INTRODUCTION
One in twenty [1] hospital admissions results in an interhospital transfer, amounting to approximately 1.7 million patients being transferred annually. Inter-hospital transfers are growing in number due to increasing consolidation of healthcare systems [2] and specialty services that are concentrated at urban academic medical centers. Transferred patients strain healthcare systems’ resources due to increased lengths of stay, increased resource utilization, and increased mortality. Efforts to ameliorate these burdens are receiving increased attention.
There is strong national consensus about the need to develop useful clinical decision support tools to improve healthcare delivery by leveraging the vast amount of electronic medical record (EMR) data to guide clinicians, patients, and families in making difficult healthcare decisions [3–7]. Currently, limited evidence and no national guidelines [8] exist to support decision makers when considering if they should transfer a patient to another hospital, a decision that can carry significant financial burdens for individuals (i.e. patients) and health systems.
Interhospital transfer patients present several challenges when attempting to include and analyze data to either refine current risk prediction models, or build a clinical decision support system capable of using real-time data. A primary challenge is the lack of access to transport EMRs, precluding incorporating transport data into any hospital-based decision support system. Another problem is the improper application of risk mortality prediction tools such as the Acute Physiology and Chronic Health Evaluation (APACHE) IV tool [9], widely used as the national benchmark for mortality prediction and resource use. The APACHE IV tool is designed for use with the patient’s first 24 hours of physiologic data, skewing results when applied to transported patients who are often >24 hours post-admission from their incident admission at the sending hospital.
Because of these reasons it is not possible to compare transferred versus non-transferred patients using current scoring systems [10–12], or to evaluate the prognostic value of information associated with patients’ transfer encounters. The purpose of this paper is hence to assess if common data elements from medical transport provides incremental prognostic value on post-transfer mortality, both individually and in combination with the APACHE IV risk model estimates.
MATERIALS AND METHODS
Patients transported within the Cleveland Clinic health system, that consists of a quaternary main campus in Cleveland and eight surrounding community hospitals, by the hospital-based Critical Care Transport team from 2010 to 2015 where included in the study. The primary source of data used in this study was The Cleveland Clinic Transport Data Mart (CCTDM) which is an IRB-approved (IRB# 14-1556) EMR-based data repository that includes all patients undergoing medical transport to or from a Cleveland Clinic Health System facility. The primary data domains within the CCTDM include all health system based hospital encounters, all variables included in APACHE prediction modelling, and common transport data elements.
The APACHE IV data and associated risk score is obtained for all transported patients according to standard protocol, although this information is unavailable within the registry for a small number of patients. For this study, we analyzed all transported patients with valid APACHE IV data and associated CCTDM data. Only the most recent transport encounter was analyzed for each patient.
The data were randomly partitioned into an 75% model development cohort and a (remaining) 25% test cohort prior to analysis, in order to minimize the likelihood of over-fitting the models to a specific training dataset [13].
Generally, we evaluated the accuracy of probability estimates for in-hospital mortality through two lenses: discrimination and calibration. Discrimination was characterized using concordance indices (or C-statistics). C-statistics range from 0.5 to 1.0, where a value of 0.5 indicates no discriminative ability for a risk score (i.e., similar to flipping a coin) and a value of 1.0 indicates perfect separation of events from non-events according to the risk score. Together with a point estimate for the C-statistics, we estimated bootstrap 95% confidence intervals. Calibration was assessed graphically using the method of Dalton [14].
Three models were evaluated on calibration and discrimination: 1) the original APACHE IV predicted probability of mortality; 2) the predicted probability of mortality arising from a logistic regression model that incorporated (only) predictors from the CCTDM (see below); and 3) the predicted probability of mortality arising from a logistic regression model that incorporated the APACHE IV score in conjunction with the predictors from the CCTDM.
