Abstract
A 79-year-old obese man with obstructive sleep apnea, who ambulates with assistance comes to you to discuss post-polypectomy surveillance colonoscopy. His last colonoscopy was performed 5 years ago, during which two small adenomas were removed.
Post-polypectomy surveillance is an increasingly common indication for colonoscopy in the United States. As screening uptake increases and our population ages, we will see growing numbers of older adults who are due for surveillance. For many, the balance of benefits and harms will be uncertain. In addition, unlike for average-risk screening, where there are clear recommendations for when to stop, there is no specific guidance on when to stop surveillance (1,2). We therefore propose five “rules of thumb,” to guide gastroenterologists in making decisions about stopping surveillance in older adults (Table 1).
Table 1. Summary of the five rules of thumb for making surveillance colonoscopy decisions in older adults.
| Rules of thumb | Rationale | Example |
|---|---|---|
| 1. Know the data | Knowing the data on CRC* risk and colonoscopy-related harms is essential if we are to make sound recommendations and have meaningful discussions with our patients. | Know the lifetime risk of CRC in patients with LRAs versus HRAs. |
| 2. Get the full history | Incomplete information on prior colonoscopy quality and findings creates unnecessary ambiguity. | Obtain prior colonoscopy and pathology reports. |
| 3. Individualize benefits and harms | Benefits and harms vary widely between patients, especially as they get older. | Use decision support tools (e.g., www.screeningdecision.com) and validated life expectancy calculators (e.g., ePrognosis). |
| 4. Engage the patient | Understanding patients' perspectives can guide decision-making, especially in cases that are not clear cut. | Ask patients about their preferences and values, including worry about cancer and the burdens of colonoscopy. |
| 5. Work with your colleagues | PCPs* know their patients' current medical and functional status and often have greater insight into their values and preferences. | Act as a consultant, providing clear guidance with appropriate qualifications that provide the PCP with flexibility. |
CRC, colorectal cancer; HRA, high-risk adenoma; LRA, low-risk adenoma; PCP, primary care provider.
Know the Data
Patients and providers tend to over- or underestimate the risk of colorectal cancer (CRC) in individuals with adenomas. However, the data are very clear. Patients with prior high-risk adenomas (HRAs: adenoma ≥ 10 mm in size, presence of villous features or high-grade dysplasia, or three or more adenomas of any size) are nearly twice as likely to have metachronous advanced neoplasia as those with low-risk adenomas (LRAs: 1 or 2 adenomas <10 mm in size), and this risk increases with the number and size of prior adenomas (3). Furthermore, individuals with LRAs have a lifetime CRC risk that is at or below the average-risk population (4% lifetime risk), whereas those with HRAs have two- to fivefold higher risk (3–5). As a result, in the United Kingdom, surveillance colonoscopy is not recommended for those with LRAs after index polypectomy and those with HRAs are recommended for more intensive surveillance than in the United States (6).
In contrast, patients and providers tend to underestimate the risk of colonoscopy-related harms in older adults. For example, bowel preparation, including diet changes and ingestion of purgative, are more burdensome in older adults due to comorbid health conditions and limited mobility, leading to greater risk for electrolyte disturbances (e.g., hypokalemia), dehydration, and falls. Older adults are also more likely to suffer sedation-related cardiopulmonary complications, such as aspiration and cardiac arrhythmias. Furthermore, the likelihood of incomplete colonoscopy is higher in older adults due to greater likelihood of inadequate bowel preparation (7). Finally, older adults are at higher risk for bowel perforation and its morbid, and potentially mortal, sequelae. We recommend that gastroenterologists familiarize themselves with data on CRC risk and procedure-related harms, and how these harms vary by age, so they can better guide older adults in decision making.
Get the Full History
It is tough to make decisions if you do not know all the details. For example, was the prior colonoscopy complete with adequate bowel preparation? Does the patient have a prior history of HRAs? The majority of patients do not recall these details, which are necessary to estimate their risk of CRC. Therefore, we recommend that gastroenterologists be diligent about obtaining and reviewing prior endoscopy and pathology reports. When colonoscopy reports are unavailable, “erring on the side of caution” and performing colonoscopy may be unwise among older adults in whom the potential harms of colonoscopy may outweigh the benefits.
