Abstract
Importance
Chronic nasal congestion often persists in children despite empirical treatment using intranasal corticosteroids, systemic antihistamines, and/or leukotriene receptor antagonists. Symptoms are often reported even with negative results of skin or blood allergy testing. Inferior turbinoplasty has been effective in adults and children, but outfracture of inferior turbinates in children is rarely reported, as is use of validated quality-of-life measures to quantify improvements after intervention. Effective use of these 2 procedures for treating chronic nasal congestion may reduce the need for medication and improve sinonasal quality of life.
Objective
To quantify changes in sinonasal quality of life for children after outfracture of inferior turbinates and concomitant submucous microdebrider inferior turbinoplasty for chronic nasal congestion.
Design, Setting, and Participants
A case series with planned data collection was conducted in an ambulatory pediatric otolaryngology clinic among 43 patients with chronic nasal congestion who underwent surgical intervention between January 1, 2014, and May 31, 2015.
Exposures
Microdebrider submucous inferior turbinoplasty (without bony resection) and outfracture of inferior turbinates.
Main Outcomes and Measures
Demographics and medication use before and after the procedure were reviewed. Scores on the Sinus and Nasal Quality of Life Survey (SN-5) and quality-of-life scores were collected at baseline, 4 to 6 weeks after the procedure, and more than 6 months after the procedure.
Results
Among the 43 patients (14 girls and 29 boys; mean age, 11.2 years [range, 4.8-17.6 years]), every domain showed significant improvements in scores on the Sinus and Nasal Quality of Life Survey and quality-of-life scores 1 to 2 months after the proecdure: sinus infection (–2.55; 95% CI, 1.85-3.26), nasal obstruction (–3.51; 95% CI, 2.88-4.14), allergy symptoms (–2.14; 95% CI, 1.43-2.86), emotional distress (–2.37; 95% CI, 1.68-3.06), activity limitation (–1.70; 95% CI, 1.14-2.25), and overall quality of life (3.72; 95% CI, 2.95-4.48). At long-term follow-up, improvement was maintained in all categories. Significant improvements in SN-5 and quality-of-life scores correlated with proportional decreased reporting of snoring after the procedure (33 [77%] vs 1 [2%]; absolute reduction, 75%; 95% CI, 62%-88%), as well as nasal congestion (41 [95%] vs 1 [2%]; absolute reduction, 93% ; 95% CI, 85%-100%), and rhinorrhea (44 [41%] vs 1 [2%]; absolute reduction, 42%; 95% CI, 27%-57%). The proportion reporting use of intranasal corticosteroids (25 [58%] vs 2 [5%]; absolute reduction, 50%; 95% CI, 39%-71%), antihistamines (27 [63%] vs 1 [2%]; absolute reduction, 61%; 95% CI, 46%-75%), and leukotriene receptor antagonists (13 [30%] vs 0; absolute reduction, 30%; 95% CI, 16%-44%) also decreased.
Conclusions and Relevance
Concomitant outfracture and submucous microdebrider inferior turbinoplasty improves quality of life in children with chronic nasal congestion and can reduce use of daily medication.
This case series examines changes in sinonasal quality of life for children after outfracture of inferior turbinates and concomitant submucous microdebrider inferior turbinoplasty for chronic nasal congestion.
Key Points
Question
What is the effect on quality of life in children with chronic nasal congestion who undergo outfracture and submucous microdebrider inferior turbinectomy?
Findings
This case series of 43 children with chronic nasal congestion found that, at long-term and short-term follow-up, patients who underwent outfracture and submucous microdebrider inferior turbinectomy reported a decrease in symptoms, demonstrated by scores on the Sinus and Nasal Quality of Life Survey, decreased use of medication, and improvement in quality of life.
Meaning
Concomitant outfracture and submucous microdebrider inferior turbinectomy improves quality of life in children with chronic nasal congestion and can reduce use of daily medication.
