Abstract
In localities with combined sewer systems, combined sewer overflow (CSO) events frequently occur following high precipitation and can result in the release of untreated sewage and industrial wastewater into surface waters. We hypothesized that either direct contact with or proximity to aerosolized CSO effluent would increase the risk for childhood emergency department (ED) visits for asthma, gastrointestinal (GI) illnesses, and skin and soft tissue infections (SSTIs) in Cincinnati, OH, USA. ED visits for 2010–2014 due to GI diseases, asthma, and SSTIs were extracted from the Cincinnati Children’s Hospital Medical Center electronic health records. The location and timing of CSO events were obtained from the Metropolitan Sewer District (MSD) of Greater Cincinnati. ED visits with a residential address within 500 m of a CSO site were used in a case-control crossover study with two bi-directional control periods. Conditional logistic regression models were used to estimate the risk of an ED visit associated with a CSO event at lag periods of 0 to 7 days. Statistically significant elevated risks for GI-related ED visits was observed two (OR: 1.16 [95% CI 1.04,1.30]) days after CSO events. CSO events were not significantly associated with asthma- or SSTI-related ED visits, but show similar trends. Our findings suggest an increased risk for GI-related ED visits following CSO events among children who reside near CSO sites.
GRAPHICAL ABSTRACT
1. Introduction
Urban sewer systems are designed to collect and transport sewage, industrial wastewater, and storm water runoff to wastewater treatment facilities. Most modern sewers employ separate systems, one to collect sewage/industrial wastewater and another to collect storm water runoff. These discrete systems allow for independent transport of sewage/industrial water and storm water runoff to treatment facilities and surface waters, respectively. However, many older localities in the United States (US) and elsewhere continue to employ a combined sewer system (CSS) wherein sewage/industrial wastewater and storm water runoff are collected in one pipe for transport to treatment facilities (US EPA, 2004). A significant limitation to combined systems is the potential for the collective volume of wastewater and storm water runoff to exceed the capacity of the system during wet weather events. When this occurs, a CSS is designed to permit a portion of the untreated combined wastewater to overflow directly into nearby surface water through outfall structures. The location and discharge of untreated combined wastewater through these structures are referred to as combined sewer overflows (CSO) (Ohio EPA).
While the construction of combined sewer systems are, in general, no longer permitted in the US, existing CSO sites remain significant sources of contamination for local streams, rivers, and other bodies of water. CSO discharge, or effluent, may contain multiple pollutants including polycyclic aromatic hydrocarbons, pharmaceutical compounds, nutrients, metals, and pesticides (Gasperi et al., 2012; Phillips et al., 2012; US EPA, 2004). In addition, viruses, parasites, indicator and pathogenic bacteria (e.g. Escherichia coli, Campylobacter, and Salmonella), protozoa (including Giardia and Cryptosporidium parvum), culturable viruses, adenoviruses, and noroviruses have all been identified in CSO discharge and linked to increased concentrations of these in CSO-receiving bodies of water following overflow events (Rodriguez et al., 2012; States et al., 1997; US EPA, 2004). Untreated sewage or wastewater may also contain irritants, including endotoxins, ammonia, and other chemicals, that can prompt respiratory symptom responses including bronchoconstriction common to asthma exacerbations or affect the skin with rashes and infections (Lewis et al., 2002).
In a 2004 Report to Congress, the US Environmental Protection Agency (EPA) identified a total of 9348 CSO outfalls in 746 communities (US EPA, 2004). These communities were primarily located in the Northeast and Great Lakes regions, including Illinois, Indiana, Michigan, New York, and Pennsylvania. In Cincinnati, Ohio approximately 40% of the sewer system is a CSS that treats approximately 700 million L of sewage per day (MSD, 2017). Currently, a total of 204 CSO sites are located in Greater Cincinnati and result in approximately 43.5 billion L of untreated sewage and storm water being released annually into local waterways during overflow events (MSD, 2017). Despite the potential for microbial pathogens and chemical irritants found in CSO discharges to cause respiratory morbidity, gastrointestinal (GI) illnesses, and skin and soft tissue infections (SSTI) in humans, there is limited epidemiologic evidence of an association between residential proximity to CSO events and human health. Thus, the objective of this study was to examine the association between CSO events and child health outcomes in Cincinnati, OH. Given the unique position of Cincinnati Children’s Medical Hospital Center (CCHMC) as the only pediatric hospital in the region that cares for >80% of all pediatric ED visits in the study area, we chose to focus on children’s health. We hypothesized that, among children whose residence was near CSO sites, the risk for ED visits for asthma exacerbations, GI illnesses, and SSTIs would be significantly elevated following a CSO event compared to control periods pre- and post-CSO due to direct contact with CSO effluent, possibly through recreational activities or aerosolized irritants and pathogens.
