Abstract
This analysis uses SEER Medicaid data to quantify changes in health insurance coverage under the Affordable Care Act among nonelderly patients newly diagnosed with cancer.
The Affordable Care Act (ACA) has reduced the number of uninsured persons in the United States to a historic low. Debate continues about potential changes to the law that could affect coverage for millions, particularly those with preexisting conditions. Meanwhile, cancer is the leading cause of death among Americans aged 19 to 64 years. Treatment is often unaffordable for uninsured patients, and some studies suggest that expanding insurance coverage could improve cancer-related outcomes. Our objective was to quantify changes in health insurance coverage under the ACA among patients newly diagnosed with cancer.
Methods
Data came from the National Cancer Institute’s Surveillance, Epidemiology, and End Results program, 2010 through 2014. The program is a coordinated registry of all patients with cancer in participating areas in the United States, covering 28% of the population and representative of national demographics. Our sample included adults aged 19 to 64 years with a first-time cancer diagnosis. Indiana University’s institutional review board deemed this study to be nonhuman subjects research that did not require their approval or patient informed consent.
The outcome was the percentage of adults uninsured at diagnosis. We analyzed unadjusted changes in 2014, when the ACA health insurance exchanges and Medicaid expansion went into effect, compared with pre-ACA years 2010-2013. We repeated this analysis stratifying by (1) tumor location for the 5 most common types of nonskin cancer, (2) cancer stage, (3) race/ethnicity, and (4) county poverty rate. We used difference-in-differences regression to assess whether changes in coverage were greater in states with Medicaid expansion than in nonexpansion states, with robust SEs clustered at the state level and adjusting for patient and county characteristics. All analysis was conducted using Stata software, version 14 (StataCorp). P values are 2-sided, and P < .05 indicates statistical significance.
Results
Data were obtained from the SEER Program for 858 193 nonelderly adults with new cancer diagnoses. Of these, 468 131 (54.55%) were women, and the mean (SD) age was 52.44 (9.66) years. The Table shows unadjusted changes in the uninsured rate. Before 2014, 5.73% of these persons were uninsured vs 3.81% in 2014, a 1.92 percentage point decrease (95% CI, −2.02 to −1.81; P < .001) or 33.51% relative decline. Significant declines were present across all stages and sites we assessed. The largest absolute declines were for distant disease (−3.03 percentage points [95% CI, −3.32 to −2.74]) and lung and bronchial cancer (−2.95 percentage points [95% CI, −3.44 to −2.46]), but these represented relative declines similar to those in the full sample (−33.26% for distant disease, −32.67% for lung and bronchial cancer, and −33.51% for the full sample). By demographic features, changes in uninsurance were greatest for persons of Hispanic ethnicity and other race (relative changes of −39.87% for Hispanic and −46.19% for individuals of other race) and residents of wealthier counties (relative change of −36.12% for residents of counties that had an above-median poverty rate).
Table. Changes in Percentage of Patients Without Health Insurance at Cancer Diagnosis, 2010-2014a.
| Characteristic | Sample Size | Unadjusted Percentage of Patients Without Health Insurance | |||
|---|---|---|---|---|---|
