Abstract
Objectives
The Korea International Cooperation Agency (KOICA) established 4 health centers to provide hypertension screening and a health support program in a deprived urban area of Lima, Peru. This case report provides a mid-term evaluation of the KOICA’s hypertension prevention and control programs.
Methods
A follow up study was performed on 663 residents who were diagnosed with prehypertension or hypertension (Stage 1 and 2) in the 4 KOICA health centers. Patients participated in programs designed to prevent and control hypertension through education sessions over the course of 6 months. Using simple descriptive statistics and computer simulations, we evaluated the effect of hypertension prevention and control programs on the participants.
Results
The KOICA health programs appeared to significantly contribute to lowering the blood pressure (BP) of the participants. The total number of participants with normal BP increased from none to 109. Overall, the female and younger patients responded better to the KOICA programs than the male and older participants. In addition, the average systolic BP, diastolic BP, and body mass index of all participants was significantly reduced.
Conclusion
The KOICA programs were effective at lowering blood pressure, particularly amongst the prehypertension group than the Stage 1 and 2 hypertension groups. This suggests that providing an extensive screening service for adults with prehypertension will help control hypertension in the early stages.
Keywords: hypertension, Peru, prehypertension, screening, KOICA
Introduction
In 2014, hypertension was amongst the most common causes of death in Peru for those aged 65 years and older. Hypertension is a major risk factor for non-communicable diseases, such as cardiovascular disease, which is the second most common cause of death for the elderly in Peru [1]. Hypertension is essentially an outcome of the epidemiological transition in Peru where health profiles are undergoing major changes [2]. Sedentary work and increased consumption of salt, saturated fats, and refined carbohydrates have resulted in higher rates of obesity, diabetes, elevated lipids, and hypertension [3]. Hypertension is also associated with inadequate fruit and vegetable consumption, lower education levels, cigarette smoking, and psychological stress [4]. The prevalence of hypertension was 14.8% amongst Peruvian adults over 15 years old in 2014, according to the National Institute of Statistics and Computing [5]. Some researchers estimated the prevalence of hypertension to be around 16%–17% for men and 15%–23% for women in selected areas [6]. It tends to rise steeply as people, particularly women, grow older. Approximately 50% of Peruvian adults with hypertension are unaware of their condition, and most of them neither control their condition nor receive treatments [6].
The awareness, control, and treatment of hypertension was particularly low amongst adults in the deprived urban area of Peru. The rapid growth in population and urbanization in the outskirts of urban Latin America resulted in the encroachment of public spaces, such as parks, playing fields, and walking paths; this decreased opportunity for residents to engage in physical activities or sports, as workers increasingly depend on public transport, including buses and trains, for their commutes [3]. The most common health issues in urban areas of Peru are being overweight, obesity, hypertension, smoking, drinking, depression, low levels of physical activity, and unhealthy eating habits [7, 8]. Therefore, health initiatives have attempted to address these issues in deprived urban neighborhoods in recent years. Community activities and an increased awareness of the risk factors amongst health professionals and local residents have proven to be effective in preventing hypertension [9, 10]. Specifically, prevention, control, and treatment of hypertension in local communities have reduced the risks of heart failure, stroke, kidney disease, and myocardial infarction [11–14].
In 2014, the Peruvian Ministry of Health requested the support of the Korean government for non-communicable disease prevention and control programs through official development assistance. Thereafter, Korea International Cooperation Agency (KOICA)-Yonsei carried out health requirement assessments in Peru’s urban areas and found that high consumption of salt and fried food resulted in a high prevalence of hypertension and obesity. With the help of local partners, including district governors, health authorities, universities, the World Health Organization (WHO), and the Ministry of Health, 4 KOICA health centers in Comas and Callao districts in the western and northern suburbs of the Lima metropolitan area were established. The main objective of the KOICA health centers was to provide screening for hypertension in local adult residents, as well as education regarding the prevention, control, and treatment of hypertension. The KOICA health centers also hired and trained local health workers to increase their capacity and support health promotion in local communities.
The Peruvian Ministry of Health published a guideline for clinical practice for the diagnosis, treatment, and control of hypertensive disease in 2015. However, it is unclear whether the guideline is being observed by local health practitioners. The ministry has not been monitoring the clinical practice and there are no data that can be used to evaluate its effectiveness. Therefore, we evaluated the impacts of the KOICA-Yonsei programs on the prevalence, control, and treatment of hypertension. Our evaluation report will contribute to understanding the effectiveness of the intervention programs in Peru and serve as a useful reference for the Peruvian government and other development agencies.
