Abstract
Objective
Determination of clinical outcomes following resuscitation from cardiac arrest remains elusive in the immediate post-arrest period. Echocardiographic assessment shortly after resuscitation has largely focused on left ventricular (LV) function. We aimed to determine whether post-arrest right ventricular (RV) dysfunction predicts worse survival and poor neurologic outcome in cardiac arrest patients, independent of LV dysfunction.
Methods
A single-center, retrospective cohort study at a tertiary care university hospital participating in the Penn Alliance for Therapeutic Hypothermia (PATH) Registry between 2000 and 2012.
Patients
291 in- and out-of-hospital adult cardiac arrest patients at the University of Pennsylvania who had return of spontaneous circulation (ROSC) and post-arrest echocardiograms.
Measurements and main results
Of the 291 patients, 57% were male, with a mean age of 59 ± 16 years. 179 (63%) patients had LV dysfunction, 173 (59%) had RV dysfunction, and 124 (44%) had biventricular dysfunction on the initial post-arrest echocardiogram. Independent of LV function, RV dysfunction was predictive of worse survival (mild or moderate: OR 0.51, CI 0.26–0.99, p < 0.05; severe: OR 0.19, CI 0.06–0.65, p = 0.008) and neurologic outcome (mild or moderate: OR 0.33, CI 0.17–0.65, p = 0.001; severe: OR 0.11, CI 0.02–0.50, p = 0.005) compared to patients with normal RV function after cardiac arrest.
Conclusions
Echocardiographic findings of post-arrest RV dysfunction were equally prevalent as LV dysfunction. RV dysfunction was significantly predictive of worse outcomes in post-arrest patients after accounting for LV dysfunction. Post-arrest RV dysfunction may be useful for risk stratification and management in this high-mortality population.
Keywords: Cardiac arrest, Myocardial dysfunction, Echocardiography, Right ventricle, Survival, Neurologic outcome
Introduction
Cardiac arrest carries a substantial morbidity and mortality burden in the United States (US).1–3 The American Heart Association (AHA) reports a combined out-of-hospital (OHCA) and in-hospital cardiac arrest (IHCA) incidence of 568,400 events per year, with survival rates of only 9.5% and 23.9%, respectively.4 Clinical opportunities to improve post-arrest outcomes include targeted therapies to achieve temperature management, hemodynamic stability and multi-organ support. Despite advances in these areas, there remains a critical need to rapidly identify patients at risk of early deterioration so that management strategies may be implemented more aggressively in this population.5–7 A potential method of risk stratification includes the incorporation of early echocardiographic findings into the care management protocols for post-arrest patients.
To date, there has been significant focus on left ventricular function in the immediate post-arrest setting as a prognostic indicator.8–12 Recently, however, a growing emphasis on right ventricular function in a spectrum of stress states has emerged as a result of a more in-depth understanding of the right ventricle (RV) and its response to hemodynamic disturbance.13–16 The RV demonstrates distinct cellular, morphological, and metabolic characteristics compared to the left ventricle (LV), which may play a crucial role in the handling of cardiac arrest. On this basis, we hypothesized that patients with post-arrest RV dysfunction would have worse neurological outcomes and lower survival than patients without post-arrest RV dysfunction.
Materials and methods
The Penn Alliance for Therapeutic Hypothermia (PATH) database is a multicenter registry of cardiac arrest patients, which includes in- and out-of-hospital cardiac arrests of all rhythms. This was a retrospective cohort study from the PATH registry of successfully resuscitated cardiac arrest patients between May 2000 and July 2012. Between 2000 and 2012, 932 cardiac arrest patients from the University of Pennsylvania Hospital system were recorded in the PATH registry, 436 patients (47%) of whom had return of spontaneous circulation (ROSC). An echocardiogram was completed in 301 (69%) of the patients who had ROSC. We analyzed echocardiograms from 291 (97%) of these patients as the remaining 10 patients (3%) were excluded due to inadequate echocardiographic windows or incomplete information in the PATH registry. This study was approved by the Institutional Review Board of the University of Pennsylvania (approval # 817655). Demographic, baseline, pre-arrest, and peri-arrest information was available in PATH, as previously described.17
Finalized clinical echocardiogram reports were separately abstracted in a blinded fashion for all subjects in the registry. The index transthoracic echocardiogram (TTE) was defined as the first echocardiogram performed post-arrest. No cutoff for time to index TTE was applied in our analysis. LV systolic dysfunction was defined as an LV ejection fraction (LVEF) ≤ 50%. RV size was subjectively characterized as normal, mildly dilated, moderately dilated or severely dilated by a level III board-certified echocardiographer. Similarly, RV systolic function was subjectively characterized as normal, mildly depressed, moderated depressed, or severely depressed by a level III board-certified echocardiographer. RV size was assigned a categorical grade based on the echocardiographer interpretation, with a score of 0 (normal), 1 (mildly dilated), 2 (moderately dilated), or 3 (severely dilated). RV systolic function was also categorically graded with a score of 0 (normal), 1 (mildly depressed), 2 (moderately depressed), or 3 (severely depressed). A composite RV dysfunction score (RVDS) was calculated by combining these RV size and RV systolic function scores to generate the RVDS (0–6). Patients were then numerically stratified into three final RV dysfunction groups based on the composite RVDS: Group I for normal RV function (RVDS = 0); Group II for mild or moderate RV dysfunction (RVDS = 1–4); and Group III for severe RV dysfunction (RVDS = 5–6). Neurologic outcomes were based on cerebral performance category (CPC) scores at hospital discharge. A good neurologic outcome corresponded to a CPC score of 1 or 2, and a poor neurologic outcome corresponded to a CPC score of 3–5.
