Abstract
This longitudinal study examined whether post-transplant cancer survivors (N = 254, 9 months to 3 years after stem cell transplant treatment) with greater personal resilience resources demonstrated better psychological outcomes and whether this could be attributed to reductions in depressive symptoms and/or four meaning-making processes (searching for and finding reasons for one’s illness; searching for and finding benefit from illness). Hierarchical linear regression analyses examined associations of survivors’ baseline personal resilience resources (composite variable of self-esteem, mastery, and optimism), which occurred an average of 1.7 years after transplant, and 4-month changes in psychological outcomes highly relevant to recovering from this difficult and potentially traumatic treatment: post-traumatic stress disorder (PTSD) symptoms and purpose in life. Boot-strapped analyses tested mediation. Greater personal resilience resources predicted decreases in PTSD stress symptoms (b = −0.07, p = 0.005), mediated by reductions in depressive symptoms (b = −0.01, 95% CI: −0.027, −0.003) and in searching for a reason for one’s illness (b = −0.01, 95% CI: −0.034, −0.0003). In addition, greater resilience resources predicted increases in purpose in life (b = 0.10, p < 0.001), mediated by reductions in depressive symptoms (b = 0.02, 95% CI: 0.003, 0.033). Having greater personal resilience resources may promote better psychological adjustment after a difficult cancer treatment, largely because of improvements in depressive symptoms, although decreased use of a potentially maladaptive form of meaning-making (searching for a reason for one’s illness) was also important for reducing PTSD symptoms.
Keywords: resilience, meaning-making, depressive symptoms, cancer survivorship, hematopoietic stem cell transplant
Cancer survivors experience substantial physical and emotional challenges as a result of their diagnosis and treatment, which can negatively impact their quality of life (Mosher, Redd, Rini, Burkhalter, & DuHamel, 2009). This is particularly true for those treated with hematopoietic stem cell transplant (SCT)—a toxic, intensive treatment that involves high-dose chemotherapy and, for some, total body irradiation (Giralt & Bishop, 2009; Mohty & Mohty, 2011; Mosher et al., 2009). Although often lifesaving, it causes considerable psychological and physical morbidity in addition to conferring risk of death over and above the diseases it treats (Copelan, 2006; Giralt & Bishop, 2009; Syrjala et al., 2004) and is experienced by many survivors as a traumatic event (DuHamel et al., 2004; Jacobsen et al., 1998). Likewise, an estimated 5–28% of transplant survivors experience post-traumatic stress disorder (PTSD) symptoms including intrusive thoughts and feelings, and avoiding reminders of their illness experience (El-Jawahri et al., 2015; Jacobsen et al., 2002; Mosher et al., 2009; Smith, Redd, DuHamel, Vickberg, & Ricketts, 1999; Widows, Jacobsen, & Fields, 2000).
Stem cell transplant can also adversely affect survivors’ sense of purpose in life (Curbow, Legro, Baker, Wingard, & Somerfield, 1993) by disrupting valued activities and goals that provided a sense of direction in their life (Ryff & Singer, 1998; Scheier et al., 2006). Having a sense of purpose in life plays an important role in well-being and is associated with reduced morbidity and mortality, and increased adherence to health-promoting behaviors (Cohen, Bavishi, & Rozanski, 2015; Kim, Strecher, & Ryff, 2014). Therefore, survivors’ ability to remain engaged with valued activities and goals that contribute to their purpose in life (or to establish alternatives if old ones become unattainable) may determine whether they are able to successfully resume life as normal as possible after treatment (Carver, Lehman, & Antoni, 2003; Wrosch & Scheier, 2003).
Personal resilience resources
Although it is clear that the transplant experience can result in PTSD symptoms and disrupt survivors’ sense of purpose in life, there is variability in psychological adjustment after treatment, with some survivors adjusting better than others (Syrjala et al., 2004; Widows, Jacobsen, Booth-Jones, & Fields, 2005). One factor that may be contributing to this variability is resilience, the capacity to maintain or recover well-being in the face of adversity (Dunkel-Schetter & Dolbier, 2011; Rutter, 2006; Ryff & Singer, 1998; Stewart & Yuen, 2011). The present study focused on resilience characteristics or “personal resilience resources” of optimism, self-esteem, and mastery, which have been studied together in chronically ill populations (Schwabish, 2011; Stewart & Yuen, 2011). Together, these stable, dispositional characteristics indicate the extent to which individuals hold generally positive beliefs about the future, themselves, and their ability to exercise control over important outcomes (Benight & Bandura, 2004; Dunkel-Schetter & Dolbier, 2011; Scheier & Carver, 1992) and would be an important resource for coping with the SCT experience. Cross-sectional studies demonstrate an inverse relationship between cancer survivors’ personal resilience resources and PTSD symptoms (Schwabish, 2011). Resilience characteristics, assessed before SCT, also predict emotional and physical well-being, and less situational avoidant coping 1-year post-SCT (Hochhausen et al., 2007; Schoen, Altmaier, & Tallman, 2007) and post-traumatic growth 9-years post-SCT (Tallman, Shaw, Schultz, & Altmaier, 2010). In addition, more resilient survivors experience fewer illness-related disruptions in activities that provide a sense of purpose, or they are able to redirect attention to alternative activities and more attainable goals (Carver et al., 2003; Wrosch & Scheier, 2003).
However, research is lacking on the mechanisms through which having greater personal resilience resources may lead to better psychological adjustment. When facing a threatening event, individuals may engage in a tripartite of coping behaviors: Eliminate or change the event itself, find meaning in the event, or manage distress associated with the event (Pearlin & Schooler, 1978; Taylor, 1983). In the context of SCT, survivors’ illness and treatment are events that are not amenable to change; however, it is possible to cope by finding meaning in their experience and managing their distress, both of which are associated with resilience and better adjustment after trauma (Adelstein, Anderson, & Taylor, 2014; Loberiza et al., 2002; Park & Folkman, 1997; Thompson & Pitts, 1993).
Potential pathways: Meaning-making and depressive symptoms
Meaning-making
A traumatic event challenges individuals’ core goals and fundamental assumptions about the self and the world (Janoff-Bulman, 1992; Park & Folkman, 1997). According to the meaning-making model, searching for and then finding meaning that helps integrate the event’s meaning with adaptive global views (e.g., bad things can happen to good people) results in better psychological adjustment after a potentially traumatic event (Park, 2010; Park & Folkman, 1997). Personal resilience resources may be associated with better adjustment in part because of their potential to facilitate finding meaning. Survivors with these resources may attribute meaning to their illness experience that is consistent with their positive global views reflecting self-worth, confidence in their ability to cope, and positive future expectations (Benight & Bandura, 2004; Carver & Scheier, 2014; Dunkel-Schetter & Dolbier, 2011; Park & Folkman, 1997). Furthermore, they may seek two types of meaning that are independently associated with adjustment: (1) To understand what has happened (e.g., find a reason for their illness) and (2) to identify benefits from the experience (Davis, Nolen-Hoeksema, & Larson, 1998; Taylor, 1983). Attempts to find meaning in these ways are consistent with more resilient individuals’ tendency to attend to important negative health information, rather than using denial or avoidance (Aspinwall & MacNamara, 2005), and to cope through positive reframing and benefit finding (Carver et al., 1993; Nes & Segerstrom, 2006).