Materials and Methods
A demographic report provided by the National Institute of Statistics and Informatics of Peru showed that the total population of Comas and Callao districts was about 185,605, as shown in Table 1. Most of the local residents are Hispanic or Mestizos of mixed Amerindian and European origin, and have free access to primary and secondary education. About 80% of the residents are covered by public health insurance however, large influxes of migrants from rural areas have resulted in poorer access to health care services.
Table 1.
Location of Korea International Cooperation Agency health centers and local district population.
| District* | Name of Health Center* | District Population* |
|---|---|---|
| Comas | Santa Luzmila II | 33,369 |
| Comas | Laura Rodriguez Dulanto | 34,246 |
| Callao | Bellavista | 75,163 |
| Callao | Pachacutec | 42,827 |
| Total | 185,605 |
Source: National Institute of Statistics and Informatics, Peru (2007)
A total of 11,623 adults aged 18 or older from the 4 districts were randomly selected for a blood pressure (BP) measurement. Of those adults, 1,243 were diagnosed with high BP and agreed to participate. However, this study was based on only 663 adults who completed the KOICA programs for 6 months. From April 1 to April 30 2015, BP measurements were recorded by 8 trained nurses who used a validated automatic blood pressure monitor (Omron HEM-7113) and categorized measurements into BP levels as described by the American Society of Hypertension, as shown in Table 2. Trained nurses and nutritionists at each health center then prepared for a 6-month program to follow up on participants who belonged to the prehypertension, Stage 1, and Stage 2 hypertension groups. From June 1 to December 31, 2015, the nurses and nutritionists delivered 8 sessions, which consisted of personal counseling and education regarding healthy lifestyles and prevention, as well as the control and treatment of hypertension. Each session and activity is described in Table 3. They also provided information, education, and communication materials, such as posters, pamphlets, websites, and Facebook pages about healthy lifestyles and prevention. After 6 months, the participants were expected to maintain healthy lifestyles and monitor their BP by themselves. From January 1 to March 31, 2016, the nurses measured and recorded the BP of participants who completed the program.
Table 2.
Blood pressure chart.
| Category*† | Top number (systolic) (mmHg) *† | Bottom number (diastolic) (mmHg) *† | |
|---|---|---|---|
| Normal | ≤120 | and | ≤80 |
| Prehypertension | 120–139 | or | 80–89 |
| Stage 1 hypertension | 140–159 | or | 90–99 |
| Stage 2 hypertension | 160 higher | or | ≥ 100 |
Source: the American Society of Hypertension (http://www.ash-us.org/ASH-Patient-†Portal/Get-Information/What-Is-Hypertension.aspx#HowIsBPMeasured)
Table 3.
Description of the Korea International Cooperation Agency (KOICA) - Yonsei intervention programs from June 1st to December 31st, 2015.
| Session | Activity | Description | Provider (Time) |
|---|---|---|---|
| 1 | Health Assessment |
|
Nurse (50 min) |
|
| |||
| 2 | Blood Pressure Management Training |
|
Nurse (30 min) |
|
|
|
||
| 3 |
|
Nurse (30 min) | |
|
| |||
| 4 | Physical Exercise Training |
|
Nurse & Nutritionist (30 min) |
|
|
|
||
| 5 |
|
||
|
| |||
| 6 | Nutrition Education |
|
Nutritionist (30 min) |
|
|
|
||
| 7 |
|
||
|
| |||
| 8 | Self-Care Education |
|
Nurse (30 min) |
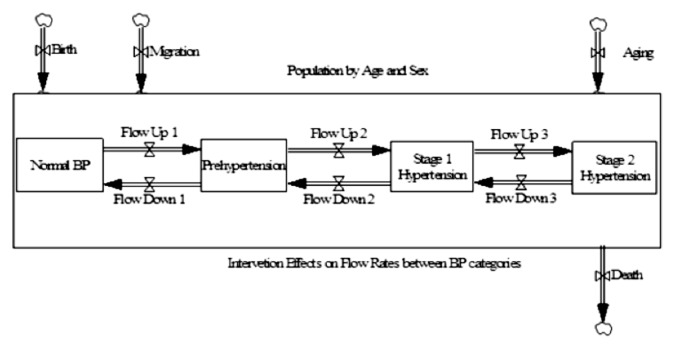
The effects of the KOICA-Yonsei programs on the people who fully participated for 1 year were then assessed by examining the change in their BP before and after the intervention programs. The effects of the KOICA-Yonsei programs on the prevalence of hypertension using a stock and flow simulation model, were shown in Figure 1.