Statistical analysis
We analyzed several demographic and arrest variables in the PATH database (Table 1). Using Student’s t-tests and Wilcoxon rank-sum on continuous variables, and chi-square tests on categorical variables, we assessed the relationship between each factor and RV function. Univariate analyses were completed to characterize the association between predictor variables and neurologic, as well as survival outcomes. Importantly, the inclusion of several variables increases the risk of incorrectly identifying predictive variables. As such, multivariate logistic regression was completed to assess for the association between RV dysfunction and outcomes, while accounting for all significant variables defined in the univariate analyses using step-wise backward elimination. These variables were LV dysfunction, targeted temperature management (TTM), dose of epinephrine, duration of arrest and initial rhythm. For this study, statistical significance was defined as a p value of <0.05.
Table 1.
Baseline demographics.
| All N = 291 (%) |
RV dysfunctiona N = 173 (59%) (Groups II and III) |
No RV dysfunctiona N = 118 (41%) (Group I) |
p value | |
|---|---|---|---|---|
| Demographic factors | ||||
| Age (mean ± SD) | 59 ± 16 | 59 ± 16 | 58 ± 17 | 0.78 |
| Male | 166 (57) | 101 (59) | 65 (55) | 0.50 |
| Lung disease | 62 (21) | 26 (22) | 36 (21) | 0.82 |
| Hypertension | 153 (53) | 85 (49) | 68 (58) | 0.17 |
| Diabetes | 98 (34) | 63 (37) | 35 (30) | 0.22 |
| Prior stroke | 22 (8) | 13 (8) | 9 (8) | 0.98 |
| Arrhythmia | 47 (16) | 33 (19) | 14 (12) | 0.10 |
| CAD | 72 (25) | 46 (27) | 26 (22) | 0.36 |
| Prior MI | 39 (13) | 21 (12) | 18 (15) | 0.46 |
| CHF | 63 (22) | 43 (25) | 20 (17) | 0.10 |
| Arrest factors | ||||
| OHCA | 200 (70) | 116 (67) | 84 (71) | 0.50 |
| IHCA | 87 (30) | 56 (33) | 31 (27) | |
| Witnessed | 226 (82) | 133 (80) | 93 (84) | 0.44 |
| TTM | 171 (59) | 109 (63) | 62 (53) | 0.07 |
| LV systolic dysfunction | 179 (63) | 124 (75) | 55 (47) | <0.001 |
| Biventricular dysfunction | 124 (44) | 124 (75) | 0 (0) | <0.001 |
| Duration of arrest, min (medians) | 20 (10, 35) | 21 (12, 38) | 19 (9, 30) | 0.03 |
| Epi given | 222 (79) | 140 (85) | 82 (71) | 0.01 |
| Epi dose, mg (medians) | 3 (2, 4) | 3 (2, 4) | 2 (1, 4) | 0.005 |
| Cardiac etiology | 166 (77) | 100 (79) | 66 (74) | 0.37 |
| Rhythm factors | ||||
| VT/VF | 99 (37) | 52 (32) | 47 (44) | 0.053 |
| Asystole | 59 (22) | 40 (25) | 19 (18) | 0.17 |
| PEA | 110 (41) | 69 (43) | 41 (38) | 0.46 |
SD, standard deviation; CAD, coronary artery disease; MI, myocardial infarction; CHF, congestive heart failure; IHCA, in-hospital cardiac arrest; OHCA, out-of-hospital cardiac arrest; TTM, targeted temperature management; VT, ventricular tachycardia; VF, ventricular fibrillation; PEA, pulseless electrical activity.
Group I: RVDS score 0; Group II: RVDS score 1–4; Group III: RVDS score 5–6.