One caveat is that prolonged unsuccessful searching for meaning has been theorized to be maladaptive (Adelstein et al., 2014; Park & Folkman, 1997; Tomich & Helgeson, 2002), and this may differ for these two types of meaning (i.e., reason for their illness and identifying benefits from illness) (Davis et al., 1998). In both long-term breast cancer survivors (≥ 5 years post-treatment) and healthy women, a continued search for meaning to understand or make sense of the most stressful event occurring 5 years ago was associated with poor quality of life (Tomich & Helgeson, 2002). Searching for this type of meaning may initially promote beneficial cognitive processing; however, if not found, prolonged searching can evolve into intrusive thoughts that must be managed with corresponding attempts to avoid reminders about the event (i.e., PTSD symptoms) (Horowitz, Wilner, & Alvarez, 1979; Park, 2010). Given the complexities of illnesses requiring SCT, it may be more difficult for survivors to find meaning to understand their illness. Therefore, discontinuing an unsuccessful search may be associated with better adjustment or psychological outcomes (Wrosch & Scheier, 2003). More resilient survivors may be more likely to discontinue an unsuccessful search for this type of meaning, than their less resilient counterparts, because of their tendency to disengage from unattainable goals (Aspinwall & Richter, 1999; Wrosch & Scheier, 2003).
On the other hand, research that has examined searching for benefit in a stressful event suggests that searching for this type of meaning closer to the event may reflect an illusory cognitive strategy to reduce distress, whereas searching for benefit further away from the event may reflect actual positive growth (Helgeson, Reynolds, & Tomich, 2006; Tomich & Helgeson, 2002, 2004). Considering that finding benefit from stressful experiences is consistent with resilient individuals’ positive global views (Carver & Antoni, 2004; Rini et al., 2004), they may be more likely than their less resilient counterparts to engage in this type of meaning, regardless of time since event, and be associated with positive outcomes. In light of these findings, we explored both searching for a reason for the illness and for benefits in the illness experience, and having found these two types of meaning as potential mechanisms underlying the association between having greater resilience resources and adjustment after SCT.
Depressive symptoms
The second potential mechanism we investigated was depressive symptoms. An estimated 26–36% of SCT survivors report depressive symptoms, which is important considering its associations with increased mortality and reductions in quality of life (Artherholt, Hong, Berry, & Fann, 2014; Kenzik, Huang, Rizzo, Shenkman, & Wingard, 2015; Loberiza et al., 2002; Mosher et al., 2009; Syrjala et al., 2004). Furthermore, depressive symptoms can persist even after recovery of physical functioning following SCT (Syrjala et al., 2004).
More resilient SCT survivors have lower depressive symptoms (Baker, Marcellus, Zabora, Polland, & Jodrey, 1997; Min et al., 2013), perhaps because they are better able than their counterparts to effectively manage negative emotions (e.g., through active rather than avoidant coping) (Carver et al., 1993; Nes & Segerstrom, 2006; Schoen et al., 2007). In turn, this should promote better psychological adjustment after SCT, such as no longer experiencing it as a traumatic event and re-establishing a sense of purpose in life (Carver, 2005; El-Jawahri et al., 2015; Scheier et al., 2006; Wrosch & Scheier, 2003). Furthermore, although depressive and PTSD symptoms may co-occur, studies have demonstrated that depressive symptoms can lead to PTSD symptoms (Schindel-Allon, Aderka, Shahar, Stein, & Gilboa-Schechtman, 2010). For instance, a longitudinal study with SCT patients demonstrated that increases in depressive symptoms during SCT hospitalization prospectively predicted PTSD symptoms 6 months later (El-Jawahri et al., 2015).
Present study
The present study was a secondary analysis of a longitudinal study with post-SCT cancer survivors to examine the role of personal resilience resources in psychological adjustment during the survivorship period after transplant and the potential mechanisms of this association. First, we hypothesized that having greater personal resilience resources would be associated with increases in a sense of purpose in life and decreases in PTSD symptoms from baseline (i.e., assessed at an average of 1.7 years after SCT) to 4 months later. Second, we hypothesized that the association of personal resilience resources with these outcomes would be at least partially mediated by: (1) decreases in depressive symptoms and/or (2) survivors’ reports of having found meaning (vs. continuing to search for meaning). In particular, we examined whether this meaning-making would differ for more resilient survivors according to two types of meaning: Searching for and/or finding a reason for their illness and searching for and/or finding benefits from the illness experience.
Methods
Participants
Participants were from a randomized controlled trial evaluating a psychosocial intervention for post-transplant survivors who were 9 months to 3 years after SCT (Rini et al., 2014). Participants in this parent study were English-speaking adults who had successfully completed their SCT treatment (i.e., without relapse or transplant failure) and who had been screened for having at least mild survivorship problems, according to published cutoffs or study findings, in one or more of four domains: general distress (Derogatis & Spencer, 1993), transplant-specific distress (Horowitz et al., 1979), poor health-related quality of life (McQuellon et al., 1997), or low purpose in life (Scheier et al., 2006) (see Rini et al., 2014 for details). The present study’s sample included participants who provided baseline (assessed prior to randomization in the parent study) and follow-up (assessed 4 months after baseline) data on the variables of interest. The participants were older (p < 0.001; 54.8 years vs. 49.0 years) and had higher optimism scores at baseline (p = 0.01) than excluded participants but were similar on remaining sociodemographics, other resilience characteristics (self-esteem, mastery), and dependent variables (PTSD symptoms, purpose in life).
Measures
Personal resilience resources
Optimism, self-esteem, and mastery were assessed at baseline pre-randomization in the parent study. Optimism was assessed with the 10-item Life Orientation Test-Revised (Scheier, Carver, & Bridges, 1994), which uses a response scale from 0 (strongly disagree) to 4 (strongly agree). Self-esteem was assessed with the 10-item Rosenberg Self-Esteem Scale (Rosenberg, 1965), which measures global sense of self-worth using a response scale from 1 (strongly disagree) to 4 (strongly agree). Mastery was assessed with the seven-item Mastery Scale (Pearlin & Schooler, 1978), which measures the extent to which people perceive that valued outcomes are under their control using a response scale from 1 (strongly disagree) to 4 (strongly agree). Higher scores on these scales indicate greater resources. Internal reliability was good for all three (Cronbach α of 0.77, 0.87, and 0.76, respectively). For our independent variable, scores on these measures were standardized and summed to create a personal resilience resources composite variable.
Meaning-making
Meaning-making was assessed with four face-validated items from prior research (Wu et al., 2008) administered at baseline and at follow-up for four meaning-making variables: searching for and having found a reason for my illness, and searching for and having found benefits of the illness. Using a response scale from 1 (strongly disagree) to 5 (strongly agree), participants reported the extent to which they disagreed or agreed with statements indicating that they were searching for and had found a reason for their illness (“I have been trying to find a reason or explanation for why I got sick” and “I have been able to find a reason or explanation for why I got sick”), and the extent to which they were searching for and had found benefits of the illness (“When I think of my illness I have been looking for positive things that have come out of it for me or my family” and “When I think of my illness I have been able to find positive things that have come out of it for me or my family”). Although the scale’s instructions did not specify a time frame, we believe that participants likely responded in a way that reflected how they felt at that moment. Higher scores on each of the four meaning-making variables indicate stronger endorsement of searching for or having found meaning (i.e., reason for my illness or benefits from the illness).
Depressive symptoms
Depressive symptoms were assessed at baseline and follow-up with the six-item depression subscale of the 53-item Brief Symptom Inventory (Derogatis & Spencer, 1993), using a five-point scale from 0 (not at all) to 4 (extremely). Higher scores indicate greater depressive symptoms. Internal reliability was good (baseline α = 0.84, follow-up α = 0.87).
PTSD symptoms
Post-traumatic stress disorder symptoms were assessed at baseline and follow-up with the 15-item Impact of Events Scale (Horowitz et al., 1979), which measures intrusion and avoidance using a scale of 0 (not at all), 1 (rarely), 3 (sometimes), and 5 (often). In this study, the reference event was participants’ illness and transplant. Higher scores indicate greater PTSD symptoms. Internal reliability was good (baseline α = 0.88, follow-up α = 0.87).
