Summary
Objectives
The objective of this study is to evaluate the feasibility, participation, preliminary efficacy and retention in a couples‐based weight loss intervention among Black men.
Design, setting, participants
Two‐arm pilot randomized clinical trial in an academic clinical setting. Forty self‐identified Black men and their female cohabitating partners (n = 80) aged 18 to 65 years with body mass index from 25 to 45 kg/m2 were randomized using computer generated tables to allocate treatments.
Intervention
Participants were randomized to a standard behavioural weight loss (Standard) programme or the Standard programme plus partner involvement (Enhanced). Both interventions focused on calorie reduction, physical activity and self‐monitoring to facilitate weight loss. Enhanced included couples skills training and couple's communication components.
Main outcome and measures
Changes in weight from baseline to 3 months among men. Partner weight loss (secondary).
Results
Forty Black couples (men mean [SD] age, 47.4[11] years; body mass index, 35.0[6.1]), were recruited. Retention was 100% of the men and 98% of female partners. Attendance at group sessions was 63–73%. Between groups, mean (SD) weight changes among men were −3.4[.04] and −4.7[5.9] kg (p = 0.57) and among women −0.23[4.46] and −2.47[3.62] kg (p = 0.09), in the standard and enhanced groups.
Conclusions
Weight losses from an intervention enhanced by partner involvement and an intervention with no partner involvement were not different. Treatment choice can be based on preference rather than outcome as both treatments are effective in producing clinically significant percent weight loss.
Trial registration Clinical Trials NCT02458053.
Keywords: African Americans, Male, Social support, Weight loss
Introduction
According to the Office of Minority Health, 70% of Black men age 20 and older are overweight and obese (body mass index [BMI] >25 and >30, respectively) 1. Although preventive or routine visits could prevent or reduce many health problems, Black men are less likely to seek treatment for obesity‐related conditions, 2, 3, 4, 5 compared with both White men and Black women. This contributes to disparities in morbidity and mortality of the top chronic diseases in the population. Differences in health behaviours contribute partly to these health inequalities among Black men.
Little is known about how to produce higher levels of weight loss among this population because few studies include data on Black men in sufficient quantities to enable evaluation of their weight related behaviours and outcomes. In several landmark weight loss trials, Black men achieved an initial weight loss of 3–7% at 6 months, which would likely be of a level that would confer cardiovascular disease benefit.6, 7, 8 Unfortunately, Black men represented only 4–12% of the total study population of these studies and lost less weight than Whites. In a published review of interventions reporting weight loss, diet or physical activity among Black men, only four studies were specifically designed for Black men; only one of these interventions was a randomized controlled trial, and none of the studies had weight change as the primary outcome demonstrating the paucity of published weight loss interventions both attracting and developed for this population. 9
To address ineffective engagement of and reduced efficacy in a population, Castro et al. suggest cultural adaptation of evidence‐based interventions.10 The Centers for Disease Control supports these findings for Black men, emphasizing the need for cultural competence in programme design and implementation as a vehicle to produce effective communication between care provider and participant/patient. 11 Addressing the sociocultural needs of both being a male and being Black in strategies and programme designs may be important.
Family is culturally valued in the Black community; family provides consistent social connections that lay the foundation for exchange of social support.12, 13, 14, 15 Moreover, family members, specifically partners, can reinforce strategies and behaviours for the targeted individual. Research suggests that romantic relationships have influence on weight management and provide a potential unit of intervention.16 Spousal support, defined as support from a spouse or romantic partner, is naturally occurring, and is associated with adopting new health behaviours and with short‐term and long‐term weight loss. 17
Previous studies among adults have used a spousal support‐based approach for promoting weight loss in the general population. In one review of couples‐based weight loss interventions, inconsistent findings were reported, with some studies suggesting advantages to partner inclusion and others not supporting a couples‐based approach.18 Intervention strategies focused on improving spousal support included partner attendance at group sessions, signing commitment contracts, self‐monitoring behaviours and providing encouragement and modelling. In these studies, participants were majority White women leaving questions regarding the findings generalizability to men and non‐White populations. However, a weight loss study for Black adults found no difference in weight change when assigned to participate with a family member or friend. Interestingly, of the 130 pairs, only 18% were romantic couples as opposed to friends or family.13 Thus, this study does not provide sufficient data to evaluate the effect of a couples‐based approach among Blacks. The importance of support in changing behaviours and the value of family reported by this population suggest a couples' approach as a promising strategy that should be evaluated, both for attracting Black men to participate and for promoting weight loss. To date, no study has used spouses or partner to provide social support for weight loss among Black men.
This current paper describes Together Eating & Activity Matters (TEAM): a 12‐week randomized clinical pilot study for weight loss among Black men testing whether adding a spousal support component to a standard behavioural intervention produces greater weight loss compared with the standard behavioural weight loss treatment alone. The group with the added spousal support component was hypothesized to have greater percent weight loss at 12 weeks compared with a standard behavioural weight loss group. Thus, this study evaluated the feasibility, participation, preliminary efficacy and retention in a couples‐based weight loss intervention among Black men.
Methods
Design overview
TEAM was a two‐arm randomized controlled pilot study conducted at the University of North Carolina Weight Research Programme in Chapel Hill, North Carolina. Each participant was provided with 12 weeks of weight loss intervention and participated in two assessments, one at baseline (up to 2 weeks before treatment) and one at follow‐up (up to 2 weeks after treatment.)
Recruitment
Potential participants (n = 73) were screened through the study website for approximately 7 months. Participants were recruited from community organizations, universities, churches and fraternities through brochures, listservs, flyers and referrals and face‐to‐face engagement. Eligible participants were self‐identified as a Black male, between 18 and 65 years of age, with a BMI of 25–45 kg/m2 and with access to the Internet and a personal email at least twice a week. The exclusion criteria were current enrolment in a weight loss programme, having lost 10 lb or more in the last 6 months, currently being treated for cancer, being diagnosed with type 1 diabetes and taking medications that affects body weight (e.g. insulin and chronic steroid use). Participants were ineligible if self‐reported a diagnosis of schizophrenia, bipolar disorder or being hospitalized for psychological reasons. Participants had to live with their self‐identified Black female spouse or cohabiting intimate partner, who also had to agree to participate in the study. Eligibility was assessed using an online screener. Eligible participants and their partners e‐signed informed consent forms and completed baseline questionnaires online. In‐person orientations conducted with each couple included signing paper informed consents, physical/clinical baseline assessments and random assignment to the enhanced treatment (spousal support enhanced behavioural weight loss) or standard treatment (standard behavioural weight loss) group. The study protocol was approved by the Institutional Review Board at the University of North Carolina at Chapel Hill.