Figure 1.
Stock and flow simulation model for population with different levels of blood pressure.
The population stock in each category changed in response to changes in flow ups and downs. The birth, death, and migration rates were assumed to be zero because the simulation period was set for a year or 365 days only. The flow rates or the rates of change were calculated based on information from the first and second blood pressure (BP) measurements.
Results
The prevalence of hypertension by age and sex before and after the KOICA-Yonsei programs, are shown in Table 4. A total of 663 adults completed the programs. Thirty-two percent were men and 68% were women, whereas 40% were aged under 60 years and 60% were aged 60 years or more. The mean and standard error for the age of all participants was 61.71 and 11.08 years, respectively. It suggests that the majority of people who have high BP and seek treatment tend to be female and elderly. The total number of male and female participants with normal BP rose from none to 109 because of the programs. The female groups showed better results in lowering blood pressure than male groups, however, there were more female participants than male participants, and the prevalence of hypertension among females was higher than that amongst males when the KOICA-Yonsei programs were initiated.
Table 4.
Hypertension prevalence by age and sex before and after the Korea International Cooperation Agency (KOICA) -Yonsei programs (n = 663).
| n | Before | % | After | % | % Change | p | ||
|---|---|---|---|---|---|---|---|---|
| Male | Normal BP | 0 | 0% | 9 | 4% | +9* | ||
| Prehypertension | 108 | 51% | 123 | 58% | 0.14 | |||
| 1st Stage Hypertension | 49 | 23% | 41 | 19% | −0.16 | |||
| 2nd Stage Hypertension | 55 | 26% | 39 | 18% | −0.29 | |||
| Total | 212 | 212 | 100% | 212 | 100% | |||
| SBP (mmHg) | 212 | 136.22 ± 21.01 | 127.97 ± 17.11 | < 0.001 | ||||
| DBP (mmHg) | 212 | 75.40 ± 12.05 | 73.175 ± 11.50 | < 0.001 | ||||
| BMI | 125 | 29.67 ± 5.20 | 29.04 ± 5.09 | < 0.001 | ||||
| Ab. Circumf. (cm) | 124 | 98.34 ± 10.39 | 97.75 ± 8.83 | < 0.100 | ||||
| Female | Normal BP | 0 | 0% | 100 | 22% | +1001 | ||
| Prehypertension | 256 | 57% | 215 | 48% | −0.16 | |||
| 1st Stage Hypertension | 101 | 22% | 109 | 24% | 0.08 | |||
| 2nd Stage Hypertension | 94 | 21% | 27 | 6% | −0.71 | |||
| Total | 451 | 451 | 100% | 451 | 100% | |||
| SBP (mmHg) | 451 | 133.72 ± 21.03 | 123.16 ± 18.05 | < 0.001 | ||||
| DBP (mmHg) | 451 | 73.33 ± 12.30 | 70.48 ± 10.62 | < 0.001 | ||||
| BMI | 302 | 29.51 ± 4.87 | 28.83 ± 4.54 | < 0.001 | ||||
| Ab. Circumf. (cm) | 303 | 96.13 ± 10.81 | 96.45 ± 10.80 | < 0.100 | ||||
| < 60 years† | Normal BP | 0 | 0% | 72 | 0% | +72* | ||
| Prehypertension | 192 | 55% | 158 | 55% | −0.18 | |||
| 1st Stage Hypertension | 13 | 23% | 17 | 23% | 0.31 | |||
| 2nd Stage Hypertension | 57 | 22% | 15 | 22% | −0.74 | |||
| Total | 262 | 262 | 100% | 262 | 100% | |||
| SBP (mmHg) | 262 | 133.30 ± 20.01 | 122.13 ± 16.52 | < 0.001 | ||||
| DBP (mmHg) | 262 | 78.01 ± 12.07 | 74.96 ± 10.72 | < 0.001 | ||||
| BMI | 180 | 29.67 ± 4.63 | 28.88 ± 4.54 | < 0.001 | ||||
| Ab. Circumf. (cm) | 180 | 97.65 ± 11.51 | 97.01 ± 10.74 | < 0.100 | ||||
| ≥ 60 years† | Normal BP | 0 | 0% | 37 | 27% | +37* | ||
| Prehypertension | 172 | 73% | 180 | 60% | 0.05 | |||
| 1st Stage Hypertension | 137 | 5% | 133 | 6% | −0.03 | |||
| 2nd Stage Hypertension | 92 | 22% | 51 | 6% | −0.45 | |||
| Total | 401 | 401 | 100% | 401 | 100% | |||
| SBP (mmHg) | 401 | 135.38 ± 21.67 | 126.43 ± 18.55 | < 0.001 | ||||
| DBP (mmHg) | 401 | 71.38 ± 11.67 | 68.97 ± 10.51 | < 0.001 | ||||
| BMI | 246 | 29.50 ± 5.39 | 28.98 ± 5.21 | < 0.001 | ||||
| Ab. Circumf. (cm) | 247 | 96.08 ± 10.08 | 96.63 ± 9.88 | < 0.100 |
Ab Cicumf = abdominal circumference; BMI = body mass index; BP = blood pressure; DBP = diastolic blood pressure; SBP = systolic blood pressure.
