Abstract
Purpose of Review
This review aims to describe the tendon transfer options for treating irreparable rotator cuff tears (RCTs). Options for transfer include latissimus dorsi and lower trapezius transfers for posterior-superior RCTs and pectoralis major and latissimus dorsi transfer for anterior-superior RCTs.
Recent Findings
While the latissimus dorsi tendon transfer has historically been performed for posterosuperior RCTs, the lower trapezius transfer is a more anatomic option and has demonstrated promising results in recent studies. Similarly, the pectoralis major transfer has historically been the tendon transfer of choice for anterosuperior RCTs. However, the latissimus dorsi tendon transfer has recently been shown to be a safe and anatomic tendon transfer for subscapularis insufficiency.
Summary
The treatment of irreparable RCTs involves complex decision making. Tendon transfer procedures can restore the glenohumeral joint force couples, allowing restoration of near-normal shoulder kinematics. Benefits include reliable pain relief, increased function, and increased strength. Proper selection of donor tendon is crucial, and the principles of tendon transfer procedures must be adhered to for maximal benefit.
Keywords: Tendon transfer, Rotator cuff tear, Latissimus dorsi, Lower trapezius, Pectoralis major
Introduction
Rotator cuff disease is among the most common musculoskeletal disorders. The rotator cuff muscles include the supraspinatus superiorly, subscapularis anteriorly, and infraspinatus and teres minor posteriorly. The tendons of the rotator cuff converge at the proximal humerus providing compression of the humeral head to the glenoid [1]. This compressive force allows the periscapular muscles to move the humerus around the glenoid through the arc of motion. Disruption of the normal force couples causes abnormal kinematics in the anterior-posterior and superior-inferior planes.
The incidence of rotator cuff pathology increases with advanced age, with asymptomatic tears present in up to 54% of patients > 60 years [2]. Many patients are not symptomatic enough to require surgical intervention, but these tears often progress over time [3, 4]. Though the incidence of progression is currently poorly understood, some tears progress to an irreparable stage [5].
Rotator cuff tears (RCTs) are classified as massive and irreparable if they (1) involve two or more tendons, (2) are retracted and shortened to the level of the glenoid, and (3) are associated with advanced fatty infiltration of the muscle belly as described by Goutallier et al. (Table 1) [5–7]. Attempted repair of these tears results in failure to heal in up to 94% of patients [8]. Failure generally occurs within 6 months of primary fixation [9, 10]. Symptoms of re-tear include impaired overhead function, increased pain, decreased strength, limited passive ROM, and lower overall satisfaction with shoulder function [11].
Table 1.
ᅟSagittal T1-106 weighted magnetic resonance imaging
| Goutallier grading system of fatty degeneration in rotator cuff tear | |
|---|---|
| Grade 0 | Completely normal muscle, without any fatty streaks |
| Grade 1 | Some fatty streaks |
| Grade 2 | Fat is present, but less fat than muscle |
| Grade 3 | As much fat as muscle |
| Grade 4 | More fat is present than muscle |
Additionally, progressive shoulder osteoarthritis is often noted in patients with irreparable RCTs over time as eccentric loads are placed upon the glenoid. Therefore, there is interest in attempting to restore more anatomic joint mechanics to slow the progression of osteoarthritis or halt the progression altogether, particularly in younger patients. In these cases, tendon transfer procedures provide options to restore shoulder function.
History, Physical Exam, and Imaging
Irreparable RCTs present with varying levels of dysfunction and pain, though not all are symptomatic [12]. Most patients present with an acute loss of function after a traumatic incident, though patients may present with a slow functional decline and increasing pain without a history of trauma.
Examination of the shoulder and periscapular area includes inspection for atrophy, especially over the supraspinatus and infraspinatus fossae. Patients with an irreparable RCT may present with a wide variety of active shoulder ROM, from full ROM to pseudoparalysis.
Diagnosing insufficiency of the posterior-superior cuff involves assessment of the supraspinatus, infraspinatus, and teres minor. The supraspinatus is assessed with the Jobe test [13]. The infraspinatus is assessed through external rotation with the arm in adduction. A lag sign may be present in these patients. Importantly, a positive lag sign has been correlated with the size of RCT [14]. The teres minor is assessed with the arm in 90° of abduction while evaluating external rotation against resistance.
Insufficiency of the anterior-superior cuff is determined through assessment of the subscapularis. These occur less frequently than posterior-superior tears [15]. The subscapularis functions as the primary internal rotator and anterior dynamic stabilizer of the shoulder [16]. Patients presenting with an anterior-superior deficiency often describe internal rotation weakness and anterior shoulder pain. Multiple physical examination maneuvers are used to test the subscapularis including the belly-press [17], lift-off [18], and bear-hug tests [19]. These tears often allow anterosuperior escape of the humeral head.
Imaging begins with plain film radiographs including an anteroposterior (AP) view to assess glenohumeral joint pathology as well as superior migration of the humeral head (Fig. 1). Imaging features consistent with an irreparable posterior-superior tear on the AP view include and acromiohumeral distance < 7 mm [20], or static superior migration of the humeral head [21]. Additionally, axillary and scapular-Y views should be obtained to assess anterior or posterior subluxation and the supraspinatus outlet, respectively.
Fig. 1.

Anteroposterior (AP) radiograph showing superior migration of the humeral head due to massive rotator cuff tear. Additionally, there is significant glenohumeral arthritis present
Advanced imaging should be performed to further characterize the RCT. Sagittal T1-weighted magnetic resonance imaging (MRI) is used to assess muscle bellies for fatty infiltration as described by Goutallier et al. (Table 1, Fig. 2) [5]. Repair of Goutallier grade 3 and 4 RCTs have shown poor results [22].