Purpose in life
The six-item Life Engagement Test (Scheier et al., 2006) assessed purpose in life, defined as the extent to which respondents engage in valued and important activities that give their life purpose, using a scale of 1 (strongly disagree) to 5 (strongly agree). Higher scores indicate perceiving greater purpose in life. Internal reliability was good (baseline α = 0.84, follow-up α = 0.83).
Demographic and medical characteristics
Participants’ sociodemographic (sex, age, race/ethnicity, household income, married/living as married, education, work status) and medical characteristics (allogeneic vs. autologous transplant, history of relapse, history of graft vs. host disease (GvHD), number of non-GvHD transplant complications, and number of medical comorbidities) were collected at baseline through self-report and clinical records.
Procedure
During 2008–2011, post-transplant cancer survivors were recruited for the parent study through patient databases at two medical centers in the northeastern USA or through announcements in transplant or illness-related websites and newsletters. After a telephone screening interview, eligible participants provided informed consent and completed the baseline assessment (a phone interview and mailed questionnaire) 1 week later. The intervention began 1 week after baseline; participants wrote about their transplant experience in four guided brief writing sessions over 4 weeks, using writing instructions specific to their assigned study group. The instructions included a control group that wrote about facts of their transplant or, for the other three groups, different combinations of writing for themselves and/or writing to share their experiences with fellow patients. The follow-up assessment (a phone interview and mailed questionnaire) was completed 3-months postintervention (4 months after baseline). We controlled for the intervention groups in the present study’s analyses. Additional intervention details and its results can be found in the main publication (Rini et al., 2014). All study procedures were approved by the study sites’ institutional review boards.
Data analyses
Data were examined for outliers and missing data, and assumptions for normality and homogeneity of variance and nonmulticollinearity among the variables were confirmed. Variables had minimal missing data, with three or fewer participants’ missing data on any one variable; therefore, mean imputation was used to replace these values. Descriptive analyses using categorical variables were used to examine the percentage of participants reporting searching for meaning and having found meaning at baseline and follow-up. To compute these categorical variables, a score of ≥4 (agree to strongly agree) was coded as searching for or having found meaning and a score ≤3 (neither agree nor disagree to strongly disagree) was coded as not searching for or not having found meaning. Residualized change scores for the mediators (depressive symptoms and the four continuous [nondichotomized] meaning-making variables) and the outcome variables (PTSD symptoms, purpose in life) were calculated using established procedures where follow-up scores are regressed on baseline scores, saving the standardized residual as an estimate of change over time (Prochaska, Velicer, Nigg, & Prochaska, 2008; Zumbo, 1999).
For our main analyses, two hierarchical linear regression models examined whether baseline personal resilience resources and residualized changes in depressive symptoms and the four meaning-making variables predicted residualized changes in PTSD symptoms and purpose in life. Sociodemographic and medical characteristics significantly associated (p < 0.05) with the outcome variable and three dummy variables for the RCT’s intervention arms were included as controls. Finally, bootstrap analyses examined the indirect effects involving potential mediators, using a macro developed for multiple mediation models (Preacher & Hayes, 2008). We generated 5,000 bootstrap samples to calculate 95% bias-corrected accelerated confidence intervals (BCa CI). Evidence for mediation was indicated if the 95% BCa CI’s associated with the indirect effects did not contain zero. Analyses were conducted using SPSS version 22 (IBM Corporation, New York, NY, USA).
Results
Participant descriptives
Sociodemographic and medical characteristics are presented in Table 1. 85% were non-Hispanic White, 68% were college-educated, 75% were married or living as married, and approximately 70% had an income of ≥ $65,000 (range = < $20,000 to >$110, 000). It had been an average of 88 weeks (SD = 35.01, range = 39.43–168.43 weeks) since participants had undergone SCT treatment. Age was negatively associated with changes in PTSD symptoms (r = −0.19, p = 0.003) and women had greater increases in purpose in life than men (M = 0.13, SD = 0.95 vs. M = −0.17, SD = 1.03, respectively; p = 0.02). Therefore, these variables were controlled in the relevant models. Medical characteristics were not associated with the outcome variables.
Table 1.
Demographic and medical characteristics of participants (N = 254).
| Variable | n (%) | M (SD) |
|---|---|---|
| Female | 145 (57) | |
| Age (years) | 54.82 (11.56) | |
| Non-Hispanic/White | 216 (85) | |
| Annual household income (Mdn) | $80,000–$95,000 | |
| Married/living as married | 191 (75) | |
| College degree or higher | 172 (68) | |
| Works full- or part-time | 99 (39) | |
| Transplant type | ||
| Autologous | 139 (55) | |
| Allogeneic | 115 (45) | |
| History of relapse | 93 (37) | |
| Missing | 5 (2) | |
| History of graft vs. host disease (GvHD)a | 94 (37) | |
| Number of non-GvHD SCT complications | 2.57 (1.66) | |
| Number of medical comorbidities | 1.20 (1.19) | |
SCT, stem cell transplant.
Note:
Includes acute or chronic GvHD.
Categorical variables were coded as: Gender: 1, female, 0, male; race/ethnicity: 1, non-Hispanic White, 0, non-White; married/living as married: 1, yes, 0, no; college degree or higher: 1, yes, 0, no; works fulltime or part time: 1, yes, 0, no; transplant type: 1, autologous, 2, allogeneic; history of relapse: 1, yes, 0, no; history of GvHD: 1, yes, 0, no.
Descriptive statistics
Descriptive statistics for the study variables are presented in Table 2 and the bivariate correlations among the change scores are presented in Table 3. Correlations of personal resilience resources with the potential mediators at baseline and follow-up indicated a negative association with depressive symptoms (rbaseline = −0.65, p < 0.001, rfollow-up = −0.60, p < 0.001), searching for a reason for their illness (rbaseline = −0.23, p < 0.001, rfollow-up = −0.29, p < 0.001), and having found a reason for their illness (rbaseline = −0.12, p = 0.052, rfollow-up = −0.14, p < 0.02). Having greater personal resilience resources was positively associated with searching for benefits from their illness (rbaseline = 0.15, p < 0.02, rfollow-up = 0.15, p < 0.02) and having found benefits (rbaseline = 0.25, p < 0.001, rfollow-up = 0.21, p < 0.001).
Table 2.
Study variable descriptives.
| Baseline M (SD) | Follow-up M (SD) | Change* M (SD) | |
|---|---|---|---|
| Depressive symptoms | 0.50 (0.57) | 0.49 (0.58) | −0.10 (0.39) |
| Searching for illness reason | 2.54 (1.32) | 2.34 (1.32) | −0.20 (1.07) |
| Found illness reason | 2.22 (1.23) | 2.15 (1.23) | −0.07 (1.11) |
| Searching for benefits | 3.78 (1.18) | 3.82 (1.14) | 0.04 (1.16) |
| Found benefits | 3.79 (1.17) | 3.87 (1.17) | 0.07 (1.01) |
| Post-traumatic stress disorder symptoms | 15.87 (12.74) | 14.48 (12.47) | −1.39 (9.56) |
| Purpose in life | 24.39 (4.00) | 24.92 (4.08) | 0.53 (3.82) |
| Optimisma | 18.17 (4.23) | — | — |
| Masterya | 26.43 (3.19) | — | — |
| Self-esteema | 34.74 (3.98) | — | — |
| Personal resilience resources composite scorea | 0.09 (2.53) | — | — |
Note: N = 254.
Optimism, mastery, and self-esteem at baseline were used to calculate the personal resilience resources composite score.
Follow-up–baseline.
Table 3.
Bivariate correlations among change in study variables (N = 254).