RESULTS
The transport registry included a total of 12,359 total records, corresponding to 11,218 unique patients. Taking the most recent admission per patient, 4,016 were then removed due to unavailable transport data – most often related to no patient transfer. An additional 170 patients with partial missing data were removed, leaving a final analyzed sample of 7,032 patients. Descriptive statistics on these 7,032 patients are given in Table 1.
Table 1.
Summary of baseline patient characteristics.
| Age (years, mean ± sd) | 60.6 ± 16.5 |
| Male Sex (percent) | 52.4 |
| Race (percent) | |
| White/Caucasian | 74.8 |
| Black/African/Haitian | 17.3 |
| Other/Unknown | 7.8 |
| APACHE IV Probability of In-Hospital Mortality (median [q1, q3]) | 0.12 [0.05, 0.29] |
| Source of Admission (percent) | |
| ED | 42.8 |
| Gen Floor | 0.8 |
| ICU | 22.5 |
| SDU/Telemetry Unit | 0.6 |
| Non-Specific | 33.3 |
| Diabetes Mellitus (percent) | 25.6 |
| AIDS (percent) | 0.3 |
| COPD (percent) | |
| None | 78.9 |
| No Limitations | 10.8 |
| Moderate | 1.1 |
| Severe | 9.2 |
| Dialysis (percent) | 4.7 |
| Heart Rate (BPM, mean ± sd) | 97.7 ± 30.5 |
| Hematocrit (%, mean ± sd) | 31.8 ± 7.6 |
| Mean Arterial Pressure (mmHg, mean ± sd) | 91.6 ± 37.4 |
| Potassium (mEq/L median [q1, q3]) | 3.8 [3.4, 4.3] |
| Respiratory Rate (breaths/min, mean ± sd) | 34.2 ± 13.7 |
| Serum Albumin (g/dL, median [q1, q3]) | 3.1 [2.5, 3.8] |
| Serum Bicarbonate (mEq/L, median [q1, q3]) | 22.0 [19.0, 25.0] |
| Serum Bilirubin mg/dL, median [q1, q3]) | 0.6 [0.4, 1.1] |
| Serum BUN (mg/dL, median [q1, q3]) | 22.0 [14.0, 37.0] |
| Serum Creatinine (mg/dL, median [q1, q3]) | 0.9 [0.7, 1.7] |
| Serum Na (mEq/L, mean ± sd) | 137.6 ± 6.1 |
| Serum WBC x 103 cells/μL, median [q1, q3]) | 10.2 [7.2, 15.8] |
| Reason For Transport (percent) | |
| Unknown | 54.3 |
| Care Not Available | 28.5 |
| Protocol (Autolaunch) | 8.8 |
| Other | 8.4 |
| Time En Route To Completed (min, median [q1, q3]) | 71.0 [0.0, 103.0] |
| Time Arrived To Completed (min, median [q1, q3]) | 52.0 [0.0, 75.0] |
| Time Departing Facility To Completed (min, median [q1, q3]) | 31.0 [0.0, 48.0] |
| Transport Modality (percent) | |
| Adult Ground | 21.2 |
| Adult Rotor | 17.2 |
| Non CCT Transport | 15.1 |
| Adult Fixed Wing | 1.1 |
| Unknown/Other | 45.4 |
| Hospital Referring Unit (percent) | |
| ED | 50.1 |
| ICU | 38.7 |
| CCU | 2.7 |
| Other/Unknown | 8.5 |
| Arterial Line Placed (percent) | 14.8 |
| Intubation (percent) | 1.7 |
| Central Line Placed (percent) | 0.7 |
| Cardiac Assist Device Used (percent) | 0.3 |
| Pacer Used (percent) | <0.1 |
Our randomly-selected training cohort contained 5,274patients and our test cohort contained 1,758 patients. After fitting the logistic regression models and applying the models to the test cohort to obtain predicted probabilities, we found C-statistics [95% confidence intervals] of 0.854 [0.830 – 0.877] for the original APACHE-IV model; 0.640 [0.606 – 0.673] for the model that involved only variables associated with the transport encounter; and 0.854 [0.831 – 0.876] for the model that included both the APACHE-IV probability of mortality and the transport variables. Odds ratio estimates from the two models we estimated are given in Table 2.