Fig. 2.
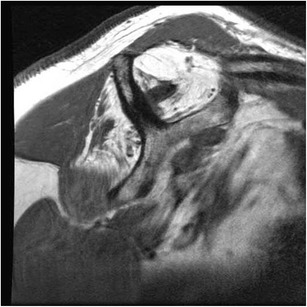
Sagittal T1-weighted MRI view of scapula demonstrating a massive anterior-superior rotator cuff tear with fatty degeneration of the supraspinatus and infraspinatus musculature
Management Options
Nonoperative management can be beneficial for patients with irreparable RCTs. Guided physical therapy should focus on strengthening any remaining cuff tissue, periscapular strengthening, and deltoid reconditioning [23]. Nonsteroidal anti-inflammatory medications and corticosteroid injections can also be performed.
However, patients who fail nonoperative management should be considered for surgical intervention. Surgical options include arthroscopic débridement, partial RCT repair, superior capsular reconstruction, arthroplasty, or tendon transfer procedures [24–26]. Shoulder function and pain often improves after débridement or partial repair [27, 28]. However, progressive shoulder osteoarthritis frequently develops over time [28]. Reverse shoulder arthroplasty has shown good results in non-arthritic patients with massive RCTs, but is not a sustainable option for younger, active patients [29]. Tendon transfer procedures can provide treatment options for these patients.
When considering tendon transfer reconstruction, all procedures should adhere to the following important principles: (1) the transferred muscle should be expendable without compromising the donor site, (2) the transferred and recipient muscle should have a similar excursion and tension, (3) the line of pull of the transferred tendon and recipient muscle should be similar, and (4) the transferred muscle should replace one function of the recipient muscle [30].
Posterior Superior Tear Tendon Transfer Options
Traditionally, the latissimus dorsi transfer with or without teres major has been used for posterior-superior RCTs. However, the lower trapezius transfer now offers an additional option that more closely adheres to the principles of tendon transfer reconstruction.
Latissimus Dorsi Transfer
The latissimus dorsi adducts, internally rotates, and extends the humerus. It has a broad origination from the sacrum, posterior iliac crest, spinous processes of T7-L5, and ribs 10–12 (Fig. 3). The tendon inserts onto the intertubercular groove of the proximal humerus between the pectoralis major anteriorly and the teres major posteriorly. The thoracodorsal nerve (C6-C8) from the posterior cord of the brachial plexus innervates the latissimus, while the thoracodorsal artery provides the blood supply. The neurovascular pedicle enters the muscle approximately 2-cm medial to the musculotendinous border [31]. The axillary nerve lies proximal to the latissimus insertion, while the radial nerve lies inferior and medial to the latissimus insertion.
Fig. 3.
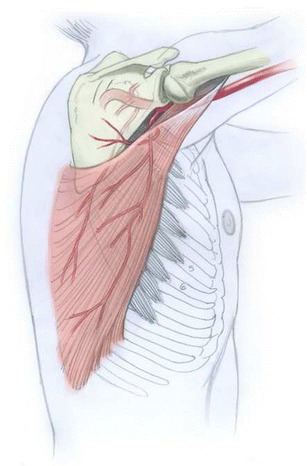
Latissimus dorsi anatomy highlighting the muscle’s origin and insertion. This figure also shows the blood supply of latissimus dorsi muscle provided by the thoracodorsal artery
The latissimus dorsi transfer is most commonly used to reconstruct posterior-superior RCTs. Originally described by Gerber in 1988, the latissimus is transferred to provide an inferior force that is counterbalanced by the deltoid and intact subscapularis [20]. This action reconstitutes the posterior force couple, allowing the latissimus to effectively function as an external rotator and humeral head depressor [30].
Proper patient selection is critical for positive, lasting results after latissimus transfer. The subscapularis should be functioning and intact to properly recreate the posterior force couple with the latissimus transfer [32•]. Additionally, an intact subscapularis increases glenohumeral stability after latissimus transfer [33]. Preoperative passive and active shoulder range of motion measurement is critical, as poor results have been shown in patients with passive abduction and forward flexion less than 80° as well as shoulder pseudoparalysis [34, 35].
Preoperative imaging findings also predict results after latissimus transfer. The AP plain films should be scrutinized for glenohumeral arthritis and rotator cuff arthropathy. Patients with acromial acetabularization and decrease in acromiohumeral interval (Hamada stage III) or narrowing of the glenohumeral interval (Hamada stage IVa) are at risk of failure after latissimus transfer [32•, 36]. Improved outcomes have been shown in patients with teres minor Goutallier grade 2 or less, with better forward flexion and external rotation after transfer than patients with Goutallier grade 3 or grade 4 changes [37, 38].
The open approach for latissimus transfer originally described by Gerber involves two incisions [20]. A superior approach to the rotator cuff is performed with the incision placed just medial to the lateral acromial border. An osteotomy is performed through the lateral acromion which contains the origin of the middle deltoid. After mobilizing the lateral acromion, the integrity of the rotator cuff is evaluated. The subscapularis is repaired when feasible, and tendons of the infraspinatus and supraspinatus are trimmed to healthy tissue and mobilized. The tendons are mobilized to the greater tuberosity if possible and repaired, either partially or fully. As the muscles often have changes of fatty infiltration and atrophy, and repair is highly susceptible to re-rupture, the repair will be augmented with the latissimus dorsi tendon transfer. The second incision over the latissimus muscle belly in the axilla and the muscle is identified running anteriorly to the teres major. The interval between the two muscles is identified distally, and dissection is performed proximally and distally to fully mobilize the tendon. The tendon is then released from the humerus, and a path for the tendon transfer is created between the deltoid and remaining posterior rotator cuff. The tendon is passed and secured to the anterior portion of the greater tuberosity and proximal tendon of the subscapularis for further augmentation.