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. Personal resilience resources | — | |||||||
| 2. Δ Depressive symptoms | −0.15* | — | ||||||
| 3. Δ Searching for illness reason | −0.18** | 0.14* | — | |||||
| 4. Δ Found illness reason | −0.10 | 0.03 | 0.15* | — | ||||
| 5. Δ Searching for benefits | 0.09 | −0.12 | 0.13* | 0.03 | — | |||
| 6. Δ Found benefits | 0.07 | −0.10 | 0.01 | 0.09 | 0.61*** | — | ||
| 7. Δ Post-traumatic stress symptoms | −0.17** | 0.23*** | 0.19** | 0.04 | −0.01 | −0.07 | — | |
| 8. Δ Purpose in life | 0.25*** | −0.29*** | −0.08 | 0.02 | 0.27*** | 0.25*** | −0.06 | — |
Note. Δ, residualized change scores.
p < 0.05,
p < 0.01,
p < 0.001, two tailed.
At baseline and follow-up, a substantial proportion of participants reported searching for and having found benefits from their illness, whereas fewer reported searching for and having found a reason for their illness (Figure 1 upper panel). Half of the participants reported no change in meaning-making from baseline to follow-up, but the remainder reported increases or decreases (Figure 1 lower panel). Finally, for the study outcomes, 33% reported clinically significant improvement in PTSD symptoms and 37% reported clinically signifi-cant improvement in purpose in life over the 4-month study period, using one-third of a standard deviation as a cutoff, which has been suggested to indicate clinical significance in patient-reported data (Sloan, Cella, & Hays, 2005).
Figure 1.
Percentage of participants reporting searching for and having found types of meaning at baseline and follow-up (upper panel), and changes in meaning-making from baseline to follow-up (lower panel).
PTSD symptoms
In the hierarchical regression model for residualized changes in PTSD symptoms, age and the three dummy variables (intervention groups) were entered first, personal resilience resources were entered second, and residualized changes in depressive symptoms and in the four meaning-making variables were entered in the third step. This model explained 13% of variance for changes in PTSD symptoms (F(10, 243) = 3.71, p < 0.001). Having greater resilience resources significantly predicted decreases in PTSD symptoms (b = −0.07, p = 0.005) and its significance was reduced (p = 0.06) with the addition of depressive symptoms and the meaning-making variables (Table 4). Increases in depressive symptoms (b = 0.18, p = 0.005) and in searching for a reason for the illness (b = 0.16, p = 0.01) were independently associated with increases in PTSD symptoms. Changes in having found a reason for the illness, and searching for and having found benefits were not predictors (p’s > 0.05).
Table 4.
Hierarchical regressions for study variables predicting residualized changes in post-traumatic stress disorder symptoms (upper panel) and purpose in life (lower panel) (N = 254).
| Outcome: changes in PTSD symptoms | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Step 1 | Step 2 | Step 3 | ||||
|
|
|
|
||||
| B | SE | B | SE | B | SE | |
| Constant | 0.87 | 0.31** | 0.84 | 0.31** | 0.85 | 0.31** |
| Age | −0.02 | 0.005** | −0.02 | 0.005** | −0.02 | 0.005** |
| Dummy group 1 | 0.05 | 0.17 | 0.11 | 0.17 | 0.14 | 0.16 |
| Dummy group 2 | −0.01 | 0.17 | −0.02 | 0.17 | −0.07 | 0.17 |
| Dummy group 3 | −0.02 | 0.18 | 0.01 | 0.18 | −0.03 | 0.18 |
| Personal resilience resources | −0.07 | 0.02** | −0.05 | 0.02 | ||
| Δ Depressive symptoms | 0.18 | 0.06** | ||||
| Δ Search for reason for illness | 0.16 | 0.06* | ||||
| Δ Found reason for illness | 0.02 | 0.06 | ||||
| Δ Search for benefits in illness | 0.02 | 0.08 | ||||
| Δ Found benefits in illness | −0.05 | 0.08 | ||||
| F for full model | 3.71*** | |||||
| R2 for full model | 0.13 | |||||
| Outcome: changes in purpose in life | ||||||
|
| ||||||
| Constant | −0.21 | 0.14 | −.20 | 0.14 | −15 | 0.13 |
| Gender | 0.31 | 0.12* | 0.32 | 0.12* | 0.32 | 0.11** |
| Dummy group 1 | 0.05 | 0.17 | −0.02 | 0.17 | −0.09 | 0.16 |
| Dummy group 2 | −0.10 | 0.17 | −0.08 | 0.17 | −0.17 | 0.16 |
| Dummy group 3 | 0.23 | 0.18 | 0.17 | 0.17 | 0.12 | 0.17 |
| Resilience Resources | 0.10 | 0.02*** | 0.07 | 0.02** | ||
| Δ Depressive symptoms | −0.22 | 0.06*** | ||||
| Δ Search for reason for illness | −0.05 | 0.06 | ||||
| Δ Found reason for illness | 0.05 | 0.06 | ||||
| Δ Search for benefits in illness | 0.16 | 0.07* | ||||
| Δ Found benefits in illness | 0.11 | 0.07 | ||||
| F for full model | 7.04*** | |||||
| R2 for full model | 0.22 | |||||
Note: Personal resilience resources were assessed at baseline (after transplant). Δ, residualized change.
p < 0.05;
p < 0.01;
p < 0.001.
We next tested the indirect effects (Preacher & Hayes, 2008) of changes in depressive symptoms and searching for a reason for the illness. Age and intervention dummy variables were included as controls. The specific indirect effects test indicated that decreases in depressive symptoms (b = −0.011, 95% Bca CI: −0.034, −0.0003) and in searching for reason for the illness (b =−0.012, 95% Bca CI: −0.027, −0.003) were significant mediators. The unstandardized coefficients for the “a” paths (i.e., association between personal resilience resources and mediators) and “b” paths (i.e., association between mediators and PTSD symptoms) and the direct effect are displayed in Figure 2. Having greater personal resilience resources at baseline was associated with decreases in depressive symptoms and searching for a reason for the illness, which in turn was associated with decreases in PTSD symptoms. Personal resilience resources were not associated with changes in PTSD symptoms independent of the mediators (direct effect c′ = −0.05, p = 0.09).
Figure 2.
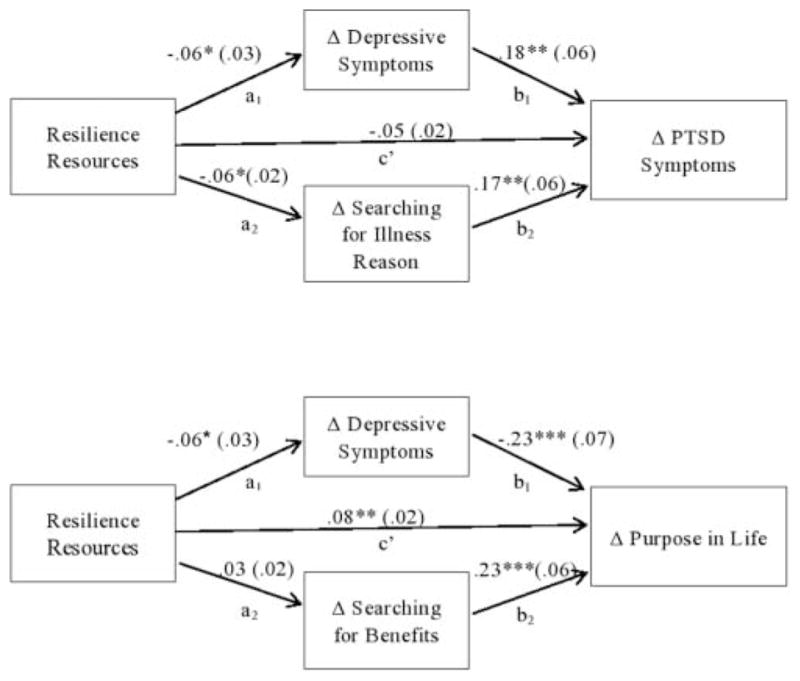
Mediation models for outcomes of residualized changes in PTSD symptoms (upper) and purpose in life (lower). Unstandardized coefficients (SE). Δ = residualized change. *p < .05, **p < .01, ***p < .001.
