||
| Familial aplastic anemia/MDS with SRP72 mutation | Screen newborns for congenital sensorineural deafness20 | ||
| Inherited syndromes associated with thrombocytopenia and platelet dysfunction | Educate the patient and his/her physicians that no specific treatment is required for asymptomatic thrombocytopenia | Provide platelet transfusions prior to major surgery or childbirth and consider HLA-matched platelets to avoid alloimmunization | ANKRD26: Do MEK inhibitors effectively improve platelet counts without limiting toxicities in patients with thrombocytopenia 2?80 |
| Thrombocytopenia 2 (ANKRD26) | Treatments for ITP, such as steroids and splenectomy, are ineffective and should be avoided10,11,17-19,28 | ||
| Thrombocytopenia 5 (ETV6) | Education regarding possible excessive bleeding risk with surgery, childbirth, or injury due to platelet dysfunction and to inform his/her hematologist prior to any invasive procedure for management recommendations | Consider allogeneic HSCT if a patient develops a regular transfusion requirement, clonal cytogenetic abnormality, dysplasia, or an overt hematologic malignancy | ETV6: Are colon cancer, GERD, myopathy and/or autoimmune disorders part of the clinical phenotype?17-19 |
| FPD/AML (RUNX1) | Consider platelet aggregation assays to evaluate platelet function | RUNX1: Can gene-corrected induced pluripotent stem cells reconstitute hematopoiesis and cure the BM manifestations?81 | |
| GATA2 deficiency syndromes (GATA2) | Screen for HPV infection and HPV-related cervical, head and neck, and anogenital cancers76 | Screen for HPV infections and HPV-related malignancies at least every 12 mo76 | Consider systemic interferon α for patients with refractory HPV or herpesvirus infections76 |
| Consider HPV vaccination76 | Repeat pulmonary function testing annually or sooner if new symptoms develop76 | ||
| Perform baseline pulmonary evaluation with pulmonary function testing. Include CT scan if symptoms warrant76 | Consider allogeneic transplant if a patient develops: a regular transfusion requirement, clonal cytogenetic abnormality, dysplasia, overt BM malignancy or recurrent severe infections | ||
| Educate the patient and his/her physicians regarding the increased risk of opportunistic infections (especially mycobacterial infections) due to immunodeficiency | Consider allogeneic transplant if patient shows somatic ASXL1 mutations and/or elevated (or increasingly elevated) FLT3 ligand39 | ||
| Consider azithromycin prophylaxis76 | |||
| Replace immunoglobulins if low and repeated infections | |||
| Screen for congenital deafness and avoid ototoxic drugs | |||
| Telomere syndromes due to TERC or TERT mutation | Consider telomere length measurement by flowFISH as first diagnostic test or to aid in diagnosis in those without an identifiable telomere-related mutation and/or variant of uncertain significance | If BM failure develops and warrants treatment, | |
| •avoid immunosuppression as a therapeutic strategy for telomere syndrome-associated AA given lack of efficacy (refer to DC guidelines statement77) | |||
| •carefully consider allogeneic HSCT | |||
| •androgens may lead to hematologic response82,83 | |||
| Educate patient to avoid smoking and pulmonary and BM toxic medications and to report any disease associated symptoms promptly for evaluation | |||
| Perform baseline pulmonary evaluation including pulmonary function tests ± CT scan for all with symptoms (eg, chronic cough or dyspnea) and asymptomatic carriers at age 40 y or 5-10 y earlier than the earliest pulmonary fibrosis or emphysema case in the family | Repeat pulmonary function tests every 1-3 y or sooner if any symptoms develop | ||
| Assess liver function tests; if abnormal, perform hepatic ultrasound and consider hepatology evaluation with telomere syndrome experienced physician | Assess liver function tests annually or with symptoms; perform hepatic ultrasound and consider hepatology evaluation if abnormal | ||
| Screen for clinical symptoms of head and neck cancer and perform baseline dental and head and neck exam | Screen for head and neck cancer via thorough dental evaluations every 6 mo ± otolaryngology evaluation annually or with symptoms | ||
| Screen for clinical symptoms of anogenital cancer; for females, perform pap/pelvic exam | Screen for clinical symptoms of anogenital cancer; for females, perform pap/pelvic exam annually | ||
| Consider HPV vaccination | |||
| Awareness that younger generations may present with more severe disease at earlier ages (anticipation) | If HSCT is warranted, choose a conditioning regimen with known efficacy and lack of excess toxicity in patients with telomere syndromes (eg, avoid busulfan-based regimens)73-75 | ||
| Li-Fraumeni syndrome | CBC with differential and ESR/LDH every 4 mo32,71 | Follow chosen Li-Fraumeni syndrome screening protocol (interval for exams and screening tests every 4-6 mo)32,71 | |
| Consider a comprehensive screening program, ideally on a clinical trial, for the core Li-Fraumeni syndrome cancers (eg, breast, brain, and sarcoma) | |||
| Avoid unnecessary radiation to prevent radiation-induced malignancies79 |
CT, computed tomography; DC, dyskeratosis congenita; ESR, erythrocyte sedimentation rate; flowFISH, fluorescent in situ hybridization with flow cytometry; GERD, gastroesophageal reflux disease; HPV, human papillomavirus; LDH, lactate dehydrogenase.