Results
Of the 291 patients, 57% were male, with a mean age of 59 ± 16 years. The patient cohort had several cardiopulmonary risk factors (Table 1). The overall median time from cardiac arrest to the index echocardiogram was 574 min (interquartile range (IQR) 258, 1257). There was no significant difference in median time to echocardiogram between the three RV groups (Group I vs. Group II, p = 0.12; Group I vs. Group III, p = 0.20; Group II vs. Group III, p = 0.79; p values reflect comparison of means), or between RV dysfunction patients and LV dysfunction patients (p = 0.438). Time to index echocardiogram was not significantly associated with survival or neurologic outcomes in the overall cohort, or in the different RV dysfunction groups. The median time from cardiac arrest to index echocardiogram stratified by RV dysfunction group was: 624 min for Group I (IQR 315, 1390), 528 min for Group II (IQR 204, 1238), and 587.5 for Group III (IQR 234, 1048). The median time from cardiac arrest to index echocardiogram for patients with LV dysfunction was 600 min (IQR 262, 1163). There was no significant difference in median time to echocardiogram between the three RV groups (p = NS), or between RV dysfunction patients and LV dysfunction patients (p = 0.438). The duration of TTM and rewarming was comparable between all three groups (Group I vs. Group II, p = 0.34; Group I vs. Group III, p = 0.68; Group II vs. Group III, p = 0.89; p values reflect comparison of means).
179 (63%) patients had LV dysfunction (55 of whom had isolated LV dysfunction), 173 (59%) patients had RV dysfunction (49 of whom had isolated RV dysfunction), and 124 (44%) patients had biventricular dysfunction on the index echocardiogram. Factors associated with survival and good neurologic outcome (CPC 1 or 2) in the univariate logistic regression included witnessed arrest and shockable rhythm (Table 2). Among patients with RV dysfunction, a number of factors were associated with outcomes, including pulseless time, dose of epinephrine, and female gender (Table 3).
Table 2.
Factors associated with cardiac arrest outcomes at hospital discharge.
| Survival Odds ratio (CI) (n = 138) |
p value | CPC 1–2 Odds ratio (CI) (n = 56) |
p value | |
|---|---|---|---|---|
| Demographic factors | ||||
| Age (mean ± SD) | 1.00 (0.99–1.01) | 0.859 | 1.00 (0.98–1.01) | 0.782 |
| Male | 1.54 (0.96–2.45) | 0.071 | 1.84 (1.14–2.97) | 0.013 |
| Lung disease | 0.74 (0.43–1.30) | 0.296 | 0.82 (0.47–1.44) | 0.492 |
| Hypertension | 0.90 (0.57–1.42) | 0.636 | 1.10 (0.69–1.74) | 0.701 |
| Diabetes | 0.64 (0.39–1.04) | 0.071 | 0.64 (0.39–1.05) | 0.075 |
| Prior stroke | 2.24 (0.89–5.67) | 0.089 | 2.58 (1.05–6.35) | 0.04 |
| Arrhythmia | 0.66 (0.35–1.23) | 0.191 | 0.79 (0.42–1.50) | 0.474 |
| CAD | 0.88 (0.52–1.49) | 0.637 | 0.94 (0.55–1.61) | 0.829 |
| Prior MI | 1.32 (0.67–2.61) | 0.417 | 1.94 (0.98–3.83) | 0.056 |
| CHF | 0.87 (0.50–1.52) | 0.626 | 0.81 (0.46–1.43) | 0.46 |
| Arrest factors | ||||
| OHCA | 1.50 (0.91–2.47) | 0.111 | 1.22 (0.73–2.02) | 0.449 |
| Witnessed | 2.15 (1.22–3.76) | 0.008 | 2.58 (1.42–4.71) | 0.002 |
| Cardiac etiology | 1.50 (0.89–2.52) | 0.129 | 1.70 (0.99–2.93) | 0.053 |
| Rhythm factors | ||||
| VT/VF | 2.72 (1.65–4.48) | <0.001 | 3.36 (2.03–5.55) | <0.001 |
| Asystole | 0.61 (0.35–1.08) | 0.091 | 0.42 (0.23–0.79) | 0.006 |
| PEA | 0.54 (0.33–0.88) | 0.013 | 0.54 (0.33–0.89) | 0.016 |
SD, standard deviation; CI, confidence interval; CPC, cerebral performance category; CAD, coronary artery disease; MI, myocardial infarction; CHF, congestive heart failure; OHCA, out-of-hospital cardiac arrest; VT, ventricular tachycardia; VF, ventricular fibrillation; PEA, pulseless electrical activity.
Table 3.
