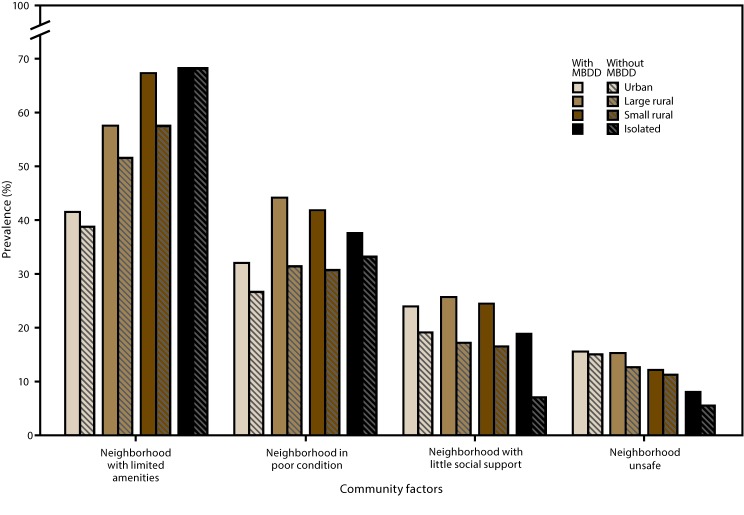
FIGURE 2.
Prevalence of selected community factors* among children aged 2–8 years with and without mental, behavioral, and developmental disorders† in urban and rural areas§ — National Survey of Children’s Health, United States, 2011–2012
Abbreviations: MBDD = mental, behavioral, or developmental disorder; RUCA = rural-urban commuting area.
* Neighborhood with limited amenities: Based on responses of “no” to at least one of the following statements: “Please tell me if the following places and things are available to children in your neighborhood, even if [the child] does not actually use them”: 1) sidewalks or walking paths; 2) a park or playground area; 3) a recreation center, community center, or boys’ or girls’ club; 4) a library or bookmobile. Neighborhood in poor condition: Based on responses of “yes” to any of the following three questions: “In your neighborhood, is there litter or garbage on the street or sidewalk? How about poorly kept or rundown housing? How about vandalism such as broken windows or graffiti?” Neighborhood with little social support: Based on responses of “definitely agree,” “somewhat agree,” “somewhat disagree,” or “definitely disagree” to the following four statements about their neighborhood or community: “People in this neighborhood help each other out; we watch out for each other’s children in this neighborhood; there are people I can count on in this neighborhood; if my child were outside playing and got hurt or scared, there are adults nearby who I trust to help my child.” Responses were scored 1–4 (“definitely agree” through “definitely disagree”), and an average score was calculated; averages ≥2.25 indicated a lack of support. Neighborhood unsafe: Based on responses of “never” or “sometimes” (compared with “usually” or “always”) to the question, “How often do you feel [the child] is safe in your community or neighborhood?”
† Significant differences in the prevalence of certain community factors were found between children with and without MBDDs in certain urban and rural areas. Neighborhood with limited amenities: no areas; neighborhood in poor condition: urban, large rural, and small rural areas; neighborhood with little social support: urban, large rural, and isolated areas; neighborhood unsafe: no areas.
§ Urban and rural designations were determined using the four-category classification of the 2006 RUCAs, a census tract–based classification system. Urban areas (RUCA codes 1.0, 1.1, 2.0, 2.1, 3.0, 4.1, 5.1, 7.1, 8.1, and 10.1) include metropolitan areas and surrounding towns from which commuters flow to an urban area; large rural areas (RUCA codes 4.0, 4.2, 5.0, 5.2, 6.0, and 6.1) include large towns (micropolitan areas) with populations of 10,000–49,999 and their surrounding areas; small rural areas (RUCA codes 7.0, 7.2, 7.3, 7.4, 8.0, 8.2, 8.3, 8.4, 9.0, 9.1, and 9.2) include small towns with populations of 2,500–9,999 and their surrounding areas; isolated areas (RUCA codes 10.0, 10.2, 10.3, 10.4, 10.5, and 10.6) are not near towns with a population of ≥2,500 (Source: US Department of Health and Human Services, Health Resources and Services Administration. The health and well-being of children in rural areas: a portrait of the nation 2011–2012. Rockville, MD: US Department of Health and Human Services; 2015. https://mchb.hrsa.gov/nsch/2011-12/rural-health/pdf/rh_2015_book.pdf).