2. Methods
2.1. Study design and population
We conducted a case-crossover study (Maclure, 1991) to investigate the association between CSO events and child health outcomes, including pediatric ED visits for asthma exacerbations (as a marker of respiratory illnesses), GI illnesses, and SSTIs. In a case-crossover study design, each case serves as its own control and is therefore matched for fixed individual characteristics including sex, age, and socioeconomic status. Control periods are defined as fixed time intervals preceding and following each case period. In our analyses, each case was denoted by the date of the ED visit and two control periods were defined as 14 days before and after the case period. We selected a 14 day “wash out” periods to limit the potential for time-varying confounders including season and temperature. For each case and control period we examined the number of CSO events within varying distances of their home address (further defined below) on the case/control date and the preceding seven days. A seven day exposure window was selected based on potential direct and indirect routes of exposure and incubation periods of probable infectious organisms. A diagram illustrating the case-crossover study design is shown in Fig. 1.
Fig. 1.
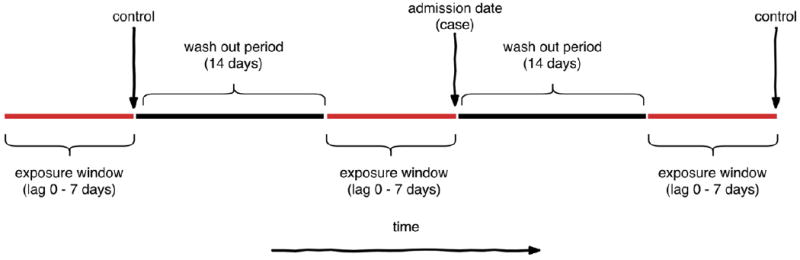
Case-crossover study design. Caseswere defined as ED visit dates and were considered to be exposed to a CSO event if the ED visit occurredwithin 7 days and 500mof a CSO event. Two bi-directional control periods for each casewere defined as 14 days before and after the case period. For each outcome, lag periods of 0 to 7 dayswere examined in order to consider varying time periods between CSO events and disease onset considering variation in exposure routes and incubation periods.
Cases were defined as pediatric (i.e. aged 0–18 years) ED visits to Cincinnati Children’s Hospital Medical Center (CCHMC) occurring between January 31, 2010 and December 9, 2014, during which time CSO monitoring data were available. Specific reasons or diagnoses related to ED visits were defined a priori for three categories of interest. Data were extracted from the electronic health record with primary diagnoses of asthma (ICD-9 code 493.xx), common infectious GI diseases (ICD-9 codes 001–009, 558.9, 787.0, 787.01, 787.03, 787.4, 787.9, 787.91), and SSTIs (ICD-9 codes 35, 376.01, 457.2, 528.5, 566, 607.2, 614.4, 680–682, 684, 686.9, 704.8). All data were obtained following review and approval of the study by the CCHMC Institutional Review Board.
2.2. Exposure to combined sewer overflow events
The locations of all CSO sites were obtained from the Metropolitan Sewer District (MSD) of Greater Cincinnati. At each CSO site real-time measurements of overflow are monitored using Telog Instruments (Victor, NY) and this data was obtained from the MSD for all CSO sites for the study period. A photograph of a CSO site and Telog Instrument monitoring device located near the Mill Creek, a CSO-receiving body of water, is shown in Fig. 2.
Fig. 2.
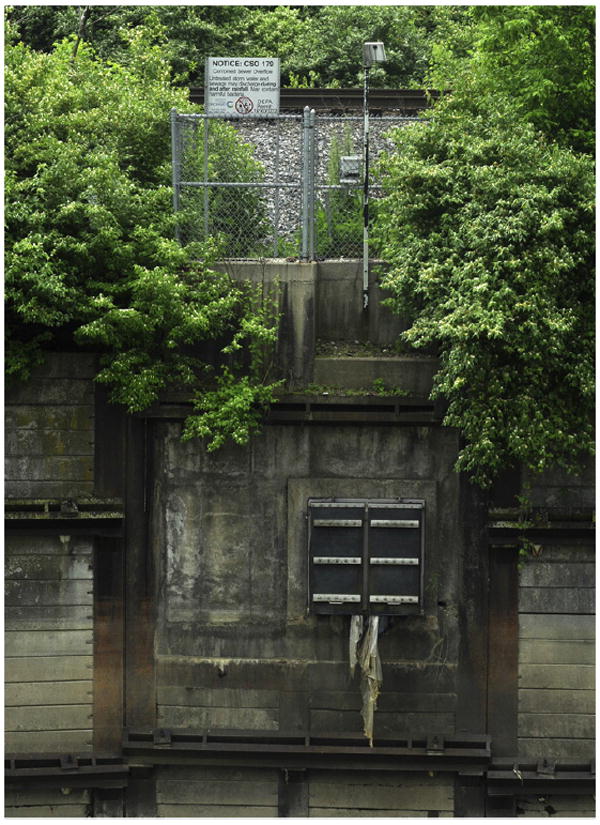
Photograph of a CSO overflow site along the Mill Creek. A wireless Telog monitor which measures CSO activity sits on top of the metal post next to a sign warning people not to recreate in the water. The sign reads “Untreated storm water and sewage may discharge during and after rainfall. May contain harmful bacteria.” The black door below is the effluent site where the overflow empties into the receiving stream just below.