Estimate Benefits and Harms Individualized to your Patient
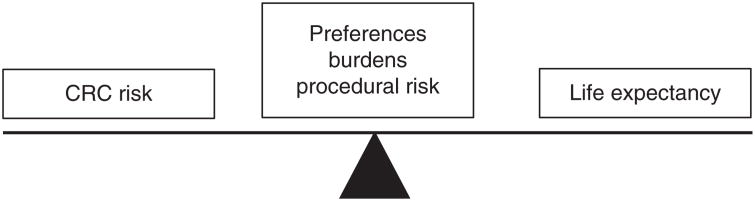
As gastroenterologists, we should inform older adults about the benefits and harms of surveillance colonoscopy (Figure 1). This includes the risks of the preparation (i.e., stopping anticoagulants, diet changes, and consuming the purgative), conscious or deep sedation, and the procedure itself. To determine whether benefits outweigh harms for a given patient, we need to consider both CRC risk and life expectancy, in lieu of age alone (8). However, physicians' “gestalt” estimates of life expectancy are often inaccurate. Fortunately, quantitative tools to estimate life expectancy (such as ePrognosis—http://eprognosis.ucsf.edu/ (9)) are readily available. Other tools, such as www.screeningdecision.com, weigh benefits and harms, simultaneously considering both CRC risk and life expectancy (10). We recommend that gastroenterologists become familiar with available tools and use them when decisions about surveillance are not clear cut.
Figure 1.
Key factors to consider when making surveillance colonoscopy decisions in older adults. *CRC, colorectal cancer; higher CRC risk is associated with higher benefit; lower life expectancy is associated with lower benefit.
As patients with LRAs have CRC risk similar to that of the screened population, it is not unreasonable to utilize an approach similar to that for average-risk screening. The American College of Physicians, e.g., recommends that average-risk CRC screening be discontinued in patients with a life expectancy of <10 years (the average life expectancy for a 75-year-old in the United States) (11). T us, we recommend discussion about stopping surveillance colonoscopy in older adults with LRAs when 10-year life expectancy using ePrognosis (or a similar, validated tool) is <50% or when comorbidity-adjusted life expectancy (12) is <10 years.
Engage the Patient
Guidelines often fail to present benefits and harms in a clinically meaningful way and patients may not understand the magnitude of risks of screening tests and of en overestimate benefits (13). Therefore, we must talk to our patients, eliciting their values and preferences. This is of utmost importance among older adults who may have competing comorbidities or limited life expectancy. If you have a strong recommendation, be clear; otherwise shared decision-making is one approach for incorporating preferences in the face of uncertainty. Data show that trust in physicians is associated with patients having greater comfort stopping surveillance if they are in poor health (14). We recommend selective use of shared decision-making in older adults for whom the benefits and harms of surveillance are particularly uncertain.
Work with your Colleagues
Communicate clearly and thoughtfully with referring primary-care physicians (PCPs) (15). During the interval between index and surveillance colonoscopy, there may be substantial changes in the overall health status of an older adult. As a result, recommendations that were made in the past may no longer be appropriate, but these recommendations may still carry considerable weight and potentially encourage inappropriate care. Indeed, data show that PCPs are likely to follow the surveillance interval recommended by the endoscopist (16).
In addition, pathology follow-up letters may contain non-neutral language to describe findings, which may heighten perceived risk of CRC among both patients and providers. For example, using the term ‘pre-cancerous’ to describe an isolated diminutive adenoma may lead patients and providers alike to believe that there is a falsely high risk of CRC, despite data showing the contrary. Therefore, we recommend careful phrasing when communicating pathology results. Specifically, we should avoid using ambiguous or alarming language (e.g., “precancerous polyp”) and avoid strict recommendations without qualification when health status may change.
Conclusion
In summary, the decision to pursue surveillance colonoscopy in older adults should carefully weigh both potential benefits and potential harms. For the patient in our scenario, we know that he is at low risk for CRC due to his personal history of LRAs (Rule 1) and absence of HRAs on prior colonoscopy reports (Rule 2). Using ePrognosis, we estimate that his 10-year life expectancy is <40% (Rule 3). Further discussion reveals that bowel preparation is very challenging for him due to his limited mobility (Rule 4). In the end, you decide together that surveillance colonoscopy is unlikely to be of substantial benefit and may be burdensome or harmful. You send a letter to his PCP explaining this decision and its rationale (Rule 5).
Acknowledgments
Guarantor of the article: Sameer D. Saini, MD, MS.
Financial support: No funding sources were used for this publication.