Table 2.
Transport Only and Transport with APACHE Regression Models
| Variable | Transport-Only Model | Transport + APACHE-IV Model |
|---|---|---|
| APACHE-IV Probability of Mortality (per 10% increase) | n/a | 1.85 [1.78, 1.93] |
| Time between Arrival and Completion (per 10 minutes) | 1.01 [1.00, 1.02] | 1.01 [1.00, 1.02] |
| Arterial Line Placed | 1.91 [1.58, 2.31] | 0.96 [0.76, 1.22] |
| Cardiac Assist Device Used | 2.49 [0.71, 8.76] | 2.26 [0.49, 10.3] |
| Central Line Placed | 3.28 [1.51, 7.10] | 2.67 [0.97, 7.33] |
| Time between Departure and Completion (per 10 minutes) | 0.99 [0.98, 1.00] | 0.99 [0.98, 1.00] |
| Time between En-Route and Completion (per 10 minutes) | 1.01 [1.00, 1.02] | 1.01 [1.00, 1.02] |
| Intubation | 1.80 [1.15, 2.82] | 0.64 [0.38,.10] |
| Mode Completed: Adult Ground | (reference) | (reference) |
| Mode Completed: Adult Fixed Wing | 1.28 [0.67, 2.42] | 1.59 [0.76, 3.32] |
| Mode Completed: Adult Rotor | 0.98 [0.77, 1.25] | 0.82 [0.61, 1.09] |
| Mode Completed: Non CCT Transport | 0.81 [0.61, 1.07] | 1.06 [0.77, 1.47] |
| Mode Completed: Unknown/Other | 1.02 [0.77, 1.36] | 1.01 [0.72, 1.42] |
| Reason for Transport: Unknown | (reference) | (reference) |
| Reason for Transport: Care Not Available | 0.85 [0.64, 1.11] | 0.87 [0.62, 1.21] |
| Reason for Transport: Other | 0.97 [0.69, 1.36] | 1.08 [0.72, 1.61] |
| Reason for Transport: Protocol (Autolaunch) | 0.86 [0.60, 1.24] | 0.59 [0.38, 0.92] |
| Referring Unit: ED | (reference) | (reference) |
| Referring Unit: CCU | 1.68 [1.10, 2.55] | 1.79 [1.10, 2.92] |
| Referring Unit: ICU | 1.64 [1.40, 1.92] | 1.35 [1.11, 1.63] |
| Referring Unit: Other/Unknown | 0.82 [0.60, 1.12] | 1.05 [0.74, 1.49] |
Odds ratios and approximate 95% confidence intervals for effects within a) the model using only predictors obtained from transport encounter data and b) the model using both the APACHE-IV probability of mortality score and the predictors from the transport encounter. The intercept for the transport-only model was −1.826 and the intercept term for the model using both APACHE-IV and transport data was −3.265.