Uniform recommendations.
The age at which a baseline hematopoietic evaluation should be performed is based on the specific syndrome and family presentation. For example, an individual with a germ line DDX41 mutation and 3 relatives with MDS/AL with earliest case at 60 years of age should start surveillance in their 40s, whereas even children should be monitored in syndromes such as thrombocytopenia 5 that feature lifelong thrombocytopenia and platelet dysfunction. The initial baseline evaluation should include a CBC with differential, HLA typing, and consideration of a BM biopsy with cytogenetic analysis. Individuals with HMMSs featuring specific organ-system dysfunction should be monitored and treated for signs or symptoms of these conditions. All asymptomatic individuals with a normal baseline evaluation should have routine CBCs every 6 to 12 months. A repeat BM with cytogenetic analysis is essential if an individual develops CBC abnormalities. If this BM remains normal or similar to the patient’s baseline, a repeat CBC should be performed monthly and a repeat BM should be considered in 3 to 4 months, as recommended for IBMFSs featuring AA/MDS/AL.3,23,32,72 The diagnosis of low-grade MDS without an identifiable cytogenetic abnormality is especially difficult in the setting of a germ line HMMS mutation. First, the mutation itself may cause subtle dyspoiesis. In addition, up to 81% of patients with germ line mutations in RUNX1 and GATA2, the 2 HMMSs examined to date, will develop clonal hematopoiesis by 50 years of age, further complicating the interpretation of acquired mutations in the PB or BM of these patients.58 It is not yet clear which of these mutations signals impending malignancy development. At present, new clonal hematopoiesis in a patient should trigger closer surveillance and a more extensive workup. Genotyping of the pathogenic allele in matched related donors should be considered at diagnosis to avoid delays associated with genetic testing at the time of any future MDS/AL diagnoses. The prophylactic use of allogeneic HSCT in these individuals has been anecdotal to date and remains controversial in the field.84 In some cases, an HSCT may be indicated for severe HMMS manifestations other than MDS/AL, such as AA in telomere syndromes, repeated severe infections in GATA2 deficiency syndromes, or the development of clonal hematopoiesis.76
Individuals with clinically defined HMMS.
A substantial portion of families suspected of having an HMMS will fail to have a positive molecular diagnosis after testing for the currently known HMMS is complete. How should one care for families where the history is consistent with an HMMS but the molecular lesion remains undefined? If the personal or family history is undeniable (ie, a patient with pathologically confirmed AML in 4 first-degree family members, but a negative workup for all currently known gene mutations; or a patient with lymphedema, mycobacterial infection, and early-onset chronic myelomonocytic leukemia whose testing is negative for a GATA2 mutation), we provide a clinical diagnosis of the respective HMMS and provide care appropriate for that HMMS. If the family history is not clear, it is crucial to take into account the patient’s options and act in his/her best interests. We attempt to enroll patients suspected of having an HMMS, but who test negative for known pathogenic variants, on research protocols designed to both prospectively follow the patients as well as to facilitate new syndrome discovery (Figure 2).
Areas of active research
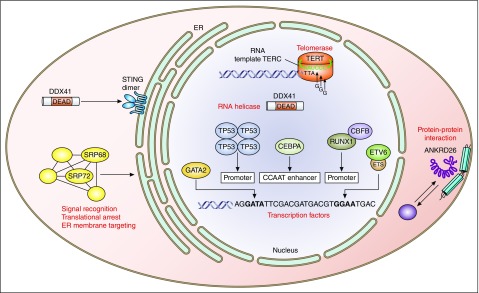
Much remains to be learned in the field of HMMSs. We urge international centers to take family pedigrees and collect both germ line and malignant tissues from every patient using institutional review board–approved research protocols.85 Participation should be offered to affected and unaffected family members to facilitate discovery, develop penetrance estimates, and populate long-term follow-up studies. Questions actively being pursued include: identification of novel inherited HM alleles, the prevalence of HMMSs in adult populations, the lifetime risks for specific HM and/or syndromic health problems, and the molecular mechanisms of disease in HM (Figure 3)6,8,9,17-19,34,35,80,86-89 and the implications of these processes for the development of novel therapeutics and long-term patient care.
Figure 3.
