Abstract
Objective
Mortality due to intensive care unit (ICU) acquired primary blood stream infections (PBSI) is related primarily to patient co-morbidities, types of pathogens and quality of care. The objective of this study is to determine the impact of various types of pathogen on ICU mortality.
Methods
Data from the German National Nosocomial Infection Surveillance System of patients with PBSI from 2006 to 2015 was used for this analysis. A BSI is primary when the pathogen recognized is not related to an infection on another site. Only mono-microbial infections stratified into the 13 pathogens most frequently causing PBSI were considered. Univariate and multivariate risk factor analyses were performed using the following risk factors: Sex, age, length of stay, device use, time until onset of PBSI, type and size of hospital, type of ICU and type of pathogen. ICU mortality following S.aureus PBSI was used as the reference value.
Results
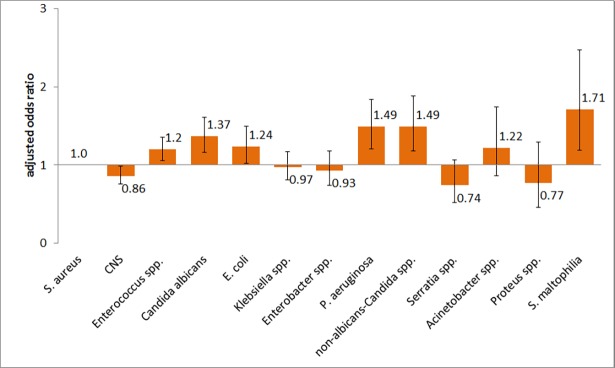
A total of 4,556,360 patients with 16,978,882 patient days from 937 ICUs were considered in the analysis. Of 14,626 PBSI in total, 12,745 mono-microbial PBSI were included. The ICU mortality was 18.6%. Compared with S.aureus and adjusted by age, sex and type of ICU, S.maltophilia was associated with significantly higher ICU mortality (OR 1.71; 95%CI 1.19–2.47) as followed by Enterococci (OR 1.20; 95%CI 1.06–1.36), E.coli (OR 1.24; 95%CI 1.02–1.49), C.albicans (OR 1.37; 95%CI 1.16–1.61), non albicans Candida spp. (OR 1.49; 95%CI 1.18–1.88) and P.aeruginosa (OR 1.49; 95%CI 1.21–1.84). Coagulase negative Staphylococci were associated with significant lower ICU mortality (OR 0.86; 95%CI 0.75–0.99).
Conclusion
Because of the limitation of the study in adjusting for severity of illness and appropriateness of therapy, the differences between the pathogens may not only be explained by differences in virulence, but may reflect the prognosis after receiving the microbiological results and may therefore be useful for intensive care physicians.
Introduction
Primary bloodstream infections (PBSI) in intensive care units (ICU) are associated with high mortality. This mortality is related to patient factors (sex, age and underlying diseases), adequate antibiotic therapy ICU factors (staff to patient ratios, safety climate, etc.) and the pathogens responsible. Some pathogens (e.g. P.aeruginosa) and some multi-drug resistant variants of pathogens (e.g. multiresistant A.baumannii) are known to be associated with significantly higher ICU mortality [1–3]. However, such information is not available for many other pathogens that frequently cause primary bloodstream infections (PBSI).
The reason for this lack of information is the need to analyze large numbers of PBSI cases. In addition, it would be preferable to diagnose infections by applying definitions designed for surveillance and not those derived from other databases, e.g. discharge data. Furthermore, information about the most important risk factors needs to be available, including the time interval between ICU admission and the onset of infection. Therefore, only a few studies have been able to provide comparable information about mortality based on the type of pathogen [3–8]. Many included only a small number of species or did not consider information for such frequently occurring pathogens like E.coli or Enterococci.
The ICU component of the German National Nosocomial Infection Surveillance System (KISS) includes a large number of ICUs [9]. In the case of healthcare-associated PBSI, it records not only the type of pathogen isolated from relevant microbiological samples, but also the time from admission to the ICU until occurrence of PBSI. This database allows the analysis of differences between various pathogens that cause PBSI in ICUs in ICU mortality.
The objective of this study is to determine the impact of the type of pathogen on ICU mortality following a ICU-acquired PBSI.
Material and methods
Ethics statement
All data was anonymous and was collected in accordance with the German recommendations for good epidemiological practice with respect to data protection ((DAE) AEMdDAE (2013) Leitlinien und Empfehlungen zur Sicherung von Guter Epidemiologischer Praxis (GEP): http://www.gesundheitsforschung-bmbf.de/_media/GEP.pdf. Accessed 05 May 2017). A federal law, the German Protection against Infection Act (Infektionsschutzgesetz §23) regulates the prevention and management of infectious disease in humans. All hospitals are obliged to continuously collect and analyse healthcare-associated infections and drug-resistant pathogens (German Protection against Infection Act. "Gesetz zur Verhütung und Bekämpfung von Infektionskrankheiten beim Menschen" (2013): http://www.gesetze-im-internet.de/ifsg/index.html. Accessed 05 May 2017). This data is reported regularly to the National Reference Centre for the Surveillance for Nosocomial Infections. Ethical approval and informed consent were, therefore, not required.