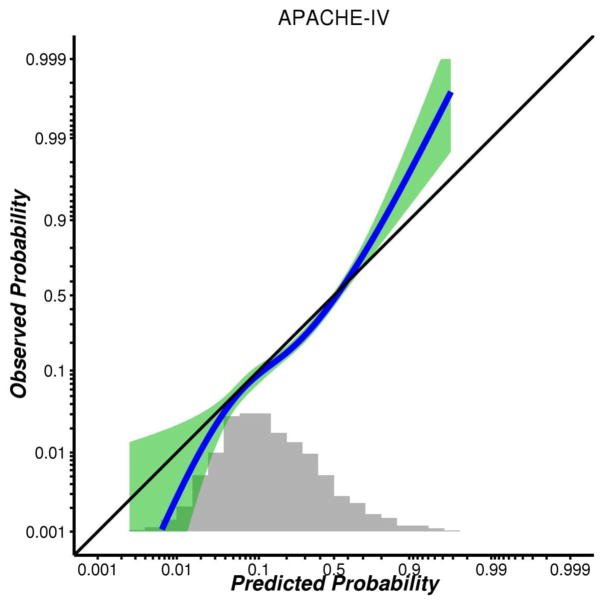
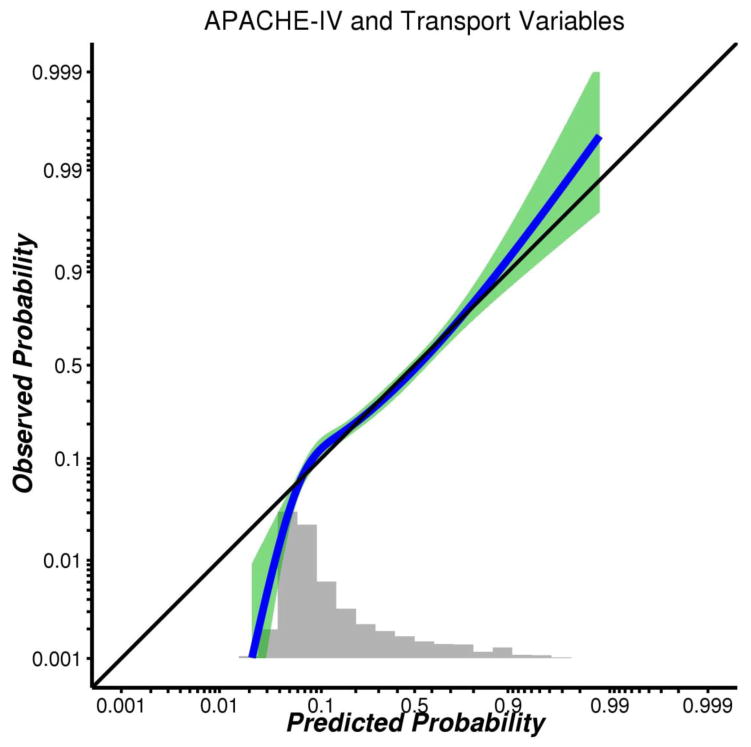
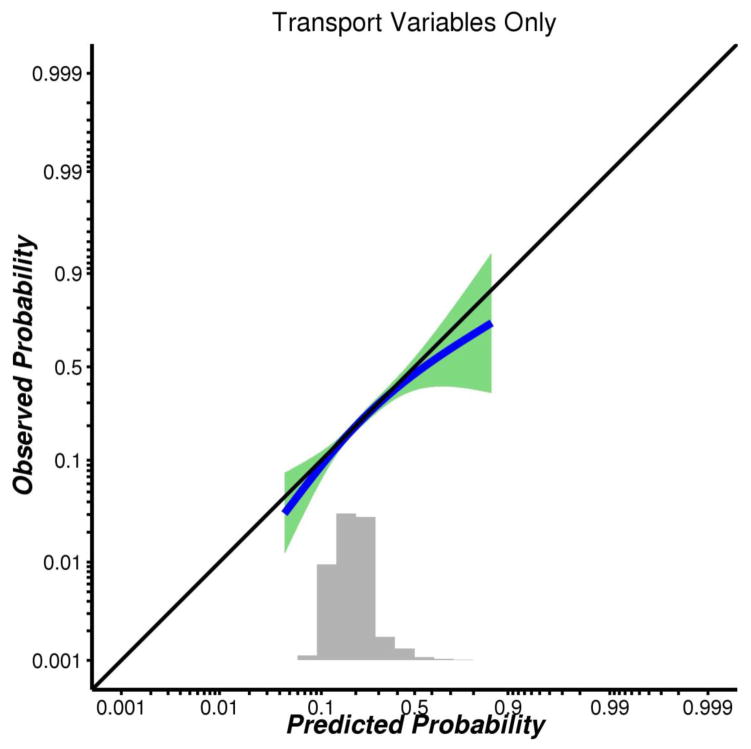
Calibration plots for these three models, based on test-cohort data, are given in Figures 1–3. These plots indicate that: i) calibration was generally good for the APACHE-IV model, save for some under-estimation among patients with extremely high predicted probabilities of mortality (say, >0.8); ii) calibration was good for the transport-only model, although the distribution of predicted risk was rather condensed around values between 0.1 and 0.3; and iii) the combined model had good calibration (save for some over-estimation among patients with predicted probabilities below about 0.04) and a more dispersed distribution of predicted risk.