For some CSO sites, the location where the effluent is discharged into the receiving surface body of water, referred to as an effluent site, is connected to the CSO site via an outfall pipe. To identify the location where effluent enters the CSO-receiving surface water and may potentially result in exposure, we identified effluent sites as the terminal end of a CSO-connected outfall pipe which lead to a surface river or stream. CSO sites not connected to an outfall pipe were considered an effluent site if the CSO site itself was located within 40 m of a receiving river or stream.
We also hypothesized a priori that the potential for exposure to CSO effluent may differ based on the characteristics of the receiving body of water and that these may modify the association between CSOs and ED visits. Therefore, each effluent site was categorized into one of the following four potential receiving bodies of water based on its location, flow rate, sidewall material, and other characteristics: (1) “Ohio River”, (2) “Mill Creek”, (3) “Little Miami River”, and (4) “Other Stream” (defined as a small stream or creek not classified into one of the first three categories). Briefly, the Ohio River is a large river that separates Ohio from Kentucky at Cincinnati, the Mill Creek is centrally located in the Cincinnati region adjacent to multiple industrial sources of waste-water, and the Little Miami River is a tributary of the Ohio River that runs to the east of Downtown Cincinnati. The location of all effluent sites as categorized by receiving stream is shown in Fig. 3.
Fig. 3.
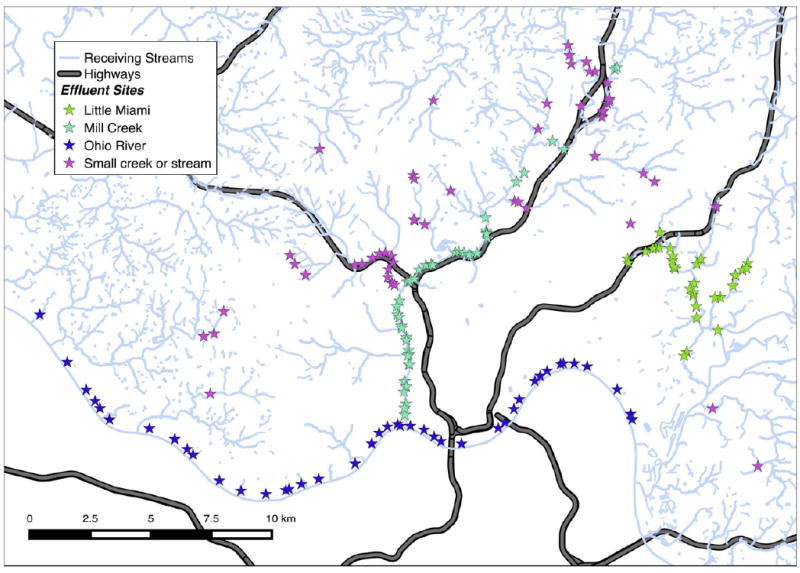
The study area of Cincinnati, Ohio, USA. The location of CSO effluent sites are represented by stars and the type of CSO effluent sites categorized by its receiving stream is are represented by the color of each star.
The home address for all study participants contributing an ED visit were extracted from electronic health records and geocoded using TIGER/Line address range files. A priori, we defined residential locations within 500 m of an effluent site as potentially exposed and these were retained for further analysis. In addition, we conducted a series of sensitivity analyses by examining home addresses located within 250, 400, 600, and 750 m of effluent sites.
2.3. Statistical analysis
The objective of the statistical analysis was to estimate the increase in odds of an ED visit for an increase in one CSO event occurring within 500 m of a participant’s home address. Given that the mechanism for morbidity may differ by diagnostic categories, we analyzed each outcome (GI, asthma, SSTI) separately. Conditional logistic regression models were estimated for each outcome using a stratified Cox model with each child assigned to their own stratum (Gail et al., 1981). For each outcome, lag periods of 0 to 7 days were chosen to examine varying time periods between CSO events and disease onset considering variation in exposure routes (e.g., direct contact) and incubation periods.
To examine whether the type of receiving stream modified the association between CSOs and health outcomes, we included an interaction term in the conditional logistic regression model between the type of receiving stream and number of CSO events. A significance test was used to determine if the interaction significantly differed from zero for every lag period of each ED visit cause group. To estimate the receiving-stream specific effects of a CSO event, the conditional logistic regression model was modified to only include the interactions between receiving stream type and number of CSO events and exclude a term for number of CSO events on its own.
Sensitivity analyses were completed by including the daily average temperature and relative humidity within the conditional logistic regression model. Weather data was retrieved from the North American Regional Reanalysis Data as a daily mean from the 32 km square grid containing the study area (Mesinger et al., 2006).
All statistical computing was done in R, version 3.1.2 (R Core Team, 2016). Geospatial calculations were done using the sp. (Pebesma and Bivand, 2005), rgeos (Bivand and Rundel, 2017), and rgdal (Bivand et al., 2016) packages and the conditional logistic regression model was created using the survival package (Therneau, 2015). Code is available from the corresponding author upon request.