Randomization
Participants were randomly allocated 1:1 to the enhanced or standard group. Before randomization, partners agreed to attend group sessions with partners and accept randomization in the informed consent form. The randomization sequences were generated by a protocol using the Rand function in Microsoft Excel using unique participant identification numbers. This study included four cohorts of participants; cohort inclusion was based on the time of enrolment. Twenty participant identification numbers were randomized per cohort. Randomizations were performed by a UNC Weight Research staff not affiliated with the study. During individual orientations, the randomization process and probability of assignment to each group were explained to participants. Group assignment was revealed to the participant and their partner through sequentially labelled opaque envelopes prepared by staff. Participants selected the next available envelope to reveal assignment.
Intervention
One interventionist delivered both study treatments that were adapted specifically for this population from a variety of studies conducted by the UNC Weight Research Centre,19, 20, 21, 22, 23 based largely on the Diabetes Prevention Programme and Look AHEAD interventions. Table 1 presents intervention components. Both groups received seven face‐to‐face group sessions over 12 weeks, each lasting 60 min (four weekly session in the first 4 weeks, two bi‐weekly sessions in the second 4 weeks and one session during the last 4 weeks.) In each session, a behavioural topic was presented; participants discussed barriers and facilitators to meeting weekly goals, and group and individual activities were completed. Group session topics aligned with emailed weekly lessons. Weekly emailed lessons presented standard behavioural weight loss topics and tips; the seven group sessions covered key concepts covered in emailed lessons over the previous 1 or 2 weeks. Participants monitored daily weight, dietary intake and physical activity using the free web/smartphone based calorie counter, diet and exercise journal, MyFitnessPal. At baseline, all participants received an exercise plan based on their baseline minutes of physical activity, a caloric prescription based on weight at baseline; prescriptions were designed to help participants lose 1–2 lb per week. Each week, progress on individual goals was assessed, and feedback was provided in group sessions and by email by the group facilitator. Feedback and weekly lessons were provided in separate emails. All participants received a programme notebook and a digital scale. Each treatment recommended that participants weigh themselves and track weight daily.
Table 1.
Intervention Components, Concepts/Constructs Targeted, Method & Strategies
| Intervention component | E | S | Concept/construct targeted: method | Strategy |
|---|---|---|---|---|
| Couples Skill Building Session | X | – | TM: Communication | Couples participate in partner activities to build communication skills and complete a workbook with information on improving communication skills (Listener‐Speaker) and activities. |
| X | – | TM: Commitment | Couples sign a Commitment Contract committing to each other, weight loss and the TEAM programme. | |
| X | – | TM: Scenario‐based risk information (change awareness and risk perception) | Couples are introduced to a fictional couple or man with similar health profile. | |
| X | – | CC: Problem coping strategy (Cognitive) | Couples participate in partner activities to build coping skills and complete a workbook. | |
| X | – | CC: Emotional coping strategy (proactive, anticipatory, preventive, reactive‐ downward comparison, avoidance, support seeking) | Couples participate in partner activities to build coping skills and complete a workbook | |
| X | – | SS: Communication | Couples participate in scenario activities requiring using communication skills. | |
| X | ‐ | SS: Problem solving | Couples participate in scenario activities requiring collaborate problem solving. | |
| X | – | SS: Skills training | Couples participate in workshop practicing providing various forms of support in real life scenarios. | |
| Group sessions | ||||
| X | – | TM: Fear arousal scenario‐based risk information (change awareness and risk perception) | Couples participate in group scenario based activities focused on diet, exercise and weight loss topics. | |
| X | – | CC: Problem coping strategy (Cognitive) | Couples participate in group scenario based activities focused on diet, exercise and weight loss topics. | |
| X | – | CC: Emotional coping strategy (proactive, anticipatory, preventive, reactive‐downward comparison, avoidance, support seeking) | Couples participate in group scenario based activities focused on diet, exercise and weight loss topics. | |
| X | X | SE: Mastery experience | Participants practice skills and techniques during session i.e. self‐ monitoring, refusal, reward, and goal setting. | |
| X | X | SE: Modelling | Group facilitator presents material providing examples of desired behaviours i.e. lecture, video, speak guest. Group discussion among peers provides opportunity to display modelled behaviour. | |
| X | X | SE: Verbal persuasion | Group facilitator presents material highlighting desired behaviour. Group discussion among peers provides opportunity to discuss success stories/experiences. | |
| X | X | SE: Guided practice | Participants practice skills and techniques during session under the supervision/guidance of trained staff. | |
| X | X | SR: Goal setting | Participants set diet, activity and physical activity goals during session. (Can share with group if desired‐accountability, reinforcement). | |
| X | X | SR: Enlisting social support | Participants participate in scenario‐based activities requiring decisions on when, how and what support to provide. | |
| X | – | SS: Persuasive communication | Participants attending with partners learn and practice techniques to influence partners through communication. | |
| X | – | SS: Modelling | Lecture/discussion | |
| X | – | SS: Problem solving | Activities | |
| X | – | SS: Skills training | Participants learn skills with partners. | |
| Behavioural lessons | ||||
| 12 weekly behavioural lessons | X | X | BC: Facilitation | Participants are provided with a reference tool composed of all lessons, techniques, tips, etc. to be successful in weight loss attempt and maintenance. |
| Couples At‐Home Activities | ||||
| 12 weekly couple activities | X | – | SS: Skill building | Participants are provided with short entertaining weekly activities to practice closeness and communication. |
| Tailored emails | ||||
| Tailored feedback on weight loss progress | X | X | R: Feedback | Participants receive weekly emails providing feedback on their previous week's diet, activity and weight loss goal. |
| Tailored feedback on dietary and physical activity behaviours | X | X | SR: Feedback | Participants receive weekly emails providing feedback on their previous week's diet, activity and weight loss goal. |
| Diary (Food and physical activity)‐online/mobile | ||||
| MyFitnessPal | X | X | SE: Mastery experience | Participants record diet and activity daily on electronic diary. |
| X | X | SR: Self‐monitoring | Participants record diet and activity daily on electronic diary. |
BC, Behavioural Capability; CC, Communal Coping; E, Enhanced group; R, Reinforcement; S, Standard group; SE, Self‐ Efficacy; SR, Self‐Regulation; SS, Social Support; TM, Transformation of Motivation.