This number denotes a change in the absolute number of people. This is because the initial number of people with normal blood pressure in each category is zero, thus mathematically yielding an indefinite value when calculating the percentage change.
The National Institute of Statistics and Information (INEI) of Peru divides the age groups into below and over 60 years on the demographic and health survey (DHS), when measuring blood pressure. Therefore, the Korea International Cooperation Agency programs also followed the age standard after consultation with the INEI.
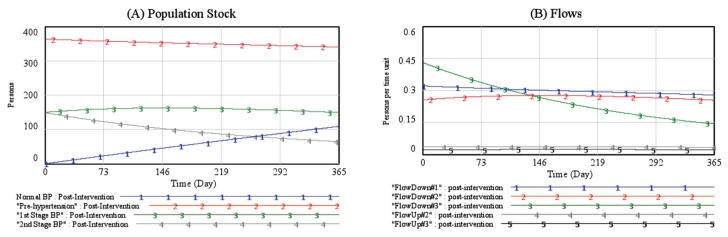
The participants who were <60 years also showed better results in lowering blood pressure than those ≥60 years. Overall, the female and younger groups performed better than the male and older groups, as can be seen from the percentage changes in Table 4. However, there was an increase in some BP categories after the KOICA-Yonsei programs. For example, the prehypertension group of men and participants aged over 60 years, and the Stage 1 hypertension group of women and participants less than 60 years increased in number. It may partially reflect the trend that BP levels tend to increase with age. However, it is mainly because a greater number of participants with Stage 1 and Stage 2 hypertension lowered their BP. In other words, Flow Downs (BP improvement) were higher than Flow Ups (BP deterioration) (Figure 2).
Figure 2.
Estimated impacts of the Korea International Cooperation Agency (KOICA) - Yonsei programs on blood pressure for all participants in the Comas and Callo districts, Lima, Peru, 2015.
Figure 2 was generated by a simulation model, which provided further insights into the dynamics of a population with hypertension in response to the KOICA programs. Figure 2(A) showed the simulation results of the sum of each BP category or population stock. The number of participants with normal BP increased from none to 109 on Day 365. Moreover, the number of participants with prehypertension and Stage 1 hypertension remained almost the same, while the number of participants with Stage 2 hypertension decreased from 149 to 66. Therefore, it appeared that the increase in the number of participants with normal BP largely stemmed from a decrease in the number of participants with Stage 2 hypertension. However, given the sample size, a steady increase in the number of participants with normal BP originated not only from a decrease in the number of participants with Stage 2 hypertension (Flow Down 3), but also from participants with Stage 1 hypertension (Flow Down 2) and prehypertension (Flow Down 1). In fact, Figure 2(B) showed that Flow Down 1 from prehypertension to normal BP was consistently higher than all other flows, although Flow Down 3 from Stage 2 hypertension to Stage 1 hypertension was initially higher and then diminished. Therefore, the KOICA programs were more effective in lowering BP amongst the prehypertension group than the 1st and 2nd Stage hypertension groups.
Discussion
The results in this study suggest that providing an extensive screening service for adults with prehypertension may be beneficial in helping control hypertension in its early stages. In other words, the earlier people start monitoring their BP and receiving treatments, the better chances they have of lowering their overall average BP. In addition, the average systolic BP, diastolic BP, and BMI of all participants were significantly reduced after the KOICA programs, as shown in Table 4.
The KOICA-Yonsei programs have contributed to significantly lowering the BP of the participants in this study. Overall, the female and younger groups performed better than the male and older groups. The programs were found to be more effective in lowering BP amongst the prehypertension group than the 1st and 2nd Stage hypertension groups. It suggests that the Peruvian government can effectively reduce the prevalence of hypertension in urban areas by providing a screening service and health education programs to inform the population on the importance of a healthy lifestyle, particularly for young adults. The average systolic BP, diastolic BP, and BMI of all participants also reduced significantly.