Introduction
Chronic nasal congestion is a common pediatric symptom that prompts visits to otolaryngologists. Most primary care physicians empirically prescribe medication typically used to treat allergic rhinitis for children with nasal congestion. Daily medications generally include intranasal corticosteroids (INS), 1 or more systemic antihistamines, and leukotriene receptor antagonists. Patients may or may not have been evaluated by allergy or pulmonology subspecialists for atopy or asthma, and they report persistent symptoms and dissatisfactory nasal airway condition despite months and even years of use of daily medications. Approximately 10% to 20% of the US pediatric population is affected by allergic rhinitis, and 17% of the population reports symptoms lasting more than 31 days. Initial treatment consists of lifestyle modifications, including avoidance of identifiable triggers, such as exposure to nicotine and smoke and dust mites from carpeting, stuffed animals, and bedding. Symptoms of chronic nasal congestion persist despite negative results on the appropriate allergy workup for allergic rhinitis, including IgE blood testing and skin testing for allergies to common aeroallergens. Nasal obstruction and congestion decrease quality of life, can reduce concentration or attention span, affect quality of sleep, and cause obstructive sleep apnea or sleep-disordered breathing. Sleep disturbance and sleep-disordered breathing can contribute to behavioral challenges and decreased school performance for school-aged children.
Inferior turbinates are the largest of the 3 pairs of turbinates; the head of the inferior turbinate takes up the greatest cross-sectional area, which determines nasal resistance during inspiration. Excessive and persistent inferior turbinate hypertrophy may represent a pathologic condition not caused by atopy in the normal nasal cycle. During the normal nasal cycle, each turbinate alternates being engorged in its mucosa such that total resistance of the nasal airway may be higher than normal, resulting in airflow through only 1 naris. Inferior turbinates consist of bone, capacitance tissue, submucosal glandular lamina propria, and respiratory epithelium. Inferior turbinate mucosa may become engorged and hypertrophic owing to allergic rhinitis, vasomotor rhinitis, viral upper respiratory tract infections, hormonal influences, crying, and other causes. When the inferior turbinate mucosa is engorged bilaterally or unilaterally, decreased airflow results in subjective experience of nasal obstruction and a “stuffed” or “blocked” nose as reported by children and perceived by parents or caretakers. Inferior turbinoplasty (IT) can reduce the volume of the vascular stromal tissue of the inferior turbinate, which can increase the cross-sectional area of the anterior nasal passage for airflow, leading to increased nasal patency. The outfracture of inferior turbinates involves fracturing the laterally based bony attachment such that the body of the inferior turbinate is positioned more laterally, creating greater space for laminar airflow between the medial aspect of the inferior turbinate to the septum. There are studies reporting the effectiveness of IT procedures in children, but, to our knowledge, there are no published outcomes for outfracture of inferior turbinates in children for chronic nasal congestion. Arganbright et al reported their 10-year review on the safety and efficacy of IT in 1770 children regardless of techniques, with 63 parents completing follow-up telephone surveys. Langille and El-Hakim reported in 2011 that IT in children was safe and improved quality of life when performed with or without adenoidectomy. To demonstrate the applicability of a proven safe procedure to a similar but separate disease process, this study aimed to quantify the changes in sinonasal quality of life for children with chronic nasal congestion after outfracture of inferior turbinates and concomitant submucous microdebrider IT.
Methods
We performed a review of medical records for data acquisition on a case series with planned data collection on 43 consecutive children who underwent both IT and outfracture IT between January 1, 2014, and May 31, 2015, for chronic and persistent nasal congestion despite maximal medical therapy. Patients presented to an ambulatory pediatric otolaryngology clinic of a single surgeon (J.L.W.); all patients had persistent symptoms despite daily use of INS, antihistamines, or leukotriene receptor antagonists. For children 4 years or older, a trial of daily saline irrigation is routinely recommended before any surgical intervention. To qualify for maximal medical therapy, all patients were using INS, antihistamines, and leukotriene receptor antagonists at one time, in addition to a trial of daily saline irrigation. In addition, one of us (J.L.W.) routinely obtains the patient’s diet and dietary habit history to determine if nocturnal reflux may be a contributing factor to the nasal congestion. This information consists of dinner time, bed time, amount of dairy in the child’s diet, and snacking until bedtime. Patients who were at risk for reflux underwent treatment through habit adaptation. If their symptoms persisted, those patients were included in the study. This study was approved by the Nemours Children’s Hospital Institutional Review Board, Orlando, Florida, which waived requirement for parental consent as this was a retrospective case summary.