Figure 1.
Figure 3.
DISCUSSION
We found that transport-related predictors did not add to the predictive accuracy of the APACHE-IV model. When modelled alone, common transport variables had poorer accuracy than the current APACHE-IV prediction model. Significant predictors of mortality post-transfer from the CCTDM included procedures (placement of an arterial line, placement of a central catheter, or intubation) and being transferred from an intensive care unit – regardless of intensive care unit type.
Our findings that procedures performed by transport crews predict increased mortality are potentially useful in consideration of studies that have shown that patients transported by critical care transport teams show improved prediction scores, or less likelihood of dying, upon arrival at the receiving institution [12]. However, the improved mortality scores upon arrival are not correlated with increased rates of survival and thus represents an intermittent improvement in physiologic stability without concomitant change in survival trajectory. Although transport teams may provide short-term improvement in a patient’s physiologic status, the overall impact of transport may be diminished when considering the patient’s overall clinical trajectory.
Additionally, the finding that procedures performed by transport teams significantly predict post-transfer mortality are likely due to the procedure variables acting as a surrogate indicator for patient severity of illness. Although the procedures are performed and whether potentially appropriate interventions are administered or not (e.g. arterial line placement and antihypertensive medication administration) associated reductions in mortality are not realized. While noted limitations of current studies include not having access to data on previous interventions and the patient’s response to treatment[15–17] at the sending hospital and during transport, the anticipated improved predictive accuracy of these additional predictors may be of limited value during the transport phase.
After combining the CCTDM and APACHE data, admission source remained one of only two significant predictors in the final combined model. Admission source is widely supported as a significant predictor of post-transfer mortality in multiple patient populations [15, 17–21]. Similar to transport team procedures, while controlling for admission source via a single categorical variable may generally account for some “undefined, unmeasured, source of severity” of illness, or poor response to care [15] at the sending hospital, such an approach is not sensitive to potentially-useful details which may underlie observed clinical differences between patients from different admission sources. Further, admission source is not included in the other most commonly used Mortality Probability Model III [22, 23]. Just as procedures performed by the transport team is a significant predictor, the significance of admission source requires further investigation to discern if it is a surrogate marker for severity of illness and patient trajectory that may be unaffected by transfer and admission to higher levels of care.
Only one variable predicted improved mortality after transfer, that being the reason for transport as autolaunch. Autolaunch is the name of the expedited transfer process that is initiated when a patient presenting with a time-sensitive condition (i.e. myocardial infraction, trauma, stroke, aortic syndrome) is transferred after one phone call which immediately dispatches a helicopter that transfers the patiently directly to a waiting team treatment team (i.e. catheterization lab, operating room) at the receiving hospital. These results are consistent with studies that have shown a survival advantage for those experiencing time-sensitive emergencies and receive earlier treatment [24, 25].
There are several limitations of this study. The primary limitation is that the data are limited to one health system, and as such are not generalizable beyond it. Second, only records that contained complete data were used potentially introducing a selection bias. Lastly, this study did not include all transport related variables, due to data incompleteness, potentially limiting the impact that transport data may have on post-transport prediction modelling.