Long-term results have been favorable with the two-incision approach. Gerber demonstrated long-term viability of the transfer with 74% good or excellent results at 10-year follow-up. Mean subjective shoulder value (SSV) increased from 29% preoperatively to 70% at final follow-up, with significantly increased ROM in forward flexion, abduction, external rotation, as well as increased strength [6]. Similarly, El-Azab et al. reported on 93 shoulders at 9-year follow-up treated with latissimus dorsi transfer with similarly positive results in pain relief, shoulder function, and strength [32•]. The failure rate was 10% at final follow-up, and 4% of patients were converted to a reverse shoulder arthroplasty (RSA). Complications after the procedure included axillary hematoma requiring surgical release in the majority of patients, deltoid insufficiency after attempted repair, frozen shoulder, and traumatic failure of the tendon.
Less invasive techniques have been explored for latissimus transfer. With the originally described two-incision technique, deltoid muscle strength is frequently impaired due to iatrogenic injury [39]. A one-incision approach was therefore described by Habermeyer et al. to preserve the corachumeral arch and deltoid muscle. This was further refined through an arthroscopic-assisted approach to latissimus transfer [40]. This technique that involves harvest of the latissimus is performed as described above for the open procedure. The latissimus tendon is tubularized using two nonabsorbable sutures for fixation [41]. The arthroscope is introduced through the posterior portal and the infraspinatus fossa is prepared using a high-speed burr. The arthroscope is then placed into the anterior portal and the plane between the deltoid and infraspinatus fascia is developed. A large curved clamp is passed from the anterior portal through the newly created space to the axillary incision to pass the tubularized latissimus tendon, and the tendon is secured to the humerus via transosseous technique [42].
Results after arthroscopically assisted latissimus transfer have compared favorably to the traditional two-incision open approach [39, 43, 44]. Grimberg et al. reported outcomes of arthroscopically assisted latissimus dorsi transfer for posterosuperior RCTs in 55 patients [45]. Patients improved SSV from 26% preoperatively to 71% postoperatively, which compare favorably to Gerber’s results [20]. Additionally, significant improvements were noted in forward flexion, abduction, external rotation, and abduction strength. These results were confirmed in other series, most notably through the largest series by Castricini et al. [46•]. This series included 86 patients with a 3-year follow-up with patients experiencing significant improvements in pain, range of motion, and strength. Excellent or good outcomes were achieved in 82% of patients in the series. Notably, patients who had previously had rotator cuff repair or biceps tenodesis were found to have worse outcomes when compared to patients without previous surgery in motion and strength. Additionally, these patients were less likely to be satisfied with the operation and have a lower Constant and Murley score (CMS) versus primary surgery patients. Finally, though latissimus dorsi transfer for posterosuperior RCTs is indicated for young, high demand patients, the results of arthroscopically assisted latissimus transfer for patients up to 69 years old have been favorable [45], especially those with high preoperative CMS. Therefore, functional status, rather than age, seems to be the factor to consider when determining surgical candidates. Complications are similar to the open approach, including seroma after latissimus tunneling, frozen shoulder, and failure of the tendon attachment [46•].
Lower Trapezius Transfer
The trapezius muscle has three parts: the upper, middle, and lower which function together to elevate, retract, and externally rotate the scapula (Fig. 4) [47]. It originates from the spinous processes of C7-T12 and the occiput. The upper portion inserts over the lateral third of the posterior clavicle, while the middle and lower portions attach over the medial acromion and spine of the scapula. The trapezius receives its blood supply from the transverse cervical artery and innervation from the spinal accessory nerve (cranial nerve XI) [48, 49].
Fig. 4.
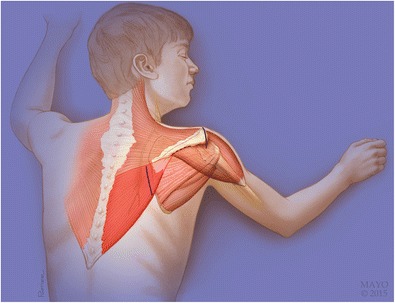
Origin and insertion of the trapezius muscle, highlighting the lower trapezius. Incisions for the open lower trapezius transfer are shown with solid lines. A 5-cm incision is made 1-cm medial to the medial scapular spine as shown here. The tendon will be passed through the area designated by the dashed line. Note the close proximity of the spinal accessory nerve (CN XI) to the incision. The nerve lies below the fascia of the trapezius, making superficial dissection in this region safe. Used with permission of Mayo Foundation for Medical Education and Research. All rights reserved
The lower trapezius is a more anatomic alternative tendon transfer for irreparable posterior-superior RCTs than the latissimus dorsi. As shown in a recent cadaveric study, the lower trapezius is an ideal transfer option as its origin is cranial to the latissimus dorsi and medial to the infraspinatus fossa of the scapula, with a nearly identical line of pull as the infraspinatus [50]. The lower trapezius transfer provided a more effective external rotation moment arm when compared to the latissimus dorsi transfer. Additionally, excursion and tension forces are very similar to the infraspinatus [48].