All patients with more than a 3-month history of reported daily nasal congestion with or without rhinorrhea despite use of daily medications for allergic rhinitis were eligible for inclusion. Patients were excluded if they had a history of turbinate reduction procedures or if turbinate reduction procedures were planned in conjunction with other nasal procedures, including adenoidectomy and/or septoplasty. All patients underwent outpatient outfracture of inferior turbinates and IT by the same surgeon using the same technique.
Sinus and Nasal Quality of Life Survey and Quality-of-Life Survey
The Sinus and Nasal Quality of Life Survey (SN-5) is a validated and reliable assessment of quality of life for children with persistent sinonasal symptoms. When the survey is administered to the same patient over time, the score has been proven to correlate with direct estimates of clinical change.
All parents or primary caretakers were asked to complete the SN-5 and a separate quality-of-life survey, administered together, during the initial office visit (baseline) and again at the follow-up visit 4 to 6 weeks after the procedure (mean, 5.6 weeks; median, 4 weeks; range, 4-8 weeks). At the postoperative visit, caretakers were also asked about the presence and severity of symptoms of nasal congestion, “stuffiness,” rhinorrhea, and snoring, as well as about medication use. Long-term follow-up, including online SN-5 and quality-of-life assessments, was performed 1 to 2 years after the procedure (mean, 1.5 years; median, 1.6 years; range, 0.5-2.2 years).
For each domain of the SN-5, the question was, “How often has there been a problem for your child during the past 4 weeks for the specific symptom?” The scores range from 0 to 7, with 0 corresponding to the answer “none of the time” and 7 to the answer “all of the time” for each question. Higher numerical scores indicate worse problems. In the overall quality-of-life survey, quality of life is determined by the primary caretaker’s answer to the question: “How would you rate your child’s quality of life as a result of nose or sinus problem?” A face and numerical rating scale corresponds to various levels of quality of life as associated with the sinonasal symptoms. On the scale, 0 represents the worst possible quality of life and 10 represents the best possible quality of life.
Surgical Procedures
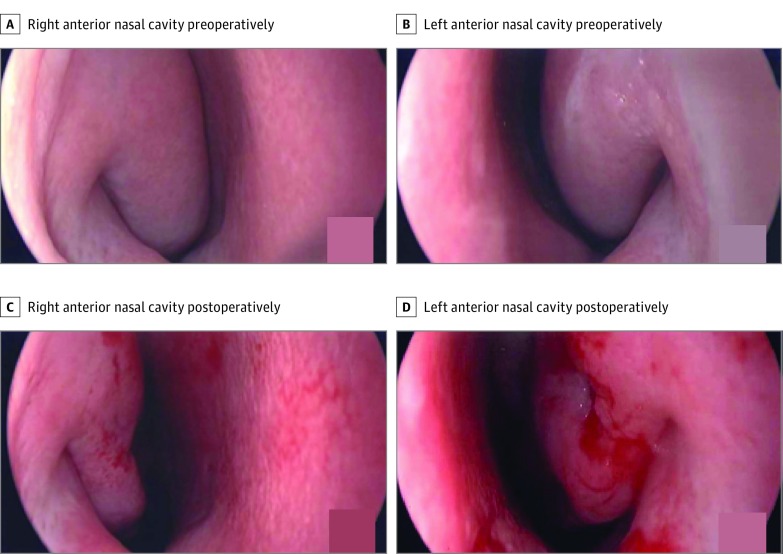
After patients were administered general anesthesia and underwent endotracheal intubation but before any intervention, photographic documentation was obtained of each side of the relationship between the head of the inferior turbinate and septum. Attention was directed to the right side first. Approximately 1 mL of bupivacaine, 0.25%, with epinephrine in a 1:200 000 ratio was injected in the head of the inferior turbinates. Then, a 2-mm pediatric microdebrider turbinoplasty blade (Medtronic) was used to make a single puncture into the submucosal space. Inferior turbinoplasty was performed with the blade gently removing vascular stromal tissue in the anterior half of the length of the inferior turbinate. Care was taken not to cause any perforations along the mucosal flap and to stay medial to the inferior turbinate bone. The turbinoplasty blade was then removed. Next, a long nasal speculum was introduced into the nasal passage, with blades parallel to the length of the inferior turbinate. Outfracture was performed by opening the speculum and gently and manually using the blade to lateralize each inferior turbinate, keeping the speculum in the open position. Once outfracture was completed, 2 long, cotton pledgets soaked with oxymetazoline were placed along the nasal passage between the septum and inferior turbinate and left in place for 1 to 2 minutes to achieve hemostasis. These steps were repeated for the left side. Photographs were taken to document the new relationship between the inferior turbinate head and septum (Figure). Rolled-up Telfa pad (Covidien) coated with bacitracin ointment was then placed between the inferior turbinate and septum to minimize bleeding and was removed just before the patient was extubated. After the procedure, patients were instructed to apply antibiotic ointment to the anterior nares 2 or 3 times daily for 3 to 5 days and were restricted to light activity on the day of surgery.