Future Directions
There are several significant findings from this study that inform next steps for investigation and clinical considerations. First, this is the first study with adequate power to assess the influence that transport has on post-transfer outcome. The most significant finding is that mode of transport, often the primary focus of most medical transfer studies, has no influence on post-transfer outcome [26–28]. Another significant finding is that transport time intervals (e.g. time between arrival and completion) where also not significant predictors of post-transfer mortality, countering previous findings that support time as an independent predictor [29]. The previous two findings, when taken in combination, directly challenge the primary assumption that more severely ill patients need to be moved by helicopter because it reduces out of hospital time and therefore improves patient outcomes.
Second, the primary finding that transport variables do not add prognostic value is an important finding that addresses one of the two major gaps in research of transported patient outcomes—those gaps being what happens to the patient prior to transfer and during transfer. These findings support focusing on the pre-transfer period specifically. Focusing on the pretransfer period is significant for several reasons. There is a major push to leverage the now widely available electronic medical record data to achieve a learning health care system—or the concept of using clinical data and analyzing it in near real-time to improve clinical practice on an individual patient basis [30]. Using data from the pre-transport phase is necessary to drive a clinical decision support system that would support a clinician deciding whether to transport a patient because that is the only data that is available at the time the decision is being made, simplifying future data modelling approaches.
Third, the finding that patients experiencing a time-sensitive emergency and undergo an autolaunch transfer exhibit improved mortality supports focusing future data modelling efforts on prospectively identifying patients that will benefit from earlier transfer to a high level of care for those that may be likely to fail conventional therapy or require aggressive therapy and interventions. Identifying patients that may or will require aggressive care earlier, and sending them to the tertiary center before they decompensate to the point of requiring tertiary services, can be one approach to reducing mortality for patients requiring transfer. Recent applications of telemedicine monitoring of community hospital ICUs by tertiary care providers has provided support of the usefulness of expert providers identifying patients that require transfer sooner [31, 32].
CONCLUSIONS
In Conclusion, we found that common transport variables did not in isolation, or in combination with APACHE-IV variables add to predictive accuracy of transferred patients post-transport mortality.
Future work should focus on the pre-transfer hospitalization and identifying factors that predict which patients require earlier transfer to higher levels of care.
Figure 2.
Highlights.
Interhospital transfer patients experience increased mortality compared to patients that present directly to the same hospital and did not undergo interhospital transfer.
Transport data in combination with APACHE data does not increase post-transport mortality prognostication.
Patients transferred from sending hospital ICUs experience higher mortality rates.
Patients transferred via expedited helicopter transfer protocols (Autolaunch) experience increased survival post-transfer.
Future research should focus on pre-transport data.
Acknowledgments
Funding: JED was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant KL2TR000440. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