Participants in the enhanced spousal support group attended one Couples Skills Training session with their partners prior to beginning the standard behavioural weight loss group sessions. Training consisted of signing commitment contracts, communication exercises and honing collaborative problem‐solving skills using scenarios. Weight loss was not required of spouse/partners; however, partners were given weight goals, exercise plans and calorie prescriptions upon request. Each lesson included a section devoted to at‐home couples' activities and supplemented the one session Skills Training; each weekly lesson included an additional section entitled ‘Just the Two of Us’. This section provided a weekly ‘to‐do’ list to be completed as a couple, targeting the core concepts of the Couples Skills Training: commitment, communication and social support. The ‘to‐do’ lists consisted of tasks reinforcing the lesson of the week (e.g. Week 4 Get FITT‐ Commit: Chat about the role physical activity plays in your relationship). Couple counselling materials were developed using content and activities used in family/couple counselling. The workbook provided during the Skills Training session was reviewed and evaluated by a social support expert and a family weight loss among minority populations expert in the research group. In group sessions, couples were encouraged to complete in‐class activities together (e.g. modifying a favourite recipe) and share obstacles and successes as a couple to the group during the open discussion.
Participants in the standard group attended group sessions without partners, and lessons did not include couples' activities.
Measures
Participants completed a physical measurement and online questionnaires at baseline and 12 weeks. To improve retention, participants were provided a $40 check and two (2) free personal training sessions at a local fitness centre (given at week 12). The main components of the physical examination included body weight, height, waist circumference and blood pressure. Current minutes of moderate to vigorous physical activity were assessed using the Paffenbarger Physical Activity Questionnaire. The Paffenbarger included items about minutes of brisk walks, number of flights of stairs climbed and type and duration of sports and recreation activities in the last previous week. Dietary intake was assessed using two 24‐h dietary recalls using the Automated Self‐Administered 24‐h dietary recall (ASA 24‐2014) at baseline and week 12.
The primary outcome was weight change expressed as kilogram lost and as the percent of initial body weight lost from baseline to post‐intervention (week 12). Body weight (kg) was assessed using a digital scale at the UNC Weight Research Centre at baseline and at 6 and 12 weeks wearing light clothing and no shoes. Two readings were recorded to the nearest 0.1 kg at the time of assessment. If two measurements were not within 0.2 kg, a third measure was taken.
Secondary outcomes included changes in weekly energy expenditure and daily caloric intake from baseline to week 12. Partner's weight change was also measured from baseline to post‐intervention as a secondary outcome.
Adherence was measured by logging attendance at group sessions and recording frequency of self‐monitoring of weight, dietary intake and physical activity. Self‐monitoring frequency was assessed by accessing participants' MyFitnessPal accounts and recording the number of days per week of entries of weight and each behaviour.
Statistical analysis
This study was designed as a preliminary investigation to test the effect of spousal support on weight loss. Experimental, quasi‐experimental and observational studies were used to estimate the sample size. The studies took into account several factors: treatment duration, intervention arms and target population (male and Black). Given the weight loss differences in previous studies ranged from 1.1 to 4.4 kg, the treatment durations ranged from 6 weeks to 6 months, and the use of an active comparison group was variable, a difference in weight loss of 2.5 kg was chosen as an indicator of additional clinical benefit. 13, 24, 25 With 80% power, a total of 20 participants per group allowed a 2.5 kg difference to be detected between groups at 3 months with a standard deviation of 2.75 kg. The sample size reflects only male participants; a total of 40 couples (80 total measured participants) were recruited reflecting male participants and their partners.
Descriptive statistics of baseline characteristics and comparison between study groups were evaluated using chi‐square and t‐tests. For analysis of the primary outcome, t‐tests and effect sizes were calculated for difference between groups at 12 weeks. Given the small sample size, frequency distribution of percent weight loss was also calculated. For analysis of secondary outcomes, chi‐square and t‐tests were conducted for categorical and continuous variables, respectively. Fischer's exact test and Wilcoxon's Signed Rank were used when appropriate. To assess change, change scores were calculated from differences from baseline to 12 weeks on each variable. There are no adjustments for baseline variables. sas software (Version 9.4, SAS Institute, Cary, NC) was used for all analyses.
Results
Baseline characteristics and enrolment
Seventy‐three Black men and their partners were screened over a 7‐month period of recruitment. Twenty‐four of 73 (32.9%) were ineligible, 49 were invited to an orientation; 40 completed baseline assessments and were randomized to the two treatment groups (Figure 1). Table 2 shows baseline characteristics by study group. Participants were on average 47.3 years old (±11), obese (BMI of 35.0 kg/m2 [±6.1]), and had a baseline weight of 112.7 kg (±22.8). Most participants reported being married (90%). Most men had at least a 4‐year college degree (67.5%), worked full time (85%) and had a yearly income of $60,000 or more (60%). Based on self‐reported measures, less than half had high blood pressure (42.5%), high triglyceride/cholesterol (27.5%) and few reported heart disease (2.5%). At baseline, participants reported an average caloric intake of 2219.0 kcal per day (±1037.2) and 100.4 min (±121.8) of moderate to vigorous activity per week. There were no significant differences in baseline characteristics between the intervention and comparison group.
Figure 1.
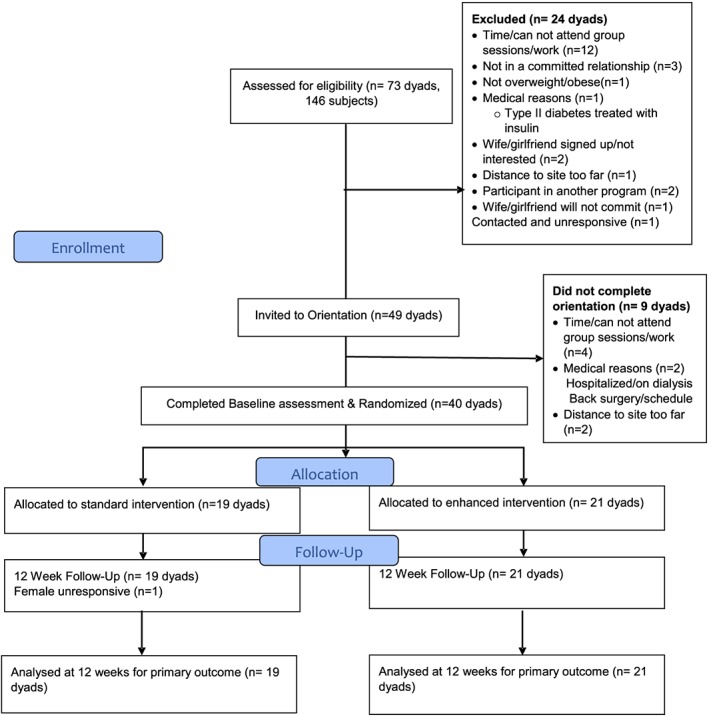
CONSORT participant flow diagram for randomized clinical pilot: Together Eating & Activity Matters Trial
Table 2.