Figure. Nasal Airway Before and After the Procedure.
Endoscopic view of relationship between head of inferior turbinate to septum before and after outfracture of inferior turbinates and inferior turbinoplasty.
Statistical Analysis
Data were collected in Excel (Microsoft Corp). Statistical analysis was performed with SPSS, version 21 (SPSS Inc). Demographics and other categorical variables were summarized by frequencies and percentages. Quantitative variables were summarized by medians. Paired 2-sample t tests were performed to analyze the difference between SN-5 and quality-of-life scores before and after the procedure. Comparisons of 2 unpaired proportions were performed to explore changes in proportions of patients with subjective symptoms and use of medication before and after the procedure.
Results
Forty-three consecutive patients (14 girls and 29 boys; mean age, 11.2 years; median age, 10.7 years; range, 4.8-17.6 years) underwent the described procedures. The changes in proportions of subjectively reported symptoms and use of medication from before the procedure to 1 to 2 months after the procedure are shown in Table 1. At baseline and preoperatively, nasal congestion or obstruction was the chief symptom (41 [95%]), followed by snoring (33 [77%]) and rhinorrhea (19 [44%]). Most patients were taking multiple daily medications, including oral antihistamines (27 [63%]), INS (25 [58%]), and leukotriene receptor antagonists (13 [30%]). At the 1- to 2-month follow-up visit, 1 patient (2%) reported persistent nasal congestion, 1 patient (2%) reported persistent rhinorrhea, and 1 patient (2%) reported persistent snoring. Only 2 patients (5%) still used daily INS, and only 1 patient (2%) was taking an oral antihistamine. All patients stopped taking leukotriene receptor antagonists after the procedure. The decrease in proportions for subjectively reported symptoms between preoperative and postoperative visits was significant for nasal congestion (absolute reduction, 93%; 95% CI, 85%-100%), rhinorrhea (absolute reduction, 42%; 95% CI, 27%-57%), and snoring (absolute reduction, 75%; 95% CI, 62%-88%). The decrease in proportions for subjectively reported use of medication between the preoperative and postoperative visits was significant for INS (absolute reduction, 50%; 95% CI, 39%-71%), oral antihistamines (absolute reduction, 61%; 95% CI, 46%-75%), and leukotriene receptor antagonists (absolute reduction, 31%; 95% CI, 16%-44%).
Table 1. Proportions of Patients Subjectively Reporting Symptoms and Medication Use Before and After the Procedure.
| Characteristic | Patients Before the Procedure, No. (%) (N = 43) |
Patients 1-2 mo After the Procedure, No. (%) (N = 43) |
Absolute Reduction, % (95% CI) |
|---|---|---|---|
| Nasal congestion | 41 (95) | 1 (2) | 93 (85-100) |
| Snoring | 33 (77) | 1 (2) | 75 (62-88) |
| Antihistamines | 27 (63) | 1 (2) | 61 (46-75) |
| Use of INS | 25 (58) | 2 (5) | 50 (39-71) |
| Rhinorrhea | 19 (44) | 1 (2) | 42 (27-57) |
| LTRAs | 13 (30) | 0 | 30 (16-44) |
Abbreviations: INS, intranasal corticosteroids; LTRAs, leukotriene receptor antagonists.
History and reported results of prior allergy testing are shown in Table 2. Twenty patients (47%) had previously undergone formal allergy testing, with 12 of those tested (60%) reporting skin testing and 4 (20%) reporting IgE blood testing; 4 parents (20%) were unable to recall which specific form of testing their child underwent. Positive test results were reported in the categories of dust mites (4 [20%]), grass or pollen (10 [50%]), mold (2 [10%]), food (6 [30%]), and animals (6 [30%]). Six of the patients who underwent testing (30%) had uniformly negative results despite reported daily experience of persistent nasal congestion or obstruction.