Lower trapezius transfer was originally described by Elhassan et al. for patients with a paralytic shoulder lacking external rotation [48]. This is performed through an open approach. A 5-cm vertical incision is placed 1-cm medial to the medial scapular spine, and dissection carried through subcutaneous tissue to the lower trapezius (Fig. 4). The lateral border of the muscle is identified above an area of triangular fat. The tendon is detached from the spine of the scapula and dissected medially along the upper border of the tendon. Importantly, the spinal accessory nerve lies within the fascial layer on the undersurface of the trapezius, approximately 2-cm medial to the medial border of the scapula. This makes superficial dissection safe to separate the lower and middle trapezius, but deep dissection should be avoided. Two nonabsorbable sutures are placed on each side of the tendon in a Krakow configuration, and the tendon is left in the wound. A limited exposure to the rotator cuff is then performed as described above for the open latissimus exposure. An Achilles tendon allograft is used for greater excursion and attached using the previously placed Krakow sutures (Fig. 5a, b). The tendon is then passed deep to the deltoid, through the infraspinatus fascia using a blunt, curved clamp to retrieve the tendon from the medial incision (Fig. 6a–c). The Achilles allograft is then secured to the lateral portion of the posterosuperior greater tuberosity using multiple transosseous nonabsorbable sutures, and the wound is closed over a deep drain.
Fig. 5.
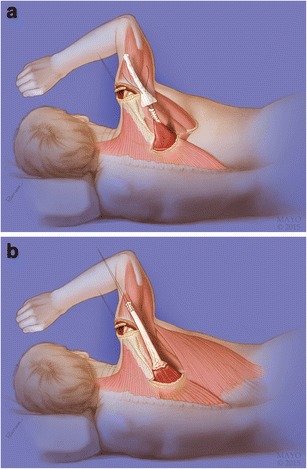
a Tendon augmentation using Achilles tendon allograft for length. The thin portion of the Achilles allograft is attached to the tendinous portion of the lower trapezius using two nonabsorbable sutures. b Prepared lower trapezius augmented with Achilles allograft. Used with permission of Mayo Foundation for Medical Education and Research. All rights reserved
Fig. 6.
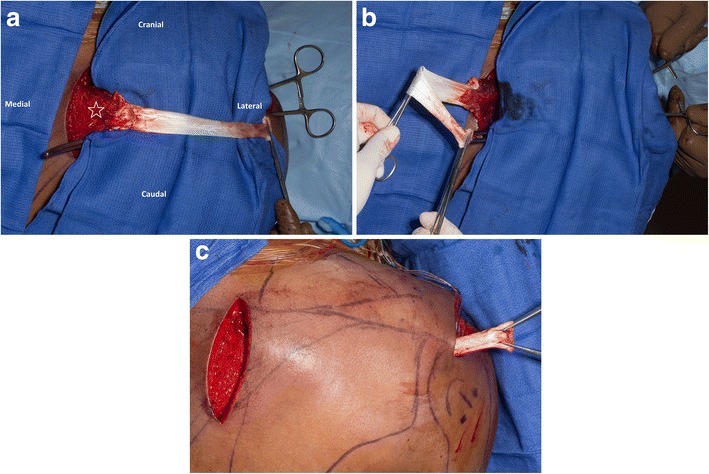
Intraoperative image of lower trapezius (star) augmented with Achilles allograft. b Preparing tendon for transfer through previously created path. The clamp is passed deep to the posterior deltoid towards the medial wound. c The tendon is retrieved through the lateral wound
This technique for lower trapezius transfer for patients with paralytic shoulders lacking external rotation was performed in 111 patients. External rotation improvement was achieved in all patients, with a mean improvement in external rotation of 70° [48]. In another study of 52 patients with traumatic brachial plexus injuries, lower trapezius transfer was performed alone or as part of multiple transfers. Significant improvements were noted in external rotation, pain scores, and SSV scores [30]. The most common complication after the procedure was seroma (10%) after transfer due to subcutaneous tunneling for the transfer [48].
Due to these encouraging biomechanical and clinical results, the use of the lower trapezius transfer has expanded with multiple studies demonstrating effectiveness in restoring external rotation [30, 48, 50]. Elhassan et al. reported outcomes in 33 patients treated with lower trapezius transfer using an Achilles tendon allograft for reconstruction of symptomatic irreparable RCTs. At a final follow-up of nearly 4 years, 97% of patients had a significant improvement in pain, SSV, and shoulder and hand score. Range of motion increased significantly with mean improvements of 50° in forward flexion, 50° in abduction, and 30° in external rotation. Additionally, patients with > 60° of preoperative flexion achieved more significant range of motion gains. Due to these favorable outcomes, lower trapezius transfer is our preferred method to reconstruct posterior-superior RCTs [51•].
Anterior-Superior Tear
Several transfer options for anterior-superior RCTs have been reported including pectoralis major transfer and latissimus dorsi transfer with or without teres major. While the pectoralis transfer has traditionally been performed, latissimus dorsi transfer is now our preferred method for reconstruction of the subscapularis.