Baseline characteristics of TEAM participants (men, n = 40)
| Variable | All (n = 40) | Standard treatment (n = 19) | Enhanced (n = 21) | p‐value |
|---|---|---|---|---|
| Age, years, n ± SD | 47.4 ± 11 | 46.0 ± 12 | 49.0 ± 10 | 0.43 |
| Education level, n (%) | 0.91 | |||
| Less than college | 13 (32.50) | 6 (31.58) | 7 (33.33) | |
| College or more | 27 (67.50) | 13 (68.42) | 14 (66.67) | |
| Marital Status, n (%) | 0.33* | |||
| Married | 36 (90.0) | 16 (84.21) | 20 (95.24) | |
| Living with partner | 4 (10.0) | 3 (15.79) | 1 (4.76) | |
| Employment, n (%) | 0.21* | |||
| Working full‐time | 34 (85.0) | 15(78.95) | 19 (90.48) | |
| Working not full‐time | 6 (15.0) | 4(21.05) | 2 (9.52) | |
| Income, n (%) | 0.41* | |||
| Less than $60,000 | 12 (30.0) | 6 (31.58) | 6 (28.57) | |
| $60,000 or more | 24 (60.0) | 10 (52.63) | 14 (66.67) | |
| Prefer not to answer | 4 (10.0) | 3 (15.79) | 1 (4.76) | |
| Tobacco user, n (%) | 1.00* | |||
| Yes | 1 (2.50) | 0 (0) | 1 (4.76) | |
| No | 39 (97.50) | 19 (100) | 20 (95.24) | |
| Weight, kg, n ± SD | 112.7 ± 22.8 | 114.2 ± 20.8 | 111.3 ± 24.9 | 0.69 |
| BMI, kg/m2, n ± SD | 35.0± 6.1 | 35.2± 6.2 | 34.9± 6.2 | 0.85 |
| Energy intake, kcal/dayb, n ± SD | 2219.0± 1037.2 | 2344.8 ± 1171.3 | 2099.8 ± 908.3 | 0.48 |
| Energy expenditure, kcal/week | 938.6 ± 1387.2 | 1423.4 ± 1822.0 | 500.0 ± 582.7 | 0.05 |
| Marital satisfaction | 25.7± 8.1 | 25.6 ± 8.0 | 25.8 ± 8.4 | 0.96 |
| Comorbid conditions, n (%) | ||||
| Diabetes | 0.65* | |||
| 1 = Yes | 5 (12.50) | 3 (15.79) | 2 (9.52) | |
| 2 = No | 35 (87.50) | 16 (84.21) | 19 (90.48) | |
| High blood pressure | 0.55 | |||
| 1 = Yes | 17 (42.50) | 9 (47.37) | 8 (38.10) | |
| 2 = No | 23 (57.50) | 10 (52.63) | 13 (61.90) | |
| High triglycerides/cholesterol | 0.58 | |||
| 1 = Yes | 11 (27.50) | 6 (31.58) | 5 (23.81) | |
| 2 = No | 29 (72.50) | 13 (68.42) | 16 (76.19 | |
| Heart disease | 0.48* | |||
| 1 = Yes | 1 (2.50) | 1 (5.26) | 0 (0) | |
| 2 = No | 39 (97.50) | 18 (94.74) | 21 (100) | |
| Cancer | ||||
| 1 = Yes | 0 (0) | 0 (0) | ||
| 2 = No | 40 (100) | 19 (100) | 21 (100) | |
TEAM, Together Eating & Activity Matters.
Total: n = 36 (standard: n = 19; enhanced: n = 17).
Fisher's Test ‘%’ of the cells have expected counts less than 5. Chi‐square not be a valid test.
Retention and adherence
At 12 weeks, 100% of physical measures and 95% of online assessments for the male participants were completed; there were no differences in completion rates among groups. No adverse events were reported during the course of the study. At 12 weeks, 97.5% of female participants completed the physical measurement.
Among the enhanced group, 85.7% of couples attended the initial Couples Skills Training session. Male participants attended 63% (mean = 4.4 [2.5]; median = 5) and 73% (mean = 5.1 [1.9]; median = 6) of seven possible group weight loss sessions in the standard and enhanced group, respectively. There was no difference in attendance among groups (t = −1.03, p = 0.31). The average number of days of self‐weighing was low; 19 and 23 days of the 90 days prescribed, among the standard and enhanced groups, respectively. There was no difference in weighing frequency among groups (t = −0.55, p = 0.58). Mean days of calorie tracking among male participants was also low 29 and 31 out of 90 prescribed days in standard and enhanced groups, respectively, with no significant difference between groups (t = −0.72, p = 0.47). Out of 90 prescribed days, the average number of days of activity tracking was 18 in the standard group compared with 16 days in the enhanced group. No differences were observed between groups (t = 0.22, p = 0.77) (Table 3).
Table 3.
Recruitment and adherence to assessments, group session attendance and self‐monitoring
| Variable | All (n = 40) | Standard (n = 19) | Enhanced (n = 21) | p‐value |
|---|---|---|---|---|
| Recruitment, n (%) | 0.67 | |||
| Passive (email, website, flyer) | 14 (35.0) | 6 (31.58) | 8 (38.10) | |
| Active (another participant, face‐to‐face) | 26 (65.0) | 13 (68.42) | 13 (61.90) | |
| Clinic visit completion, n (%) | ||||
| 6 weeks | 30 (75.0) | 13 (68.42) | 17 (80.95) | 0.36 |
| 12 weeks | 19 (100) | 21 (100) | ||
| Online survey completion, n (%) | ||||
| 6 weeks | 27 (67.50) | 11 (57.89) | 16 (76.19) | 0.22 |
| 12 weeks | 38 (95.00) | 17 (89.47) | 21 (100) | 0.22 |
| Session attendance | ||||
| Couples training, n (%) | – | 18 (85.71) | ||
| Male Weekly Sessions, n (SD) | ||||
| Mean days | 4.8 ± 2.2 | 4.4 (2.5) | 5.1 (1.9) | 0.31 |
| Couple Attendance, n (SD) | ||||
| Mean days | – | 4.8(1.8) | ||
| Self‐monitoring, n (SD) | ||||
| Self‐weighing frequencya | ||||
| Mean days | 21.1 ± 24.4 | 18.7 ± 23.27b | 23.10 ± 25.59 | 0.59 |
| Dietary tracking frequencya | ||||
| Mean days | 34.63 ± 27.68 | 31.0 ± 25.51b | 37.57 ± 29.62 | 0.47 |
| Activity tracking frequencya | ||||
| Mean days | 17.08 ± 20.51 | 18.18 ± 19.94b | 16.19 + 21.41 | 0.77 |
n = 38 (n = 2 no login information).
n = 17.