| Pre-ACA, % (95% CI)b | Post-ACA, % (95% CI)c | Absolute Difference (95% CI)d | Relative Change, % | ||
| Full sample | 858 193 | 5.73 (5.67 to 5.78) | 3.81 (3.72 to 3.91) | –1.92 (–2.02 to –1.81) | –33.51 |
| Stage at diagnosis | |||||
| In situ | 79 392 | 3.01 (2.87 to 3.14) | 2.30 (2.07 to 2.53) | –0.70 (–0.97 to –0.44) | –23.26 |
| Local | 382 560 | 4.25 (4.18 to 4.32) | 2.80 (2.69 to 2.92) | –1.45 (–1.58 to –1.31)e | –34.13 |
| Regional | 193 756 | 6.03 (5.91 to 6.15) | 3.93 (3.74 to 4.12) | –2.10 (–2.33 to –1.87)e | –34.83 |
| Distant | 178 669 | 9.11 (8.96 to 9.26) | 6.08 (5.84 to 6.33) | –3.03 (–3.32 to –2.74)e | –33.26 |
| Cancer site | |||||
| Breast | 188 941 | 2.90 (2.82 to 2.99) | 2.15 (2.00 to 2.29) | –0.75 (–0.92 to –0.59) | –25.86 |
| Prostate | 95 729 | 3.24 (3.12 to 3.37) | 2.29 (2.06 to 2.53) | –0.95 (–1.21 to –0.69) | –29.32 |
| Colorectal | 68 216 | 7.85 (7.62 to 8.08) | 5.20 (4.84 to 5.56) | –2.65 (–3.08 to –2.22)f | –33.75 |
| Lung and bronchial | 63 767 | 9.03 (8.78 to 9.28) | 6.08 (5.66 to 6.50) | –2.95 (–3.44 to –2.46)f | –32.67 |
| Thyroid | 44 027 | 3.82 (3.62 to 4.03) | 2.56 (2.24 to 2.88) | –1.26 (–1.64 to –0.88) | –32.98 |
| Race/ethnicityg | |||||
| White | 560 229 | 4.57 (4.51 to 4.63) | 2.91 (2.81 to 3.00) | –1.67 (–1.78 to –1.55) | –36.54 |
| Black | 108 082 | 8.66 (8.47 to 8.84) | 7.12 (6.77 to 7.46) | –1.54 (–1.93 to –1.15) | –17.78 |
| Hispanic | 111 288 | 9.58 (9.38 to 9.77) | 5.75 (5.46 to 6.05) | –3.82 (–4.18 to –3.47)h | –39.87 |
| Other | 69 743 | 4.59 (4.42 to 4.77) | 2.47 (2.22 to 2.73) | –2.12 (–2.42 to –1.81)h | –46.19 |
| County poverty ratei | |||||
| Below-median poverty rate | 612 209 | 5.04 (4.98 to 5.10) | 3.37 (3.27 to 3.48) | –1.66 (–1.78 to –1.54) | –32.94 |
| Above-median poverty rate | 244 887 | 7.53 (7.41 to 7.65) | 4.81 (4.63 to 4.99) | –2.72 (–2.94 to –2.51)j | –36.12 |
Abbreviations: ACA, Affordable Care Act; SEER, Surveillance, Epidemiology, and End Results program.
Calculations are based on SEER data from 2010 to 2014. Sample is restricted to first-time cancer diagnoses for adults aged 19 to 64 years. Diagnoses with unknown or missing insurance status, which represented 7% of the sample, are omitted. Sample sizes refer to the number of diagnoses over the 5-year period from 2010 to 2014. Stage of diagnosis is based on SEER’s summary stage variable.
Pre-ACA refers to 2010 through 2013.
Post-ACA refers to 2014.
All absolute differences represented a significant change in the percentage of uninsured patients with newly diagnosed cancer from the pre-ACA period to the post-ACA period at P < .001.
Estimate is significantly different from in situ cancer at P < .05.
Estimate is significantly different from breast cancer at P < .05.
SEER cancer registries abstract race and ethnicity information from medical records and use a standardized method to group these into the basic categories. The data set documentation notes that the initial collection of race/ethnicity information and procedures for identifying and verifying race/ethnicity may differ across health care facilities and practitioners.
Estimate is significantly different from white race at P < .05.
The cutoff for the median county poverty rate was 18.7%.
Estimate is significantly different from below median poverty rate at P < .05.
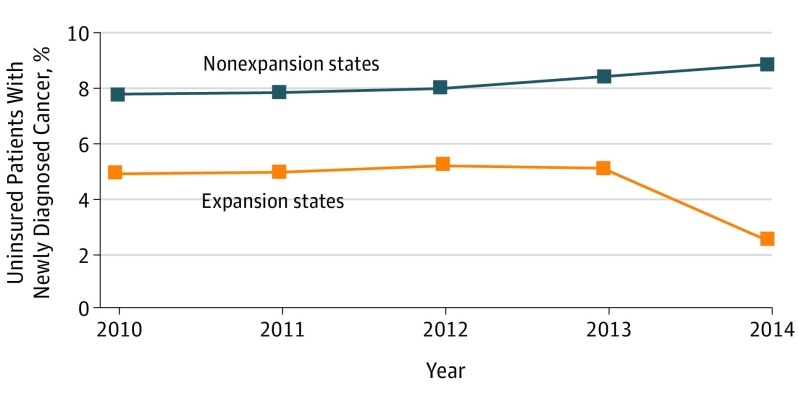
The Figure shows changes based on Medicaid expansion status. The uninsured rate was flat in states without expansion before and after 2014, but it declined sharply in 2014 in expansion states. The Medicaid expansion difference-in-differences estimate was −2.4 percentage points (95% CI, −4.0 to −0.8; P = .007).