Cellular roles of proteins encoded by genes involved in HMMSs. Pathogenic germline mutations involved in HMMSs affect protein products that are involved in a variety of cellular mechanisms. CEBPA, ETV6, GATA2, RUNX1, and TP53 are transcription factors that localize to the nucleus.6,8,9,17-19,34,35,86 TERT and TERC both constitute subunits of telomerase and also localize to the nucleus.87 DDX41 is an RNA helicase and localizes to the cytosol.88 SRP72 is a ribonucleoprotein that is involved in signal recognition, RNA binding, and cellular trafficking.89 The function of ankyrin repeat domain-containing protein 26 is not well known, but the protein likely localizes to the inner part of the cell membrane and centrosome.80 ER, endoplasmic reticulum.
Conclusions
The field of HMMSs has expanded rapidly with the dissemination of more affordable NGS techniques and increased family history collection in adult hematology clinics. Early estimates suggest the proportion of unselected HM patients that may have a hereditary component approaches rates seen in other tumor types, such as high-risk breast cancer. Thus, there is a growing need for physicians, genetic counselors, and nurses who are well-versed in the diagnosis and management of individuals with HMMSs. Much remains to be learned about HMMSs, but we are hopeful that continued progress will be made and will eventually produce methods of prevention similar to the progress made in hereditary breast and ovarian cancers.
Acknowledgments
The authors thank their patients and families for their inspiration and participation in the research that has helped advance the field of inherited hematopoietic malignancies.
Contributor Information
Collaborators: Michael W. Drazer, Simone Feurstein, Allison H. West, Matthew F. Jones, Jane E. Churpek, and Lucy A. Godley
Authorship
Contribution: M.W.D., S.F., J.E.C., and L.A.G. cowrote the paper and assisted with construction of tables and figures; and A.H.W. and M.F.J. assisted with editing of the paper and assisted with construction of tables and figures.
Conflict-of-interest disclosure: J.E.C. and L.A.G. receive royalties from their coauthored article on inherited hematopoietic malignancies in UpToDate. The remaining authors declare no competing financial interests.
The current affiliation for S.F. is Klinik für Innere Medizin III, Abteilung Hämatologie und Onkologie, Universitätsklinikum Ulm, Ulm, Germany.
A complete list of the members of The University of Chicago Hematopoietic Malignancies Cancer Risk Team who contributed to this article appears in “Appendix.”
Correspondence: Jane E. Churpek, The University of Chicago, 5841 S. Maryland Ave, MC 2115, Chicago, IL 60637; e-mail: jchurpek@medicine.bsd.uchicago.edu; and Lucy A. Godley, The University of Chicago, 5841 S. Maryland Ave, MC 2115, Chicago, IL 60637; e-mail: lgodley@medicine.bsd.uchicago.edu.
Appendix
Members of The University of Chicago Hematopoietic Malignancies Cancer Risk Team who contributed to this article include: Michael W. Drazer, Simone Feurstein, Allison H. West, Matthew F. Jones, Jane E. Churpek, and Lucy A. Godley.
References
- 1.Gunz FW, Gunz JP, Veale AM, Chapman CJ, Houston IB. Familial leukaemia: a study of 909 families. Scand J Haematol. 1975;15(2):117–131. doi: 10.1111/j.1600-0609.1975.tb01063.x. [DOI] [PubMed] [Google Scholar]
- 2.Luddy RE, Champion LA, Schwartz AD. A fatal myeloproliferative syndrome in a family with thrombocytopenia and platelet dysfunction. Cancer. 1978;41(5):1959–1963. doi: 10.1002/1097-0142(197805)41:5<1959::aid-cncr2820410540>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 3. Fanconi anemia: guidelines for diagnosis and management. 4th ed. Eugene, OR: Fanconi Anemia Research Fund, Inc; 2014. http://fanconi.org/index.php/publications/guidelines_for_diagnosis_and_management. Accessed 14 July 2016.