There are no conflicts of interest to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Reimer AP, Schiltz N, Koroukian SM, Madigan E. National Incidence of Medical Transfer: Patient Characteristics and Regional Variation. Journal of Health and Human Services Administration. 2015;38(4):509–28. [PubMed] [Google Scholar]
- 2.Cutler DM, Scott Morton F. Hospitals, market share, and consolidation. JAMA. 2013;310(18):1964–70. doi: 10.1001/jama.2013.281675. [DOI] [PubMed] [Google Scholar]
- 3.Kohn L, Corrigan JM, Donaldson M, editors. Committee on Quality of Health Care in America. Washington, DC: Institute of Medicine: National Academy Press; 2000. To Err is Human: building a safer healthcare system. [Google Scholar]
- 4.Crossing the Quality Chasm: A New Health System for the 21st century. Washington, DC: Institute of Medicine: National Academy Press; 2001. [PubMed] [Google Scholar]
- 5.Berner ES. Clinical Decision Support Systems: State of the Art. Rockville, Maryland: 2009. [Google Scholar]
- 6.Lobach D, Sanders GD, Bright TJ, Wong A, Dhurjati R, Bristow E, et al. Evidence Report No. 203. (Prepared by the Duke Evidence-based Practice Center under Contract No. 290-2007-10066-I.) Rockville, MD: Agency for Healthcare Research and Quality; 2012. Enabling Health Care Decisionmaking Through Clinical Decision Support and Knowledge Management. [PMC free article] [PubMed] [Google Scholar]
- 7.Medicine) IIo. Digital Infrastructure for the Learning Health System: The Foundation for Continuous Improvement in Health and Health Care: Workshop Series Summary. Washington, DC: 2011. [PubMed] [Google Scholar]
- 8.Floccare DJ, Stuhlmiller DF, Braithwaite SA, Thomas SH, Madden JF, Hankins DG, et al. Appropriate and safe utilization of helicopter emergency medical services: a joint position statement with resource document. Prehosp Emerg Care. 2013;17(4):521–5. doi: 10.3109/10903127.2013.804139. [DOI] [PubMed] [Google Scholar]
- 9.Zimmerman JE, Kramer AA, McNair DS, Malila FM. Acute Physiology and Chronic Health Evaluation (APACHE) IV: hospital mortality assessment for today’s critically ill patients. Crit Care Med. 2006;34(5):1297–310. doi: 10.1097/01.CCM.0000215112.84523.F0. [DOI] [PubMed] [Google Scholar]
- 10.Droogh JM, Renes MH, Ligtenberg JJ, Zijlstra JG. A prolonged ICU stay after interhospital transport? Crit Care. 2012;16(6):465. doi: 10.1186/cc11857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barratt H, Harrison DA, Rowan KM, Raine R. Effect of non-clinical inter-hospital critical care unit to unit transfer of critically ill patients: a propensity-matched cohort analysis. Crit Care. 2012;16(5):R179. doi: 10.1186/cc11662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Droogh JM, Smit M, Absalom AR, Ligtenberg JJ, Zijlstra JG. Transferring the critically ill patient: are we there yet? Crit Care. 2015;19:62. doi: 10.1186/s13054-015-0749-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hastie T, Tibshirani R, Friedman J. The Elements of Statistical Learning: data mining, inference and prediction. 2. Springer-Verlang; 2009. [Google Scholar]
- 14.Dalton JE. Flexible recalibration of binary clinical prediction models. Stat Med. 2013;32(2):282–9. doi: 10.1002/sim.5544. [DOI] [PubMed] [Google Scholar]
- 15.Rosenberg AL, Hofer TP, Strachan C, Watts CM, Hayward RA. Accepting Critically Ill Transfer Patients: Adverse Effect on a Referral Center’s Outcome and Benchmark Measures. Annals of Internal Medicine. 2003;138(11):882–90. doi: 10.7326/0003-4819-138-11-200306030-00009. [DOI] [PubMed] [Google Scholar]
- 16.Visser P, Harriss LR, Hart GK, Bohensky M, Sundaresan L, Kennedy M. Factors involved in intensive care unit mortality following medical retrieval: identifying differences between intensive care unit survivors and non-survivors. Emerg Med Australas. 2013;25(3):260–7. doi: 10.1111/1742-6723.12075. [DOI] [PubMed] [Google Scholar]
- 17.Escarce JJ, Kelley MA. Admission source to the medical intensive care unit predicts hospital death independent of APACHE II score. JAMA. 1990;264(18):2389–94. [PubMed] [Google Scholar]