3. Results
3.1. Cohort characteristics
Residential addresses were successfully geocoded for 21,108 asthma-related ED visits, 34,142 ED visits for GI disease, and 18,634 visits for SSTIs during the study period (1/31/10–12/9/14). Overall, children visiting the ED for asthma were 38% female and 53% black while children visiting the ED for GI illnesses and SSTIs were 48% and 51% female, respectively, and 32% and 36% black, respectively. Our study included only patients with a home address within 500 m of an effluent point resulting in 1169 ED visits for asthma (5.5% of all asthma visits), 1559 for GI illnesses (4.6% of all GI visits), and 980 for SSTIs (5.3% of all SSTI visits).
3.2. CSO events
There were a total of 205 active CSO sites in the study region during the study time period. Seventeen were not able to be linked to a receiving body of water by either a sewer pipe with an outfall or close proximity to a receiving body of water. Through personal communication, MSD officials (Todd Trabert and others, July 2015) hypothesized that these likely feed into another sewer system not maintained by the MSD. The 188 CSO sites that could result in effluent exposure were used for the exposure assessment and subsequent tests of association with ED visits. These were linked to 171 effluent sites (Fig. 3). Of the total 188 CSO sites, 181 fed only one effluent site and 7 CSO sites fed two different effluent sites. 157 of the 171 effluent sites were fed by only one CSO site, nine of the effluent sites were fed by two different CSO sites, and five effluent sites were fed by at least three different CSO sites. See the Supplementary information for a figure detailing the layout of a portion of the CSO sites, effluent sites, and outfall sewers.
Telog Instruments monitors at the 188 CSO sites included in the analysis recorded overflow events at 11.7% (40,309) out of 343,288 total station-days during the 2010–2014 study period. Thirteen CSO sites recorded an overflow event on at least 365 days (20% of the total 2010–2014 study period) while 27 sites experienced an overflow event on <90 days of the total study period. Only one CSO site did not experience an overflow event during the study period. Additional information regarding the number of CSO events and an interactive map displaying CSO sites is provided as an HTML file (“cso_dashboard.html”) in the Supplementary information, available online.
3.3. CSO events and ED visits
For each of the 3708 total ED visits considered, there were 24 total possible exposure days (three exposure periods—one case and two controls, each eight days long). As shown in Table 1, a total of 492 (14%) of ED visits did not have a CSO event occur during the 24 total possible exposure days. For the remaining participants, at least one CSO event occurred within 500 m of their home during an exposure period with 337 (9%) children exposed to twelve or more CSO events.
Table 1.
Number of CSO events occurring <500 m of residence during the 24 possible exposure days (three exposure periods—one case and two controls, each of eight days long).
| CSO events n | Total children n (%) |
|---|---|
| 0 | 492 (14%) |
| 1 | 365 (10%) |
| 2 | 388 (11%) |
| 3 | 390 (11%) |
| 4 | 395 (11%) |
| 5 | 366 (10%) |
| 6 | 268 (7%) |
| 7 | 223 (6%) |
| 8 | 150 (4%) |
| 9 | 111 (3%) |
| 10 | 93 (3%) |
| 11 | 64 (2%) |
| ≥12 | 337 (9%) |
Odds ratios and 95% confidence intervals for each health outcome and lag period (days 0–7) are presented in Fig. 4. Although not statistically significant, an increased risk per CSO event for an asthma-related ED visit was observed 1 and 5 days following CSO events (OR: 1.11 [95% CI: 0.98,1.25] and OR: 1.12 [0.99,1.27], respectively) while a decreased risk was observed on 2, 3, and 7 days following CSO events (OR: 0.88 [0.77,1.00], 0.83 [0.73,0.95], and 0.90 [0.79, 1.02], respectively). A statistically significant increased risk for GI-related ED visits was observed two days following the event (OR: 1.16 [1.04,1.30]). Although not statically significant, an increased risk for a GI-related asthma visit occurred five days following the event (OR: 1.07 [0.95,1.20]) while a decreased risk for GI-related ED visit was observed on day 3 (OR = 0.92 [0.82,1.04]). CSO events were associated with an increased, but not statistically significant, risk for SSTI-related ED visit three days following the event (OR: 1.06 [0.93,1.20]).
Fig. 4.