Table 2. Type and Results of Formal Allergen Testing.
| Characteristic | Overall, No. | Skin Prick Allergen Test, No. | Allergen-Specific IgE Test, No. | Unknown Form of Allergen Testing, No. |
|---|---|---|---|---|
| Underwent testing | 20 | 12 | 4 | 4 |
| Positive resultsa | ||||
| Dust mites | 4 | 1 | 2 | 1 |
| Grass or pollen | 10 | 6 | 3 | 1 |
| Mold | 2 | 2 | 0 | 0 |
| Food | 6 | 3 | 1 | 2 |
| Animal | 6 | 4 | 1 | 1 |
| Negative to all allergens | 6 | 4 | 1 | 1 |
Some patients reacted to multiple allergens.
There were significant improvements (reduction in SN-5 domain scores) for all domains as well as an increase in the overall quality-of-life score at 1 to 2 months after the procedure compared with baseline (sinus infection, –2.55; 95% CI, 1.85-3.26; nasal obstruction, –3.51; 95% CI, 2.88-4.14; allergy symptoms, –2.14; 95% CI, 1.43-2.86; emotional distress, –2.37; 95% CI, 1.68-3.06; activity limitation, –1.70; 95% CI, 1.14-2.25; and overall quality of life, 3.72; 95% CI, 2.95-4.48) (Table 3). Long-term follow-up was available for 23 patients, who remained representative of the overall group’s baseline SN-5 and quality-of-life scores and demographics (Table 4). The remaining patients were unavailable for follow-up. Statistically significant improvements were maintained in all domains of the SN-5 and overall quality-of-life surveys, as shown by scores at 1 to 2 years after the procedure (sinus infection, –1.43; 95% CI, 0.35-2.52; nasal obstruction, –2.60; 95% CI, 1.56-3.65; allergy symptoms, –1.47; 95% CI, 0.31-2.65; emotional distress, –2.00; 95% CI, 1.04-2.96; activity limitation, –0.87; 95% CI, 0.03-1.71; and overall quality of life, 3.13; 95% CI, 2.01-4.25).
Table 3. Results of Sinonasal Quality of Life and Overall Quality of Life Survey at Baseline and 1-2 Months After the Procedurea.
| Domain | Mean Score (95% CI) | Change in Score (95% CI)b |
|
|---|---|---|---|
| Baseline | 1-2 Months After Procedure | ||
| Sinus infection | 4.55 (3.95-5.15) | 2.00 (1.61-2.39) | −2.55 (1.85-3.26) |
| Nasal obstruction | 5.72 (5.31-6.13) | 2.21 (1.73-2.69) | −3.51 (2.88-4.14) |
| Allergy symptoms | 4.59 (4.03-5.15) | 2.45 (1.99-2.91) | −2.14 (1.43-2.86) |
| Emotional distress | 4.16 (3.58-4.74) | 1.79 (1.42-2.16) | −2.37 (1.68-3.06) |
| Activity limitation | 2.88 (2.35-3.41) | 1.18 (1.01-1.35) | −1.70 (1.14-2.25) |
| Overall quality of life | 5.21 (4.57-5.85) | 8.93 (8.50-9.36) | 3.72 (2.95-4.48) |
N = 43.
Changes of 0.50 are considered trivial change, 0.50-0.99 are small, 1.00-1.49 are moderate, and 1.50 are large. Negative changes indicate improvement for individual domains of the quality of life. Positive changes indicate improvement for overall quality of life.
Table 4. Results of Sinonasal Quality of Life and Overall Quality of Life Survey at Baseline and 1-2 Years After the Procedurea .
| Domain | Mean Score (95% CI) | Change in Score (95% CI)b |
|
|---|---|---|---|
| Baseline | 1-2 Years After Procedure | ||
| Sinus infection | 3.82 (3.00-4.64) | 2.39 (1.63-3.15) | −1.43 (0.35-2.52) |
| Nasal obstruction | 5.30 (4.64-5.96) | 2.70 (1.84-3.56) | −2.60 (1.56-3.65) |
| Allergy symptoms | 4.17 (3.30-5.04) | 2.70 (1.87-3.53) | −1.47 (0.31-2.65) |
| Emotional distress | 4.04 (3.22-4.86) | 2.04 (1.48-2.60) | −2.00 (1.04-2.96) |
| Activity limitation | 2.48 (1.76-3.20) | 1.61 (1.14-2.08) | −0.87 (0.03-1.71) |
| Overall quality of life | 5.39 (4.53-6.25) | 8.52 (7.76-9.28) | 3.13 (2.01-4.25) |
N = 23.