Pectoralis Major Transfer
The pectoralis major adducts, flexes, and internally rotates the humerus. The pectoralis major is made up of two heads, the clavicular and sternal head. The clavicular head originates on the medial aspect of the clavicle, and the sternal head originates from the upper portion of the sternum and the second through fourth ribs. The two heads converge near their insertion with the sternal head rotating posteriorly and the clavicular head inserting more superficially at the lateral bicipital groove [52]. The main blood supply is from the pectoral branch of the thoracoacromial artery and innervation from the medial and lateral pectoral nerves. The lateral and medial pectoral nerves enter the muscle 12.5 and 11.9 cm from the tendinous insertion, respectively [52]. The lateral pectoral nerve passes medial to the pectoralis major, making dissection lateral to the pectorals minor safe [53].
The pectoralis major transfer is the most common tendon transfer performed for anterior-superior insufficiencies to restore the anterior force couple due to subscapularis insufficiency. First described by Wirth and Rockwood, the transfer was originally performed anterior to the conjoined tendon [54]. Resch et al. further refined the technique to be performed under the conjoined tendon [55], which has been shown to be biomechanically superior [56]. To perform the transfer, a standard deltopectoral approach is performed with the cephalic vein taken laterally. The deltoid is mobilized from the humerus and a retractor is placed below it to allow access to the proximal humerus. The axillary nerve is identified as it travels posteriorly around the humeral neck and protected with a vessel loop. Next, the subscapularis is released circumferentially to allow better mobilization. The superior and inferior borders of the pectoralis tendon at the humeral insertion are identified. The superior one-half to two-thirds of the pectoralis major tendon is released from the insertion, and the sternal and clavicular heads are identified. The sternal head is mobilized, and the clavicular head is then repaired back to its humeral insertion. Multiple nonabsorbable sutures are placed through the sternal head of the pectoralis major tendon for passage. The subcoracoid space is then developed between the conjoint tendon and the pectoralis minor below. Special attention is paid to the musculocutaneous nerve which must be protected at all times. The nerve should remain deep to the pectoralis major as it is passed. The tendon is passed in this space and repaired to the lesser tuberosity using multiple nonabsorbable sutures in a Mason-Allen technique. The wound is irrigated and closed over a deep drain.
Outcomes for the pectoralis major transfer have been variable, providing consistent improvements in pain while providing varying functional improvements [55]. Resch et al. reported constant score increases from 22 to 54 after transfer [55]. Similarly, Elhassan et al. reported increases from 41 to 61 in constant scores after pectoralis transfer, with better outcomes reported in patients with a well-centered humeral head preoperatively [57]. Better outcomes were also achieved in patients with an intact supraspinatus [58, 59]. Poor outcomes and frequent failures occur in patients with anterior subluxation of the humeral head [57].
Pectoralis Major Transfer Versus Latissimus Dorsi Transfer
While pectoralis major transfers have provided consistent pain relief, reports have shown only modest improvements in function and stability [57]. These variable results are likely due to the pectoralis major tendon transfer not replacing the lost function of the subscapularis muscle biomechanically. The line of pull of the pectoralis major is significantly differently than that of the subscapularis. Notably, the pectoralis major originates from an anterior position from the clavicle and sternum while the subscapularis originates from a posterior position from the scapular fossa. This causes the line of pull of the two muscles to be nearly orthogonal to one another in certain arm positions which causes anterior translation of the humeral head instead of desired internal rotation. This likely explains the poor results reported in patients with anterior subluxation of the humeral head preoperatively [57].
In contrast, the latissimus dorsi transfer to the subscapularis insertion provides a more anatomic transfer. The latissimus dorsi originates from posterior chest wall and inserts just medial and inferior to the subscapularis, more closely replicating the insertion and origin of the subscapularis [60•].
Latissimus Dorsi Transfer
Our preferred method for latissimus transfer for irreparable subscapularis tears is through an arthroscopically assisted technique. The latissimus harvest is performed at the level of the axillary fold with a 5-cm incision over the palpable muscle belly. Dissection is performed towards the insertion of the latissimus, taking care to separate the tendon from the teres major. The latissimus is placed under tension and released from the bony insertion and tagged with multiple nonabsorbable Krakow sutures. The arthroscope is introduced through a posterior portal, and anterior and anterolateral portals are created. A large grasping clamp is placed into the anterolateral portal and passed deep to the pectoralis major toward the latissimus dorsi harvest site. Once visualized, the latissimus is grasped and brought arthroscopically from the posterior wound through to the level of the humeral head.
The latissimus is intussuscepted into a trough at the subscapularis insertion and secured using transcortical button to the posterior cortex of the humerus.
Elhassan et al. recently described the feasibility and safety of this transfer with or without teres major transfer [60•]. The risk of nerve compression was found to be low when transferring the latissimus dorsi to the lesser tuberosity. Additionally, the origin and insertion of the latissimus dorsi nearly replicate the line of pull of the subscapularis. Therefore, latissimus dorsi transfer is now our preferred method for reconstruction of the subscapularis.
Conclusion
Management of massive irreparable rotator cuff tears, especially in young active patients, is complex. Tendon transfer operations can reconstitute the force couple of the shoulder, leading to improved biomechanics. While multiple transfer options exist, our preferred transfer options are the lower trapezius for posterosuperior insufficiency and the latissimus dorsi for anterosuperior insufficiency.