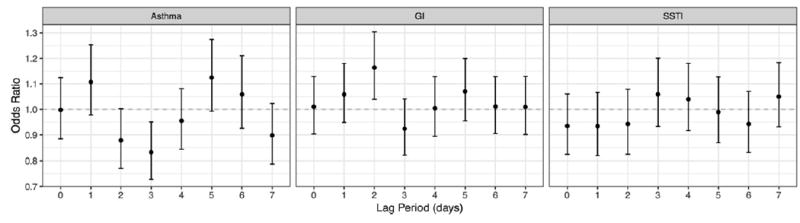
Odds ratio for visiting the ED due to an increase of one CSO event. Each panel represents different causes for ED visits and each odds ratio is from a different conditional logistic regression model utilizing the specified lag period between the CSO exposure and the observation for an ED visit
3.4. Sensitivity analysis
As a sensitivity analysis, we repeated the exposure assessment with buffer radii of 250, 400, 600, and 750 m in addition to the 500 m used in the analysis and results of the conditional logistic regression models using these radii are presented in Fig. 5. The overall patterns of odds ratios by lag time for each ED visit cause group are similar to the primary radii (500 m), although the odds ratio for SSTI-related ED visits increased significantly when using a smaller exposure buffer radius of 250 m. The resulting increase in precision, indicated by reduced confidence intervals with larger buffer radii, reflects the increased confidence in estimating odds ratios with a larger number of visits within range of a CSO site. However, the larger buffer radius might include more subjects who are not realistically exposed to CSO effluent, biasing the odds ratio towards the null, indicated by the ORs shifting towards 1 with larger buffer radii. Overall, the sensitivity analysis strengthens our findings because the shorter radii have higher odds ratio estimates.
Fig. 5.
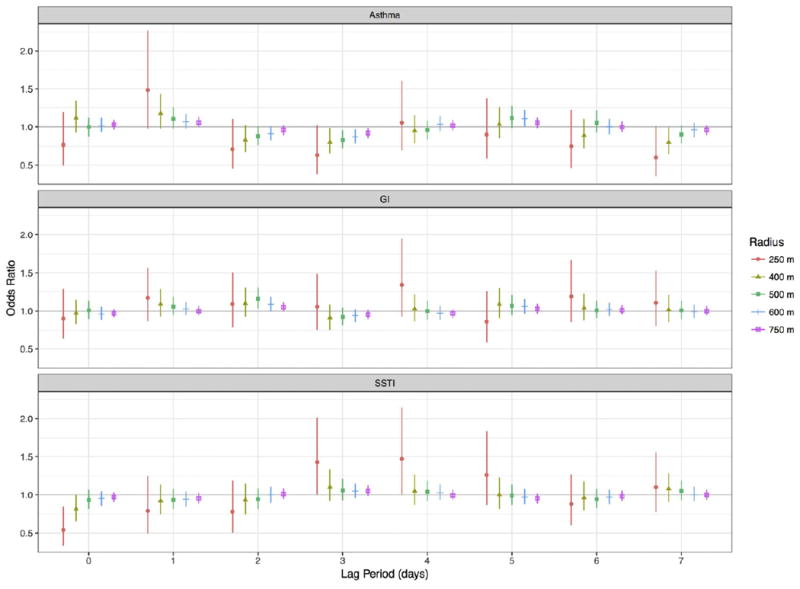
Odds ratios froma sensitivity analysis where the exposure assessmentwas repeatedwith buffer radii of 250, 400, 600, and 750min addition to the 500mused in the analysis. The resulting odds ratios and confidence intervals from the conditional logistic regression models are plotted.
As an additional sensitivity analysis, we repeated the primary analyses using 500 m buffer radii but also controlled for temperature and humidity. The overall results did not significantly change, suggesting that our findings were not biased by these temporal confounders (Supplementary information, Fig. 3).
3.5. Modification of CSO effect by type of receiving stream
To examine whether the type of receiving body of water for each CSO event modified the association between CSOs and ED visits, we classified each site by the receiving body of water (Fig. 3). Interaction terms between the type of receiving stream and number of CSO events were added to the model and were found to be significantly different from zero for every lag period of each ED visit cause group (p b 0.001). Fig. 6 shows the receiving stream specific odds ratios for each ED visit type plotted as a joined line and 95% confidence band for each lag period with the results of the analysis without the interaction term included for reference. When examining the risk for an asthma-related ED visit, the highest risk occurred one and five days after a CSO event largely driven by exposures occurring at the “Mill Creek” and “Other Stream” locations (Fig. 6). Low sample size for asthma-related ED visits and residential locations nearby “Ohio River” exposure sites (n = 77) resulted in larger confidence intervals for the estimated odds ratios. The highest risk for a GI-related ED visit occurred two and five days post CSO-overflow, primarily due to exposure occurring at “Little Miami” CSO locations.
Fig. 6.
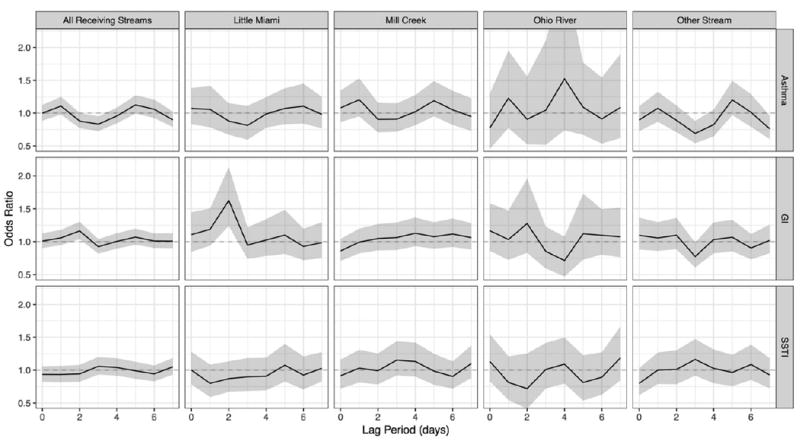
Each of the 171 effluent sites was classified as “Ohio River”, “Mill Creek”, “LittleMiami”, or “Other Stream” and an interaction term was added to the conditional logistic regression models to identify the effectmodification of the type of receiving stream on the odds of an ED visit due to an increase in one CSO event. To better illustrate the trends, the estimates at each lag period and their 95% confidence intervals are represented by a line and shaded band, respectively.