Data collection
Surveillance data from a ten-year period from January 2006 until December 2015 was used for the analysis. ICU-KISS is a unit-based surveillance system like the ICU component of the American National Healthcare Safety Network (NHSN). During this period, CDC definitions were used to diagnose PBSI [10]. A primary BSI was defined as a positive blood culture with one (or more) pathogen(s) which was not related to an infection on another site. For a BSI with skin germs, for example with coagulase negative Staphylococci (CNS), the definition also requires further clinical signs and the physician starts according to an antibiotic therapy. However, beginning in 2011 a new CDC definition of PBSI with skin germs was introduced [11]. Since that time two separate blood cultures are required for skin germs in combination with other clinical signs. The PBSI was defined as CVC-associated when the patient that had a CVC at the time of or within 48 hours before onset of the infection.
In the case of an ICU-acquired PBSI, the surveillance staff has to record the time to BSI, the ICU mortality and the pathogens identified in the blood culture. Up to four pathogens can be recorded per infection. Only mono-microbial infections were considered in the analysis. The 13 most common organisms causing PBSI were analyzed individually: coagulase negative Staphylococci (CNS), Enterococcus spp., S.aureus, C.albicans, non-albicans-Candida spp., E.coli, Klebsiella spp., Enterobacter spp., P.aeruginosa, Serratia spp., Acinetobacter spp., Proteus spp., and S.maltophilia. All other pathogens were analyzed as type “other”. In addition, for the 13 organisms specified we categorized the organisms into the pathogen groups (gram-positive/gram-negative bacteria/fungi) and multi-drug resistance groups (non-MDR/MDR). MDR was defined as Methicillin resistant for S.aureus, Vancomycin resistant for E.faecalis and E.faecium, and a resistance to at least three antibiotic groups for P.aeruginosa, Acinetobacter spp., Enterobacter spp., E.coli, S.maltophilia, Klebsiella spp. and/or the resistance mechanisms ESBL for K.pneumonia and E.coli.
Statistical analysis
In our analysis, the primary outcome was ICU mortality following ICU-acquired PBSI. Univariable and multivariable risk factor analyses were performed to identify organisms (pathogen groups and/or multidrug resistance groups) associated with increased or decreased risk of ICU mortality as well as additional related factors and confounders, such as sex (male/female), age group (≤45/46-55/56-65/66-75/>75years), time from admission to the ICU until onset of PBSI(days), CVC associated with PBSI (no/yes), type of ICU (8 categories), size of ICU (</≥12 beds), type of hospital (tertiary care yes/no), and size of hospital (</≥600 beds), season(Dec-Feb/Mar-May/Jun-Aug/Sep-Nov) and long-term time trends (year). In the univariable analysis, differences were tested by Chi-Square test or Wilcoxon rank-sum test. Parameters with more than two categories were tested as binary parameters.
In the multivariable analysis, a logistic regression analysis was performed. Since observations within an ICU are not statistically independent due to varying patient populations (especially the treatment management), adjusted odds ratios (OR) with 95% confidence intervals (CI) were calculated. They were based on generalized estimating equation (GEE) models which account for this clustering effect by using an exchangeable correlation structure. The multivariable model building strategy was performed stepwise backward, from a full model with all parameters, non-significant parameters were excluded with the significance level of p = 0.05 for excluding a parameter from the model in the type III test. S.aureus was used as reference micro-organisms because this pathogen frequently causes PBSI, and it is very likely that, when detected in a blood culture, it is the responsible pathogen, in contrast to coagulase negative Staphylococci, which are often regarded as skin contaminants. In addition, experts agree that S.aureus is a common cause of severe bloodstream infections, and mortality and morbidity of S.aureus bacteremia still remain considerably high [12–13]. Furthermore, other studies have provided substantial information about S.aureus mortality which can be used for comparison [8], [14]. For epidemiological reasons, age group and sex were included in all models. P-values less than 0.05 were considered significant.
Beside age, gender and time to PBSI, no more individual patient-based parameters are available in the multivariable analysis which describe the severity of illness of the patients. However, structure parameters, such as type and size of ICU, and type and size of the hospital where the ICU is located, were considered in the multivariable analysis.
In addition, to better characterize risk potential of patients, we conducted a further multivariable analysis which considered the monthly mean of length of stay (LOS), device use (central venous catheter, invasive ventilation and urinary tract catheter) and bed occupation of the ICU in which the PBSI occurs. These results do not differ from the results without these parameters. Therefore, we present the results without these parameters.
All analyses were performed using SPSS [IBM SPSS statistics, version 23, Somer, NY, USA] and SAS 9.4 [SAS Institute, Cary, NC, USA].
Results
A total of 4,556,360 patients with 16,978,882 patient days from 937 ICUs (> = 1 PBSI) were considered in the analysis. Table 1 describes the characteristics of the ICUs included.
Table 1. Characteristics of 973 intensive care units (ICU) included in the study, ICU-KISS, 2006–2015.