Weight
Weight data were obtained for 100% (40 of 40) of male participants at 12 weeks (Table 4). Both groups did not experience a significant reduction in weight over time (standard group: −3.4 kg [8.04] (t = 0.50, p = 0.62) vs. enhanced: −4.7 kg (5.9) (t = 0.61, p = 0.55). The difference in weight between groups was −1.3 kg (t = −0.58, p = 0.57). The effect size was small (d = 0.18). Findings for percent weight loss were significant; standard group = 3.0% (t = −2.11, p < 0.05) and enhanced group = 4.0% (t = −3.86, p = 0.001). However, no difference between the groups (t = −0.76, p = 0.45). In the standard group, 42% (8 of 19) lost at least 5% of initial weight, compared with 38% (8 of 21) in the enhanced. Among standard participants, 11% (2 of 19) lost 10% of initial weight compared with 14% (3 of 21) of enhanced participants (Table 5).
Table 4.
Outcomes across groups at baseline and 12 weeks
| Change from baseline to 12 weeks | |||||||
|---|---|---|---|---|---|---|---|
| Outcome variable and group | Baseline mean (SD) | 12 weeks mean (SD) | p‐value within group | p‐value for standard vs. enhanced | Mean (SD) | p‐value for standard vs. enhanced | Effect size Cohen's d |
| Weight (kg) | |||||||
| Standard | 114.2 (20.8) | 110.8 (21.7) | 0.62 | 0.58 | −3.4 (8.04) | 0.57 | 0.18 |
| Enhanced | 111.3 (24.9) | 106.6 (25.4) | 0.55 | −4.7 (5.9) | |||
| % Weight change | |||||||
| Standard | 3.0 (6.0) | 0.05 | 0.45 | 0.18 | |||
| Enhanced | 4.0 (5.0) | 0.001 | |||||
| BMI | |||||||
| Standard | 35.2 (6.2) | 34.0 (5.7) | 0.56 | 0.73 | −1.2 (2.3) | 0.64 | 0.15 |
| Enhanced | 34.9 (6.2) | 33.3 (6.4) | 0.39 | −1.5 (1.8) | |||
| Waist circumference (cm) | |||||||
| Standard | 111.3 (12.8) | 107.7 (12.0)a | <.0001 | 0.89 | −2.9 (4.0)a | 0.27 | 0.39 |
| Enhanced | 113.2 (15.2) | 108.4 (16.7) | <.0001 | −4.7 (5.3) | |||
| Systolic blood pressure (mmHg) | |||||||
| Standard | 131.6 (39.3) | 134.0 (25.3) | 0.83 | 0.51 | N = 16 2.4 (38.3) | 0.52 | 0.23 |
| Enhanced | 136.1 (21.9) | 129.2 (19.4) | 0.29 | N = 20–4.4 (18.0) | |||
| Diastolic blood pressure (mmHg) | |||||||
| Standard | 83.3 (27.8) | 78.0 (12.6) | 0.46 | 0.64 | −4.3 (26.2)d | 0.46 | 0.26 |
| Enhanced | 86.7 (11.5) | 76.2 (10.4) | 0.004 | −9.35 (8.47)b | |||
| Energy intake (kcal/day) | |||||||
| Standard | 2344.8 (1171.3)c | 1952.8 (908.8)d | 0.29 | 0.18 | −366.046 (1103)d | 0.55 | 0.21 |
| Enhanced | 2099.8 (908.3)e | 1572.0 (692.7)c | 0.06 | −593.843 (1101)c | |||
| Energy expenditure (kcal/week) | |||||||
| Standard | 1423.4 (1822.0) | 1412.2 (1076.6)d | 0.98 | 0.88 | 308.4 (845.3)d | 0.07 | 0.63 |
| Enhanced | 500.0 (582.7) | 1363.8 (866.8)e | 0.001 | 826.1 (806.4)e | |||
| Partner's weight | |||||||
| Standard | 86.5 (16.4) | 86.5 (17.3)c | 0.99 | 0.44 | −0.23 (4.46) | 0.09 | 0.55 |
| Enhanced | 94.0 (23.7) | 91.5 (22.1) | 0.73 | −2.47 (3.62) | |||
| Partner's % weight change | |||||||
| Standard | −0.15 (6.21) | 0.22 | 0.42 | ||||
| Enhanced | −2.24 (3.43) | ||||||
n = 15.
n = 20.
n = 18.
n = 16.
n = 19.
Table 5.
Distribution of percent weight loss for male participants (n = 40)
| n (%) | −10% | −5–9% | −1–4% | +1 > n < −1 | +1–4% | +5–9% | +10% |
|---|---|---|---|---|---|---|---|
| Standard | 2 (10.5) | 6 (31.6) | 7 (36.8) | 2 (10.5) | 0 | 1 (5.3) | 1 (5.3) |
| Enhanced | 3 (14.2) | 5 (23.8) | 7 (33.3) | 4 (19.0) | 2 (9.5) | 0 | 0 |
Anthropometric outcomes
There was no significant change in BMI over 12 weeks standard: −1.2 kg/m2 (t = 0.59, p = 0.56) and enhanced: −1.5 kg/m2 (t = 0.86, p = 0.39), and no between group difference (effect size d = 0.14, t = −0.47, p = 0.64). Mean waist circumference in both decreased significantly over 12 weeks (standard: −2.9 cm [4.0], t = −13.16, p = 0.001 and enhanced: −4.7 cm [5.3] , t = −11.61, p = 0.006), but no difference between groups (effect size d = 0.38, t = −1.11, p = 0.27). There was no significant difference between groups in systolic blood pressure (effect size d = 0.22, t = −0.65, p = 0.52,). In the enhanced group, there was a significant decrease in diastolic blood pressure, over time (t = 3.04, p = 0.004); however, no significant difference between groups was observed (d = 0.26, t = −0.75, p = 0.46).
Behavioural outcomes
There were no differences between groups in caloric intake (d = 0.21, t = −0.60, p = 0.55) and energy expenditure (d = 0.63, t = −1.85, p = 0.07). From baseline to 12 weeks, there was no change in caloric intake per day in the standard group (−366 ± 1103 kcal, t = 1.08, p = 0.29) nor the enhanced group (−594 ± 1101 kcal, t = 1.98, p = 0.06), although the change over time showed a trend. Change in caloric intake had a significant positive correlation with change in weight from baseline to 12 weeks (r = 0.40, p = 0.02). At 12 weeks, there was a significant increase in energy expenditure in the enhanced group (t = −3.73, p = 0.001). Energy expenditure was not significantly correlated with weight change (r = 0.09, p = 0.59).
