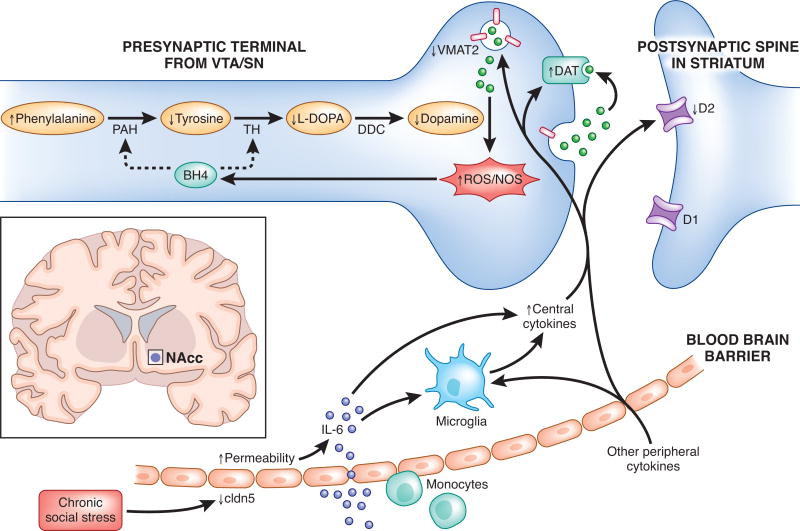
Figure 2.
Potential signaling pathways linking peripheral inflammation to disruption of dopaminergic function. Adapted from [66]. As suggested by one recent study [59], individuals who go on to develop a depressive phenotype following stress show increased permeability of the blood brain barrier (BBB) to peripheral cytokines such as IL-6. The peripheral cytokines that cross the blood brain barrier, as well as central cytokines produced by activated microglia, may contribute to oxidative stress and reactive oxygen species (ROS) generation. This, in turn, may increase the oxidation of tetrahydrobiopterin (BH4), a cofactor required for the conversion of phenylalanine to tyrosine and tyrosine to L-3,4-dihydroxyphenylalanine (L-DOPA), thereby impeding DA synthesis. Additionally, central inflammatory cytokines may decrease the expression or function of the vesicular monoamine transporter 2 (VMAT2) as well as increase the expression or function of the dopamine transporter (DAT), increasing DA and leading to increased generation of ROS. Finally, inflammatory cytokines may also decrease DA signaling by reducing DA D2 receptors. D1, dopamine 1 receptor 1; D2, dopamine 2 receptor; DDC, dopamine decarboxylase; NOS, nitric oxide synthase; PAH, phenylalanine hydroxylase; ROS, reactive oxygen species; SN; substantia nigra; TH, tyrosine hydroxylase; VTA, ventral tegmental area.