- 4.Nagy R, Sweet K, Eng C. Highly penetrant hereditary cancer syndromes. Oncogene. 2004;23(38):6445–6470. doi: 10.1038/sj.onc.1207714. [DOI] [PubMed] [Google Scholar]
- 5.Uno H, Cronin AM, Wadleigh M, Schrag D, Abel GA. Derivation and validation of the SEER-Medicare myelodysplastic syndromes risk score (SMMRS). Leuk Res. 2014;38(12):1420–1424. doi: 10.1016/j.leukres.2014.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Song WJ, Sullivan MG, Legare RD, et al. Haploinsufficiency of CBFA2 causes familial thrombocytopenia with propensity to develop acute myelogenous leukaemia. Nat Genet. 1999;23(2):166–175. doi: 10.1038/13793. [DOI] [PubMed] [Google Scholar]
- 7.Smith ML, Cavenagh JD, Lister TA, Fitzgibbon J. Mutation of CEBPA in familial acute myeloid leukemia. N Engl J Med. 2004;351(23):2403–2407. doi: 10.1056/NEJMoa041331. [DOI] [PubMed] [Google Scholar]
- 8.Hahn CN, Chong CE, Carmichael CL, et al. Heritable GATA2 mutations associated with familial myelodysplastic syndrome and acute myeloid leukemia. Nat Genet. 2011;43(10):1012–1017. doi: 10.1038/ng.913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ostergaard P, Simpson MA, Connell FC, et al. Mutations in GATA2 cause primary lymphedema associated with a predisposition to acute myeloid leukemia (Emberger syndrome). Nat Genet. 2011;43(10):929–931. doi: 10.1038/ng.923. [DOI] [PubMed] [Google Scholar]
- 10.Noris P, Perrotta S, Seri M, et al. Mutations in ANKRD26 are responsible for a frequent form of inherited thrombocytopenia: analysis of 78 patients from 21 families. Blood. 2011;117(24):6673–6680. doi: 10.1182/blood-2011-02-336537. [DOI] [PubMed] [Google Scholar]
- 11.Pippucci T, Savoia A, Perrotta S, et al. Mutations in the 59 UTR of ANKRD26, the ankirin repeat domain 26 gene, cause an autosomal-dominant form of inherited thrombocytopenia, THC2. Am J Hum Genet. 2011;88(1):115–120. doi: 10.1016/j.ajhg.2010.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saliba J, Saint-Martin C, Di Stefano A, et al. Germline duplication of ATG2B and GSKIP predisposes to familial myeloid malignancies. Nat Genet. 2015;47(10):1131–1140. doi: 10.1038/ng.3380. [DOI] [PubMed] [Google Scholar]
- 13.Polprasert C, Schulze I, Sekeres MA, et al. Inherited and somatic defects in DDX41 in myeloid neoplasms. Cancer Cell. 2015;27(5):658–670. doi: 10.1016/j.ccell.2015.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lewinsohn M, Brown AL, Weinel LM, et al. Novel germ line DDX41 mutations define families with a lower age of MDS/AML onset and lymphoid malignancies. Blood. 2016;127(8):1017–1023. doi: 10.1182/blood-2015-10-676098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li R, Sobreira N, Witmer PD, Pratz KW, Braunstein EM. Two novel germline DDX41 mutations in a family with inherited myelodysplasia/acute myeloid leukemia. Haematologica. 2016;101(6):e228–e231. doi: 10.3324/haematol.2015.139790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cardoso SR, Ryan G, Walne AJ, et al. Germline heterozygous DDX41 variants in a subset of familial myelodysplasia and acute myeloid leukemia [published online ahead of print 20 May 2016]. Leukemia. doi:10.1038/leu.2016.124. [DOI] [PMC free article] [PubMed]
- 17.Zhang MY, Churpek JE, Keel SB, et al. Germline ETV6 mutations in familial thrombocytopenia and hematologic malignancy. Nat Genet. 2015;47(2):180–185. doi: 10.1038/ng.3177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Noetzli L, Lo RW, Lee-Sherick AB, et al. Germline mutations in ETV6 are associated with thrombocytopenia, red cell macrocytosis and predisposition to lymphoblastic leukemia. Nat Genet. 2015;47(5):535–538. doi: 10.1038/ng.3253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Topka S, Vijai J, Walsh MF, et al. Germline ETV6 mutations confer susceptibility to acute lymphoblastic leukemia and thrombocytopenia. PLoS Genet. 2015;11(6):e1005262. doi: 10.1371/journal.pgen.1005262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kirwan M, Walne AJ, Plagnol V, et al. Exome sequencing identifies autosomal-dominant SRP72 mutations associated with familial aplasia and myelodysplasia. Am J Hum Genet. 2012;90(5):888–892. doi: 10.1016/j.ajhg.2012.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dokal I, Vulliamy T. Inherited bone marrow failure syndromes. Haematologica. 2010;95(8):1236–1240. doi: 10.3324/haematol.2010.025619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holme H, Hossain U, Kirwan M, Walne A, Vulliamy T, Dokal I. Marked genetic heterogeneity in familial myelodysplasia/acute myeloid leukaemia. Br J Haematol. 2012;158(2):242–248. doi: 10.1111/j.1365-2141.2012.09136.x. [DOI] [PubMed] [Google Scholar]