Footnotes
Specific author contributions: Jennifer K. Maratt, Audrey H. Calderwood, and Sameer D. Saini contributed to writing and revision of this manuscript. Audrey H. Calderwood and Sameer D. Saini contributed to conception and supervision of this manuscript. All authors approved the final draft that is submitted.
Conflict of Interest: Potential competing interests: None.
References
- 1.Lieberman DA, Rex DK, Winawer SJ, et al. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2012;143:844–57. doi: 10.1053/j.gastro.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 2.US Preventive Services Task Force. Bibbins-Domingo K, Grossman DC, et al. Screening for colorectal cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2016;315:2564–75. doi: 10.1001/jama.2016.5989. [DOI] [PubMed] [Google Scholar]
- 3.Martínez ME, Baron JA, Lieberman DA, et al. A pooled analysis of advanced colorectal neoplasia diagnoses after colonoscopic polypectomy. Gastroenterology. 2009;136:832–41. doi: 10.1053/j.gastro.2008.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Atkin WS, Morson BC, Cuzick J. Long-term risk of colorectal cancer after excision of rectosigmoid adenomas. N Engl J Med. 1992;326:658–62. doi: 10.1056/NEJM199203053261002. [DOI] [PubMed] [Google Scholar]
- 5.Calderwood AH, Lasser KE, Roy HK. Colon adenoma features and their impact on risk of future advanced adenomas and colorectal cancer. World J Gastrointest Oncol. 2016;8:826–34. doi: 10.4251/wjgo.v8.i12.826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martínez ME, Tompson P, Messer K, et al. One-year risk for advanced colorectal neoplasia: U.S. versus U.K. risk-stratifcation guidelines. Ann Intern Med. 2012;157:856–64. doi: 10.7326/0003-4819-157-12-201212180-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Calderwood AH, Anderson JC, Robinson CR, et al. Incomplete colonoscopies in older adults: an analysis of the New Hampshire Colonoscopy Registry. American College of Gastroenterology Annual Scientific Meeting; Orlando, FL. October 2017. [Google Scholar]
- 8.Saini SD, van Hees F, Vijan S. Smarter screening for cancer: the possibilities and challenges of personalization. JAMA. 2014;312:2211–5. doi: 10.1001/jama.2014.13933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee SJ, Lindquist K, Segal MR, et al. Development and validation of a prognostic index for 4-year mortality in older adults. JAMA. 2006;295:801–8. doi: 10.1001/jama.295.7.801. [DOI] [PubMed] [Google Scholar]
- 10.Saini SD, Solomon J. Should my patient get a screening colonoscopy? [Accessed: 20 July 2017]; Available at www.screeningdecision.com.
- 11.Wilt TJ, Harris RP, Qaseem A. Screening for cancer: advice for high-value care from the American College of Physicians. Ann Intern Med. 2015;162:718–25. doi: 10.7326/M14-2326. [DOI] [PubMed] [Google Scholar]
- 12.Cho H, Klabunde CN, Yabroff R, et al. Comorbidity-adjusted life expectancy: a new tool to inform recommendations for optimal screening strategies. Ann Intern Med. 2013;159:667–77. doi: 10.7326/0003-4819-159-10-201311190-00005. [DOI] [PubMed] [Google Scholar]
- 13.Sutkowi-Hemstreet A, Vu M, Harris R, et al. Adult patients' perspectives on the benefits and harms of overused screening tests: a qualitative study. J Gen Intern Med. 2015;30:1618–26. doi: 10.1007/s11606-015-3283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maratt JK, Lewis C, Safar D, et al. Veterans' attitudes towards de-intensification of surveillance colonoscopy for low-risk adenomas. Am J Gastro-enterol. 2016;111:S119–S120. doi: 10.1016/j.cgh.2018.03.029. [DOI] [PubMed] [Google Scholar]
- 15.Le ST, Lash BR, Schroy PC, III, et al. Physician perceptions of surveillance follow-up colonoscopy in older adults. J Am Board Family Med. 2017;30:371–3. doi: 10.3122/jabfm.2017.03.160386. [DOI] [PubMed] [Google Scholar]
- 16.Read AJ, Weissman A, Schoenfeld PS, et al. Are endoscopists preventing primary care providers from choosing wisely? Results of a national survey of when to repeat screening and surveillance colonoscopy. Gastroenterology. 2015;148:S208–S209. [Google Scholar]