Purpose in life
In the hierarchical regression predicting residualized changes in purpose in life, sex and three dummy variables (intervention arms) were entered first, personal resilience resources were entered second, and residualized changes in depressive symptoms and the four meaning-making variables were entered in the third step (Table 4). The model explained 22% of the variance for purpose in life changes (F(10, 243) = 7.04, p < 0.001). Having greater personal resilience resources was associated with increases in purpose in life (b = 0.10, p < 0.001) and this remained a significant predictor (p = 0.001) in the third step with the addition of remaining variables. Decreases in depressive symptoms (b = −0.33, p < 0.001) and increases in searching for benefits in the illness (b = 0.16, p = 0.03) independently predicted increases in purpose in life. Changes in searching for and having found a reason for the illness, and having found benefits in the illness were not predictors (p’s > 0.05).
We next tested the indirect effects (Preacher & Hayes, 2008) of changes in depressive symptoms and searching for benefits. Sex and intervention dummy variables were included as controls. The specific indirect effects test indicated that only decreases in depressive symptoms were a mediator (b = 0.015, 95% Bca CI: 0.003, 0.033). The unstandardized coefficients for “a” paths (i.e., association between personal resilience resources and mediators) and “b” paths (i.e., association between mediators and purpose in life) and the direct effect are displayed in Figure 2. Having greater resilience resources at baseline was associated with decreases in depressive symptoms, which in turn was associated with increases in purpose in life. In this mediation model, the direct effect remained significant, suggesting unmeasured mediators of this relationship (c′ = 0.08, p = 0.0002).
Discussion
Being diagnosed with a life-threatening illness and undergoing SCT is, for many, a traumatic experience that is associated with substantial psychological and physical morbidity (Janoff-Bulman, 1992; Mosher et al., 2009; Park & Folkman, 1997). This experience can lead to PTSD symptoms and a diminished sense of purpose in life due to a disruption of valued activities and goals (Janoff-Bulman, 1992; Syrjala et al., 2004). Having personal resilience resources is associated with better psychological outcomes to traumatic illness experiences; however, the mechanisms of this association are unclear (Hochhausen et al., 2007; Kenzik et al., 2015; Rosenberg et al., 2015). In this study, we examined whether transplant survivors with greater resilience resources have better psychological outcomes after treatment, and whether this may be partly due to their meaning-making processes and/or greater likelihood of improvements in depressive symptoms, as these are also associated with SCT adjustment (Artherholt et al., 2014; El-Jawahri et al., 2015; Vickberg et al., 2001). Furthermore, we examined whether this may differ for two types of meaning-making: searching for or finding a reason for the illness and/or benefits in the illness experience.
Consistent with other research, survivors with greater personal resilience resources reported better outcomes as indicated by improvements in PTSD symptoms and in a sense of purpose in life (Stewart & Yuen, 2011). We also found that decreases in depressive symptoms were associated with improvements in both PTSD symptoms and a purpose in life. In addition, decreases in a search for why one became ill were beneficial, in the sense that it was associated with improvements in PTSD symptoms, not that they needed to have found the reason. Finding a reason for one’s illness may be difficult considering the complexities of these illnesses requiring SCT treatment. Instead, it may be more important that an individual is able to disengage from a futile search for why one became ill (Bonanno, Wortman, & Nesse, 2004; Tomich & Helgeson, 2002; Wu et al., 2008). Finally, we found that increases in a search for benefits from the illness experience, but not increases in having found benefits, were associated with increased purpose in life. Perhaps continuing to search for benefits from the illness may be similar to “counting one’s blessings” or having gratitude for how things had turned out considering that these were survivors who had had a successful transplant (Emmons & McCullough, 2003). In turn, this gratitude may motivate survivors to pursue valued activities and goals that contribute to sense of purpose in life.
Another point to consider is whether this benefit-oriented meaning-making may reflect different adjustment processes for resilient vs. less resilient survivors. Survivors in the upper quartile of personal resilience resources were more likely to report searching for benefits at baseline and follow-up than survivors in the lower quartile (p’s < 0.01, unreported findings). Based on the research with optimistic mothers of children undergoing SCT and cancer survivors high in dispositional hope (Rini et al., 2004; Stanton, Danoff-Burg, & Huggins, 2002), we suspect that for more resilient survivors, searching for benefits may reflect their positive outlook and confidence in managing difficulties, whereas for less resilient survivors, this process may reflect avoidant coping through wishful thinking. Overall, these findings suggest future research avenues to better understand how different types of meaning, and searching for vs. finding them, may reflect different adjustment processes depending on survivors’ dispositional resilience.
Our second purpose of this study was to examine potential mechanisms of why more resilient survivors adjust well to their illness experience. To this effect, we examined meaning-making processes and depressive symptoms as these have been reported as associated with psychological outcomes in SCT recipients (Adelstein et al., 2014; Artherholt et al., 2014; Vickberg et al., 2001). Understanding these mechanisms can inform the development of interventions to target psychological morbidity in less resilient survivors (Mosher et al., 2009). We found that improvements in depressive symptoms and decreases in a search for a reason for the illness partially explained the association of having greater resilience resources with decreases in PTSD symptoms. In addition, improvements in depressive symptoms partially explained the association with increases in purpose in life. These findings extend prior evidence of depressive symptoms as mechanisms of transplant survivors’ mental health-related quality of life (El-Jawahri et al., 2015; Kenzik et al., 2015) and that discontinuing an unsuccessful search for meaning, particularly as related to understanding one’s illness, may be beneficial (Bonanno et al., 2004; Tomich & Helgeson, 2002; Wu et al., 2008).
It is noteworthy that depressive symptoms were a mechanism in both the positive and negative outcomes considering that depressed transplant survivors have a greater mortality risk than nondepressed (Loberiza et al., 2002). Addressing these symptoms may improve survival and help survivors to achieve a more complete return to life as “normal”—i.e., no longer experiencing the transplant as a traumatic experience (PTSD symptoms) and engaging in valued activities (purpose in life). Furthermore, by examining the independent influences of depressive symptoms and meaning-making rather than confounding with unsuccessful searching (Bonanno, Papa, Lalande, Zhang, & Noll, 2005; Park, 2008), we have shown that both have a role in adjustment. Further research is needed to clarify how these processes operate together to promote adjustment. For instance, research could examine whether decreases in searching for meaning of the illness precede improvements in depressive symptoms, or whether they operate in a reciprocal feedback function. These findings also suggest the management of depressive symptoms and cognitive approaches to disengage unsuccessful meaning-making as potential intervention components.
Finally, it is notable that having found meaning (either the reason for the illness or its benefits) was not a mechanism of more resilient survivors’ adjustment. This is inconsistent with the meaning-making model’s assertion that finding meaning promotes adjustment after a traumatic experience (Park, 2010; Park & Folkman, 1997). However, it is consistent with other researchers’ assertion that a substantial proportion of people or even more resilient individuals do not need to find meaning for adjustment (Bonanno et al., 2004; Davis, Wortman, Lehman, & Silver, 2000). Another possibility to consider is that more resilient survivors may have already found meaning closer to their diagnosis and treatment, and their sense of having found meaning remained stable over the study period. Almost half reported no change in having found meaning from baseline to follow-up. Further research that occurs closer to diagnosis and treatment is needed to determine whether the type of meaning found early is important and whether it differs for more and less resilient individuals.