Partner outcomes
Among female partners in the standard group, there was a 0.2 kg (0.2%) decrease in weight from baseline to 12 weeks. In the enhanced group, there was a 2.5 kg (2.2%) decrease in weight. No significant between group differences were observed (p = 0.21); effect size weight change, d = 0.55. Female participants' weight loss was marginally associated with men's weight loss (r = −0.29, p = 0.07).
Discussion
This study demonstrated the feasibility of recruiting 40 Black couples and retaining almost 100% of the sample (100% of the male participants and 98% of the female participants). Attendance at group sessions was acceptable but not high, 63–73% of sessions were attended by men or men and their partners. Men in the enhanced group, who attended weight loss groups with their partner, lost 1% more weight than those men in the standard group who attended weight loss groups without their partners. As there was no statistical difference between groups and the effect size was small, there is no support of our hypothesis that a weight loss programme enhanced by partner involvement would be superior to weight loss achieved with a programme that did not involve the partner during initial weight loss. These results suggest Black men provided the option to participate with romantic partners, will enroll in weight loss programmes and lose clinically significant weight. The effects of partner involvement during weight maintenance, a time period where participants would be more dependent on partners due to receiving less engagement or support from study staff, were not assessed due to the duration of the study. Therefore, a longer study duration including a weight maintenance phase would more accurately assess the benefit of partner involvement during initial weight loss.
The study was powered to detect a fairly large between group difference (2.5 kg) with a small standard deviation (2.75 kg). The difference observed here was smaller than initially projected (1.3 kg difference, d = .18) and with greater variability (3.2 kg). This partly explains the lack of statistical significance of mean weight change over time, where significance is determined by the probability of replication. However, changes were clinically significant highlighting the practical importance of the change in real life and practice. Percent weight change, representing the magnitude of change, was both statistically and clinically significant; mean weight change measured absolute change. The magnitude or relative change observed in this study in both groups is likely to be replicated in future investigations and represents practical significance. As this was a pilot study, effect sizes were also examined. 26 Small to medium effects were observed between groups on most outcomes and provide some preliminary evidence for future investigations or larger randomized trials.
Importantly, our study results add to the limited research on weight management among Black men. These results are consistent with research involving active treatment comparison groups among Blacks. In a randomized controlled trial of older Black male adults, at 3 months, a −2.0‐kg difference was observed between groups (intervention: −2.2 kg, usual care: 0.3 kg)24 compared with −1.3 kg difference in this study. Previous studies reporting weight outcomes during similar time points reported weight reduction up to −2.2 kg.24, 27 In our study, weight reductions in both groups compare favorably to these interventions at similar time points; our enhanced group lost double the amount at the same time point compared with previous interventions (−4.7 kg vs. −2.2. kg, respectively). Other interventions had greater contact time; 8–12 group sessions lasting at least 90 min each compared with seven 60‐min group sessions used in this study. A longer intervention and follow‐up would be needed to compare with most other weight loss trials enrolling and reporting the weight losses of Black men specifically. Furthermore, in trials that enrolled Black adults, index participants experienced greater weight reduction when a family member was an active participant.12, 13 Similar associations between male weight loss and partner weight change were observed (r = −0.33, p = 0.04). Future studies should investigate dose of partner participation to maximize health benefits.
Interestingly, in our study, female partners were not required to be overweight at enrolment or to lose weight; however, in the enhanced group, partners experienced weight loss. Female partners in the enhanced group experienced clinically significant weight loss (2.24%). The weight losses observed in the enhanced treatment is in accordance with the results of Look AHEAD, where a Ripple effect on spouses whose partners were enrolled in the intensive lifestyle intervention was found. 28 The impact on both the index participant and partner can provide a synergic effect for the household and reduce family‐level obesity risk.
On other outcomes, compared with the standard group, small to medium effects in the expected direction among male participants in the enhanced group were observed. For example, enhanced group participants showed positive changes in BMI, waist circumference, blood pressure (systolic and diastolic), energy intake and energy expenditure that were in the expected direction when compared with the standard group. Male participants in the enhanced group attended more group sessions and completed more days of self‐monitoring of weight and caloric intake compared with the standard group, although overall rates of self‐monitoring in this population were low. Thus, our study demonstrates a slight advantage in participating with a partner that might be investigated in a longer and larger study. Men in the standard group experienced significant percent weight loss and blood pressure changes. These findings suggest the effectiveness of the standard treatment and provide evidence Black men can make clinically significant improvements without partner involvement. Furthermore, these findings can inform decision making for the most efficient and effective approaches to engage and impact Black men. Recruiting men alone is easier and requires less time of others. Future investigation should focus on improving adherence to behavioural techniques to possibly produce better outcomes. In particular, in both our study groups, self‐monitoring was low. A potential explanation for the weight losses observed in both groups is participants used other methods to monitor behaviour. In this study, participants were not formally asked about other forms of monitoring or the degree of behaviour change from baseline to post‐intervention. One weight loss study in men reported adherence for other forms of self‐monitoring including a checklist form (23.4%) and self‐monitoring their diet using a mobile application or website (44.7%). Daily self‐weighing had greater adherence in that study compared with this one.29 Interventions focusing on daily self‐weighing can produce clinically significant weight loss.30 Unfortunately, suitable studies to compare approaches to self‐monitoring among Black men were not found. Future research is needed to evaluate approaches to improve adherence to self‐monitoring among this population.
To our knowledge, our study is the first to use a couples‐based approach to weight loss among Black men. Previous couples‐based weight loss interventions were primarily designed to treat women as the index subject and enrolled mostly White participants. These studies have yielded mixed results. When compared with usual care, interventions using a couples' approach were more effective.18 More interestingly, of the randomized controlled trials comparing partner involvement vs. no involvement, 50% of the couple‐focused interventions were more effective.31 Our approach to use wives/co‐habitating girlfriends capitalized on previous strategies and expanded them to include a theoretically dyadic approach compared with the typical intrapersonal approaches used in weight loss research. Through the use of the Couples Skills Training, joint group session attendance and weekly couples' activities, this intervention sought to improve the functioning of the couple as a means to facilitate weight loss. Fifteen percent of couples did not attend the Couples Skills Training session and the extent to which couples completed the at‐home activities was not assessed. One possibility is that the dose of Couples Skills Training was not sufficient to see a meaningful effect of spousal support on weight loss. Further research should measure the dose received of the intervention delivered to fairly assess improvements in aspects of couple functioning like communication.