Compliance with Ethical Standards
Conflict of Interests
The authors whose names are listed above certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Rotator Cuff Repair
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Burkhart SS. Arthroscopic treatment of massive rotator cuff tears. Clinical results and biomechanical rationale. Clin Orthop Relat Res. 1991;267:45–56. [PubMed] [Google Scholar]
- 2.Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am. 1995;77(1):10–15. doi: 10.2106/00004623-199501000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Yamaguchi K, Tetro AM, Blam O, Evanoff BA, Teefey SA, Middleton WD. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elb Surg. 2001;10(3):199–203. doi: 10.1067/mse.2001.113086. [DOI] [PubMed] [Google Scholar]
- 4.Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006;88(8):1699–1704. doi: 10.2106/JBJS.E.00835. [DOI] [PubMed] [Google Scholar]
- 5.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78–83. [PubMed] [Google Scholar]
- 6.Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82(4):505–515. doi: 10.2106/00004623-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Liem D, Lengers N, Dedy N, Poetzl W, Steinbeck J, Marquardt B. Arthroscopic debridement of massive irreparable rotator cuff tears. Arthroscopy. 2008;24(7):743–748. doi: 10.1016/j.arthro.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 8.Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86-A(2):219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Koh KH, Laddha MS, Lim TK, Park JH, Yoo JC. Serial structural and functional assessments of rotator cuff repairs: do they differ at 6 and 19 months postoperatively? J Shoulder Elb Surg. 2012;21(7):859–866. doi: 10.1016/j.jse.2011.05.027. [DOI] [PubMed] [Google Scholar]
- 10.Iannotti JP, Deutsch A, Green A, Rudicel S, Christensen J, Marraffino S, Rodeo S. Time to failure after rotator cuff repair: a prospective imaging study. J Bone Joint Surg Am. 2013;95(11):965–971. doi: 10.2106/JBJS.L.00708. [DOI] [PubMed] [Google Scholar]
- 11.Shamsudin A, Lam PH, Peters K, Rubenis I, Hackett L, Murrell GA. Revision versus primary arthroscopic rotator cuff repair: a 2-year analysis of outcomes in 360 patients. Am J Sports Med. 2015;43(3):557–564. doi: 10.1177/0363546514560729. [DOI] [PubMed] [Google Scholar]
- 12.Moosmayer S, Smith HJ, Tariq R, Larmo A. Prevalence and characteristics of asymptomatic tears of the rotator cuff: an ultrasonographic and clinical study. J Bone Joint Surg Br. 2009;91(2):196–200. doi: 10.1302/0301-620X.91B2.21069. [DOI] [PubMed] [Google Scholar]
- 13.Jain NB, Luz J, Higgins LD, Dong Y, Warner JJ, Matzkin E, et al. The diagnostic accuracy of special tests for rotator cuff tear: the ROW cohort study. Am J Phys Med Rehabil. 2017;96(3):176–183. doi: 10.1097/PHM.0000000000000566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Castoldi F, Blonna D, Hertel R. External rotation lag sign revisited: accuracy for diagnosis of full thickness supraspinatus tear. J Shoulder Elb Surg. 2009;18(4):529–534. doi: 10.1016/j.jse.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 15.Lyons RP, Green A. Subscapularis tendon tears. J Am Acad Orthop Surg. 2005;13(5):353–363. doi: 10.5435/00124635-200509000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Perry J. Anatomy and biomechanics of the shoulder in throwing, swimming, gymnastics, and tennis. Clin Sports Med. 1983;2(2):247–270. [PubMed] [Google Scholar]
- 17.Burkhart SS, Tehrany AM. Arthroscopic subscapularis tendon repair: technique and preliminary results. Arthroscopy. 2002;18(5):454–463. doi: 10.1053/jars.2002.30648. [DOI] [PubMed] [Google Scholar]
- 18.Gerber C, Krushell RJ. Isolated rupture of the tendon of the subscapularis muscle. Clinical features in 16 cases. J Bone Joint Surg Br. 1991;73(3):389–394. doi: 10.1302/0301-620X.73B3.1670434. [DOI] [PubMed] [Google Scholar]
- 19.Barth JR, Burkhart SS, De Beer JF. The bear-hug test: a new and sensitive test for diagnosing a subscapularis tear. Arthroscopy. 2006;22(10):1076–1084. doi: 10.1016/j.arthro.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 20.Gerber C, Vinh TS, Hertel R, Hess CW. Latissimus dorsi transfer for the treatment of massive tears of the rotator cuff. A preliminary report. Clin Orthop Relat Res. 1988;232:51–61. [PubMed] [Google Scholar]
- 21.Omid R, Lee B. Tendon transfers for irreparable rotator cuff tears. J Am Acad Orthop Surg. 2013;21(8):492–501. doi: 10.5435/JAAOS-21-08-492. [DOI] [PubMed] [Google Scholar]
- 22.Gladstone JN, Bishop JY, Lo IK, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007;35(5):719–728. doi: 10.1177/0363546506297539. [DOI] [PubMed] [Google Scholar]