Factors associated with outcome in RV dysfunction patients on univariate analysis.
| Group | Survival | Neurologic outcome | ||
|---|---|---|---|---|
|
|
|
|||
| OR [95% CI] | p value | OR [95% CI] | p value | |
| Pulseless time | 0.98 [0.97–1.0] | 0.033 | 0.98 [0.96–1.0] | 0.049 |
| Epinephrine dose | 0.69 [0.54–0.87] | <0.001 | 0.75 [0.60–0.7] | 0.027 |
| Female | 0.60 [0.32–1.13] | 0.113 | 0.40 [0.19–0.83] | 0.013 |
| TH | 1.32 [0.70–2.53] | 0.389 | 0.98 [0.49–1.96] | 0.964 |
| LV systolic dysfunction | 1.36 [0.66–2.81] | 0.403 | 1.50 [0.67–3.37] | 0.321 |
Shown are the odds ratios (OR), confidence intervals (CI) and p values for each factor stratified by outcome.
A similar percentage of patients survived to discharge in the low LVEF and the normal LVEF groups (51% vs. 52%, p = 0.91). A similar percentage of patients had a favorable neurologic outcome (CPC 1 or 2) at discharge in the low LVEF and the normal LVEF groups (43% vs. 42%, p = 0.88).
In the multivariate logistic regression, independent of LV function, RV dysfunction was predictive of worse neurologic outcome (Group II/RVDS 1–4: OR 0.33, CI 0.17–0.65, p = 0.001; Group III/RVDS 5–6: OR 0.11, CI 0.02–0.50, p = 0.005) compared to patients with normal RV function (Group I/RVDS 0). Independent of LV function, RV dysfunction was predictive of worse survival (Group II/RVDS 1–4: OR 0.51, CI 0.26–0.99, p < 0.05; Group III/RVDS 5–6: OR 0.19, CI 0.06–0.65, p = 0.008) compared to patients with normal RV function (Group I/RVDS 0) (Fig. 1). There was a consistent graded relationship between degree of RV dysfunction, death and poor neurologic outcome (Fig. 1).
Fig. 1.
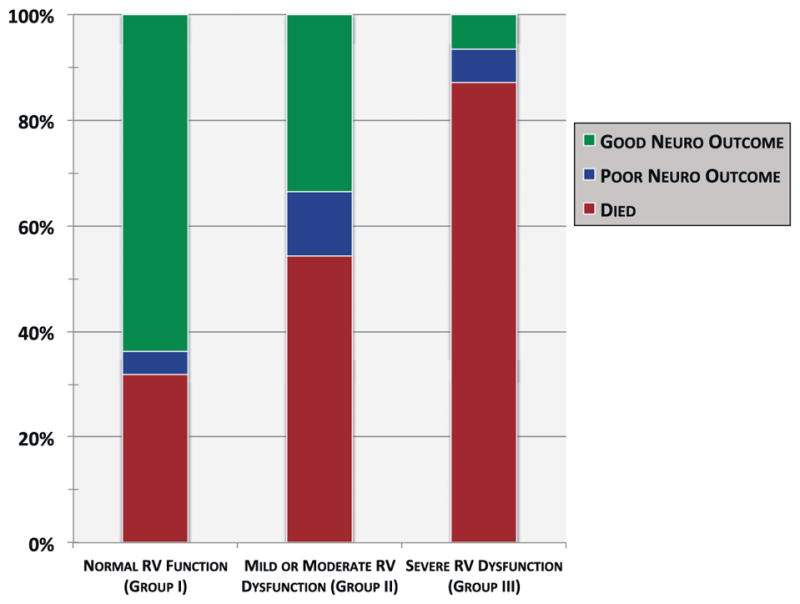
Neurologic and survival outcomes in cardiac arrest patients with post-arrest RV dysfunction. p < 0.05 for comparisons between all three groups.
Of patients who had both mild or moderate RV dysfunction and LV dysfunction, 50% (106) survived, and of those who had mild or moderate RV dysfunction with no LV dysfunction, 46% (64) survived (p = 0.482). Of patients with both mild or moderate RV dysfunction and LV dysfunction, 41% (87) had a favorable neurologic outcome (CPC 1 or 2). Of patients with mild or moderate RV dysfunction and no LV dysfunction, 34% (47) had a favorable neurologic outcome (CPC 1 or 2) (p = 0.179). Survival and neurologic outcomes for each category are shown in Table 4.
Table 4.