4. Discussion
To our knowledge, this is the first epidemiologic study to report an association between CSO events occurring near children’s homes and elevated risk for ED visits. We found evidence that CSO events occurring near residences were linked to childhood ED visits for GI illnesses, primarily acute gastroenteritis, 2 and 5 days post CSO events. Although our analyses do not enable us to identify the pathogen that may have precipitated a child’s symptoms, there is clear evidence linking a range of bacteria, viruses, and parasites to symptoms of diarrhea and vomiting.
Although not statistically significant, we also observed an association between CSOs and ED visits for asthma exacerbations, which suggests a potential aerosolized exposure route. Given limited evidence detailing such a link, we examined the literature for individuals commonly exposed to untreated sewage and wastewater. Smit et al. (2005) highlighted that wastewater treatment workers frequently express symptoms consistent with lower and upper respiratory symptoms, potentially due to endotoxin exposure. It is also possible that aerosolized microbes (viruses, bacteria, molds) may be present and contribute to respiratory infections triggering asthma exacerbations (Smit et al., 2005). These findings are similar to a report from Sweden that found an increased prevalence of airway symptoms among workers exposed to untreated sewage, also potentially due to endotoxin exposure (Thorn et al., 2002).
Although we did not identify a significant association between CSOs and ED visits for SSTIs, previous studies have demonstrated that swimming and recreating in urban waters (e.g., rivers, streams) can be associated with skin infections or non-specific rashes (Tondera et al., 2016). Direct contact with pathogens including Staphylococcus aureus, Streptococcus pyogenes, and/or Pseudomonas aeruginosa can lead to infections that include cellulitis, abscess, or fasciitiis (Mistry, 2013). Our lack of significant findings may be due to our examination of ED visits, as SSTIs may be commonly treated in outpatient settings other than the ED. It is also possible that other non-specific dermatitis diagnoses, not classified as SSTIs in our dataset, may have been more common.
Multiple studies have reported a significant association between heavy precipitation, frequently defined as >95th or 99th percentile, and acute GI-related illnesses (Bush et al., 2014; Carlton et al., 2014; Wade et al., 2014). Fewer studies, however, have examined the specific role of CSO events in these acute outbreaks. In a retrospective time-series analysis of rainfall and pediatric GI-related emergency department (ED) visits in Wisconsin, Drayna et al. (2010) found a significant association between rainfall events and ED visits independent of whether CSOs occurred during the period of excessive rainfall. In contrast, Jagai et al. (2015) observed a significant association between extreme rainfall events in Massachusetts and the rate of GI-related ED visits only in regions whose drinking water was exposed to CSOs. Similarly, pediatric ED visits for diarrheal illnesses were significantly increased following sewage-bypass events among children residing in areas whose drinking water originates from affected water sources (Redman et al., 2007).
Studies that have examined CSOs have primarily focused on their impact on drinking water as the primary route of exposure leading to health effects. While it is possible that participants in this study may have been exposed to CSO effluent through direct ingestion of contaminated water, the primary source of drinking water in our study region is the Ohio River upstream of CSO effluent sites. However, many CSO-receiving bodies of water are the site of recreational activities, including the Little Miami River, and we hypothesize that the observed association between CSO and GI illnesses is precipitated by direct contact of contaminated surface water. The incubation period for GI illnesses can vary from relatively short (1–2 days for Norwalk viruses) to longer and more variable. However, most occur within 5 days of contact (Tornevi et al., 2013) which is consistent with the timeline of our findings.
We also found that the type of receiving body of water modifies the association between CSO events and ED visits—this has not previously been observed. In the Cincinnati, OH region the increased odds for a GI-related ED visit was primarily due to CSO events occurring at the Little Miami River, a body of water commonly used for recreation, suggesting that exposure may occur through direct contact during recreation. When examining asthma-related ED visits, we found that the association was largely driven by exposure occurring at “other smaller streams” and the Mill Creek. These smaller receiving streams are often dry creek beds during periods of infrequent precipitation. Therefore, asthma-related ED-visits may be the result of aerosolized exposures occurring when dry creek beds are quickly filled with CSO effluent.