- 23.Levy O, Mullett H, Roberts S, Copeland S. The role of anterior deltoid reeducation in patients with massive irreparable degenerative rotator cuff tears. J Shoulder Elb Surg. 2008;17(6):863–870. doi: 10.1016/j.jse.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 24.Burkhart SS, Nottage WM, Ogilvie-Harris DJ, Kohn HS, Pachelli A. Partial repair of irreparable rotator cuff tears. Arthroscopy. 1994;10(4):363–370. doi: 10.1016/S0749-8063(05)80186-0. [DOI] [PubMed] [Google Scholar]
- 25.Wellmann M, Lichtenberg S, da Silva G, Magosch P, Habermeyer P. Results of arthroscopic partial repair of large retracted rotator cuff tears. Arthroscopy. 2013;29(8):1275–1282. doi: 10.1016/j.arthro.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 26.Gartsman GM. Massive, irreparable tears of the rotator cuff. Results of operative debridement and subacromial decompression. J Bone Joint Surg Am. 1997;79(5):715–721. doi: 10.2106/00004623-199705000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Iagulli ND, Field LD, Hobgood ER, Ramsey JR, Savoie FH. Comparison of partial versus complete arthroscopic repair of massive rotator cuff tears. Am J Sports Med. 2012;40(5):1022–1026. doi: 10.1177/0363546512438763. [DOI] [PubMed] [Google Scholar]
- 28.Berth A, Neumann W, Awiszus F, Pap G. Massive rotator cuff tears: functional outcome after debridement or arthroscopic partial repair. J Orthop Traumatol. 2010;11(1):13–20. doi: 10.1007/s10195-010-0084-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harreld KL, Puskas BL, Frankle M. Massive rotator cuff tears without arthropathy: when to consider reverse shoulder arthroplasty. J Bone Joint Surg Am. 2011;93(10):973–984. [PubMed] [Google Scholar]
- 30.Elhassan B, Bishop A, Shin A, Spinner R. Shoulder tendon transfer options for adult patients with brachial plexus injury. J Hand Surg Am. 2010;35(7):1211–1219. doi: 10.1016/j.jhsa.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 31.Bartlett SP, May JW, Yaremchuk MJ. The latissimus dorsi muscle: a fresh cadaver study of the primary neurovascular pedicle. Plast Reconstr Surg. 1981;67(5):631–636. doi: 10.1097/00006534-198105000-00010. [DOI] [PubMed] [Google Scholar]
- 32.El-Azab HM, Rott O, Irlenbusch U. Long-term follow-up after latissimus dorsi transfer for irreparable posterosuperior rotator cuff tears. J Bone Joint Surg Am. 2015;97(6):462–469. doi: 10.2106/JBJS.M.00235. [DOI] [PubMed] [Google Scholar]
- 33.Werner CM, Zingg PO, Lie D, Jacob HA, Gerber C. The biomechanical role of the subscapularis in latissimus dorsi transfer for the treatment of irreparable rotator cuff tears. J Shoulder Elb Surg. 2006;15(6):736–742. doi: 10.1016/j.jse.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 34.Buchmann S, Plath JE, Imhoff AB. Latissimus dorsi transfer for the treatment of irreparable rotator tears: indication, surgical technique, and modifications. Oper Orthop Traumatol. 2012;24(6):502–512. doi: 10.1007/s00064-012-0162-y. [DOI] [PubMed] [Google Scholar]
- 35.Iannotti JP, Hennigan S, Herzog R, Kella S, Kelley M, Leggin B, Williams GR. Latissimus dorsi tendon transfer for irreparable posterosuperior rotator cuff tears. Factors affecting outcome. J Bone Joint Surg Am. 2006;88(2):342–348. doi: 10.2106/JBJS.D.02996. [DOI] [PubMed] [Google Scholar]
- 36.Hamada K, Yamanaka K, Uchiyama Y, Mikasa T, Mikasa M. A radiographic classification of massive rotator cuff tear arthritis. Clin Orthop Relat Res. 2011;469(9):2452–2436. doi: 10.1007/s11999-011-1896-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Costouros JG, Espinosa N, Schmid MR, Gerber C. Teres minor integrity predicts outcome of latissimus dorsi tendon transfer for irreparable rotator cuff tears. J Shoulder Elb Surg. 2007;16(6):727–734. doi: 10.1016/j.jse.2007.02.128. [DOI] [PubMed] [Google Scholar]
- 38.Moursy M, Forstner R, Koller H, Resch H, Tauber M. Latissimus dorsi tendon transfer for irreparable rotator cuff tears: a modified technique to improve tendon transfer integrity. J Bone Joint Surg Am. 2009;91(8):1924–1931. doi: 10.2106/JBJS.H.00515. [DOI] [PubMed] [Google Scholar]
- 39.Habermeyer P, Magosch P, Rudolph T, Lichtenberg S, Liem D. Transfer of the tendon of latissimus dorsi for the treatment of massive tears of the rotator cuff: a new single-incision technique. J Bone Joint Surg Br. 2006;88(2):208–212. doi: 10.1302/0301-620X.88B2.16830. [DOI] [PubMed] [Google Scholar]
- 40.Gervasi E, Causero A, Parodi PC, Raimondo D, Tancredi G. Arthroscopic latissimus dorsi transfer. Arthroscopy. 2007;23(11):1243.e1–1243.e4. doi: 10.1016/j.arthro.2006.12.021. [DOI] [PubMed] [Google Scholar]
- 41.Goldberg BA, Elhassan B, Marciniak S, Dunn JH. Surgical anatomy of latissimus dorsi muscle in transfers about the shoulder. Am J Orthop (Belle Mead NJ) 2009;38(3):E64–E67. [PubMed] [Google Scholar]
