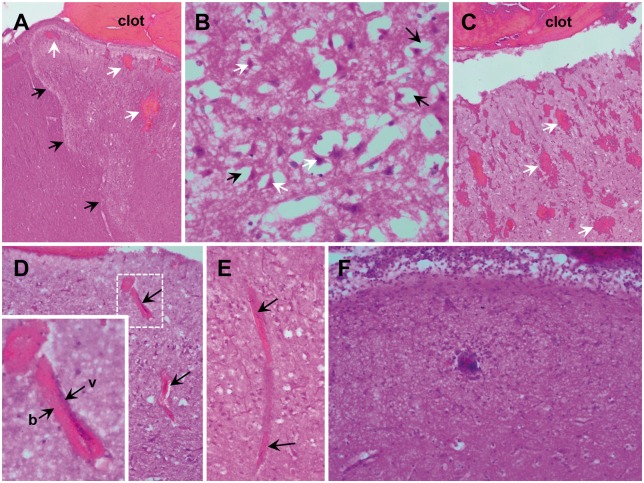
Figure 6.
Histologic sections of cortical ischaemia adjacent to sulcal subarachnoid clots. (A) Zonal oedema (black arrows show borders) of cortex with intraparenchymal haemorrhage (white arrows) adjacent to subarachnoid clot (×40). Zones of ischaemic change were irregularly shaped, extending to involve the full cortical thickness. (B) Acute hypoxic-ischaemic neuronal cell injury (×400) is observed within these zones, as well as the immediately adjacent parenchyma, marked by pericellular vacuolization (black arrows) and neurons with scalloped morphology, pyknotic nuclei, and hyper-eosinophilic cytoplasm (white arrows). (C) Blood within perivascular spaces and extension into the adjacent parenchyma (petechial haemorrhages, white arrows) was seen focally in some cases and more prominently in others (×40). (D) In general, the extension of blood within perivascular (Virchow-Robin) spaces was more prominent within superficial cortex. Perivascular blood was present at least focally in all animals, but was prominent in some. The vessels (v) surrounded by blood (b) were frequently collapsed (×100, arrows and inset), as indicated by the lack of intravascular erythrocytes and lack of distinctive vessel walls. Congestion of the capillaries, microvasculature and small venules were present in the region of oedema. (E) A representative small venule with perivascular blood and collapse superficially (top arrow) with congestion noted in the deeper aspect (bottom arrow; ×100). (F) In nearly all animals, there was moderate to prominent layering of neutrophils (polymorphonuclear leucocytes) within the leptomeninges, with extension into the superficial parenchyma (×200). Occasional arteries also contained neutrophils with margination and, rarely, focal extravasation. No intravascular thrombi were identified.