- 23.Ballew BJ, Savage SA. Updates on the biology and management of dyskeratosis congenita and related telomere biology disorders. Expert Rev Hematol. 2013;6(3):327–337. doi: 10.1586/ehm.13.23. [DOI] [PubMed] [Google Scholar]
- 24.Zhang J, Walsh MF, Wu G, et al. Germline mutations in predisposition genes in pediatric cancer. N Engl J Med. 2015;373(24):2336–2346. doi: 10.1056/NEJMoa1508054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Churpek JE, Marquez R, Neistadt B, et al. Inherited mutations in cancer susceptibility genes are common among survivors of breast cancer who develop therapy-related leukemia. Cancer. 2016;122(2):304–311. doi: 10.1002/cncr.29615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buijs A, Poddighe P, van Wijk R, et al. A novel CBFA2 single-nucleotide mutation in familial platelet disorder with propensity to develop myeloid malignancies. Blood. 2001;98(9):2856–2858. doi: 10.1182/blood.v98.9.2856. [DOI] [PubMed] [Google Scholar]
- 27.Fogarty PF, Yamaguchi H, Wiestner A, et al. Late presentation of dyskeratosis congenita as apparently acquired aplastic anaemia due to mutations in telomerase RNA. Lancet. 2003;362(9396):1628–1630. doi: 10.1016/S0140-6736(03)14797-6. [DOI] [PubMed] [Google Scholar]
- 28.Owen CJ, Toze CL, Koochin A, et al. Five new pedigrees with inherited RUNX1 mutations causing familial platelet disorder with propensity to myeloid malignancy. Blood. 2008;112(12):4639–4645. doi: 10.1182/blood-2008-05-156745. [DOI] [PubMed] [Google Scholar]
- 29.Xiao H, Shi J, Luo Y, et al. First report of multiple CEBPA mutations contributing to donor origin of leukemia relapse after allogeneic hematopoietic stem cell transplantation. Blood. 2011;117(19):5257–5260. doi: 10.1182/blood-2010-12-326322. [DOI] [PubMed] [Google Scholar]
- 30.Liew E, Owen C. Familial myelodysplastic syndromes: a review of the literature. Haematologica. 2011;96(10):1536–1542. doi: 10.3324/haematol.2011.043422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rojek K, Nickels E, Neistadt B, et al. Identifying inherited and acquired genetic factors involved in poor stem cell mobilization and donor-derived malignancy [published online ahead of print 4 August 2016]. Biol Blood Marrow Transplant. doi: 10.1016/j.bbmt.2016.08.002. doi:10.1016/j.bbmt.2016.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.National Comprehensive Cancer Network. Fort Washington, PA: National Comprehensive Cancer Network; 2016. Genetic/Familial High Risk Assessment: Breast and Ovarian Cancer. Vol. 2016. [Google Scholar]
- 33.Arber DA, Orazi A, Hasserjian R, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–2405. doi: 10.1182/blood-2016-03-643544. [DOI] [PubMed] [Google Scholar]
- 34.Gonzalez KD, Noltner Ka, Buzin CH, et al. Beyond Li Fraumeni Syndrome: clinical characteristics of families with p53 germline mutations. J Clin Oncol. 2009;27(8):1250–1256. doi: 10.1200/JCO.2008.16.6959. [DOI] [PubMed] [Google Scholar]
- 35.Bougeard G, Renaux-Petel M, Flaman JM, et al. Revisiting Li-Fraumeni Syndrome from TP53 Mutation Carriers. J Clin Oncol. 2015;33(21):2345–2352. doi: 10.1200/JCO.2014.59.5728. [DOI] [PubMed] [Google Scholar]
- 36.Churpek JE, Godley LA. Familial Acute Leukemia and Myelodysplastic Syndromes. Post TW, ed. Waltham, MA: UpToDate, Inc. www.uptodate.com. Accessed 19 April 2016.
- 37.Churpek JE, Onel K. Heritability of hematologic malignancies: from pedigrees to genomics. Hematol Oncol Clin North Am. 2010;24(5):939–972. doi: 10.1016/j.hoc.2010.06.001. [DOI] [PubMed] [Google Scholar]
- 38.Churpek JE, Lorenz R, Nedumgottil S, et al. Proposal for the clinical detection and management of patients and their family members with familial myelodysplastic syndrome/acute leukemia predisposition syndromes. Leuk Lymphoma. 2013;54(1):28–35. doi: 10.3109/10428194.2012.701738. [DOI] [PubMed] [Google Scholar]
