Abstract
Injuries to the hypoglossal and vagus nerves are the most commonly reported injuries during carotid endarterectomy. While unilateral single nerve injury is usually well tolerated, bilateral or combined nerve injuries can pose a serious threat to life. This study aims to increase awareness of the inferior pharyngeal vein, which usually passes posterior to the internal carotid artery but sometimes crosses anterior to it. Injury to either or both hypoglossal and vagus nerves can occur during control of unexpected haemorrhage from the torn and retracted edges of the inferior pharyngeal vein. We recommend careful ligation and division of this vein. In addition, we observed in 9 (17.3%) of the 52 operations that the pharyngeal vein formed a triangle with the vagus and hypoglossal nerves when it passes anterior to the internal carotid artery.
Keywords: Carotid endarterectomy, Pharyngeal vein, Triangle
Introduction
The results of carotid endarterectomy have improved over the past three decades, nevertheless, the incidence of cranial nerve injury during surgery remains high.1 The most frequently affected cranial nerves are the hypoglossal, vagus and the marginal mandibular branch of the facial nerve, in descending order of frequency.1 This article discusses hypoglossal and vagus nerves injuries. It is well known that unilateral single-nerve injury is usually well tolerated but bilateral or combined ipsilateral nerve injuries may pose a serious threat to life. Injury to the hypoglossal nerve results in ipsilateral paralysis of the tongue muscles, deviation of the tongue to the ipsilateral side during protrusion and, when severe, clumsiness during speech and mastication. Bilateral hypoglossal nerve injury can cause airway obstruction, impairment of speech and difficulty with eating.
Injury to the vagus nerve and its branches
Injury of the recurrent laryngeal nerve is the indirect result of injury to the vagus. It produces paralysis of the ipsilateral vocal cord in the paramedial position, hoarseness of voice and loss of an effective cough mechanism. Bilateral injury to the recurrent laryngeal nerve may be life threatening due to airway obstruction. Direct injury to the superior laryngeal nerve and its branches, the internal and external laryngeal nerves can occur during unclamping and reclamping of the external carotid artery. The external laryngeal nerve can also be injured during dissection and control of the superior thyroid artery, leading to paralysis of the cricothyroid muscle. This results in mild relaxation and thickening of the ipsilateral vocal cord, manifested by early fatigability of the voice and impairment of phonation at a high pitch. Bilateral damage to the internal laryngeal nerve produces anaesthesia of the mucous membrane at the entrance of the larynx, with loss of protective cough and possibly of aspiration into the lungs.
There is wide variation in the reported incidence of nerve injuries in different centres. Sajid et al.1 reviewed 31 studies published between 1985 and 2005 involving 10,847 patients. In total, there were 1020 cranial nerve injuries (9.6% P < 0.0001). The incidence varied from 1.35% to 31.25%.
Surgeons should be familiar with the detailed anatomy of the region, the potential mode of nerve injury and the resulting disability. The aim of this study is to increase awareness of the inferior pharyngeal vein and its relationship to the hypoglossal and vagus nerves. In this paper, we describe the identification of an anatomical triangle formed by the inferior pharyngeal vein, hypoglossal nerve and the vagus nerve (Fig 1).
Figure 1.

Hand drawing of the triangle.
Methodology
This paper consists of two parts, the first is based on a prospective clinical study published in 1988 and cited by 61 related articles.2 This prospective clinical study was conducted at the Bristol Royal Infirmary and included 51 consecutive patients, in whom 52 carotid endarterectomies were performed under general anaesthesia (41 men and 10 women, mean age 61 years, range 50–75 years). All patients underwent pre- and postoperative vocal cord assessment using indirect laryngoscopy. Postoperative assessment and duplex carotid scanning took place within two weeks of surgery.
The observations of the first author (MA), then, of a vein and occasionally veins crossing the internal carotid artery and its close relation to the hypoglossal and vagus nerves spurred him to explore further through anatomy textbooks and more recently to pursue an anatomical study, which forms the basis of the second part of this paper.