| Parameter | Description | Number | Percentage |
|---|---|---|---|
| ICUs | total | 937 | 100.0% |
| Surveillance time of ICU | Months (median, IQR) | 56 | 30–95 |
| Size of ICU | ICU beds (median, IQR) | 12 | 8–15 |
| Size of hospital | Hospital beds (median, IQR) | 439 | 270–749 |
| Type of hospital | Non tertiary care | 659 | 70.4 |
| Tertiary care | 278 | 29.6 | |
| Type of ICU | Interdisciplinary | 495 | 52.8% |
| Medical | 140 | 14.9% | |
| Surgical | 162 | 17.3% | |
| Neurosurgical | 24 | 2.6% | |
| Cardiosurgical | 26 | 2.8% | |
| Neurological | 19 | 2.0% | |
| Pediatric | 26 | 2.8% | |
| Other a | 45 | 4.8% | |
| Length of stay | Days (median, IQR) | 3.7 | 2.9–5.3 |
| CVC utilization rate | CVC days per 100 pd (median, IQR) | 65.9 | 51.0–79.8 |
| Ventilator utilization rate | Ventilator days per 100 pd (median, IQR) | 35.5 | 25.4–49.5 |
| UC utilization rate | UC days per 100 pd (median, IQR) | 84.0 | 72.8–91.7 |
| Incidence density PBSI | PBSI/1000 pd (median, IQR) | 0.64 | 0.33–1.14 |
PBSI, primary bloodstream infection; CVC, central venous catheter; UC, urinary catheter; pd, patient days; IQR, interquartile range.
a other than Medical-surgical, Surgical, Medical, Cardiothoracic, Neurosurgical, Neurological or Pediatric.
A total of 14,626 PBSI were recorded, that is, an incidence of 0.32 per 100 patients or 0.86 per 1000 patient days. 95% of the PBSI were CVC-associated and the proportion does not change during the study period. For 12,745 PBSI, only one pathogen was isolated from the blood culture (87.1%).
The overall ICU mortality was 18.6% for PBSI. Mortality in multi-microbial PBSI was 24.1% (RR = 1.29, 95%CI 1.17–1.43, p<0.001 compared to mono-microbial PBSI).
Time in the ICU until onset of PBSI was in median 14 days and differs depending on the type of pathogen, PBSI were observed early in the case of E.coli (11 days) or S.aureus (12 days), but late if Klebsiella spp., non-albicans Candida spp. (both 16 days), P.aeruginosa (18 days) or S.maltophilia (19 days) were found.
Table 2 shows mortality following mono-microbial PBSI for the various risk groups, confounders and pathogens in ICU-KISS from 2006 to 2015. Significances were found for sex, age, type of ICU and hospital also for type of organisms, organism groups and multidrug resistance groups responsible.
Table 2. Results of univariate analysis for mortality in intensive care units (ICU) following mono-microbial primary bloodstream infections (PBSI) according to the type of organism and further risk factors and confounders, ICU-KISS, 2006–2015.
| Parameter | Category | No. not died | No. died | Mortality (%) | p-valuea |
|---|---|---|---|---|---|
| Patients with BSI | Total | 10369 | 2376 | 18.6 | |
| Type of organism | CNS | 3579 | 641 | 15.2 | <0.001 |
| Enterococcus spp. | 1636 | 471 | 22.4 | <0.001 | |
| S. aureus | 1522 | 338 | 18.2 | 0.573 | |
| Candida albicans | 510 | 166 | 24.6 | <0.001 | |
| E. coli | 434 | 125 | 22.4 | 0.021 | |
| Klebsiella spp. | 498 | 102 | 17.0 | 0.290 | |
| Enterobacter spp. | 366 | 68 | 15.7 | 0.105 | |
| P. aeruginosa | 242 | 84 | 25.8 | 0.001 | |
| non-albicans-Candida spp. | 172 | 64 | 27.1 | 0.001 | |
| Serratia spp. | 162 | 27 | 14.3 | 0.121 | |
| Acinetobacter spp. | 91 | 21 | 18.8 | 0.977 | |
| Proteus spp. | 72 | 12 | 14.3 | 0.304 | |
| S. maltophilia | 48 | 19 | 28.4 | 0.041 | |
| Other organisms b | 1037 | 238 | 18.7 | 0.981 | |
| Time to onset of infection | Days (median) | 14 | 14 | 0.958 | |
| Gender | Male | 6989 | 1541 | 18.1 | 0.017 |
| Age | Years (median) | 68 | 73 | <0.001 | |
| Age group | ≤45 years | 2563 | 273 | 9.6 | <0.001 |
| 46–55 years | 1990 | 399 | 16.7 | 0.007 | |
| 56–65 years | 3010 | 730 | 19.5 | 0.102 | |
| >65 years | 2806 | 974 | 25.8 | <0.001 | |
| CVC associated g | Yes | 9846 | 2276 | 18.8 | 0.089 |
| Size of hospital | ≥600 beds | 5372 | 1224 | 18.6 | 0.796 |
| Size of ICU | ≥12 beds | 7264 | 1637 | 18.4 | 0.267 |
| Type of hospital | Tertiary care | 4778 | 968 | 16.8 | <0.001 |
| Type of ICU | Interdisciplinary | 4668 | 1098 | 19.0 | 0.292 |
| Medical | 1437 | 417 | 22.5 | <0.001 | |
| Surgical | 2482 | 525 | 17.5 | 0.057 | |
| Neurosurgical | 360 | 26 | 6.7 | <0.001 | |
| Cardiosurgical | 437 | 157 | 26.4 | <0.001 | |
| Neurological | 215 | 23 | 9.7 | <0.001 | |
| Pediatric | 324 | 19 | 5.5 | <0.001 | |
| Other h | 446 | 111 | 19.9 | 0.426 | |
| Year of BSI | 2006 | 687 | 157 | 18.6 | 0.426 |
| 2007 | 784 | 159 | 16.9 | 0.975 | |
| 2008 | 830 | 191 | 18.7 | 0.956 | |
| 2009 | 958 | 197 | 17.1 | 0.147 | |
| 2010 | 1000 | 230 | 18.7 | 0.957 | |
| 2011 | 1051 | 225 | 17.6 | 0.329 | |
| 2012 | 1120 | 251 | 18.3 | 0.736 | |
| 2013 | 1230 | 299 | 19.6 | 0.329 | |
| 2014 | 1335 | 318 | 19.2 | 0.505 | |
| 2015 | 1374 | 349 | 20.3 | 0.065 | |
| Season | Winter (Dec-Feb) | 2396 | 577 | 19.4 | 0.221 |
| Spring (Mar-May) | 2613 | 620 | 19.2 | 0.366 | |
| Summer (Jun-Aug) | 2797 | 609 | 17.9 | 0.182 | |
| Autumn (Sep-Nov) | 2563 | 570 | 18.2 | 0.457 | |
| Pathogen groups | Gram-positive d | 6737 | 1450 | 17.7 | <0.001 |
| (N = 11470) | Gram-negative e | 1913 | 458 | 19.3 | 0.342 |
| Fungi f | 682 | 230 | 25.2 | <0.001 | |
| Multi-drug (MDR) resistance groups (N = 6065) | MDR c | 779 | 265 | 25.4 | <0.001 |
No., number; CNS, Coagulase negative staphylococci; CVC, central venous catheter; pd, patient days.