- 42.Goldstein Y, Grimberg J, Valenti P, Chechik O, Drexler M, Kany J. Arthroscopic fixation with a minimally invasive axillary approach for latissimus dorsi transfer using an endobutton in massive and irreparable postero-superior cuff tears. Int J Shoulder Surg. 2013;7(2):79–82. doi: 10.4103/0973-6042.114223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Aoki M, Okamura K, Fukushima S, Takahashi T, Ogino T. Transfer of latissimus dorsi for irreparable rotator-cuff tears. J Bone Joint Surg Br. 1996;78(5):761–766. doi: 10.1302/0301-620X.78B5.0780761. [DOI] [PubMed] [Google Scholar]
- 44.Lehman AC, Dumpert J, Wood NA, Visty AQ, Farritor SM, Oleynikov D. In vivo robotics for natural orifice transgastric peritoneoscopy. Stud Health Technol Inform. 2008;132:236–241. [PubMed] [Google Scholar]
- 45.Grimberg J, Kany J, Valenti P, Amaravathi R, Ramalingam AT. Arthroscopic-assisted latissimus dorsi tendon transfer for irreparable posterosuperior cuff tears. Arthroscopy. 2015;31(4):599–607.e1. doi: 10.1016/j.arthro.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 46.Castricini R, De Benedetto M, Familiari F, De Gori M, De Nardo P, Orlando N, Gasparini G, Galasso O. Functional status and failed rotator cuff repair predict outcomes after arthroscopic-assisted latissimus dorsi transfer for irreparable massive rotator cuff tears. J Shoulder Elb Surg. 2016;25(4):658–665. doi: 10.1016/j.jse.2015.08.043. [DOI] [PubMed] [Google Scholar]
- 47.Gerber C. Latissimus dorsi transfer for the treatment of irreparable tears of the rotator cuff. Clin Orthop Relat Res. 1992;275:152–160. [PubMed] [Google Scholar]
- 48.Elhassan B. Lower trapezius transfer for shoulder external rotation in patients with paralytic shoulder. J Hand Surg Am. 2014;39(3):556–562. doi: 10.1016/j.jhsa.2013.12.016. [DOI] [PubMed] [Google Scholar]
- 49.Omid R, Cavallero MJ, Granholm D, Villacis DC, Yi AM. Surgical anatomy of the lower trapezius tendon transfer. J Shoulder Elb Surg. 2015;24(9):1353–1358. doi: 10.1016/j.jse.2014.12.033. [DOI] [PubMed] [Google Scholar]
- 50.Hartzler RU, Barlow JD, An KN, Elhassan BT. Biomechanical effectiveness of different types of tendon transfers to the shoulder for external rotation. J Shoulder Elb Surg. 2012;21(10):1370–1376. doi: 10.1016/j.jse.2012.01.026. [DOI] [PubMed] [Google Scholar]
- 51.Elhassan BT, Wagner ER, Werthel JD. Outcome of lower trapezius transfer to reconstruct massive irreparable posterior-superior rotator cuff tear. J Shoulder Elb Surg. 2016;25(8):1346–1353. doi: 10.1016/j.jse.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 52.Klepps SJ, Goldfarb C, Flatow E, Galatz LM, Yamaguchi K. Anatomic evaluation of the subcoracoid pectoralis major transfer in human cadavers. J Shoulder Elb Surg. 2001;10(5):453–459. doi: 10.1067/mse.2001.117125. [DOI] [PubMed] [Google Scholar]
- 53.Jennings GJ, Keereweer S, Buijze GA, De Beer J, DuToit D. Transfer of segmentally split pectoralis major for the treatment of irreparable rupture of the subscapularis tendon. J Shoulder Elb Surg. 2007;16(6):837–842. doi: 10.1016/j.jse.2007.03.030. [DOI] [PubMed] [Google Scholar]
- 54.Wirth MA, Rockwood CA. Operative treatment of irreparable rupture of the subscapularis. J Bone Joint Surg Am. 1997;79(5):722–731. doi: 10.2106/00004623-199705000-00012. [DOI] [PubMed] [Google Scholar]
- 55.Resch H, Povacz P, Ritter E, Matschi W. Transfer of the pectoralis major muscle for the treatment of irreparable rupture of the subscapularis tendon. J Bone Joint Surg Am. 2000;82(3):372–382. doi: 10.2106/00004623-200003000-00008. [DOI] [PubMed] [Google Scholar]
- 56.Konrad GG, Sudkamp NP, Kreuz PC, Jolly JT, McMahon PJ, Debski RE. Pectoralis major tendon transfers above or underneath the conjoint tendon in subscapularis-deficient shoulders. An in vitro biomechanical analysis. J Bone Joint Surg Am. 2007;89(11):2477–2484. doi: 10.2106/JBJS.F.00811. [DOI] [PubMed] [Google Scholar]
- 57.Elhassan B, Ozbaydar M, Massimini D, Diller D, Higgins L, Warner JJ. Transfer of pectoralis major for the treatment of irreparable tears of subscapularis: does it work? J Bone Joint Surg Br. 2008;90(8):1059–1065. doi: 10.1302/0301-620X.90B8.20659. [DOI] [PubMed] [Google Scholar]
- 58.Jost B, Puskas GJ, Lustenberger A, Gerber C. Outcome of pectoralis major transfer for the treatment of irreparable subscapularis tears. J Bone Joint Surg Am. 2003;85-A(10):1944–1951. doi: 10.2106/00004623-200310000-00012. [DOI] [PubMed] [Google Scholar]
- 59.Galatz LM, Connor PM, Calfee RP, Hsu JC, Yamaguchi K. Pectoralis major transfer for anterior-superior subluxation in massive rotator cuff insufficiency. J Shoulder Elb Surg. 2003;12(1):1–5. doi: 10.1067/mse.2003.128137. [DOI] [PubMed] [Google Scholar]
- 60.Elhassan B, Christensen TJ, Wagner ER. Feasibility of latissimus and teres major transfer to reconstruct irreparable subscapularis tendon tear: an anatomic study. J Shoulder Elb Surg. 2014;23(4):492–499. doi: 10.1016/j.jse.2013.07.046. [DOI] [PubMed] [Google Scholar]