- 39.West AH, Godley LA, Churpek JE. Familial myelodysplastic syndrome/acute leukemia syndromes: a review and utility for translational investigations. Ann N Y Acad Sci. 2014;1310:111–118. doi: 10.1111/nyas.12346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Babushok DV, Bessler M, Olson TS. Genetic predisposition to myelodysplastic syndrome and acute myeloid leukemia in children and young adults. Leuk Lymphoma. 2016;57(3):520–536. doi: 10.3109/10428194.2015.1115041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Churpek JE, Artz A, Bishop M, Liu H, Godley LA. Correspondence regarding the consensus statement from the Worldwide Network for Blood and Marrow Transplantation Standing Committee on Donor Issues. Biol Blood Marrow Transplant. 2016;22(1):183–184. doi: 10.1016/j.bbmt.2015.10.008. [DOI] [PubMed] [Google Scholar]
- 42.Cilloni D, Gottardi E, Messa F, et al. Piedmont Study Group on Myleodysplastic Syndromes. Significant correlation between the degree of WT1 expression and the International Prognostic Scoring System Score in patients with myelodysplastic syndromes. J Clin Oncol. 2003;21(10):1988–1995. doi: 10.1200/JCO.2003.10.503. [DOI] [PubMed] [Google Scholar]
- 43.Bienz M, Ludwig M, Leibundgut EO, et al. Risk assessment in patients with acute myeloid leukemia and a normal karyotype. Clin Cancer Res. 2005;11(4):1416–1424. doi: 10.1158/1078-0432.CCR-04-1552. [DOI] [PubMed] [Google Scholar]
- 44.Marcucci G, Maharry K, Whitman SP, et al. Cancer and Leukemia Group B Study. High expression levels of the ETS-related gene, ERG, predict adverse outcome and improve molecular risk-based classification of cytogenetically normal acute myeloid leukemia: a Cancer and Leukemia Group B Study. J Clin Oncol. 2007;25(22):3337–3343. doi: 10.1200/JCO.2007.10.8720. [DOI] [PubMed] [Google Scholar]
- 45.Santamaria CM, Chillón MC, García-Sanz R, et al. Molecular stratification model for prognosis in cytogenetically normal acute myeloid leukemia. Blood. 2009;114(1):148–152. doi: 10.1182/blood-2008-11-187724. [DOI] [PubMed] [Google Scholar]
- 46.Abbas S, Lugthart S, Kavelaars FG, et al. Acquired mutations in the genes encoding IDH1 and IDH2 both are recurrent aberrations in acute myeloid leukemia: prevalence and prognostic value. Blood. 2010;116(12):2122–2126. doi: 10.1182/blood-2009-11-250878. [DOI] [PubMed] [Google Scholar]
- 47.Green CL, Evans CM, Hills RK, Burnett AK, Linch DC, Gale RE. The prognostic significance of IDH1 mutations in younger adult patients with acute myeloid leukemia is dependent on FLT3/ ITD status. Blood. 2010;116(15):2779–2782. doi: 10.1182/blood-2010-02-270926. [DOI] [PubMed] [Google Scholar]
- 48.Paschka P, Schlenk RF, Gaidzik VI, et al. IDH1 and IDH2 mutations are frequent genetic alterations in acute myeloid leukemia and confer adverse prognosis in cytogenetically normal acute myeloid leukemia with NPM1 mutation without FLT3 internal tandem duplication. J Clin Oncol. 2010;28(22):3636–3643. doi: 10.1200/JCO.2010.28.3762. [DOI] [PubMed] [Google Scholar]
- 49.Schnittger S, Haferlach C, Ulke M, Alpermann T, Kern W, Haferlach T. IDH1 mutations are detected in 6.6% of 1414 AML patients and are associated with intermediate risk karyotype and unfavorable prognosis in adults younger than 60 years and unmutated NPM1 status. Blood. 2010;116(25):5486–5496. doi: 10.1182/blood-2010-02-267955. [DOI] [PubMed] [Google Scholar]
- 50.Schwind S, Marcucci G, Maharry K, et al. BAALC and ERG expression levels are associated with outcome and distinct gene and microRNA expression profiles in older patients with de novo cytogenetically normal acute myeloid leukemia: a Cancer and Leukemia Group B study. Blood. 2010;116(25):5660–5669. doi: 10.1182/blood-2010-06-290536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wagner K, Damm F, Göhring G, et al. Impact of IDH1 R132 mutations and an IDH1 single nucleotide polymorphism in cytogenetically normal acute myeloid leukemia: SNP rs11554137 is an adverse prognostic factor. J Clin Oncol. 2010;28(14):2356–2364. doi: 10.1200/JCO.2009.27.6899. [DOI] [PubMed] [Google Scholar]
- 52.Bejar R, Stevenson K, Abdel-Wahab O, et al. Clinical effect of point mutations in myelodysplastic syndromes. N Engl J Med. 2011;364(26):2496–2506. doi: 10.1056/NEJMoa1013343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Damm F, Chesnais V, Nagata Y, et al. BCOR and BCORL1 mutations in myelodysplastic syndromes and related disorders. Blood. 2013;122(18):3169–3177. doi: 10.1182/blood-2012-11-469619. [DOI] [PubMed] [Google Scholar]
- 54.Bejar R, Stevenson KE, Caughey B, et al. Somatic mutations predict poor outcome in patients with myelodysplastic syndrome after hematopoietic stem-cell transplantation. J Clin Oncol. 2014;32(25):2691–2698. doi: 10.1200/JCO.2013.52.3381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pabst T, Eyholzer M, Haefliger S, Schardt J, Mueller BU. Somatic CEBPA mutations are a frequent second event in families with germline CEBPA mutations and familial acute myeloid leukemia. J Clin Oncol. 2008;26(31):5088–5093. doi: 10.1200/JCO.2008.16.5563. [DOI] [PubMed] [Google Scholar]
