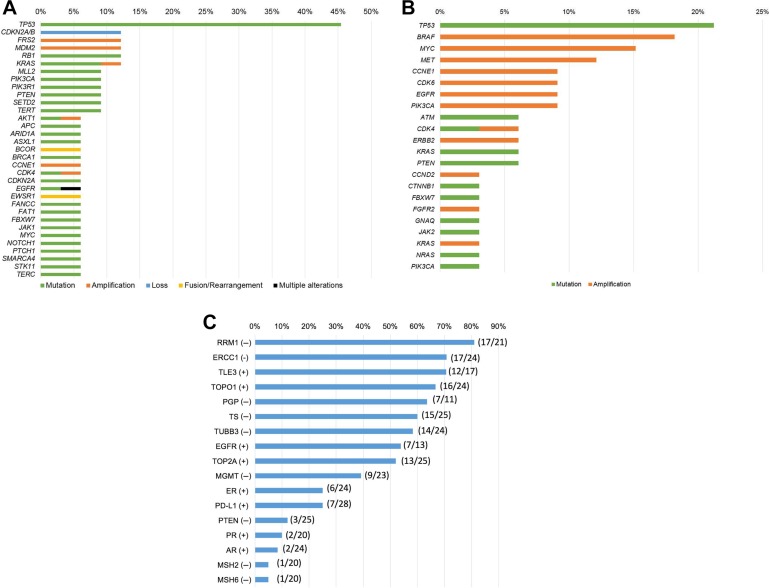
Figure 1.
Genomic and protein analyses among patients presented at Rare Tumor Clinic (n = 40). (A): Frequency of genomic alterations detected by tissue next‐generation sequencing (236 to 434 genes) in the Rare Tumor Clinic (n = 33). Included gene alterations with n ≥2. Among 33 patients who had tissue next‐generation sequencing, the most common alteration was TP53 alteration (45.5% [15/33]), followed by CDKN2A/B loss (12.1% [4/33]), FRS2 amplification (12.1% [4/33]), MDM2 amplification (12.1% [4/33]), RB1 alteration (12.1% [4/33]), and KRAS alteration (12.1% [4/33]; supplemental online Table 4). (B): Frequency of characterized genomic alterations detected by circulating‐tumor DNA (ctDNA) in the Rare Tumor Clinic (Guardant Health; 54 to 70 genes; n = 33). Among 33 patients who had ctDNA evaluation, the most common alteration was TP53 alteration (21.2% [7/33]), followed by BRAF amplification (18.2% [6/33]), MYC amplification (15.2% [5/33]), and MET amplification (12.1% [4/33]; supplemental online Table 5). (C): Frequency of protein aberrations detected via immunohistochemistry in the Rare Tumor Clinic (n = 29). Among 29 patients who had immunohistochemistry, the most common potentially actionable marker was RRM1 negative (81.0% [17/21]), followed by ERCC1 negative (70.8% [17/24]), TLE3 positive (70.6% [12/17]), and TOPO1 positive (66.7% [16/24]). Supplemental online Table 2 shows abbreviations and implications of each protein marker.