Limitations
These findings should be interpreted in the context of a few limitations. First, these mediation analyses were conducted with two time points and this limits our ability to draw a firmer conclusion about the mechanisms. Future research directions in this area should include a midpoint to better examine meaning-making and depressive symptoms as mechanisms of more resilient survivors’ adjustment to their illness experience. This future research should also consider including additional meaning-making concepts, such as attempts to align prior global views with one’s current reality appraisals or changes in life goals. The second limitation to note is that this study occurred after SCT survivors had completed treatment. It may be that more resilient survivors engage in more extensive meaning-making closer to their diagnosis and treatment. Third, the illness experience may have inspired the development of these personal resilience characteristics, similar to post-traumatic growth processes (Park & Fenster, 2004; Tedeschi & Calhoun, 2004). However, these resilience characteristics are shown to be stable over time and are indicative of dispositional traits (Carver & Scheier, 2014; Dunkel-Schetter & Dolbier, 2011). Fourth, participating in an intervention that involved revisiting the SCT experience through writing exercises may have inadvertently led to the associations of these variables. We controlled for intervention arms in the analyses to help address this possibility; however, future research should replicate and expand on these findings in a population that is not a part of an intervention. Finally, although our sample reflected some sociodemographic variability, it was a largely homogenous sample (i.e., middle-class, college educated, married/partnered), which may limit the findings’ generalizability to other populations with fewer sociodemographic resources.
Contributions
These findings provide preliminary evidence to inform intervention development to help less resilient SCT survivors achieve better adjustment after treatment. Particularly, resilience skills (e.g., self-confidence, positive reframing) may enable less resilient survivors to manage the depressive symptoms that are prevalent in this population and to engage in effective meaning-making (i.e., discontinue an unsuccessful search to understand illness) to reduce psychological comorbidities. Likewise, a cognitive-behavioral stress management intervention for breast cancer survivors that provided stress management skills similar to resilience coping styles (monitoring of negative cognitions and emotions, increasing self-confidence, relaxation, and social support assertiveness) reduced depressive symptoms and increased benefit finding, particularly among women who were initially low in optimism (Antoni et al., 2001). In addition, a therapeutic music video intervention delivered to adolescent–young adults during SCT showed increased positive coping (optimistic, supportive, nonconfrontational strategies) at postintervention and improved social integration perceptions and positive family environment 100 days post-transplant compared to an audiobook control group. Together, these suggest that delivering interventions during SCT that are designed to increase resilient coping strategies may have lasting benefits into the survivorship period.
In addition, our findings contribute to understanding the role of meaning-making in more resilient survivors’ adjustment, which has rarely been examined (Luszczynska, Mohamed, & Schwarzer, 2005; Park, 2010). In this sample, decreases in depressive symptoms and disengaging from a search for meaning of one’s illness appear important for more resilient survivors’ adjustment to their illness experience, whereas there was no support for the positive construal of meaning-making or that finding meaning was necessary (Park & Folkman, 1997). Future longitudinal research from the point of diagnosis and treatment to long-term survivorship, with multiple time points, will help clarify whether resilient survivors engage in more extensive meaning-making processes (that include positive construals of meaning) or whether they find meaning at all.
Acknowledgments
Funding
This research was supported by the American Cancer Society, Grant #RSGPB-07-285-01-CPPB (PI: Rini). Campo was supported by a Postdoctoral Research Fellowship from the National Center for Complementary and Integrative Health, Grant #T32AT003378). Wu was supported by the National Cancer Institute, Grant #7K07CA184145-02. This content is solely the responsibility of the authors and does not reflect the opinions or views of the funding and supporting agencies of NIH.
References
- Adelstein KE, Anderson JG, Taylor AG. Importance of meaning-making for patients undergoing hematopoietic stem cell transplantation. Oncology Nursing Forum. 2014;41(2):E172–E184. doi: 10.1188/14.ONF.E172-E184. [DOI] [PubMed] [Google Scholar]
- Antoni MH, Lehman JM, Kilbourn KM, Boyers AE, Culver JL, Alferi SM, … Carver CS. Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychology. 2001;20(1):20–32. doi: 10.1037//0278-6133.20.1.20. [DOI] [PubMed] [Google Scholar]
- Artherholt SB, Hong F, Berry DL, Fann JR. Risk factors for depression in patients undergoing hematopoietic cell transplantation. Biology of Blood and Marrow Transplant. 2014;20(7):946–950. doi: 10.1016/j.bbmt.2014.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aspinwall LG, MacNamara A. Taking positive changes seriously. Cancer. 2005;104(Suppl 11):2549–2556. doi: 10.1002/cncr.21244. [DOI] [PubMed] [Google Scholar]
- Aspinwall LG, Richter L. Optimism and self-mastery predict more rapid disengagement from unsolvable tasks in the presence of alternatives. Motivation and Emotion. 1999;23(3):221–245. doi: 10.1023/A:1021367331817. [DOI] [Google Scholar]
- Baker F, Marcellus D, Zabora J, Polland A, Jodrey D. Psychological distress among adult patients being evaluated for bone marrow transplantation. Psychosomatics. 1997;38(1):10–19. doi: 10.1016/S0033-3182(97)71498-1. [DOI] [PubMed] [Google Scholar]
- Benight CC, Bandura A. Social cognitive theory of posttraumatic recovery: The role of perceived self-efficacy. Behaviour Research and Therapy. 2004;42(10):1129–1148. doi: 10.1016/j.brat.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Papa A, Lalande K, Zhang N, Noll JG. Grief processing and deliberate grief avoidance: A prospective comparison of bereaved spouses and parents in the United States and the People’s Republic of China. Journal of Consulting and Clinical Psychology. 2005;73(1):86–98. doi: 10.1037/0022-006X.73.1.86. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Wortman CB, Nesse RM. Prospective patterns of resilience and maladjustment during widowhood. Psychology and Aging. 2004;19(2):260–271. doi: 10.1037/0882-7974.19.2.260. [DOI] [PubMed] [Google Scholar]
- Carver CS. Enhancing adaptation during treatment and the role of individual differences. Cancer. 2005;104(Suppl 11):2602–2607. doi: 10.1002/cncr.21247. [DOI] [PubMed] [Google Scholar]
- Carver CS, Antoni MH. Finding benefit in breast cancer during the year after diagnosis predicts better adjustment 5 to 8 years after diagnosis. Health Psychology. 2004;23(6):595–598. doi: 10.1037/0278-6133.23.6.595. [DOI] [PubMed] [Google Scholar]
- Carver CS, Lehman JM, Antoni MH. Dispositional pessimism predicts illness-related disruption of social and recreational activities among breast cancer patients. Journal of Personality and Social Psychology. 2003;84(4):813–821. doi: 10.1037/0022-3514.84.4.813. [DOI] [PubMed] [Google Scholar]