- 56.Taskesen E, Bullinger L, Corbacioglu A, et al. Prognostic impact, concurrent genetic mutations, and gene expression features of AML with CEBPA mutations in a cohort of 1182 cytogenetically normal AML patients: further evidence for CEBPA double mutant AML as a distinctive disease entity. Blood. 2011;117(8):2469–2475. doi: 10.1182/blood-2010-09-307280. [DOI] [PubMed] [Google Scholar]
- 57.Knight Johnson AE, Guidugli L, Arndt K, et al. Identification of genetic hereditary predisposition to hematologic malignancies by clinical nextgeneration sequencing [abstract]. Blood. 2015;126(23) Abstract 3854. [Google Scholar]
- 58.Churpek JE, Pyrtel K, Kanchi KL, et al. Genomic analysis of germ line and somatic variants in familial myelodysplasia/acute myeloid leukemia. Blood. 2015;126(22):2484–2490. doi: 10.1182/blood-2015-04-641100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tung N, Battelli C, Allen B, et al. Frequency of mutations in individuals with breast cancer referred for BRCA1 and BRCA2 testing using next-generation sequencing with a 25-gene panel. Cancer. 2015;121(1):25–33. doi: 10.1002/cncr.29010. [DOI] [PubMed] [Google Scholar]
- 60.Wlodarski MW, Hirabayashi S, Pastor V, et al. EWOG-MDS. Prevalence, clinical characteristics, and prognosis of GATA2-related myelodysplastic syndromes in children and adolescents. Blood. 2016;127(11):1387–1397. doi: 10.1182/blood-2015-09-669937. [DOI] [PubMed] [Google Scholar]
- 61.Rotunno M, McMaster ML, Boland J, et al. Whole exome sequencing in families at high risk for Hodgkin lymphoma: identification of a predisposing mutation in the KDR gene. Haematologica. 2016;101(7):853–860. doi: 10.3324/haematol.2015.135475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mutsaers PG, van de Loosdrecht AA, Tawana K, et al. Highly variable clinical manifestations in a large family with a novel GATA2 mutation. Leukemia. 2013;27(11):2247–2248. doi: 10.1038/leu.2013.105. [DOI] [PubMed] [Google Scholar]
- 63.The University of Chicago. Genetic Services Laboratories. http://dnatesting.uchicago.edu. Accessed July 14, 2016.
- 64.University of Washington Department of Laboratory Medicine. Genetics and Solid Tumor Diagnostic Testing. http://depts.washington.edu/labweb/Divisions/MolDiag/MolDiagGen/index.htm. Accessed 14 July 2016.
- 65.Robson ME, Storm CD, Weitzel J, et al. American Society of Clinical Oncology policy statement update: genetic and genomic testing for cancer susceptibility. J Clin Oncol. 2010;28(5):893–901. doi: 10.1200/JCO.2009.27.0660. [DOI] [PubMed] [Google Scholar]
- 66.DiNardo CD, Bannon SA, Routbort M, et al. Evaluation of patients and families with concern for predispositions to hematologic malignancies within the Hereditary Hematologic Malignancy Clinic (HHMC). Clin Lymphoma Myeloma Leuk. 2016;16(7) doi: 10.1016/j.clml.2016.04.001. 417–428.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jaiswal S, Fontanillas P, Flannick J, et al. Age-related clonal hematopoiesis associated with adverse outcomes. N Engl J Med. 2014;371(26):2488–2498. doi: 10.1056/NEJMoa1408617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Genovese G, Kahler AK, Handsaker RE, et al. Clonal hematopoiesis and blood-cancer risk inferred from blood DNA sequence. NEJM. 2014;371(26):2477–2487. doi: 10.1056/NEJMoa1409405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Schwartz MD, Valdimarsdottir HB, Peshkin BN, et al. Randomized noninferiority trial of telephone versus in-person genetic counseling for hereditary breast and ovarian cancer. J Clin Oncol. 2014;32(7):618–626. doi: 10.1200/JCO.2013.51.3226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kinney AY, Butler KM, Schwartz MD, et al. Expanding access to BRCA1/2 genetic counseling with telephone delivery: a cluster randomized trial. J Natl Cancer Inst. 2014;106(12) doi: 10.1093/jnci/dju328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Villani A, Tabori U, Schiffman J, et al. Biochemical and imaging surveillance in germline TP53 mutation carriers with Li- Fraumeni syndrome: a prospective observational study. Lancet Oncol. 2011;12(6):559–567. doi: 10.1016/S1470-2045(11)70119-X. [DOI] [PubMed] [Google Scholar]