There are several other possible reasons a larger weight loss difference was not observed between groups. Due to the pilot nature of the study, TEAM had a shorter active treatment phase compared with other weight loss interventions; more contact would provide more time to build and hone skills required to maintain weight loss. Future studies should investigate the appropriate balance of dose and length of intervention. Lastly, one eligibility criterion was commitment from a partner. From enrollment, partners agreed to support their partners, therefore partners randomized to the standard group (not participating with their male partner), may have provided support outside the programme in efforts to help men achieve their goals. In such a case, this would lessen the differential effects of the couple's component.
This study was also able to recruit and retain Black men for a weight loss intervention. Of the 73 participants screened, 33% were ineligible, only 2% of men invited to an orientation passively declined participation through non‐response. Sixteen percent of eligible participants declined participation due to work schedules, emerging medical issues and distance to travel. This is promising for scalable interventions seeking to recruit Black men, a group traditionally labelled ‘hard to reach’. Most randomized participants (65%) reported face‐to‐face interaction with a study representative or a recommendation from a current participant as the source of learning about the study. In‐person communication is reported as one of the most effect methods to engage Black men32, 33 and was the most influential method in this study as well (data not shown). The study reported excellent retention rates in both groups also shedding light on the ability to engage and retain Black men in weight management research over a short duration study (12 weeks).
Although weight losses were observed in both groups, significant changes to diet and activity were not seen. The Automated Self‐Administered 24‐h dietary assessment tool was used to measure typical dietary intake. Participants in both groups experienced difficulty using the tool. As a result, some participants completed only one dietary recall of the requested two. The issue most often reported as accounting for failure or delay to complete recalls was installation of software required to run the ASA‐24 recall. This required use of clinic computers to complete the recall, which changed the intended random nature of the assessment. In future studies, interviewer administered 24‐h recalls may result in higher completion rates. Moreover, the Paffenberger is a self‐report measure for physical activity. Reporting of physical activity may have been influenced by social desirability. Future studies should use accelerometer for objective data collection to reduce the risk of bias in reporting.
There are several additional limitations to this study. Generalizability is limited by the small sample size, which is highly educated and fairly healthy. The lack of a no treatment control group does not permit assessment of the effectiveness of the intervention compared with no treatment. Other limitations are the use of self‐report measures of eating and activity and limited study duration.
Our study also had several strengths. First, all 40 Black men and their partners for 12 weeks were retained. The success of the programme to recruit, retain and produce clinically significant weight loss in both Black men and women is promising for a population experiencing health disparities in weight‐related comorbidities. Secondly, this feasibility study was randomized and included an active comparison group to control for attention and contact, as well as general behavioural weight loss skills training, to permit examination of the additional benefit of spousal social support on weight loss. Remarkably, the inclusion of an active treatment comparison group with partner involvement provided additional weight loss benefit to partners without the additional financial cost of implementation. Thirdly, our source of social support was innovative in that it was both culturally appropriate for Blacks and self‐sustaining through the use of an existing relationship for social support. The importance of family is a strong cultural value among Blacks. More importantly, this study adds to the limited research conducted on weight loss among Black men and using a couples‐based approach to weight loss among heterosexual couples.
Future research could increase intensity of couples' component or increase intensity of the standard programme and intervene for a longer period. Additionally, incorporating follow‐up assessment post‐intervention would provide information on weight maintenance. Lastly, an assessment of environmental changes within the home and measures on behaviours of children present in the home would provide preliminary data on other potential effects of a family‐based intervention.
Conflicts of interest statement
No potential conflict of interest relevant to this article was reported.
Author contributions
Alick, Samuel‐Hodge, Ward, Rini and Tate conceived the study concept and design; Alick and Tate collected, analyzed and interpreted data; Alick drafted the manuscript; Alick, Samuel‐Hodge, Ward, Rini, Ammerman and Tate provided critical revision of the manuscript for important intellectual content; and Tate obtained funding. All authors were involved in writing the paper and had final approval of the submitted and published versions.
Acknowledgements
We are indebted to the Together Eating & Activity Matters (TEAM) group members (listed alphabetically) Brandon Bishop; Molly Diamond, MPH; Christian Eller; Karen Hatley, MPH; Laurie Hursting; Jovia Ochieng; Elissa Scherer. We thank our community organizations who provided digital weight scales and fitness passes and the participants who made this study possible.
Alick, C. L. , Samuel‐Hodge, C. , Ward, D. , Ammerman, A. , Rini, C. , and Tate, D. F. (2018) Together Eating & Activity Matters (TEAM): results of a pilot randomized‐clinical trial of a spousal support weight loss intervention for Black men. Obesity Science & Practice, 4: 62–75. doi: 10.1002/osp4.142.