- 18.Arthur KR, Kelz RR, Mills AM, Reinke CE, Robertson MP, Sims CA, et al. Interhospital transfer: an independent risk factor for mortality in the surgical intensive care unit. Am Surg. 2013;79(9):909–13. doi: 10.1177/000313481307900929. [DOI] [PubMed] [Google Scholar]
- 19.Dragsted L, Jorgensen J. Interhospital comparisons of patient outcome from intensive care: Importance of lead-time bias. Critical Care Medicine. 1989;17(5):418–22. doi: 10.1097/00003246-198905000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Golestanian E, Scruggs JE, Gangnon RE, Mak RP, Wood KE. Effect of interhospital transfer on resource utilization and outcomes at a tertiary care referral center. Crit Care Med. 2007;35(6):1470–6. doi: 10.1097/01.CCM.0000265741.16192.D9. [DOI] [PubMed] [Google Scholar]
- 21.Gerber DR, Schorr C, Ahmed I, Dellinger RP, Parrillo J. Location of patients before transfer to a tertiary care intensive care unit: impact on outcome. J Crit Care. 2009;24(1):108–13. doi: 10.1016/j.jcrc.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 22.Higgins TL, Teres D, Copes WS, Nathanson BH, Stark M, Kramer AA. Assessing contemporary intensive care unit outcome: an updated Mortality Probability Admission Model (MPM0-III) Crit Care Med. 2007;35(3):827–35. doi: 10.1097/01.CCM.0000257337.63529.9F. [DOI] [PubMed] [Google Scholar]
- 23.Higgins TL, Kramer AA, Nathanson BH, Copes W, Stark M, Teres D. Prospective validation of the intensive care unit admission Mortality Probability Model (MPM0-III) Crit Care Med. 2009;37(5):1619–23. doi: 10.1097/CCM.0b013e31819ded31. [DOI] [PubMed] [Google Scholar]
- 24.Terkelsen CJ, Sorensen JT, Maeng M, Jensen LO, Tilsted HH, Trautner S, et al. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010;304(7):763–71. doi: 10.1001/jama.2010.1139. [DOI] [PubMed] [Google Scholar]
- 25.Hacke W, Donnan G, Fieschi C, Kaste M, von Kummer R, Broderick JP, et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet. 2004;363(9411):768–74. doi: 10.1016/S0140-6736(04)15692-4. [DOI] [PubMed] [Google Scholar]
- 26.Tsuchiya A, Tsutsumi Y, Yasunaga H. Outcomes after helicopter versus ground emergency medical services for major trauma--propensity score and instrumental variable analyses: a retrospective nationwide cohort study. Scand J Trauma Resusc Emerg Med. 2016;24(1):140. doi: 10.1186/s13049-016-0335-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Borst GM, Davies SW, Waibel BH, Leonard KL, Rinehart SM, Newell MA, et al. When birds can’t fly: an analysis of interfacility ground transport using advanced life support when helicopter emergency medical service is unavailable. The journal of trauma and acute care surgery. 2014;77(2):331–6. doi: 10.1097/TA.0000000000000295. discussion 6–7. [DOI] [PubMed] [Google Scholar]
- 28.Bulger EM, Guffey D, Guyette FX, MacDonald RD, Brasel K, Kerby JD, et al. Impact of prehospital mode of transport after severe injury: a multicenter evaluation from the Resuscitation Outcomes Consortium. The journal of trauma and acute care surgery. 2012;72(3):567–73. doi: 10.1097/TA.0b013e31824baddf. discussion 73–5; quiz 803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roislien J, Lossius HM, Kristiansen T. Does transport time help explain the high trauma mortality rates in rural areas? New and traditional predictors assessed by new and traditional statistical methods. Inj Prev. 2015 doi: 10.1136/injuryprev-2014-041473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Medicine Io. Best care at lower cost: The path to continuously learning health care in America. Washington, DC: 2013. [PubMed] [Google Scholar]
- 31.Pannu J, Sanghavi D, Sheley T, Schroeder DR, Kashyap R, Marquez A, et al. Impact of Telemedicine Monitoring of Community ICUs on Interhospital Transfers. Crit Care Med. 2017;45(8):1344–51. doi: 10.1097/CCM.0000000000002487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tyler PD, Celi LA. Tele-ICU Increases Interhospital Transfers: Does Big Brother Know Better? Crit Care Med. 2017;45(8):1417–9. doi: 10.1097/CCM.0000000000002510. [DOI] [PubMed] [Google Scholar]