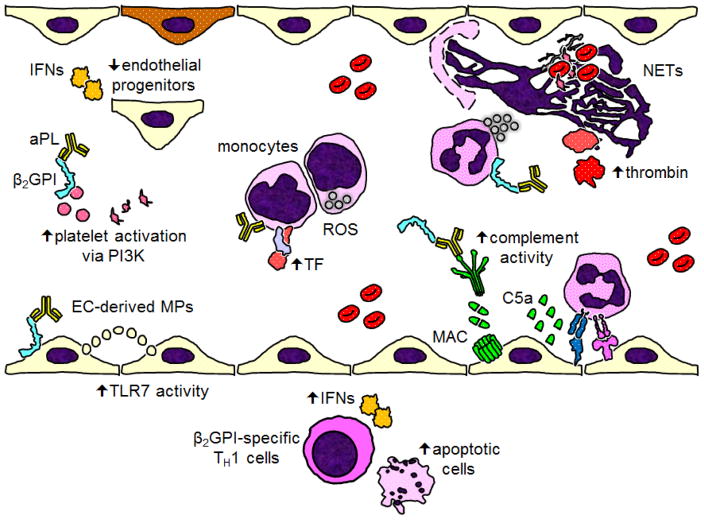
Figure 1.
Recent mechanistic insights into the pathophysiology of antiphospholipid antibodies (aPL) and APS. Starting at the bottom of the figure and moving roughly clockwise: In the vessel wall of atherosclerotic plaques, beta-2 glycoprotein I (β2GPI)-specific TH1 cells trigger cell death and release interferons (IFNs). Endothelial cells (ECs) release vesicles (like microparticles) that activate TLR7 in other ECs by delivery of single-stranded RNA. aPL-mediated platelet activation relies on phosphoinositide 3-kinase (PI3K). Type I IFNs reduce the function of restorative circulating endothelial progenitors, which may lead to the accrual of endothelial damage over time. Cofactor-independent aPL activate monocytes via endosomal reactive oxygen species (ROS), resulting in increased expression of tissue factor (TF). In response to aPL, neutrophils release neutrophil extracellular traps (NETs), which help facilitate thrombin activation. Complement activation, especially through the classical pathway, leads to the assembly of the membrane attack complex (MAC) on the endothelial surface, while also facilitating the recruitment and activation of inflammatory cells.