Mortality and neurologic outcome by group.
| % Survived (n) | % Good neurologic outcome (n) | |
|---|---|---|
| No RV dysfunction (Group I) | 68% (79) | 64% (74) |
| Mild or moderate RV dysfunction (Group II) | 46% (64) | 34% (47) |
| Severe RV dysfunction (Group III) | 13% (4) | 6% (2) |
| Any RV dysfunction (Group II and III) | 40% (68) | 29% (49) |
| Normal LV function | 52% (94) | 42% (45) |
| LV dysfunction | 51% (54) | 43% (79) |
Shown are the percent survival and percent with good neurologic outcome in each group; RV, right ventricular; LV, left ventricular.
In order to characterize the effect of reduction in RV systolic function alone (without RV dilation), we completed a multivariate logistic regression using only the RV systolic function score and not the RV dilation score. Controlling for the same variables, only moderate or severe reductions in RV systolic function were predictive of worse neurologic outcome (moderate: OR 0.36, CI 0.14–0.89, p = 0.026; severe: OR 0.25, CI 0.09–0.71, p = 0.009) compared to patients with normal RV systolic function. Similarly, only moderate or severe reductions in RV systolic function were predictive of worse survival (moderate: OR 0.34, CI 0.14–0.81, p = 0.015; severe: OR 0.36, CI 0.14–0.89, p = 0.027) compared to patients with normal RV systolic function.
Discussion
To our knowledge, this is the first study assessing echocardiographic right ventricular function and associated clinical outcomes after cardiac arrest. The present study sought to identify high-risk post-arrest patients by characterizing right ventricular systolic function and size on echocardiography to generate a composite RV dysfunction score (RVDS). We found a statistically significant relationship between RV dysfunction and mortality, as well as RV dysfunction and neurologic outcome post-arrest. Moreover, our findings support a clear, graded relationship between the RVDS, mortality, and neurologic outcome. Patients who were in Group III (severe RV dysfunction, RVDS = 5–6) demonstrated the highest mortality rates and poorest neurologic outcome. Patients in Group II (mild or moderate RV dysfunction, RVDS = 1–4) demonstrated intermediate mortality rates and neurologic outcome. Finally, patients in Group I (no RV dysfunction, RVDS = 0) demonstrated the lowest mortality rates and best neurologic outcome. Of note, the median duration of TTM and rewarming was not significantly different between the three groups. Interestingly, logistic regression analysis using RV systolic function alone without including RV dilation, resulted in a less robust effect on survival and neurologic outcomes, suggesting that RV dilation played an important role in outcomes of this population. The scoring system used to generate a semi-quantitative metric of overall RV function in this study was able to effectively stratify patients in a manner that was commensurate with morbidity and mortality burden. The simple scoring rubric (0 = normal, 1 = mild, 2 = moderate, 3 = severe) based on RV dilation and RV systolic function makes this straightforward approach an appealing potential method for future clinical use in the cardiac arrest setting. Importantly, this scoring system needs to be further validated prior further implementation.
Over the past two decades, there has been much focus on characterizing left ventricular function in the immediate post-arrest setting as a means of risk stratification.9–11,18 More recently, therapies have been tested to reduce LV dysfunction post-arrest in animal models.19 Several studies have looked at distinct aspects of the left ventricle as it relates to pre-arrest state, cardiopulmonary resuscitation (CPR), and survival outcomes without definitive evidence of association. Gonzalez et al.,9 for instance, found that patients with LV systolic dysfunction or normal LV systolic function post-arrest both had similar rates of ROSC and a similar reduction from pre-arrest LVEF, which puts into question the significance of isolated left ventricular systolic functional parameters in the post-arrest setting.
We sought to assess whether LV systolic dysfunction by itself and in combination with varying grades of RV dysfunction contributed to poor outcomes. We did not find a significant difference in survival or neurologic outcome in patients with normal LVEF as compared to those with LV systolic dysfunction. Furthermore, in patients with an LVEF < 50% in addition to mild or moderate RV dysfunction (Group II, RVDS score 1–4), there was no incremental increase in the rates of death or poor neurologic outcome compared to patients with mild or moderate RV dysfunction (Group II, RVDS score 1–4) alone. Collectively, these findings support the concept that LV systolic dysfunction parameters alone post-arrest may have limited utility in prognosticating or risk stratifying patients. It is widely known that LV systolic dysfunction in the peri-arrest setting frequently reflects myocardial stunning, which rapidly recovers with appropriate support.8,10 This reversible process may be one of a multitude of confounding factors – including pre-existing dysfunction, or acute myocardial infarction – that limit the prognostic utility of left ventricular function in the post-arrest phase.
Our findings expand upon the importance of the right ventricle in the clinical outcomes of the cardiac arrest population. Right heart failure is known to contribute to morbidity and mortality in a number of specific populations, including patients who are post-operative, particularly from cardiac surgery including cardiotomy, heart transplantation and left ventricular assist device placement.13,16,20–23 While these distinct patient populations –including post-arrest patients from our study – have shown a poor prognosis related to RV failure, the definitive causative mechanisms have yet to be clearly elucidated.