Changes of 0.50 are considered trivial change, 0.50-0.99 are small, 1.00-1.49 are moderate, and 1.50 are large. Negative changes indicate improvement for individual domains of the quality of life. Positive changes indicate improvement for overall quality of life.
Discussion
Surgical IT with concurrent outfracture improves quality of life in children with chronic nasal congestion who have persistent symptoms despite daily use of medications, regardless of test-proven sensitivity to aeroallergens. Patients who presented to our clinic for persistent nasal obstruction were identified to have less than optimal anatomical position of the inferior turbinate relative to the septum, concomitant excessive hypertrophy of inferior turbinate mucosa, or both. For those who have a reported history of test-proven atopy, routine daily medications (including INS, oral antihistamines, and leukotriene receptor antagonists) were insufficient to eliminate persistent symptoms. Consistently, one of us (J.L.W.) observed insufficient space between the medial aspect of the inferior turbinate relative to the position of the septum.
Most of these patients had been prescribed daily INS, oral antihistamines, or leukotriene receptor antagonists. They were often being empirically treated for presumed allergic rhinitis, even when results of testing showed no signs of atopy and patients reported no symptoms of hay fever. We found that once the patients and parents or caretakers perceived no further symptoms and the patients had satisfactory nasal breathing, they chose to stop taking daily medications. Elimination of INS reduces the potential of adverse effects, such as burning, nosebleeds, and nasal perforations. In addition, reducing use of medications decreases costs for families and the health care system in general.
We found consistent improvement in patients’ overall quality of life. In every domain assessed by the SN-5 survey, significant decreases in the frequency of reported symptoms were observed 1 to 2 months after the procedure. Every domain of the SN-5 survey showed large changes postoperatively, represented by a shift in scores of 1.5 or greater. At long-term follow-up (1-2 years after the procedure), improvement persisted in all categories of the SN-5 survey and in overall quality of life. Nasal obstruction, emotional distress, and overall quality of life continued to demonstrate large changes. Both patients and parents reported significant reduction of nasal symptoms, including congestion, rhinorrhea, and snoring. There were no reported adverse events in this study.
To our knowledge, there is no uniform standardized scoring or reporting system to grade inferior turbinate hypertrophy for IT. No clinical studies have shown supremacy for one surgical technique vs another, so technique is chosen based on the surgeon’s clinical judgment and training. Our patients underwent outfracture of inferior turbinates at the same time as IT, as the surgeon in our study perceives the most definitive improvement when performing both procedures concurrently.
There are many techniques described for turbinate reduction, including partial or total turbinectomy, turbinoplasty, electrocautery, cryotherapy, laser cautery, submucosal resection, submucosal resection with lateral displacement, radiofrequency-assisted turbinoplasty, microdebrider-assisted turbinoplasty, and ultrasound turbinate reduction. In the pediatric population, one of us (J.L.W.) chose the minimally invasive, nonobliterative, and submucosal technique to preserve mucociliary function. Both outfracture and turbinoplasty were performed at the same time; we did not aim to compare the 2 techniques separately. In our experience, both techniques are required to improve definitive laminar airflow, even when inferior turbinate hypertrophy is not severe. Physiological and temporal variability make the development of objective assessments or measurements of the degree of inferior turbinate hypertrophy difficult. The human nasal cycle and variability in hypertrophy of the submucosal capacitance tissue can depend on time of day, season, concomitant allergic rhinitis, reflux, and other potential causes of excessive nasal turbinate mucosal congestion. This difference may be owing to venous congestion, allergic rhinitis, anatomical abnormalities in the bony structure or position of the turbinates, or a combination of these factors. It is unclear why children experience frequent and persistent nasal congestion and have inferior turbinate hypertrophy, especially children who do not have positive test results for allergies. Inferior turbinoplasty and outfracture are 2 relatively easy procedures with minimal risks and positive results in symptom relief.