References
- 1. National Center for Health Statistics . Health, United States, 2015: With special feature on racial and ethnic health disparities. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics: Hyattsville, MD, 2016. [PubMed] [Google Scholar]
- 2. Griffith DM, Ober Allen J, Gunter K. Social and cultural factors influence african american men's medical help seeking. Research on Social Work Practice 2011; 21: 337–347. http://journals.sagepub.com/doi/abs/10.1177/1049731510388669. https://doi.org/10.1177/1049731510388669. [Google Scholar]
- 3. Barnett E, Halverson J. Local increases in coronary heart disease mortality among blacks and whites in the united states, 1985–1995. American Journal of Public Health 2001; 91: 1499–1506. https://doi.org/10.2105/AJPH.91.9.1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Harris MI, Eastman RC, Cowie CC, Flegal KM, Eberhardt MS. Racial and ethnic differences in glycemic control of adults with type 2 diabetes. Diabetes Care 1999; 22: 403–408. [DOI] [PubMed] [Google Scholar]
- 5. Warner DF, Hayward MD. Early‐life origins of the race gap in men's mortality. Journal of Health and Social Behavior 2006; 47: 209–226. https://doi.org/10.1177/002214650604700302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. West DS, Elaine Prewitt T, Bursac Z, Felix HC. Weight loss of black, white, and hispanic men and women in the diabetes prevention program. Obesity (Silver Spring) 2008; 16: 1413–1420. https://doi.org/10.1038/oby.2008.224. [DOI] [PubMed] [Google Scholar]
- 7. Svetkey LP, Ard JD, Stevens VJ, et al. Predictors of long‐term weight loss in adults with modest initial weight loss, by sex and race. Obesity (Silver Spring) 2012; 20: 1820–1828. https://doi.org/10.1038/oby.2011.88;%2010.1038/oby.2011.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wadden TA, Neiberg RH, Wing RR, et al. Four‐year weight losses in the look AHEAD study: Factors associated with long‐term success. Obesity (Silver Spring) 2011; 19: 1987–1998. https://doi.org/10.1038/oby.2011.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Newton RL Jr, Griffith DM, Kearney WB, Bennett GG. A systematic review of weight loss, physical activity and dietary interventions involving african american men. Obesity Reviews 2014; 15 Suppl 4: 93–106. https://doi.org/10.1111/obr.12209. [DOI] [PubMed] [Google Scholar]
- 10. Castro FG, Barrera M Jr, Holleran Steiker LK. Issues and challenges in the design of culturally adapted evidence‐based interventions. Annual Review of Clinical Psychology 2010; 6: 213–239. https://doi.org/10.1146/annurev‐clinpsy‐033109‐132032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Centers for Disease Control and Prevention . A closer look at african american men and high blood pressure control: A review of psychosocial factors and systems‐level interventions. U.S. Department of Health and Human Services: Atlanta, 2010. [Google Scholar]
- 12. Samuel‐Hodge CD, Holder‐Cooper JC, Gizlice Z, et al. Family PArtners in lifestyle support (PALS): Family‐based weight loss for african american adults with type 2 diabetes. Obesity 2017; 25: 45–55. https://doi.org/10.1002/oby.21700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kumanyika SK, Wadden TA, Shults J, et al. Trial of family and friend support for weight loss in african american adults. Archives of Internal Medicine 2009; 169: 1795–1804. https://doi.org/10.1001/archinternmed.2009.337. [DOI] [PubMed] [Google Scholar]
- 14. Hooker SP, Harmon B, Burroughs EL, Rheaume CE, Wilcox S. Exploring the feasibility of a physical activity intervention for midlife african american men. Health Education Research 2011; 26: 732–738. https://doi.org/10.1093/her/cyr034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dilworth‐Anderson P. Marshall S. Social support in its cultural context In: Pierce GR, Sarason BR, Sarason IG. (eds). Handbook of social support and the family. Springer Science & Business Medi: New York, 1996, p. 67. [Google Scholar]
- 16. Schierberl Scherr AE, McClure Brenchley KJ, Gorin AA. Examining a ripple effect: Do spouses' behavior changes predict each other's weight loss? Journal of Obesity 2013. 2013:297268. doi: https://doi.org/10.1155/2013/297268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Metzgar C, Preston A, Miller D, Nickols‐Richardson S. Facilitators and barriers to weight loss and weight loss maintenance: A qualitative exploration. Journal of Human Nutrition and Dietetics 2015; 28: 593–603. [DOI] [PubMed] [Google Scholar]
- 18. Black DR, Gleser LJ, Kooyers KJ. A meta‐analytic evaluation of couples weight‐loss programs. Health Psychology 1990; 9: 330–347. [DOI] [PubMed] [Google Scholar]
- 19. Jakicic JM, Tate DF, Lang W, et al. Effect of a stepped‐care intervention approach on weight loss in adults: A randomized clinical trial. JAMA 2012; 307: 2617–2626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wing RR, Tate D, Espeland M, et al. Weight gain prevention in young adults: Design of the study of novel approaches to weight gain prevention (SNAP) randomized controlled trial. BMC Public Health 2013; 13: 300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tate DF, Wing RR, Winett RA. Using internet technology to deliver a behavioral weight loss program. JAMA 2001; 285: 1172–1177. [DOI] [PubMed] [Google Scholar]
- 22. Tate DF, Jackvony EH, Wing RR. Effects of internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: A randomized trial. JAMA 2003; 289: 1833–1836. https://doi.org/10.1001/jama.289.14.1833. [DOI] [PubMed] [Google Scholar]
- 23. Tate DF, Jackvony EH, Wing RR. A randomized trial comparing human e‐mail counseling, computer‐automated tailored counseling, and no counseling in an internet weight loss program. Archives of Internal Medicine 2006; 166: 1620–1625. [DOI] [PubMed] [Google Scholar]
- 24. Agurs‐Collins TD, Kumanyika SK, Ten Have TR, Adams‐Campbell LL. A randomized controlled trial of weight reduction and exercise for diabetes management in older african‐american subjects. Diabetes Care 1997; 20: 1503–1511. [DOI] [PubMed] [Google Scholar]
- 25. Morgan PJ, Callister R, Collins CE, et al. The SHED‐IT community trial: A randomized controlled trial of internet‐ and paper‐based weight loss programs tailored for overweight and obese men. Annals of Behavioral Medicine 2013; 45: 139–152. https://doi.org/10.1007/s12160‐012‐9424‐z. [DOI] [PubMed] [Google Scholar]
- 26. Arain M, Campbell MJ, Cooper CL, Lancaster GA. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Medical Research Methodology 2010; 10: 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dean DA, Griffith DM, McKissic SA, Cornish EK, Johnson‐Lawrence V. Men on the move‐nashville: Feasibility and acceptability of a technology‐enhanced physical activity pilot intervention for overweight and obese middle and older age african american men. American Journal of Men's Health 2016. Accessed 6/7/2017 5:41:40 PM. doi: https://doi.org/10.1177/1557988316644174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gorin AA, Wing RR, Fava JL, et al. Weight loss treatment influences untreated spouses and the home environment: Evidence of a ripple effect. International Journal of Obesity 2008; 32: 1678–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Crane MM, Lutes LD, Ward DS, Bowling JM, Tate DF. A randomized trial testing the efficacy of a novel approach to weight loss among men with overweight and obesity. Obesity 2015; 23: 2398–2405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Steinberg DM, Tate DF, Bennett GG, Ennett S, Samuel‐Hodge C, Ward DS. The efficacy of a daily self‐weighing weight loss intervention using smart scales and e‐mail. Obesity 2013; 21: 1789–1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Arden‐Close E, McGrath N. Health behaviour change interventions for couples: A systematic review. British Journal of Health Psychology 2017; 22: 215–237. https://doi.org/10.1111/bjhp.12227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Friedman DB, Johnson KM, Owens OL, et al. Developing partnerships and recruiting dyads for a prostate cancer informed decision making program: Lessons learned from a community‐academic‐clinical team. Journal of Cancer Education 2012; 27: 243–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Woods VD, Montgomery SB, Herring RP. Recruiting black/african american men for research on prostate cancer prevention. Cancer 2004; 100: 1017–1025. https://doi.org/10.1002/cncr.20029. [DOI] [PubMed] [Google Scholar]