- Carver CS, Pozo C, Harris SD, Noriega V, Scheier MF, Robinson DS, … Clark KC. How coping mediates the effect of optimism on distress—A study of women with early-stage breast-cancer. Journal of Personality and Social Psychology. 1993;65(2):375–390. doi: 10.1037/0022-3514.65.2.375. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF. Dispositional optimism. Trends in Cognitive Sciences. 2014;18(6):293–299. doi: 10.1016/j.tics.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen R, Bavishi C, Rozanski A. Purpose in life and its relationship to all-cause mortality and cardiovascular events: A meta-analysis. Psychosomatic Medicine. 2015 doi: 10.1097/PSY.0000000000000274. [DOI] [PubMed] [Google Scholar]
- Copelan EA. Hematopoietic stem-cell transplantation. New England Journal of Medicine. 2006;354(17):1813–1826. doi: 10.1056/NEJMra052638. [DOI] [PubMed] [Google Scholar]
- Curbow B, Legro MW, Baker F, Wingard JR, Somerfield MR. Loss and recovery themes of long-term survivors of bone marrow transplants. Journal of Psychosocial Oncology. 1993;10:1–20. [Google Scholar]
- Davis CG, Nolen-Hoeksema S, Larson J. Making sense of loss and benefiting from the experience: two construals of meaning. Journal of Personality and Social Psychology. 1998;75(2):561–574. doi: 10.1037//0022-3514.75.2.561. [DOI] [PubMed] [Google Scholar]
- Davis CG, Wortman CB, Lehman DR, Silver RC. Searching for meaning in loss: are clinical assumptions correct. Death Studies. 2000;24(6):497–540. doi: 10.1080/07481180050121471. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Spencer P. Brief symptom inventory: BSI. Upper Saddle River, NJ: Pearson; 1993. [Google Scholar]
- DuHamel KN, Ostrof J, Ashman T, Winkel G, Mundy EA, Keane TM, … Redd W. Construct validity of the posttraumatic stress disorder checklist in cancer survivors: Analyses based on two samples. Psychological Assessment. 2004;16(3):255–266. doi: 10.1037/1040-3590.16.3.255. [DOI] [PubMed] [Google Scholar]
- Dunkel-Schetter C, Dolbier C. Resilience in the context of chronic stress and health in adults. Social and Personality Psychology Compass. 2011;5(9):634–652. doi: 10.1111/j.1751-9004.2011.00379.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Jawahri AR, Vandusen HB, Traeger LN, Fishbein JN, Keenan T, Gallagher ER, … Temel JS. Quality of life and mood predict posttraumatic stress disorder after hematopoietic stem cell transplantation. Cancer. 2015 doi: 10.1002/cncr.29818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emmons RA, McCullough ME. Counting blessings versus burdens: An experimental investigation of gratitude and subjective well-being in daily life. Journal of Personality and Social Psychology. 2003;84(2):377–389. doi: 10.1037//0022-3514.84.2.377. [DOI] [PubMed] [Google Scholar]
- Giralt S, Bishop MR. Principles and overview of allogeneic hematopoietic stem cell transplantation. Cancer Treatment and Research. 2009;144:1–21. doi: 10.1007/978-0-387-78580-6_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson VS, Reynolds KA, Tomich PL. A meta-analytic review of benefit find-ing and growth. Journal of Consulting and Clinical Psychology. 2006;74(5):797–816. doi: 10.1037/0022-006X.74.5.797. [DOI] [PubMed] [Google Scholar]
- Hochhausen N, Altmaier EM, McQuellon R, Davies SM, Papadopolous E, Carter S, Henslee-Downey J. Social support, optimism, and self-efficacy predict physical and emotional well-being after bone marrow transplantation. Journal of Psychosocial Oncology. 2007;25(1):87–101. doi: 10.1300/J077v25n01_05. [DOI] [PubMed] [Google Scholar]
- Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: A measure of subjective stress. Psychosomatic Medicine. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Jacobsen PB, Sadler IJ, Booth-Jones M, Soety E, Weitzner MA, Fields KK. Predictors of posttraumatic stress disorder symptomatology following bone marrow transplantation for cancer. Journal of Consulting and Clinical Psychology. 2002;70(1):235–240. doi: 10.1037//0022-006x.70.1.235. [DOI] [PubMed] [Google Scholar]
- Jacobsen PB, Widows MR, Hann DM, Andrykowski MA, Kronish LE, Fields KK. Posttraumatic stress disorder symptoms after bone marrow transplantation for breast cancer. Psychosomatic Medicine. 1998;60(3):366–371. doi: 10.1097/00006842-199805000-00026. [DOI] [PubMed] [Google Scholar]
- Janoff-Bulman R. Shattered assumptions: Towards a new psychology of trauma. New York: Free Press; 1992. [Google Scholar]
- Kenzik K, Huang IC, Rizzo JD, Shenkman E, Wingard J. Relationships among symptoms, psychosocial factors, and health-related quality of life in hematopoietic stem cell transplant survivors. Supportive Care in Cancer. 2015;23(3):797–807. doi: 10.1007/s00520-014-2420-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim ES, Strecher VJ, Ryff CD. Purpose in life and use of preventive health care services. Proceedings of the National Academy of Sciences of the United States of America. 2014;111(46):16331–16336. doi: 10.1073/pnas.1414826111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loberiza FR, Rizzo JD, Bredeson CN, Antin JH, Horowitz MM, Weeks JC, Lee SJ. Association of depressive syndrome and early deaths among patients after stem-cell transplantation for malignant diseases. Journal of Clinical Oncology. 2002;20(8):2118–2126. doi: 10.1002/Jco.2002.08.757. [DOI] [PubMed] [Google Scholar]
- Luszczynska A, Mohamed NE, Schwarzer R. Self-efficacy and social support predict benefit finding 12 months after cancer surgery: The mediating role of coping strategies. Psychology, Health & Medicine. 2005;10(4):365–375. doi: 10.1080/13548500500093738. [DOI] [Google Scholar]
- McQuellon R, Russell G, Cella D, Craven B, Brady M, Bonomi A, Hurd D. Quality of life measurement in bone marrow transplantation: Development of the functional assessment of cancer therapy–Bone Marrow Transplant (FACT–BMT) Scale. Bone Marrow Transplant. 1997;19(4):357–368. doi: 10.1038/sj.bmt.1700672. [DOI] [PubMed] [Google Scholar]
- Min JA, Yoon S, Lee CU, Chae JH, Lee C, Song KY, Kim TS. Psychological resilience contributes to low emotional distress in cancer patients. Supportive Care in Cancer. 2013;21(9):2469–2476. doi: 10.1007/s00520-013-1807-6. [DOI] [PubMed] [Google Scholar]
- Mohty B, Mohty M. Long-term complications and side effects after allogeneic hematopoietic stem cell transplantation: an update. Blood Cancer Journal. 2011;1 doi: 10.1038/bcj.2011.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosher CE, Redd WH, Rini CM, Burkhalter JE, DuHamel KN. Physical, psychological, and social sequelae following hematopoietic stem cell transplantation: A review of the literature. Psycho-Oncology. 2009;18(2):113–127. doi: 10.1002/pon.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nes LS, Segerstrom SC. Dispositional optimism and coping: A meta-analytic review. Personality and Social Psychology Review. 2006;10(3):235–251. doi: 10.1207/s15327957pspr1003_3. [DOI] [PubMed] [Google Scholar]
- Park CL. Testing the Meaning making model of coping with loss. Journal of Social and Clinical Psychology. 2008;27(9):970–994. doi: 10.1521/jscp.2008.27.9.970. [DOI] [Google Scholar]
- Park CL. Making sense of the meaning literature: An integrative review of meaning making and its effects on adjustment to stressful life events. Psychological Bulletin. 2010;136(2):257–301. doi: 10.1037/A0018301. [DOI] [PubMed] [Google Scholar]
- Park CL, Fenster JR. Stress-related growth: Predictors of occurrence and correlates with psychological adjustment. Journal of Social and Clinical Psychology. 2004;23(2):195–215. doi: 10.1521/jscp.23.2.195.31019. [DOI] [Google Scholar]