Figure. Changes in Percentage of Uninsured Patients With Newly Diagnosed Cancer Based on State Medicaid Expansion Status, 2010-2014.
Calculations are based on Surveillance, Epidemiology, and End Results data from 2010 to 2014. The sample is restricted to first-time cancer diagnoses for adults aged 19 to 64 years. The 2014 expansion states in the SEER database are California, Connecticut, Hawaii, Iowa, Kentucky, Michigan, New Mexico, New Jersey, and Washington. The nonexpansion states are Alaska, Georgia, Louisiana, and Utah. The difference-in-differences estimate for Medicaid expansion was −2.38 (95% CI, −3.97 to −0.79; P = .007). Standard errors were clustered at the state level. The model adjusted for patient’s age, marital status, sex, race/ethnicity, state of residence, year of diagnosis, county unemployment rate, and county median income. Trends in coverage did not differ significantly based on expansion status before 2014 (β = −0.15, 95% CI, −0.42 to 0.13; P = .26).
Discussion
Uninsurance among patients with newly diagnosed cancer fell by one-third in the ACA’s first year. Coverage gains were significant across numerous common cancers, multiple demographic groups, and early-stage and late-stage disease. Large gains among Hispanic individuals were consistent with findings of other ACA studies and may indicate narrowing disparities. Medicaid expansion states experienced significantly greater gains in coverage. These findings suggest that the general increase in coverage seen in national ACA analyses extends to this high-risk population.
Limitations of our analysis include the availability of data from 13 states and 1 year of post-ACA data. Our results are descriptive, and our quasi-experimental Medicaid analysis is subject to potential time-varying confounders. Furthermore, other research indicates that uninsured patients are less likely to be diagnosed with cancer and more likely to be diagnosed at late stages. Our finding that uninsurance was greater among those with distant disease in the pre-ACA and post-ACA periods is in line with research suggesting that uninsured patients may not seek care until their cancer has progressed. Although we provide novel evidence that fewer patients newly diagnosed with cancer were uninsured in the post-ACA period, our analysis did not separate the effects of gains in coverage among patients who would have been diagnosed in the absence of the ACA from changes in the number of diagnoses resulting from increased coverage. Future research should examine effects of coverage on cancer diagnoses, treatment, and outcomes. Policy changes that reduce Medicaid funding or weaken protections for individuals with preexisting conditions could be particularly harmful for patients with cancer.
References
- 1.Centers for Disease Control and Prevention 10 Leading causes of death by age group, United States—2015. https://www.cdc.gov/injury/images/lc-charts/leading_causes_of_death_age_group_2015_1050w740h.gif. Accessed August 22, 2017.
- 2.Dusetzina SB, Basch E, Keating NL. For uninsured cancer patients, outpatient charges can be costly, putting treatments out of reach. Health Aff (Millwood). 2015;34(4):584-591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sommers BD, Gawande AA, Baicker K. Health insurance coverage and health—what the recent evidence tells us. N Engl J Med. 2017;377(6):586-593. [DOI] [PubMed] [Google Scholar]
- 4.SEER Research Data 1973-2014. National Cancer Institute, DCCPS, Surveillance Research Program, Surveillance Systems Branch; 2017. https://www.seer.cancer.gov. Accessed August 22, 2017.
- 5.Centers for Disease Control and Prevention. Interpreting race and ethnicity in cancer data. https://www.cdc.gov/cancer/npcr/uscs/technical_notes/interpreting/race.htm#2. Accessed September 7, 2017.
- 6.Sommers BD, Gunja MZ, Finegold K, Musco T. Changes in self-reported insurance coverage, access to care, and health under the Affordable Care Act. JAMA. 2015;314(4):366-374. [DOI] [PubMed] [Google Scholar]
- 7.Simon K, Soni A, Cawley J. The impact of health insurance on preventive care and health behaviors: evidence from the first two years of the ACA Medicaid expansions. J Policy Anal Manage. 2017;36(2):390-417. [DOI] [PubMed] [Google Scholar]