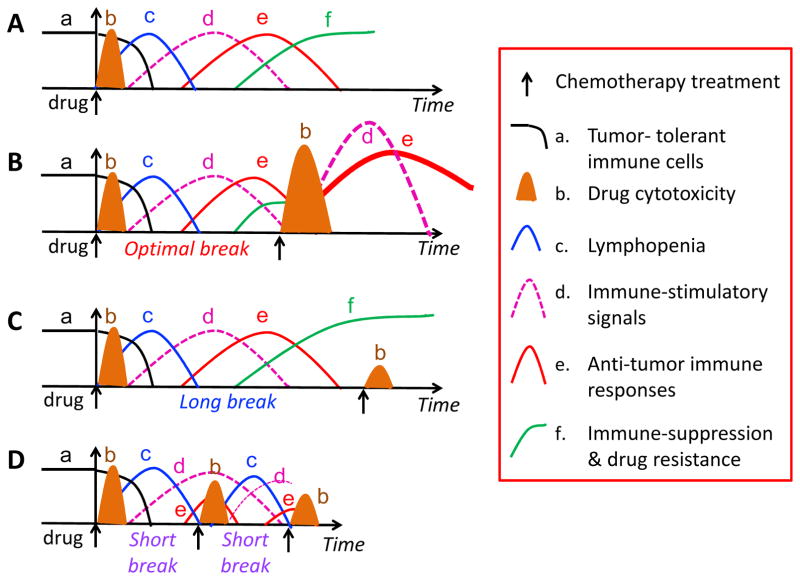
Fig. 2. Chemo-immunotherapy schedules.
(A) A single injection of a cancer chemotherapeutic drug may induce multiple events, including changes in the number of tumor-tolerant immune cells (a, black line), chemotherapy treatment-induced drug cytotoxicity (b, brown cone), which is often followed by lymphopenia (c, blue line) and immune-stimulatory signals (d, pink line). The immune stimulatory signals activate anti-tumor immune responses (e, red line), which are followed by increased immune suppression and drug resistance (f, green line). (B) An optimal drug-free break allows for an overall increase in anti-tumor immune response. A second treatment with chemotherapy may have greater effect than the first treatment due to synergism with the anti-tumor immune responses activated by the first drug treatment, and can circumvent or interrupt the emergence of immune suppression. (C) A drug-free break that is too long may enable the development of immune suppression and the emergence of drug resistance, thereby countering the effectiveness of the second drug treatment; (D) A drug-free break that is too short ablates anti-tumor immune responses prematurely, thereby reducing the efficacy of subsequent treatments with chemotherapy.