The RV, arising from the anterior heart field, is developmentally distinct from the left ventricle (LV) and thus demonstrates a number of important ischemia-resistant features that may account in part for our findings.13,24 The RV normally receives the predominance of its blood supply from the right coronary artery (RCA) circulation in right-dominant individuals, which comprises approximately 80% of the population. There are important oxygen supply-demand considerations that may play a protective role in the setting of coronary occlusion. Coronary perfusion, for instance, is phasic in the left coronary artery (LCA) system, with the predominance of flow occurring during diastole. RCA flow, however, has been shown to occur equally during diastole and systole, effectively increasing total perfusion time relative to the LCA.13 From the left anterior descending artery (LAD), the first or second septal perforator conventionally gives rise to the moderator band artery, which contributes to a more extensive collateral system along the RV myocardium that allows for uninterrupted flow in the setting of an RCA occlusion.13,25 The conus artery, which supplies the infundibular RV, has a separate ostium from the RCA in approximately 30–45% of patients, thereby protecting it from proximal RCA occlusions.13,25
At the cellular level, the RV demonstrates basal myocardial oxygen consumption that is approximately one-half to two-thirds that of the LV.25–27 Under stress conditions, the left ventricle preserves its function with augmented compensatory LCA flow given relatively fixed high levels of myocyte oxygen extraction.25–27 In the RV, however, myocytes are able to increase their oxygen extraction ratio while concurrently receiving augmented RCA flow.25–27 These salient cellular and anatomic features favor an ischemia-resistant RV substrate, thereby necessitating significant ischemic insult in order to cause RV dysfunction. Notwithstanding these developmental distinctions, other potential factors differentially affecting RV function may include ventilator-dependent factors (e.g. amount of positive end-expiratory pressure), degree of oxygenation or lack thereof, or comorbid pulmonary processes (e.g. pulmonary embolism, pulmonary hypertension), among others that were beyond the analytic scope of this database.
There are several important limitations to this study. First, our study is a retrospective cohort study and therein carries the biases of such a design including selection bias and misclassification. The infrastructure of the PATH registry and its constituent reporting system, however, addresses these biases by minimizing selection-related factors in the reporting of cardiac arrests. Misclassification or incorrect information, however, of the type of arrest as well as other patient clinical information remain potential factors intrinsic to any registry study. Finally, the PATH registry does not contain detailed information regarding the type of myocardial infarction (MI), whether revascularization was achieved, need for vasopressors, and percentage of patients with acute MI, acute pulmonary embolism, or shock, which are factors that may confound the findings in this study.
Importantly, the focus of this study was on echocardiographic findings in the setting of arrest, which were independently abstracted by study personnel directly from echocardiography reports that were finalized prior to the conception of this study. Level III board certified echocardiographers (completed National Board of Echocardiography) independently read all studies. Echocardiographic evaluation in this population has been limited to date, owing to the high level of illness acuity in this patient cohort. Importantly, there was variation in time-to-echocardiogram between patients in this study, which could have resulted in differences seen between groups to be confounded by care-related factors (e.g. therapeutic hypothermia, revascularization, etc.) In addition, the peri-arrest period presents technically challenging circumstances including significant time limitations, unstable patients, and targeted physician interest (i.e. Is there tamponade?) that can make echocardiographic assessment in this population difficult in the clinical setting.
Echocardiographic windows, in particular those pertinent to assessment of the RV, can also be compromised with patients in the ICU setting. Whereas tricuspid annular plane systolic excursion (TAPSE), RV fractional area change (FAC), tricuspid annular systolic tissue velocities, RV index of myocardial performance, RV free wall strain and 3D volumetric measures are newer quantitative methods that may outperform qualitative assessment, accurate application to RV size and function remains complicated, owing in part to the RV shape which is not amenable to geometric modeling. Recent guidelines from the American Society of Echocardiography recognize the validity of qualitative measures and recommend inclusion of a quantitative metric in the assessment of RV function when possible.28,29 This study employed a traditional semi-quantitative metric (i.e. RVDS) because RV size and function assessment were available on echocardiographic reports throughout the study period (2000–2012). During the earlier years of the study period, echocardiography labs were also not routinely employing quantitative assessments of RV size and function. Finally, the clinical utility of the presented scoring system – relying on simple RV size and function – may be more feasible in the arrest clinical setting than attempting to synthesize TAPSE, RV FAC, tissue Doppler, RV index of myocardial performance, RV free wall strain and 3D volumetric parameters in these critically ill patients. Nevertheless, these quantitative metrics may provide additional prognostic information if attainable in select patients but future studies will need to definitively address this. For the purposes of this study, we relied on expert interpretation of the echocardiograms without a separate, independent assessment.