There are limitations to our study including the assumption that residential proximity <500 m from CSO sites represents the potential for exposure. To address this assumption, we conducted sensitivity analyses that found study results to be robust to the choice of distance to an effluent site. The increased odds ratio for SSTI-related ED visits at a smaller exposure buffer radius of 250 m also suggests that varying the distance used to define exposure may be appropriate considering potential mechanisms related to the varying health outcomes under study. For example, the mechanism of SSTI-related ED visits may be through direct contact with CSO effluent and therefore result in the observed larger effect at closer CSO proximity for SSTI-related ED visits. Another potential limitation is the use of ED visits as our primary outcome. Indeed, this may represent a more severe health event that misses more common presentations of these diseases. The use of ED visits, however, may also be considered a strength given that CCHMC is the only pediatric hospital in the region and cares for N80% of all pediatric ED visits in the study area. Finally, survivor bias may be present in our analysis given the unlikelihood that a child who visits the ED during the 8-day exposure period will revisit the ED within the same lag period. Indeed, we observed a reduction in risk, indicated by odds ratios less than one, typically observed 1–3 days following periods of increased risk (see Fig. 4 in asthma (days 1 and 5), GI (days 2 and 5), and SSTI (day 3)). As with any case-crossover study, temporal variations within an individual of possible confounders can possibly bias health associations. We were not able to control for other possible confounders at the high temporal and spatial resolution needed for our model, such as air pollution or pollen levels. However, we did complete a sensitivity analysis by controlling for humidity and temperature to mitigate the effect of possible seasonal trends in CSO events and ED visits but saw no changes in the overall results.
Our study also has some important strengths including the availability of specific home addresses for ED visits. In addition, we were able to examine CSO events directly, rather than relying upon heavy precipitation as a surrogate, using recorded measurements of CSO events. The relationship of asthma- and SSTI-related ED visits with CSO events have not been previously studied and our results warrant further studies. Finally, the case-crossover study design has been shown to be appropriate to study acute health effects associated with transient exposures due to its explicit control for sex, race, age, socioeconomic, and other potential individual confounders while using shorter lag periods to limit the influence of seasonal variability.
4.1. Conclusions
These findings have important implications for future research and policy. Future studies may gather information and biological samples at the time of ED visit to elucidate potential routes of exposure and specific causal agents of GI-related illnesses. Public health efforts may focus on neighborhoods impacted by CSO sites to alert residents of the potential for exposure. Finally, projects within the study area designed to mitigate CSO events and replace CSO infrastructure are ongoing and should consider these results when prioritizing resources.
Supplementary Material
HIGHLIGHTS.
CSO events can release untreated sewage into surface waters.
Children living within 500 m of a CSO site are at increased risk for ED visits.
CSO infrastructure could be replaced to reduce ED usage following high rainfall.
Acknowledgments
The authors would like to thank Todd Trabert of the Cincinnati Metropolitan Sewer District for assistance in obtaining CSO event data and his insightful comments on overflow events and exposure assessment as well as Jacklyn Howard for the photograph of the Mill Creek CSO site.
Funding
This work was funded, in part, through a grant from National Institutes of Health [grant number 1K23AI112916].
Footnotes
Competing financial interests declaration: The authors have no competing financial interests to declare.
Appendix A. Supplementary data
Online Supplement: The Supplementary information contains interactive HTML tables and maps describing the CSO locations and events, as well as more detailed information on the choice of buffer radius and linking of effluent sites to combined sewer overflow sites. Supplementary data associated with this article can be found in the online version, at http://dx.doi.org/10.1016/j.scitotenv.2017.07.104.
References
- Bivand R, Keitt T, Rowlingson B. rgdal: Bindings for the Geospatial Data Abstraction Library. R Package Version 1.2-5. 2016 https://CRAN.R-project.org/package=rgdal.
- Bivand R, Rundel C. rgeos: Interface to Geometry Engine-Open Source (GEOS) R Package Version 0.3-22. 2017 https://CRAN.R-project.org/package=rgeos.
- Bush KF, O’Neill MS, Li S, Mukherjee B, Hu H, Ghosh S, et al. Associations between extreme precipitation and gastrointestinal-related hospital admissions in Chennai, India. Environ Health Perspect. 2014;122:249–254. doi: 10.1289/ehp.1306807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlton EJ, Eisenberg JN, Goldstick J, Cevallos W, Trostle J, Levy K. Heavy rainfall events and diarrhea incidence: the role of social and environmental factors. Am J Epidemiol. 2014;179:344–352. doi: 10.1093/aje/kwt279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drayna P, McLellan SL, Simpson P, Li S, Gorelick MH. Association between rainfall and pediatric emergency department visits for acute gastrointestinal illness. Environ Health Perspect. 2010;118(10):1439–1443. doi: 10.1289/ehp.0901671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gail MH, Lubin JH, Rubinstein LV. Likelihood calculations for matched case-control studies and survival studies with tied death times. Biometrika. 1981 Dec 1;:703–7. [Google Scholar]
- Gasperi J, Zgheib S, Cladiere M, Rocher V, Moilleron R, Chebbo G. Priority pollutants in urban stormwater: part 2—case of combined sewers. Water Res. 2012;46(20):6693–6703. doi: 10.1016/j.watres.2011.09.041. [DOI] [PubMed] [Google Scholar]
- Jagai JS, Li Q, Wang S, Messier KP, Wade TJ, Hilborn ED. Extreme precipitation and emergency room visits for gastrointestinal illness in areas with and without combined sewer systems: an analysis of Massachusetts data, 2003–2007. Environ Health Perspect. 2015;123(9):873–879. doi: 10.1289/ehp.1408971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis DL, Gattie DK, Novak ME, Sanchez S, Pumphrey C. Interactions of pathogens and irritant chemicals in land-applied sewage sludges (biosolids) BMC Public Health. 2002;2(1):11. doi: 10.1186/1471-2458-2-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol. 1991 Jan 15;133(2):144–153. doi: 10.1093/oxfordjournals.aje.a115853. [DOI] [PubMed] [Google Scholar]
- Mesinger Fedor, DiMego Geoff, Kalnay Eugenia, Mitchell Kenneth, Shafran Perry C, Ebisuzaki Wesley, Jović Dušan, et al. North American regional reanalysis. Am Meteorol Soc. 2006;87(3):343–360. [Google Scholar]
- Metropolitan Sewer District of Greater Cincinnati (MSD) Project Groundwork: Your Pipeline to Clean Water. [January 23, 2017];2017 Available: http://projectgroundwork.org/index.htm.