Results
Of the 52 endarterectomies, there were 13 temporary cranial nerve injuries reported in 12 patients (25%) (7 XII, 3 X and 3 VII)
Hypoglossal nerve
There were 7 hypoglossal nerve paresis (13.5%). Of these, three were asymptomatic (5.8%), two had mild speech difficulty (3.8%) and two (3.8%) had severe difficulty with deglutition and articulation. Both had unexpected bleeding which was controlled by diathermy. A full recovery was made within 3 months in all patients.
Vagus nerve
Ten patients (19.2%) all with normal, preoperative vocal cords had postoperative hoarseness of voice. Three (5.8%) had an immobile ipsilateral vocal cord, including one patient with an anomalous non-recurrent laryngeal nerve. Two recovered within 6 months and one within 9 months (also had mild hypoglossal paresis). Two patients had a husky voice, which tired easily, in whom indirect laryngoscopy was inconclusive. They recovered within 6 months. The remaining five patients had normal vocal cords.
While undertaking this study and during the first 22 carotid endarterectomies, there were six hypoglossal nerve injuries. Two had severe difficulty with deglutition and articulation and both had bleeding controlled by diathermy. One patient had mild hypoglossal injury with severe recurrent laryngeal nerve injury and took 9 months to recover. One patient had mild facial paresis. An observation of a small vein and occasionally two veins crossing the internal carotid artery was made (Figs 2 and 3).
Figure 2.
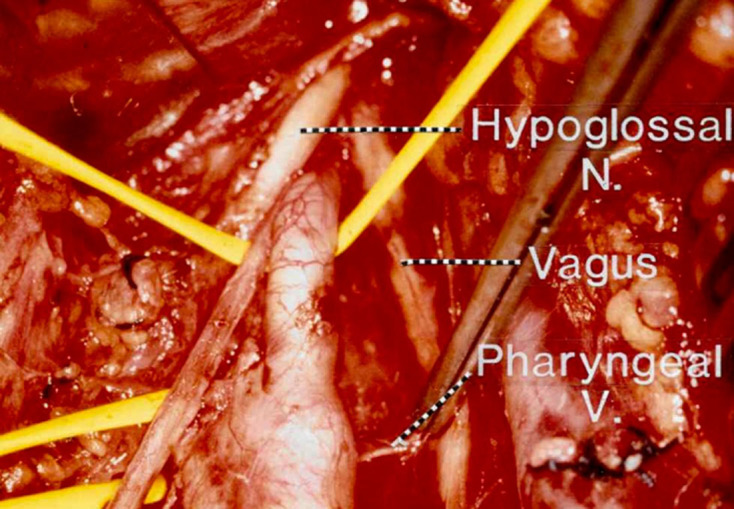
Operative image showing the pharyngeal passing posterior to the carotid bifurcation.
Figure 3.
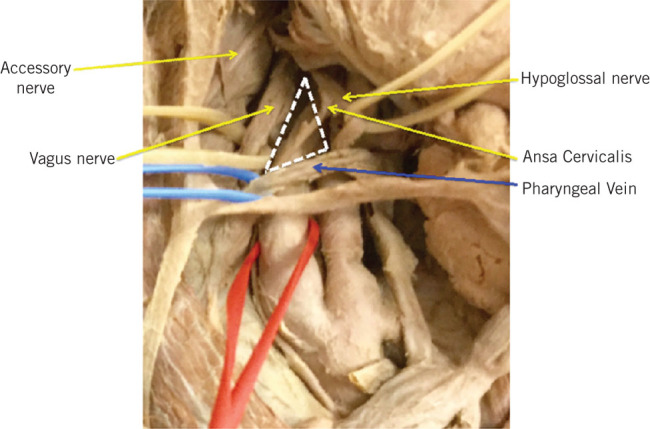
Cadaveric image showing the pharyngeal vein crossing in the front of the carotid bifurcation forming the triangle.