Conclusions
This registry study shows that post-arrest RV dysfunction predicts worse survival and neurologic outcome independent of LV systolic function. These findings underscore the potential prognostic value of assessing the right ventricle in the peri-arrest phase and suggest that post-arrest LV systolic function alone may have limited prognostic value in this population. Further studies are needed to test the clinical applicability of these findings in a prospective fashion with deliberate focus on RV size and systolic function. The future implementation of echocardiographic RV assessment and an RV dysfunction score as part of a post-arrest care bundle may potentially be one initiative to improve cardiac arrest outcomes.
Acknowledgments
This research was supported by an NIH cardiovascular training grant (T32 HL007843) for Vimal Ramjee.
Footnotes
A Spanish translated version of the abstract of this article appears as Appendix in the final online version at http://dx.doi.org/10.1016/j.resuscitation.2015.08.008.
Conflict of interest statement
VR: none; AG: AHA Pre-doctoral Award; YY: none; SMP: none; ML: AHA grant, Resuscor LLC equity, and is a consultant for Stryker Medical; JNK: none; PRF: none; DMK: none; BSA: NIH, Medtronic Foundation and Stryker Medical Grants, Heartsine and Philips Healthcare honoraria, and Resuscor LLC equity; DFG: Stryker Medical and Bard Medical. None of the listed entities played any role in the funding, design, analysis or authorship of this research study.
References
- 1.Go AS, Mozaffarian D, Roger VL, et al. Executive summary: heart disease and stroke statistics – 2013 update: a report from the American Heart Association. Circulation. 2013;127:143–52. doi: 10.1161/CIR.0b013e318282ab8f. [DOI] [PubMed] [Google Scholar]
- 2.Merchant RM, Yang L, Becker LB, et al. Incidence of treated cardiac arrest in hospitalized patients in the United States. Crit Care Med. 2011;39:2401–6. doi: 10.1097/CCM.0b013e3182257459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peberdy MA, Callaway CW, Neumar RW, et al. Part 9: post-cardiac arrest care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S768–86. doi: 10.1161/CIRCULATIONAHA.110.971002. [DOI] [PubMed] [Google Scholar]
- 4.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics – 2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morrison LJ, Neumar RW, Zimmerman JL, et al. Strategies for improving survival after in-hospital cardiac arrest in the United States: 2013 consensus recommendations: a consensus statement from the American Heart Association. Circulation. 2013;127:1538–63. doi: 10.1161/CIR.0b013e31828b2770. [DOI] [PubMed] [Google Scholar]
- 6.Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 7.Goldberger ZD, Chan PS, Berg RA, et al. Duration of resuscitation efforts and survival after in-hospital cardiac arrest: an observational study. Lancet. 2012;380:1473–81. doi: 10.1016/S0140-6736(12)60862-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nolan JP, Neumar RW, Adrie C, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A scientific statement from the International Liaison Committee on Resuscitation; the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Peri-operative, and Critical Care; the Council on Clinical Cardiology; the Council on Stroke. 2008:350–79. doi: 10.1016/j.resuscitation.2008.09.017. [DOI] [PubMed] [Google Scholar]
- 9.Gonzalez MM, Berg RA, Nadkarni VM, et al. Left ventricular systolic function and outcome after in-hospital cardiac arrest. Circulation. 2008;117:1864–72. doi: 10.1161/CIRCULATIONAHA.107.740167. [DOI] [PubMed] [Google Scholar]
- 10.Kern KB, Hilwig RW, Rhee KH, Berg RA. Myocardial dysfunction after resuscitation from cardiac arrest: an example of global myocardial stunning. J Am Coll Cardiol. 1996;28:232–40. doi: 10.1016/0735-1097(96)00130-1. [DOI] [PubMed] [Google Scholar]
- 11.Kern KB, Hilwig RW, Berg RA, et al. Postresuscitation left ventricular systolic and diastolic dysfunction. Treatment with dobutamine. Circulation. 1997;95:2610–3. doi: 10.1161/01.cir.95.12.2610. [DOI] [PubMed] [Google Scholar]
- 12.Dolacky SD, Nair S, Kallur KR, Noyes A, Lundbye J. Does left ventricular systolic function on admission impact neurologic outcome in cardiac arrest survivors undergoing therapeutic hypothermia? J Am Coll Cardiol. 2012;59:E372. [Google Scholar]