a p-values, Chi-square test or Wilcoxon rank sum test
b other than the 13 most common organisms causing PBSI: coagulase negative Staphylococci (CNS), Enterococcus spp., S. aureus, C.albicans, non-albicans-Candida spp., E. coli, Klebsiella spp., Enterobacter spp., P. aeruginosa, Serratia spp., Acinetobacter spp., Proteus spp., and S. maltophilia;
c MDR, Multi-drug resistance includes Methicillin resistant S.aureus, Vancomycin resistant E.faecalis and E.faecium, and multidrug resistance defined as a resistance to at least 3 antibiotic groups for P.aeruginosa, Acinetobacter spp., Enterobacter spp., E.coli, S.maltophilia, Klebsiella spp. and/or the resistance mechanisms ESBL for Klebsiella pneumonia and E.coli, MDR compared to Non-MDR, includes Vancomycin sensible Enterococcus spp., Methicillin sensible S. aureus and non-multi-drug resistance for E. coli, Klebsiella spp., Enterobacter spp., P. aeruginosa, Acinetobacter spp., S. maltophilia
d includes coagulase negative Staphylococci (CNS), Enterococcus spp., S. aureus;
e includes E. coli, Klebsiella spp., Enterobacter spp., P. aeruginosa, Serratia spp., Acinetobacter spp., Proteus spp., and S. maltophilia;
f C. albicans, non-albicans-Candida spp.
g device present <48h before diagnosis of infection
h other than Medical-surgical, Surgical, Medical, Cardiothoracic, Neurosurgical, Neurological or Pediatric.
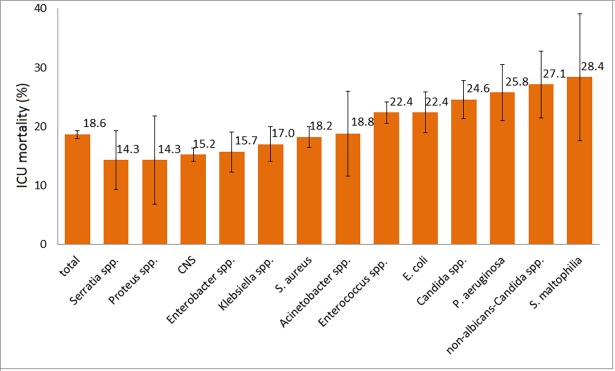
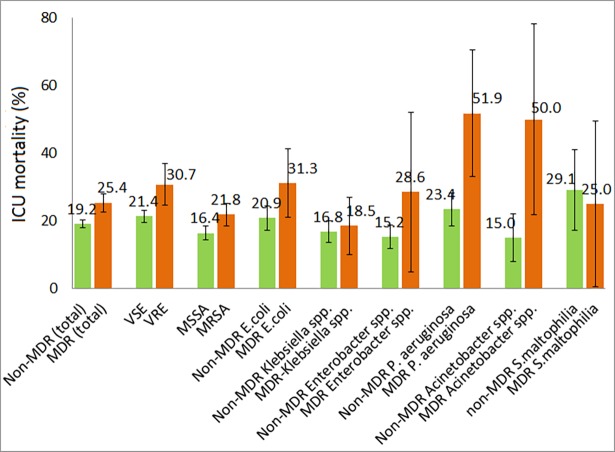
ICU mortality following mono-microbial ICU-acquired PBSI for the type of pathogen is also illustrated in Fig 1 and stratified according to the resistance of pathogen in Fig 2.
Fig 1. ICU mortality in patients with ICU-acquired primary bloodstream infections according to the type of pathogen.
ICU, intensive care unit; CNS, coagulase negative staphylococci; Whiskers represent 95% confidence interval.
Fig 2. ICU mortality in patients with ICU-acquired primary bloodstream infection according to the type and resistance of pathogen.
ICU, intensive care unit; MDR, Multi-drug resistance includes Methicillin resistant S.aureus, Vancomycin resistant E.faecalis and E.faecium, and multidrug resistance defined as a resistance to at least 3 antibiotic groups for P.aeruginosa, Acinetobacter spp., Enterobacter spp., E.coli, S.maltophilia, Klebsiella spp. and/or the resistance mechanisms ESBL for Klebsiella spp. and E.coli; Non-MDR, includes Vancomycin sensible Enterococcus spp., Methicillin sensible S. aureus and non-multi-drug resistance for E. coli, Klebsiella spp., Enterobacter spp., P. aeruginosa, Acinetobacter spp., S. maltophilia; Whiskers represent 95% confidence interval.