There was no reference to the name of this vein but, upon consulting Gray’s and Last’s anatomy textbooks, it was identified as the inferior pharyngeal vein, which drains either in the internal jugular or the common facial vein. In reaching the internal jugular vein, it passes behind internal carotid artery (Fig 2). However, the author observed in nine patients that this vein crosses in front of the internal carotid artery, thus forming a triangle with the hypoglossal and vagus nerves (Fig 3). This vein can be damaged by retraction during crucial stage of the endarterectomy procedure, specifically during feathering the atheroma at the top end of the operation. In controlling the bleeding from this vein by diathermy, the hypoglossal and/or and the vagus nerves can be damaged, as the cut end of the vein retracts behind these nerves (Fig 4).
Figure 4.

Mode of injury to cranial nerves during carotid endarterectomy.
There were six hypoglossal nerve injuries during the first 22 carotid endarterectomies. Following this observation, greater attention was paid through good exposure to identifying, ligating and dividing this vein carefully. This enabled the reduction in the incidence of hypoglossal nerve injury to only one case in the remaining 30 carotid endarterectomies.
The author observed that when this inferior pharyngeal vein occasionally crosses in front of the internal carotid artery, it forms an anatomical triangle with the hypoglossal and vagus nerves. This triangle was demonstrated in 9 (17.3%) of the 52 operations.
Cadaveric study
The anatomical part of the study was undertaken with Professor Vishy Mahadevan in December 2016 at the Royal College of Surgeons of England. A cadaveric dissection of five subjects was undertaken. This anatomical triangle was identified in two cases. To our knowledge we are the first to identify this vein and to describe this triangle.
Discussion
Although there is extensive literature on the incidence of cranial nerve injury during carotid endarterectomy, there have been few studies identifying risk factors leading to these complications.3 Both the hypoglossal and vagus nerves have intimate relations with internal carotid artery, so they are more liable to injury during carotid endarterectomy. The hypoglossal nerve is usually tethered to the internal carotid artery by the descendis hypoglossi and sternomastoid artery (branch of the occipital Artery) and the accompanying vein. Traction or mobilisation may be necessary to gain good exposure.
Imparato recommended division of the descendis hypoglossi, the sternomastoid artery and the accompanying vein, so that the nerve can be displaced superiorly and medially (Fig 5).4 Greenhalgh has suggested that gentle retraction and deviation of the nerve by tape or sling may be sufficient.5 We believe that Imparato’s manoeuvre is helpful in difficult cases, when the carotid bifurcation is high or the atheroma is extensive at distal end.
Figure 5.
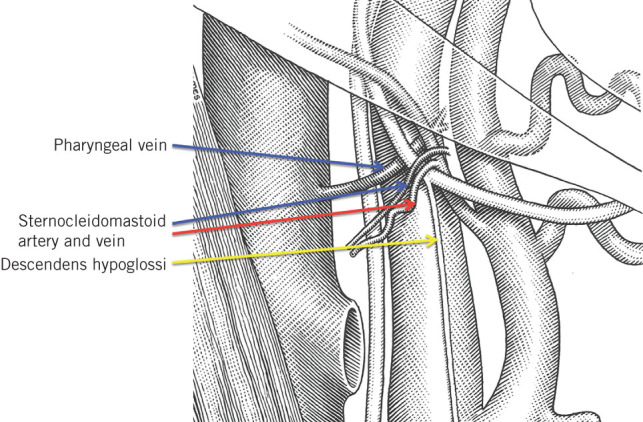
Mobilisation of the hypoglossal nerve as described by lmparato in 1972
The vagus may be damaged during dissection of the internal carotid artery and common carotid artery, by diathermy burn or by inclusion of the nerve in the tip of the arterial clamp (Fig 4). The vagus nerve descends vertically within the carotid sheath, in the posterolateral position, lying between the internal jugular vein and internal carotid artery and subsequently the common carotid artery. It occasionally winds around the carotid artery to lie anterior to the common carotid artery and medial to the internal jugular vein and may be mistaken for the descendens hypoglossi.
Injury to RLN is mostly indirect, due to damage of the medial fibres of the vagus.6 We therefore recommend gentle traction and careful use of diathermy in the triangle. Direct injury to the recurrent laryngeal nerve within the tracheo-oesophageal groove is rare; it could happen if retractor blades are placed too deeply in the medial aspect of the incision.