- 72.Savage SA, Cook EF, editors. Dyskeratosis Congenita and Telomere Biology Disorders: Diagnosis and Management Guidelines. 1st ed. New York, NY: Dyskeratosis Congenita Outreach, Inc; 2015.; https://www.dcoutreach.org/sites/default/files/DC%20%26%20TBD% 20Diagnosis%20And%20Management%20Guidelines.pdf. Accessed 14 July, 2016. [Google Scholar]
- 73.Dror Y, Freedman MH, Leaker M, et al. Lowintensity hematopoietic stem-cell transplantation across human leucocyte antigen barriers in dyskeratosis congenita. Bone Marrow Transplant. 2003;31(10):847–850. doi: 10.1038/sj.bmt.1703931. [DOI] [PubMed] [Google Scholar]
- 74.de la Fuente J, Dokal I. Dyskeratosis congenita: advances in the understanding of the telomerase defect and the role of stem cell transplantation. Pediatr Transplant. 2007;11(6):584–594. doi: 10.1111/j.1399-3046.2007.00721.x. [DOI] [PubMed] [Google Scholar]
- 75.Dietz AC, Orchard PJ, Baker KS, et al. Diseasespecific hematopoietic cell transplantation: nonmyeloablative conditioning regimen for dyskeratosis congenita. Bone Marrow Transplant. 2011;46(1):98–104. doi: 10.1038/bmt.2010.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Spinner MA, Sanchez LA, Hsu AP, et al. GATA2 deficiency: a protean disorder of hematopoiesis, lymphatics, and immunity. Blood. 2014;123(6):809–821. doi: 10.1182/blood-2013-07-515528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Al-Rahawan MM, Giri N, Alter BP. Intensive immunosuppression therapy for aplastic anemia associated with dyskeratosis congenita. Int J Hematol. 2006;83(3):275–276. doi: 10.1532/IJH97.06030. [DOI] [PubMed] [Google Scholar]
- 78.Nickels EM, Soodalter J, Churpek JE, Godley LA. Recognizing familial myeloid leukemia in adults. Ther Adv Hematol. 2013;4(4):254–269. doi: 10.1177/2040620713487399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sorrell AD, Espenschied CR, Culver JO, Weitzel JN. Tumor protein p53 (TP53) testing and Li-Fraumeni syndrome: current status of clinical applications and future directions. Mol Diagn Ther. 2013;17(1):31–47. doi: 10.1007/s40291-013-0020-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bluteau D, Balduini A, Balayn N, et al. Thrombocytopenia-associated mutations in the ANKRD26 regulatory region induce MAPK hyperactivation. J Clin Invest. 2014;124(2):580–591. doi: 10.1172/JCI71861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Connelly JP, Kwon EM, Gao Y, et al. Targeted correction of RUNX1 mutation in FPD patient specific induced pluripotent stem cells rescues megakaryopoietic defects. Blood. 2014;124(12):1926–1930. doi: 10.1182/blood-2014-01-550525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Townsley DM, Dumitriu B, Young NS. Bone marrow failure and the telomeropathies. Blood. 2014;124(18):2775–2783. doi: 10.1182/blood-2014-05-526285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Townsley DM, Dumitriu B, Liu D, et al. Danazol treatment for telomere diseases. N Engl J Med. 2016;374(20):1922–1931. doi: 10.1056/NEJMoa1515319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Saida S, Umeda K, Yasumi T, et al. Successful reduced-intensity stem cell transplantation for GATA2 deficiency before progression of advanced MDS. Pediatr Transplant. 2016;20(2):333–336. doi: 10.1111/petr.12667. [DOI] [PubMed] [Google Scholar]
- 85.Lu KH, Wood ME, Daniels M, et al. American Society of Clinical Oncology Expert Statement: collection and use of a cancer family history for oncology providers. J Clin Oncol. 2014;32(8):833–840. doi: 10.1200/JCO.2013.50.9257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Pabst T, Mueller BU, Zhang P, et al. Dominant-negative mutations of CEBPA, encoding CCAAT/enhancer binding protein-alpha (C/EBPalpha), in acute myeloid leukemia. Nat Genet. 2001;27(3):263–270. doi: 10.1038/85820. [DOI] [PubMed] [Google Scholar]
- 87.Her J, Chung IK. The AAA-ATPase NVL2 is a telomerase component essential for holoenzyme assembly. Biochem Biophys Res Commun. 2012;417(3):1086–1092. doi: 10.1016/j.bbrc.2011.12.101. [DOI] [PubMed] [Google Scholar]
- 88.Lee KG, Kim SS, Kui L, et al. Bruton's tyrosine kinase phosphorylates DDX41 and activates its binding of dsDNA and STING to initiate type 1 interferon response. Cell Rep. 2015;10(7):1055–1065. doi: 10.1016/j.celrep.2015.01.039. [DOI] [PubMed] [Google Scholar]
- 89.Nagai K, Oubridge C, Kuglstatter A, et al. Structure, function, and evolution of the signal recognition particle. EMBO J. 2003;22(14):3479–3485. doi: 10.1093/emboj/cdg337. [DOI] [PMC free article] [PubMed] [Google Scholar]