Table 3 and Fig 3 show the results of the multivariable analysis for ICU mortality following PBSI of various pathogens compared to S.aureus. Adjusted by gender, age group and the type of ICU, Enterococci, E.coli, C.albicans and Non-albicans Candida spp., S. maltophilia and P.aeruginosa were associated with higher mortality compared to S.aureus; CNS with lower mortality respectively.
Table 3. Results of multivariable analysis for mortality in intensive care units (ICU) following mono-microbial primary bloodstream infection (PBSI) according to type of organism and further risk factors and confounders, ICU-KISS, 2006–2015.
| Parameter | Category | AOR | 95%CI | p-value |
|---|---|---|---|---|
| Type of organism | Coagulase negative staphylococci | 0.86 | 0.75–0.99 | 0.030 |
| Enterococcus spp. | 1.20 | 1.06–1.36 | 0.005 | |
| Candida albicans | 1.37 | 1.16–1.61 | <.0001 | |
| E. coli | 1.24 | 1.02–1.49 | 0.029 | |
| Klebsiella spp. | 0.97 | 0.81–1.17 | 0.780 | |
| Enterobacter spp. | 0.93 | 0.74–1.18 | 0.556 | |
| P. aeruginosa | 1.49 | 1.21–1.84 | <.0001 | |
| non-albicans-Candida spp. | 1.49 | 1.18–1.88 | 0.001 | |
| Serratia spp. | 0.74 | 0.52–1.06 | 0.105 | |
| Acinetobacter spp. | 1.22 | 0.86–1.74 | 0.262 | |
| Proteus spp. | 0.77 | 0.46–1.3 | 0.324 | |
| S. maltophilia | 1.71 | 1.19–2.47 | 0.004 | |
| S. aureus | 1 = reference | |||
| Gender | Male | 0.92 | 0.86–1 | 0.042 |
| Female | 1 = reference | |||
| Age group | ≤45 years | 0.46 | 0.4–0.52 | <.0001 |
| 46–55 years | 0.70 | 0.62–0.78 | <.0001 | |
| 56–65 years | 0.79 | 0.72–0.86 | <.0001 | |
| >65 years | 1 = reference | |||
| Type of ICU | Medical | 1.12 | 0.95–1.32 | 0.161 |
| Surgical | 0.89 | 0.77–1.02 | 0.101 | |
| Neurosurgical | 0.44 | 0.27–0.72 | 0.001 | |
| Cardiosurgical | 1.48 | 1.18–1.85 | 0.001 | |
| Neurological | 0.52 | 0.39–0.71 | <.0001 | |
| Paediatric | 0.55 | 0.38–0.8 | 0.002 | |
| Other a | 1.02 | 0.8–1.3 | 0.887 | |
| Interdisciplinary | 1 = reference |
The multivariable analysis was performed using logistic regression analysis they were based on generalized estimating equation (GEE) models which account for this clustering effect by using an exchangeable correlation structure.
AOR, adjusted odds ratio; CI, confidence interval; ICU, intensive care unit.
a other than Medical-surgical, Surgical, Medical, Cardiothoracic, Neurosurgical, Neurological or Pediatric.
Fig 3. Adjusted odds ratios (AOR) for ICU mortality in patients with ICU-acquired primary bloodstream infections according to the type of pathogen.
ICU, intensive care unit; CNS, coagulase negative staphylococci; Whiskers represent 95% confidence interval; S. aureus was set as reference.
Table 4 shows the results of the multivariable analysis for mortality following PBSI stratified by pathogen groups (gram-positive, gram-negative bacteria and fungi) and table 5 by multi-drug resistance groups (non-multi-drug resistant/multi-drug resistant).
Table 4. Results of multivariable analysis for mortality in intensive care units (ICU) following mono-microbial primary bloodstream infection (PBSI) according to group of organisms, ICU-KISS, 2006–2015.
| Parameter | Category | OR | 95%CI | p-value |
|---|---|---|---|---|
| Group of organisms | Gram-negative a | 1.12 | 1.01–1.23 | 0.024 |
| Fungi b | 1.42 | 1.25–1.62 | <.0001 | |
| Gram-positive c | 1 = reference | |||
| Gender | Male | 0.92 | 0.85–0.99 | 0.036 |
| Female | 1 = reference | |||
| Age group | ≤45 years | 0.45 | 0.4–0.52 | <.0001 |
| 46–55 years | 0.70 | 0.62–0.78 | <.0001 | |
| 56–65 years | 0.79 | 0.72–0.86 | <.0001 | |
| >65 years | 1 = reference | |||
| Type of ICU | Medical | 1.15 | 0.98–1.35 | 0.085 |
| Surgical | 0.89 | 0.77–1.02 | 0.102 | |
| Neurosurgical | 0.43 | 0.26–0.69 | 0.001 | |
| Cardiosurgical | 1.45 | 1.16–1.83 | 0.001 | |
| Neurological | 0.52 | 0.39–0.7 | <.0001 | |
| Paediatric | 0.53 | 0.36–0.77 | 0.001 | |
| Other d | 1.05 | 0.82–1.34 | 0.708 | |
| Interdisciplinary | 1 = reference |
The multivariable analysis was performed using logistic regression analysis they were based on generalized estimating equation (GEE) models which account for this clustering effect by using an exchangeable correlation structure
OR, odds ratio; CI, confidence interval
Model is adjusted by age, sex and type of ICU
a includes E. coli, Klebsiella spp., Enterobacter spp., P. aeruginosa, Serratia spp., Acinetobacter spp., Proteus spp., and S. maltophilia.
b includes C. albicans, non-albicans-Candida spp.
c includes coagulase negative Staphylococci, Enterococcus spp., S. aureus;
d other than Medical-surgical, Surgical, Medical, Cardiothoracic, Neurosurgical, Neurological or Pediatric.