- 13.Haddad F, Hunt SA, Rosenthal DN, Murphy DJ. Right ventricular function in cardiovascular disease, part I: anatomy, physiology, aging, and functional assessment of the right ventricle. Circulation. 2008;117:1436–48. doi: 10.1161/CIRCULATIONAHA.107.653576. [DOI] [PubMed] [Google Scholar]
- 14.Greyson CR. Pathophysiology of right ventricular failure. Crit Care Med. 2008;36:S57–65. doi: 10.1097/01.CCM.0000296265.52518.70. [DOI] [PubMed] [Google Scholar]
- 15.Voelkel NF, Quaife RA, Leinwand LA, et al. Right ventricular function and failure: report of a National Heart, Lung, and Blood Institute working group on cellular and molecular mechanisms of right heart failure. 2006:1883–91. doi: 10.1161/CIRCULATIONAHA.106.632208. [DOI] [PubMed] [Google Scholar]
- 16.Haddad F, Couture P, Tousignant C, Denault AY. The right ventricle in cardiac surgery, a perioperative perspective: II. Pathophysiology, clinical importance, and management. Anesth Analg. 2009;108:422–33. doi: 10.1213/ane.0b013e31818d8b92. [DOI] [PubMed] [Google Scholar]
- 17.Grossestreuer AV, Abella BS, Leary M, et al. Time to awakening and neurologic outcome in therapeutic hypothermia-treated cardiac arrest patients. Resuscitation. 2013;84:1741–6. doi: 10.1016/j.resuscitation.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 18.Kim H, Hwang SO, Lee CC, et al. Direction of blood flow from the left ventricle during cardiopulmonary resuscitation in humans: its implications for mechanism of blood flow. Am Heart J. 2008;156:1222e1–7. doi: 10.1016/j.ahj.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 19.Youngquist ST, Niemann JT, Shah AP, Thomas JL, Rosborough JP. A comparison of etanercept vs. infliximab for the treatment of post-arrest myocardial dysfunction in a swine model of ventricular fibrillation. Resuscitation. 2013;84:999–1003. doi: 10.1016/j.resuscitation.2012.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim J-H, Kim H-K, Lee S-P, et al. Right ventricular reverse remodeling, but not subjective clinical amelioration, predicts long-term outcome after surgery for isolated severe tricuspid regurgitation. Circ J. 2014;78:385–92. doi: 10.1253/circj.cj-13-0790. [DOI] [PubMed] [Google Scholar]
- 21.Auffret V, Boulmier D, Oger E, et al. Predictors of 6-month poor clinical outcomes after transcatheter aortic valve implantation. Arch Cardiovasc Dis. 2014;107:10–20. doi: 10.1016/j.acvd.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 22.Cameli M, Righini FM, Lisi M, et al. Comparison of right versus left ventricular strain analysis as a predictor of outcome in patients with systolic heart failure referred for heart transplantation. Am J Cardiol. 2013;112:1778–84. doi: 10.1016/j.amjcard.2013.07.046. [DOI] [PubMed] [Google Scholar]
- 23.Raina A, Seetha Rammohan HR, Gertz ZM, Rame JE, Woo YJ, Kirkpatrick JN. Postoperative right ventricular failure after left ventricular assist device placement is predicted by preoperative echocardiographic structural, hemodynamic, and functional parameters. J Card Fail. 2013;19:16–24. doi: 10.1016/j.cardfail.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 24.Zaffran S, Kelly RG, Meilhac SM, Buckingham ME, Brown NA. Right ventricular myocardium derives from the anterior heart field. Circ Res. 2004;95:261–8. doi: 10.1161/01.RES.0000136815.73623.BE. [DOI] [PubMed] [Google Scholar]
- 25.Dell’Italia LJ. The right ventricle: anatomy, physiology, and clinical importance. Curr Probl Cardiol. 1991;16:653–720. doi: 10.1016/0146-2806(91)90009-y. [DOI] [PubMed] [Google Scholar]
- 26.Zong P, Tune JD, Downey HF. Mechanisms of oxygen demand/supply balance in the right ventricle. Exp Biol Med (Maywood) 2005;230:507–19. doi: 10.1177/153537020523000801. [DOI] [PubMed] [Google Scholar]
- 27.Crystal GJ, Silver JM, Salem MR. Mechanisms of increased right and left ventricular oxygen uptake during inotropic stimulation. Life Sci. 2013;93:59–63. doi: 10.1016/j.lfs.2013.05.011. [DOI] [PubMed] [Google Scholar]
- 28.Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685–713. doi: 10.1016/j.echo.2010.05.010. quiz 786–8. [DOI] [PubMed] [Google Scholar]
- 29.Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–39. e14. doi: 10.1016/j.echo.2014.10.003. [DOI] [PubMed] [Google Scholar]