In 1980 and in 1984, Norman Hertzer suggested that the vena commitant hypoglossi should be ligated to prevent bleeding during the crucial steps of the operation.7,8 In 1984, Roger Greenhalgh stated, ‘Any veins which cross the internal carotid artery will prevent mobilisation of the hypoglossal nerve and should be divided between clips and ligated’.5 As far as we know, no one has specifically made reference to the inferior pharyngeal vein.
The retrojugular approach was primarily introduced for re-do surgery and was later adopted for primary carotid endarterectomy. This technique enables a higher exposure of the internal carotid artery to avoid the veins crossing the internal carotid artery. In 2008, Beasley and Gibbons compared the retrojugular with the conventional anteromedial approach to carotid endarterectomy. The risk of cranial nerve injury was similar in both approaches, although a higher incidence of accessory nerve injury was reported in the retrojugular approach (Fig 3).9
On reviewing the literature, the following are independent factors associated with an increased risk of cranial nerve injury during carotid endarterectomy. Zannetti et al.10 found that the length of distal plaque extension is the only factor associated with cranial nerve injury. Gunningham retrospectively analysed the data of 1739 patients in the European Symptomatic Carotid Trial and found the length of the operation to be the only risk factor.11 Bennett et al.3 reported four independent factors: prolonged surgery, immediate re-exploration for stroke and for haemorrhage, preoperative bleeding disorder and age above 80 years.
Conclusion
The description of this anatomical triangle and the naming of the inferior pharyngeal vein, forming this triangle, may assist the surgeon in identifying, ligating and avoiding bleeding at the crucial part of the carotid endarterectomy. Good knowledge of anatomy, precise technique with attention to detail is essential for carotid surgery.
References
- 1.Sajid MS, Vijagnagar B, Singh P, Hamilton G. Literature review of cranial nerve injuries during carotid endarterectomy. Acta Chir Belg 2007; (1): 23–28. [DOI] [PubMed] [Google Scholar]
- 2.Aldoori MI, Baird RN. Local neurological complication during carotid endarterectomy. J Cardiovasc Surg (Torino) 1988; (4): 432–436. [PubMed] [Google Scholar]
- 3.Bennett KM, Scarborough JE, Shortell CK, Durham NC. Risk factors for cranial nerve injury after carotid endarterectomy. J Vasc Surg 2015; : 363–369. [DOI] [PubMed] [Google Scholar]
- 4.Imparato AM, Bracco A, Kim GE, Zeff R. The hypoglossal nerve in carotid arterial reconstruction. Stroke 1972; : 576–578. [DOI] [PubMed] [Google Scholar]
- 5.Greenghalgh RM. Carotid endarterectomy : Greenhalgh RM, Vascular Surgical Techniques. London: Butterworths; 1984. pp41–48. [Google Scholar]
- 6.Dehn TCB, Taylor GW. Cranial and cervical nerve damage associated with carotid endarterectomy. Br J Surg 1983; : 365–368. [DOI] [PubMed] [Google Scholar]
- 7.Hertzer NR, Feldman BJ, Beven EJ. A prospective study, of the incidence of injury to the cranial nerves during carotid endarterectomy. Surg Gynaecol Obstet 1980; : 781–784. [PubMed] [Google Scholar]
- 8.Hertzer NR. Vascular surgery : Rutherford RB, 2nd ed, Postoperative Management and Complications of Extra Cranial Carotid Reconstruction. Philadelphia, PA: WB Saunders; pp113–131. [Google Scholar]
- 9.Beasley WD, Gibbons CP. Cranial nerve injuries and the retrojugular approach in carotid endarterectomy. Ann R Coll Surg Engl 2008; (8): 685–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zannetti S, Parente B, De Rango P et al. . Role of surgical techniques and operative findings in cranial and cervical nerve injury during carotid endarterectomy. Eur J Vasc Endovasc Surg 1998; ; 528–531. [DOI] [PubMed] [Google Scholar]
- 11.Gunningham EJ, Bond R, Mayberg MR et al. . Risk of persistent cranial nerve injury after carotid endarterectomy, J Neurosurg 2004; : 45–48. [DOI] [PubMed] [Google Scholar]