Table 5. Results of multivariable analysis for mortality in intensive care units (ICU) following mono-microbial primary bloodstream infection (PBSI) according to multidrug resistance groups, ICU-KISS, 2006–2015.
| Parameter | Category | OR | 95%CI | p-value |
|---|---|---|---|---|
| Multi-drug (MDR) resistance groups | MDR a | 1.36 | 1.21–1.52 | <.0001 |
| Non-MDR b | 1 = reference | |||
| Gender | Male | 0.91 | 0.84–0.98 | 0.017 |
| Female | 1.00 | 1–1 | 0.000 | |
| Age group | ≤45 years | 0.46 | 0.4–0.52 | <.0001 |
| 46–55 years | 0.70 | 0.63–0.78 | <.0001 | |
| 56–65 years | 0.79 | 0.72–0.86 | <.0001 | |
| >65 years | 1 = reference | |||
| Type of ICU | Medical | 1.15 | 0.98–1.35 | 0.097 |
| Surgical | 0.92 | 0.8–1.06 | 0.236 | |
| Neurosurgical | 0.43 | 0.27–0.7 | 0.001 | |
| Cardiosurgical | 1.48 | 1.16–1.89 | 0.002 | |
| Neurological | 0.52 | 0.38–0.71 | <.0001 | |
| Paediatric | 0.54 | 0.38–0.79 | 0.001 | |
| Other c | 1.07 | 0.83–1.38 | 0.615 | |
| Interdisciplinary | 1 = reference |
The multivariable analysis was performed using logistic regression analysis they were based on generalized estimating equation (GEE) models which account for this clustering effect by using an exchangeable correlation structure
OR, odds ratio; CI, confidence interval
Model is adjusted by age, sex and type of ICU
a MDR, Multi-drug resistance includes Methicillin resistant S.aureus, Vancomycin resistant E.faecalis and E.faecium, and multidrug resistance defined as a resistance to at least 3 antibiotic groups for P.aeruginosa, Acinetobacter spp., Enterobacter spp., E.coli, S.maltophilia, Klebsiella spp. and/or the resistance mechanisms ESBL for Klebsiella spp. and E.coli
b Non-MDR, includes Vancomycin sensible Enterococcus spp., Methicillin sensible S. aureus and non-multi-drug resistance for E. coli, Klebsiella spp., Enterobacter spp., P. aeruginosa, Acinetobacter spp., S. maltophilia
c other than Medical-surgical, Surgical, Medical, Cardiothoracic, Neurosurgical, Neurological or Pediatric.
Discussion
The present study evaluated ICU mortality after PBSI in relation to various types of pathogen in a large cohort of more than 4.5 Mio ICU patients. PBSI with Enterococci, E.coli, C.albicans and Non-albicans Candida spp., S. maltophilia and P.aeruginosa were associated with higher ICU mortality compared to S.aureus, CNS were associated with significant lower ICU mortality.
The significantly higher ICU mortality rates following PBSI with E.coli and Enterococci have not been previously described and seem to be particularly interesting. Only a recent article by Ong et al. also associated enterococci PBSI with significantly higher mortality rates [7]. These authors used data from two ICUs in the Netherlands, considered ICU discharge and death as competing events. The occurrence of enterococcal bacteremia (not only PBSI) was fitted as a time time-dependent variable. The authors of this study argue that the high risk of death following entercoccal bacteremia may be a marker of impending complications that carry high risk of death in the ICU rather than being causes of death on their own. For instance, the higher mortality in Enterococci PBSI (and also E.coli) may originate in translocation from the digestive tract of patients in unstable hemodynamic conditions, such as during shock or the support of ECMO. The higher mortality of E.coli cannot be explained by the percentage of multi-drug resistant E.coli. (ICU mortality non-MDR E.coli 20.9, mortality MDR-E.coli 31.3).
Our results confirm findings from earlier studies concerning Candida spp. and P.aeruginosa which are known for a high mortality. In the past, Candida spp. was often described as leading to higher mortality. In an analysis of more than 6000 patients with BSI, Shorr et al. demonstrated that fungal organisms were associated with the highest mortality [14]. In a review, the same authors described infections caused by mixed resistant Gram-negative bacteria, extended-spectrum beta-lactamase-producing Enterobacteriaceae, multi-drug resistant Pseudomonas aeruginosa, and Acinetobacter species as being generally associated with increased mortality [1]. Lambert et al. described a very high mortality rate following P.aeruginosa PBSI in European ICU patients [5]. A recent cohort study from North Carolina reported that P.aeruginosa remained significantly associated with increased mortality following BSI relative to S.aureus and other gram-negative bacteria (Hazard ratio 1.43, p = 0.02) [15]. In another study from US hospitals that focused on severe sepsis, anaerobes and Methicillin-resistant S.aureus were significant predictors of mortality whereas Gram-negative bacteria had decreased mortality hazards [3].