Limitations
Our study has several limitations. This is a case series with planned data collection, the sample size was small, and the roles of various conditions that could affect nasal inflammation, such as allergic rhinitis and rare conditions such as cystic fibrosis, ciliary dyskinesia, or other types of immunodeficiency disorders, were unclear. In addition, our smaller sample size limited subgroup analysis. We did not find significant differences between patients with positive results of allergy testing and those with negative results; however, future studies separating these patients into 2 separate cohorts would be informative in determining if IT with concomitant oufracture of inferior turbinates is efficacious for both groups. Another limitation is the lack of current objective measurement for nasal airway patency other than inferior turbinate hypertrophy on physical examination. Rhinomanometry or other methods of quantifying airflow and nasal airway patency would further validate our findings. One final limitation is the fact that the primary caretakers completed the quality-of-life surveys, as our patients are children. Future research may consider a randomized trial comparing SN-5 scores and patient-reported outcomes for IT alone vs IT with outfracture of inferior turbinates.
Conclusions
Inferior turbinoplasty with concomitant outfracture of inferior turbinates improves the sinonasal quality of life in children who report chronic nasal obstruction regardless of whether the patient has a history of atopy.
References
- 1.Langille M, El-Hakim H. Pediatric inferior turbinoplasty with or without adenoidectomy: preliminary report on improvement of quality of life, symptom control, and safety. J Otolaryngol Head Neck Surg. 2011;40(5):420-426. [PubMed] [Google Scholar]
- 2.Jose J, Coatesworth AP. Inferior turbinate surgery for nasal obstruction in allergic rhinitis after failed medical treatment. Cochrane Database Syst Rev. 2010;(12):CD005235. [DOI] [PubMed] [Google Scholar]
- 3.Hol MK, Huizing EH. Treatment of inferior turbinate pathology: a review and critical evaluation of the different techniques. Rhinology. 2000;38(4):157-166. [PubMed] [Google Scholar]
- 4.Jiang ZY, Pereira KD, Friedman NR, Mitchell RB. Inferior turbinate surgery in children: a survey of practice patterns. Laryngoscope. 2012;122(7):1620-1623. [DOI] [PubMed] [Google Scholar]
- 5.Tan B, Chandra R. Inferior turbinoplasty, procedure In: Kountakis SE, ed. Encyclopedia of Otolaryngology, Head and Neck Surgery. Augusta, GA: Springer; 2013:1327-1330. [Google Scholar]
- 6.Arganbright JM, Jensen EL, Mattingly J, Gao D, Chan KH. Utility of inferior turbinoplasty for the treatment of nasal obstruction in children: a 10-year review. JAMA Otolaryngol Head Neck Surg. 2015;141(10):901-904. [DOI] [PubMed] [Google Scholar]
- 7.Kay DJ, Rosenfeld RM. Quality of life for children with persistent sinonasal symptoms. Otolaryngol Head Neck Surg. 2003;128(1):17-26. [DOI] [PubMed] [Google Scholar]
- 8.Juniper EF, Guyatt GH, Willan A, Griffith LE. Determining a minimal important change in a disease-specific quality of life questionnaire. J Clin Epidemiol. 1994;47(1):81-87. [DOI] [PubMed] [Google Scholar]
- 9.Corren J, Baroody FM, Pawankar R. Allergic and nonallergic rhinitis In: Adkinson NF Jr, Bochner BS, Burks AW, et al. , eds. Middleton’s Allergy: Principles and Practice. 8th ed Philadelphia, PA: Elsevier Mosby; 2013:664-685. [Google Scholar]
- 10.Leong SC, Eccles R. Inferior turbinate surgery and nasal airflow: evidence-based management. Curr Opin Otolaryngol Head Neck Surg. 2010;18(1):54-59. [DOI] [PubMed] [Google Scholar]
- 11.Larrabee YC, Kacker A. Which inferior turbinate reduction technique best decreases nasal obstruction? Laryngoscope. 2014;124(4):814-815. [DOI] [PubMed] [Google Scholar]
- 12.Bhandarkar ND, Smith TL. Outcomes of surgery for inferior turbinate hypertrophy. Curr Opin Otolaryngol Head Neck Surg. 2010;18(1):49-53. [DOI] [PubMed] [Google Scholar]