- Mistry RD. Skin and soft tissue infections. Pediatr Clin N Am. 2013;60(5):1063–1082. doi: 10.1016/j.pcl.2013.06.011. http://dx.doi.org/10.1016/j.pcl.2013.06.011. [DOI] [PubMed] [Google Scholar]
- Ohio Environmental Protection Agency (Ohio EPA) [January 23, 2017];2013 http://www.epa.ohio.gov/dsw/cso/csoindex.aspx#116135669-what-is-a-combined-sewer.
- Pebesma EJ, Bivand RS. Classes and methods for spatial data in R R News. 2005;5(2):9–13. [Google Scholar]
- Phillips PJ, Chalmers AT, Gray JL, Kolpin DW, Foreman WT, Wall GR. Combined sewer overflows: an environmental source of hormones and wastewater micropollutants. Environ Sci Technol. 2012;46:5336–5343. doi: 10.1021/es3001294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redman RL, Nenn CA, Eastwood D, Gorelick MH. Pediatric Emergency Department Visits for Diarrheal Illness Increased After Release of Undertreated Sewage. 2007;120(6):1472–1475. doi: 10.1542/peds.2007-0283. [DOI] [PubMed] [Google Scholar]
- Rodriguez RA, Gundy PM, Rijal GK, Gerba CP. The impact of combined sewage overflows on the viral contamination of receiving waters. Food Environ Virol. 2012;4(1):34–40. doi: 10.1007/s12560-011-9076-3. [DOI] [PubMed] [Google Scholar]
- Smit LA, Spaan S, Heederik D. Endotoxin exposure and symptoms in wastewater treatment workers. Am J Ind Med. 2005;48(1):30–39. doi: 10.1002/ajim.20176. [DOI] [PubMed] [Google Scholar]
- States S, Stadterman K, Ammon L, Vogel P, Baldizar J, Wright D, et al. Protozoa in river water: sources, occurrence, and treatment. J Am Water Works Assoc. 1997;89(9):74–83. [Google Scholar]
- R Core Team. R: a Language and Environment for Statistical Computing. R Foundation for Statistical Computing; Vienna, Austria: 2016. (URL https://www.R-project.org) [Google Scholar]
- Therneau T. A Package for Survival Analysis in S. R Package Version 2.38. 2015 (URL https://CRAN.R-project.org/package=survival)
- Thorn J, Beijer L, Rylander R. Work related symptoms among sewage workers: a nationwide survey in Sweden. Occup Environ Med. 2002;59(8):562–566. doi: 10.1136/oem.59.8.562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tondera K, Klaer K, Roder S, Brueckner I, Strathmann M, Kistemann T, et al. Developing an easy-to-apply model for identifying relevant pathogen pathways into surface waters used for recreational purposes. J Hyg Environ Health. 2016;219(7):662–670. doi: 10.1016/j.ijheh.2015.11.005. http://dx.doi.org/10.1016/j.ijheh.2015.11.005. [DOI] [PubMed] [Google Scholar]
- Tornevi A, Axelsson G, Forsberg B. Association between precipitation upstream of a drinking water utility and nurse advice calls relating to acute gastrointestinal illnesses. PLoS One. 2013;8(7):e69918. doi: 10.1371/journal.pone.0069918. http://dx.doi.org/10.1371/journal.pone.0069918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade TJ, Lin CJ, Jagai JS, Hilborn ED. Flooding and emergency room visits for gastrointestinal illness in Massachusetts: a case-crossover study. PLoS One. 2014;9(10):1–9. doi: 10.1371/journal.pone.0110474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Environmental Protection Agency (US EPA) Report to Congress on Impacts and Control of Combined Sewer Overflows and Sanitary Sewer Overflows. [January 23, 2017];2004 (Available: https://www.epa.gov/npdes/2004-npdes-cso-report-congress.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