According to a recent study with data from more than 600,000 in patients from 10 European hospitals, which focussed on all BSI due to S.aureus and Enterobacteriaceae and also considered competing risks, S.aureus had a greater impact on mortality than Enterobacteriacae. However, the authors pooled the data for all Enterobacteriacae and did not focus individual species such as E.coli [8]. In our study E.coli mortality was higher than Klebsiella spp., Enterobacter spp., Proteus spp. and Serratia spp..
Many authors have compared the mortality rates of the susceptible and resistant variants of the pathogens causing infections [5, 16–19]. We also tried to show the differences between the two groups of pathogens. But we must point out that we were not able to adjust for underlying diseases which seem to be a very important risk factor for multi-drug resistant bacteria. Only the time, from admission until onset of infection, could be considered, which may be a surrogate parameter for severity of illness. This is one of the most important limitations of our analysis. For example PBSI with S.maltophilia occur after a long stay on ICU (Median 19 days). However, the time to BSI was not significant in the multivariable analysis.
Our analysis has further limitations. First, our analysis only represents ICU mortality following ICU-acquired primary BSI. No BSI within the first three days on ICU or secondary BSI are included. Second, autopsies are very rarely performed in German ICUs, thus also precluding confirmation of a direct relationship between mortality and PBSI. Third, only mortality in the ICU was observed, but not during subsequent hospital stays. Fourth, it is impossible to provide information about the sensitivity of recording the death of the patients, but due to the use of web-based surveillance systems, the surveillance staff cannot complete an infection case without entering this information. Fifth, the analysis concentrates only on mono-microbial infections; mortality following poly-microbial infections was significantly higher. Sixthly, usually the time to event has been used to account for the risk of death, but because the time to the event “death” was not available for infected patients, such an analysis was not possible. Finally, the database does not include any information about the underlying diseases of the patients and empirical antimicrobial therapy (substances and the timing of antibiotics). Therefore, adjustment related to inappropriate initial antimicrobial therapy is impossible.
Conclusion
In summary, out data shows substantial differences in mortality in German ICUs according to the type of pathogen. Considering the aggressive nature of the pathogens identified with significantly higher mortality rates, information on the type of pathogen is itself important for the prognosis of patients. Therefore, taking blood cultures is important and their results should be provided to clinicians as soon as possible.
Acknowledgments
Data have been generated as part of the routine work of the nosocomial hospital infection surveillance system (KISS). Special thanks to the healthcare staff and the infection control personnel of all ICU-KISS units for their participation, their support of the surveillance project. A part of this study was presented at the congress Sepsis Update in Weimar, Germany 2015.
Data Availability
Data is available from the German National Reference Center for Surveillance of Nosocomial Infections Data Access Committee for researchers who meet the criteria for access to confidential data and agree to be bound by a non disclosure agreement regarding the publication of unaggregated data. The data is collected according to German laws and the National Reference Center for Surveillance of Nosocomial Infections is bound by a non disclosure agreement with the hospitals participating in the system. We are not allowed to publish unaggregated data which might lead to identification of individual hospitals directly or through a third party. Researchers who want to obtain the data set required to reproduce our findings are asked to direct their request to: Data Access Committee Nationales Referenzzentrum (NRZ) für Surveillance von nosokomialen Infektionen am Institut für Hygiene und Umweltmedizin Charité-Universitätsmedizin Berlin (nrz@charite.de).
Funding Statement
The authors are members of the German national reference center for surveillance of nosocomial infections which is funded by the governmental Robert-Koch-Institut (http://www.rki.de/DE/Content/Infekt/NRZ/nrz_node.html). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. However besides the general funding of the national reference center which enables it to serve its mission of promoting surveillance of nosocomial infections in German hospitals the authors received no specific funding for this work.
References
- 1.Shorr A. Review of studies of the impact on Gram-negative bacterial resistance on outcomes in the intensive care unit. Crit Care Med. 2009;37:1463–39. doi: 10.1097/CCM.0b013e31819ced02 [DOI] [PubMed] [Google Scholar]
- 2.Lemos E, de la Hoz F, Einarson T, McGhan W, Quevedo E, Castañeda C, et al. Carbapenem resistance and mortality in patients with Acinetobacter baumannii infection: systematic review and meta-analysis. Clin Microbiol Infect 2014;20:416–23. doi: 10.1111/1469-0691.12363 [DOI] [PubMed] [Google Scholar]
- 3.Ani C, Farshidpanah S, Bellinghausen Stewart A, Nguyen H. Variations in organism-specific severe sepsis mortality in the United States: 1999–2008. Crit Care Med. 2015;43:65–77. doi: 10.1097/CCM.0000000000000555 [DOI] [PubMed] [Google Scholar]