- Park CL, Folkman S. Meaning in the context of stress and coping. Review of general psychology. 1997;1(2):115–144. doi: 10.1037/1089-2680.1.2.115. [DOI] [Google Scholar]
- Pearlin LI, Schooler C. The structure of coping. Journal of Health and Social Behavior. 1978;19(1):2–21. [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Prochaska JJ, Velicer WF, Nigg CR, Prochaska JO. Methods of quantifying change in multiple risk factor interventions. Preventive Medicine. 2008;46(3):260–265. doi: 10.1016/j.ypmed.2007.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rini C, Austin J, Wu LM, Winkel G, Valdimarsdottir H, Stanton AL, … Redd WH. Harnessing benefits of helping others: A randomized controlled trial testing expressive helping to address survivorship problems after hematopoietic stem cell transplant. Health Psychology. 2014 doi: 10.1037/hea0000024. [DOI] [PubMed] [Google Scholar]
- Rini C, Manne S, DuHamel KN, Austin J, Ostroff J, Boulad F, … Redd WH. Mothers’ perceptions of benefit following pediatric stem cell transplantation: A longitudinal investigation of the roles of optimism, medical risk, and sociodemographic resources. Annals of Behavioral Medicine. 2004;28(2):132–141. doi: 10.1207/s15324796abm2802_9. [DOI] [PubMed] [Google Scholar]
- Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- Rosenberg AR, Syrjala KL, Martin PJ, Flowers ME, Carpenter PA, Salit RB, … Lee SJ. Resilience, health, and quality of life among long-term survivors of hematopoietic cell transplantation. Cancer. 2015;121(23):4250–4257. doi: 10.1002/cncr.29651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M. Implications of resilience concepts for scientific understanding. Annals of the New York Academy of Sciences. 2006;1094:1–12. doi: 10.1196/annals.1376.002. [DOI] [PubMed] [Google Scholar]
- Ryff CD, Singer B. The contours of positive human health. Psychological Inquiry. 1998;9(1):1–28. doi: 10.1207/s15327965pli0901_1. [DOI] [Google Scholar]
- Scheier MF, Carver CS. Effects of optimism on psychological and physical well-being—Theoretical overview and empirical update. Cognitive Therapy and Research. 1992;16(2):201–228. doi: 10.1007/Bf01173489. [DOI] [Google Scholar]
- Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the life orientation test. Journal of Personality and Social Psychology. 1994;67(6):1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Wrosch C, Baum A, Cohen S, Martire L, Matthews K, … Zdaniuk B. The life engagement test: Assessing purpose in life. Journal of Behavioral Medicine. 2006;29(3):291–298. doi: 10.1007/s10865-005-9044-1. [DOI] [PubMed] [Google Scholar]
- Schindel-Allon I, Aderka IM, Shahar G, Stein M, Gilboa-Schechtman E. Longitudinal associations between post-traumatic distress and depressive symptoms following a traumatic event: A test of three models. Psychological Medicine. 2010;40(10):1669–1678. doi: 10.1017/S0033291709992248. [DOI] [PubMed] [Google Scholar]
- Schoen E, Altmaier E, Tallman B. Coping after bone marrow transplantation: The predictive roles of optimism and dispositional coping. Journal of Clinical Psychology in Medical Settings. 2007;14(2):123–129. doi: 10.1007/s10880-007-9061-z. [DOI] [Google Scholar]
- Schwabish SD. Cognitive adaptation theory as a means to PTSD reduction among cancer pain patients. Journal of Psychosocial Oncology. 2011;29(2):141–156. doi: 10.1080/07347332.2010.548440. [DOI] [PubMed] [Google Scholar]
- Sloan JA, Cella D, Hays RD. Clinical significance of patient-reported questionnaire data: another step toward consensus. Journal of Clinical Epidemiology. 2005;58(12):1217–1219. doi: 10.1016/j.jclinepi.2005.07.009. [DOI] [PubMed] [Google Scholar]
- Smith MY, Redd W, DuHamel K, Vickberg SJ, Ricketts P. Validation of the PTSD checklist-civilian version in survivors of bone marrow transplantation. Journal of Traumatic Stress. 1999;12(3):485–499. doi: 10.1023/A:1024719104351. [DOI] [PubMed] [Google Scholar]
- Stanton AL, Danoff-Burg S, Huggins ME. The first year after breast cancer diagnosis: Hope and coping strategies as predictors of adjustment. Psycho-Oncology. 2002;11(2):93–102. doi: 10.1002/pon.574. [DOI] [PubMed] [Google Scholar]
- Stewart DE, Yuen T. A systematic review of resilience in the physically ill. Psychosomatics. 2011;52(3):199–209. doi: 10.1016/j.psym.2011.01.036. [DOI] [PubMed] [Google Scholar]
- Syrjala KL, Langer SL, Abrams JR, Storer B, Sanders JE, Flowers MED, Martin PJ. Recovery and long-term function after hematopoietic cell transplantation for leukemia or lymphoma. Jama-Journal of the American Medical Association. 2004;291(19):2335–2343. doi: 10.1001/jama.291.19.2335. [DOI] [PubMed] [Google Scholar]
- Tallman B, Shaw K, Schultz J, Altmaier E. Well-being and posttraumatic growth in unrelated donor marrow transplant survivors: a nine-year longitudinal study. Rehabilitation Psychology. 2010;55(2):204–210. doi: 10.1037/a0019541. [DOI] [PubMed] [Google Scholar]
- Taylor SE. Adjustment to threatening events—a theory of cognitive adaptation. Ameri-can Psychologist. 1983;38(11):1161–1173. doi: 10.1037//0003-066x.38.11.1161. [DOI] [Google Scholar]
- Tedeschi RG, Calhoun LG. Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry. 2004;15(1):1–18. doi: 10.1207/s15327965pli1501_01. [DOI] [Google Scholar]
- Thompson SC, Pitts JS. Factors relating to a person’s ability to find meaning after a diagnosis of cancer. Journal of Psychosocial Oncology. 1993;11(3):1–21. doi: 10.1300/J077V11N03_01. [DOI] [Google Scholar]
- Tomich PL, Helgeson VS. Five years later: A cross-sectional comparison of breast cancer survivors with healthy women. Psycho-Oncology. 2002;11(2):154–169. doi: 10.1002/pon.570. [DOI] [PubMed] [Google Scholar]
- Tomich PL, Helgeson VS. Is finding something good in the bad always good? Benefit finding among women with breast cancer. Health Psychology. 2004;23(1):16–23. doi: 10.1037/0278-6133.23.1.16. [DOI] [PubMed] [Google Scholar]
- Vickberg SMJ, Duhamel KN, Smith MY, Manne SL, Winkel G, Papadopoulos EB, Redd WH. Global meaning and psychological adjustment among survivors of bone marrow transplant. Psycho-Oncology. 2001;10(1):29–39. doi: 10.1002/1099-1611(200101/02)10:1<29::aid-pon482>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- Widows MR, Jacobsen PB, Booth-Jones M, Fields KK. Predictors of posttrau-matic growth following bone marrow transplantation for cancer. Health Psychology. 2005;24(3):266–273. doi: 10.1037/0278-6133.24.3.266. [DOI] [PubMed] [Google Scholar]
- Widows MR, Jacobsen PB, Fields KK. Relation of psychological vulnerability factors to posttraumatic stress disorder symptomatology in bone marrow transplant recipients. Psychosomaic Medicine. 2000;62(6):873–882. doi: 10.1097/00006842-200011000-00018. [DOI] [PubMed] [Google Scholar]
- Wrosch C, Scheier MF. Personality and quality of life: The importance of optimism and goal adjustment. Quality of Life Research. 2003;12:59–72. doi: 10.1023/A:1023529606137. [DOI] [PubMed] [Google Scholar]
- Wu L, Bonanno G, Duhamel K, Redd WH, Rini C, Austin J, … Manne S. Pre-bereavement meaning and post-bereavement distress in mothers of children who underwent haematopoietic stem cell transplantation. British Journal of Health Psychology. 2008;13(Pt 3):419–433. doi: 10.1348/135910707X204236. [DOI] [PubMed] [Google Scholar]
- Zumbo BD. The simple difference score as an inherently poor measure of change: Some reality, much mythology. In: Thompson B, editor. Advances in Social Science Methodology. Vol. 5. Greenwich, CT: JAI Press; 1999. pp. 269–304. [Google Scholar]