This success can be attributed to the active involvement of several local partners during the planning, implementation, monitoring, and evaluation phases. Representatives from both Korean and Peruvian agencies actively participated as members of the program committees. The WHO Country Office in Peru provided technical assistance on the overall program contents, survey method, and capacity building program for health professionals. The local health department provided office spaces for the program manager and staff members, and guidance for local participants on how to register with the KOICA programs. We also worked with a local university, Cayetano Heredia University, which runs the capacity building programs in collaboration with KOICA. The project activities were shown to be worthwhile and successful because of the close collaboration amongst all stakeholders.
Acknowledgements
This work was supported by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea (NRF-2016S1A5B8925203). This work was supported by Korea International Cooperation Agency (KOICA) under the title of “Health Promotion Program in North of Lima and Callao, Peru” in 2013 (No. P2013-00151-1).
Footnotes
Conflicts of Interest
There are no conflicts of interest related to the work.
References
- 1.Davies AR, Miranda JJ, Gilman RH, Smeeth L. Hypertension among adults in a deprived urban area of Peru - undiagnosed and uncontrolled? BMC Res Notes. 2008;1(2):1–7. doi: 10.1186/1756-0500-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abegunde DO, Mathers CD, Adam T, Ortegon M, Strong K. Chronic diseases 1 - The burden and costs of chronic diseases in low-income and middle-income countries. Lancet. 2007;370(9603):1929–38. doi: 10.1016/S0140-6736(07)61696-1. [DOI] [PubMed] [Google Scholar]
- 3.Yusuf S, Vaz M, Pais P. Tackling the challenge of cardiovascular disease burden in developing countries. Am Heart J. 2004;148(1):1–4. doi: 10.1016/j.ahj.2004.03.045. [DOI] [PubMed] [Google Scholar]
- 4.Dickson BK, Blackledge J, Hajjar IM. The impact of lifestyle behavior on hypertension awareness, treatment, and control in a southeastern population. Am J Med Sci. 2006;332(4):211–5. doi: 10.1097/00000441-200610000-00010. [DOI] [PubMed] [Google Scholar]
- 5.National Institute of Statistic and Computing. PERU: Non-Communicable and Communicable Diseases. [cited 2015 Sep 17]. Available from: http://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Lib1212/Libro.pdf (Spanish).
- 6.Medina-Lezama J, Zea-Diaz H, Morey-Vargas OL, et al. Prevalence and patterns of hypertension in Peruvian Andean Hispanics: the PREVENCION study. Am J Hypertens. 2007;1(3):216–25. doi: 10.1016/j.jash.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 7.Nam EW, Sharma B, Kim HY, et al. Obesity and Hypertension among School-going Adolescents in Peru. J Lifestyle Med. 2015;(2):60–7. doi: 10.15280/jlm.2015.5.2.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sharma B, Nam EW, Kim D, Yoon YM, Kim Y, Kim HY. Role of gender, family, lifestyle and psychological factors in self-rated health among urban adolescents in Peru: a school-based cross-sectional survey. BMJ Open. 2016;6(2):1–8. doi: 10.1136/bmjopen-2015-010149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Campbell NRC, Burgess E, Taylor G, et al. Lifestyle changes to prevent and control hypertension: Do they work? A summary of the Canadian Consensus Conference. Can Med Assoc J. 1999;160(9):1341–3. [PMC free article] [PubMed] [Google Scholar]
- 10.Hypertension control. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1996;862:1–83. [PubMed] [Google Scholar]
- 11.Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJL, Coll CRA. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360(9343):1347–60. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 12.Toto RD. Treatment of hypertension in chronic kidney disease. Semin Nephrol. 2005;25(6):435–9. doi: 10.1016/j.semnephrol.2005.05.016. [DOI] [PubMed] [Google Scholar]
- 13.Yusuf S, Thom T, Abbott RD. Changes in hypertension treatment and in congestive heart failure mortality in the United States. Hypertension. 1989;13(5 Suppl):174–9. doi: 10.1161/01.HYP.13.5_Suppl.I74. [DOI] [PubMed] [Google Scholar]
- 14.Moser M, Hebert PR. Prevention of disease progression, left ventricular hypertrophy and congestive heart failure in hypertension treatment trials. J Am Coll Cardiol. 1996;27(5):1214–8. doi: 10.1016/0735-1097(95)00606-0. [DOI] [PubMed] [Google Scholar]