- 4.Prowle J, Echeverri J, Ligabo E, Sherry N, Taori G, Crozier T, et al. Acquired bloodstream infection in the intensive care unit: incidence and attributable mortality. Crit Care. 2011;15(2):R100 doi: 10.1186/cc10114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lambert M, Suetens C, Savey A, Palomar M, Hiesmayr M, Morales I, et al. Clinical outcomes of health-care-associated infections and antimicrobial resistance in patients admitted to European intensive-care units: a cohort study. Lancet Infect Dis 2011;11:30–8. doi: 10.1016/S1473-3099(10)70258-9 [DOI] [PubMed] [Google Scholar]
- 6.Gastmeier P, Sohr D, Geffers C, Behnke M, Rüden H. Risk factors for death due to nosocomial infection in intensive care unit patients: Findings from the Krankenhaus Infektions Surveillance System. Infect Control Hosp Epidemiol. 2007;28:466–72. doi: 10.1086/510810 [DOI] [PubMed] [Google Scholar]
- 7.Ong D, Bonten M, Safdari K, Spitoni C, Frencken J, Witteveen E, et al. Epdemiology, Management, and risk-adjusted mortality of iCU acquired enteococcal bacteremia. Clin Infect Dis. 2015;July, pii:civ560. [DOI] [PubMed] [Google Scholar]
- 8.Stewardson A, Allignol A, Beyersmann J, Graves N, Schumacher M, Meyer R, et al. The health and economic burden of bloodstream infections caused by antimicrobial-susceptible and non-susceptible Enterobacteriaceae and Staphylococcus aureus in European hospitals, 2010 and 2011: a multicentre retrospective cohort study. Euro Surveill. 2016;August 18;21(33). doi: 10.2807/1560-7917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gastmeier P, Schwab F, Sohr D, Behnke M, Geffers C. Reproducibility of the surveillance effect to decrease nosocomal infection rates. Infect Control Hosp Epidemiol 2009;30:993–99. doi: 10.1086/605720 [DOI] [PubMed] [Google Scholar]
- 10.Horan T, Emori T. Definitions of nosocomial infections In: Abrutyn E, editor. Saunders Infection Control Reference service. Philadelphia: W.B. Saunders Company; 1998. p. 17–21. [Google Scholar]
- 11.Horan T, Andrus M, Dudeck M. CDC/NHSN surveillance definition of healthcare-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36:309–32. doi: 10.1016/j.ajic.2008.03.002 [DOI] [PubMed] [Google Scholar]
- 12.Paulsen J, Solligård E, Damås J, DeWan A, Åsvold B, Bracken M. The Impact of Infectious Disease Specialist Consultation for Staphylococcus aureus Bloodstream Infections: A Systematic Review. Open Forum Infect Dis. 2016;March 1;3(2):ofw048 doi: 10.1093/ofid/ofw048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vogel M, Schmitz R, Hagel S, Pletz M, Gagelmann N, Scherag A, et al. Infectious disease consultation for Staphylococcus aureus bacteremia—A systematic review and meta-analysis. J Infect. 2016;72:19–28. doi: 10.1016/j.jinf.2015.09.037 [DOI] [PubMed] [Google Scholar]
- 14.Shorr A, Tabak Y, Killian A, Gupta V, Liu L, Kollef M. Healthcare-associated bloodstream infection: A distinct entity? Insights from a large U.S. database. Crit Care Med. 2006;34:2588–95. doi: 10.1097/01.CCM.0000239121.09533.09 [DOI] [PubMed] [Google Scholar]
- 15.Thaden J, Park L, Maskarinec S, Ruffin F, Fowler VJ, van Duin D. Results from a 13-Year Prospective Cohort Study Show Increased Mortality Associated with Bloodstream Infections Caused by Pseudomonas aeruginosa Compared to Other Bacteria. Antimicrob Agents Chemother. 2017;61:e02671–16. doi: 10.1128/AAC.02671-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Kraker M, Wolkewitz M, Davey P, Koller W, Berger J, Nagler J, et al. Burden of antimicrobial resistance in European hospitals: excess mortality and length of hospital stay associated with bloodstream infections due to Escherichia coli resistant to third-generation cephalosporins. J Anitimicrob Chemother. 2011;66:398–407. [DOI] [PubMed] [Google Scholar]
- 17.de Kraker M, Wolkewitz M, Davey P, Grundmann H, on behalf of the BURDEN study group. Clinical impact of antimicrobial resistance in Eurpean Hospitals: Excess mortality and length of hospital stay related to Methicillin-resistant Staphylococcus aureus bloodstream infections. Antimicrob Agents Chemother. 2011;55:1598–05. doi: 10.1128/AAC.01157-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barrasa-Villar J, Aibar-Remón C, Prieto-Andrés P, Mareca-Doñate R, Moliner-Lahoz J. Impact on morbidity, mortality and length of stay of hospital acquired infections by resistant microorganisms. Clin Infect Dis. 2017;65:644–52. doi: 10.1093/cid/cix411 [DOI] [PubMed] [Google Scholar]
- 19.Adrie C, Garrouste-Orgeas M, Ibn Essaied W, Schwebel C, Darmon M, Mourvillier B, et al. Attributable mortality of ICU-acquired bloodstream infections: Impact of the source, causative micro-organism, resistance profile and antimicrobial therapy. J Infect. 2017;74:131–41. doi: 10.1016/j.jinf.2016.11.001 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is available from the German National Reference Center for Surveillance of Nosocomial Infections Data Access Committee for researchers who meet the criteria for access to confidential data and agree to be bound by a non disclosure agreement regarding the publication of unaggregated data. The data is collected according to German laws and the National Reference Center for Surveillance of Nosocomial Infections is bound by a non disclosure agreement with the hospitals participating in the system. We are not allowed to publish unaggregated data which might lead to identification of individual hospitals directly or through a third party. Researchers who want to obtain the data set required to reproduce our findings are asked to direct their request to: Data Access Committee Nationales Referenzzentrum (NRZ) für Surveillance von nosokomialen Infektionen am Institut für Hygiene und Umweltmedizin Charité-Universitätsmedizin Berlin (nrz@charite.de).