Abstract
Objectives. To describe a community-wide contraception initiative and assess changes in method use when cost and access barriers are removed in an environment with client-centered counseling.
Methods. HER Salt Lake is a prospective cohort study occurring during three 6-month periods (September 2015 through March 2017) and nested in a quasiexperimental observational study. The sample was women aged 16 to 45 years receiving new contraceptive services at health centers in Salt Lake County, Utah. Following the control period, intervention 1 removed cost and ensured staffing and pharmacy stocking; intervention 2 introduced targeted electronic outreach. We used logistic regression and interrupted time series regression analyses to assess impact.
Results. New contraceptive services were provided to 4107 clients in the control period, 3995 in intervention 1, and 3407 in intervention 2. The odds of getting an intrauterine device or implant increased 1.6 times (95% confidence interval [CI] = 1.5, 1.6) during intervention 1 and 2.5 times (95% CI = 2.2, 2.8) during intervention 2, relative to the control period. Time series analysis demonstrated that participating health centers placed an additional 59 intrauterine devices and implants on average per month (95% CI = 13, 105) after intervention 1.
Conclusions. Removing client cost and increasing clinic capacity was associated with shifts in contraceptive method mix in an environment with client-centered counseling; targeted electronic outreach further augmented these results.
The US unintended pregnancy rate recently declined for the first time in decades,1 but at 45%, it remains a persistent and costly public health issue associated with an array of adverse social and health outcomes for women, children, and communities.2–9 Healthy People 2020 aims to improve pregnancy planning and spacing and prevent unintended pregnancy.10 The availability and affordability of family planning services, including the full range of contraceptive methods, is critical to meeting this goal.
Groundbreaking efforts in St. Louis, Missouri11; Iowa12; and Colorado13 established that eliminating financial barriers contributes to the increased use of highly effective reversible methods, including intrauterine devices (IUDs) and implants. Although increased access to all contraception is critical for women’s autonomy, the increased use of IUDs and implants further reduces population-level unintended pregnancy and abortion rates.12,14 These efforts laid the foundation for important next steps in implementation research.
Utah has unique barriers, including limited public funding for contraceptives, vast rural and frontier areas with limited women’s health care providers, and persistent issues with staffing trained providers and stocking IUDs and implants. In 2014, Utah voted against Medicaid expansion under the Affordable Care Act and, as of 2017, has yet to authorize a Medicaid family planning waiver. A post-Affordable Care Act evaluation determined that 207 350 Utah women were in need of publicly supported family planning services.15 However, even with the unique barriers and coverage gap, Utah has 1 of the nation’s highest rates of IUD and implant use.16 This is owing in large part to safety net systems such as Title X, a federal family planning grant program. The Planned Parenthood Association of Utah (PPAU) is the state’s only Title X grantee and is the leading provider of contraceptive services. Eight of the 9 PPAU health centers in Utah participate in Title X; the ninth site does not receive Title X and also provides abortion services. Through Title X, PPAU health centers offer financial support for a broad range of family planning methods and services per Title X grant agreements.
The University of Utah Family Planning Program partnered with PPAU to garner community, foundation, and pharmaceutical support for the HER Salt Lake Contraceptive Initiative (HER Salt Lake). Initially, we used the acronym HER to stand for highly effective reversible methods; however, as the initiative progressed we referred to it just as HER Salt Lake—with “her” as emphatic support for the women served, rather than favoring specific methods. Using a reproductive justice framework and incorporating social ecological theory, we considered public policy–, organizational-, community-, interpersonal-, and individual-level factors throughout the initiative.17,18 HER Salt Lake is a prospective cohort study that occurred during three 6-month periods and that was nested in a quasiexperimental observational study.
We have reported on differences in method use between the control period, intervention 1, and intervention 2 in an all-served cohort and a survey arm. Additionally, we evaluated the initiative in the context of IUD and implant use trends before study initiation and compared this with nonparticipating PPAU health centers.
METHODS
The prospective study took place during 3 periods: the control period (September 28, 2015 through March 27, 2016), intervention 1 (March 28, 2016 through September 25, 2016), and intervention 2 (September 26, 2016 through March 25, 2017). Participants who opted to participate in the survey arm received surveys at 1-, 3-, 6-, 12-, 18,- 24-, 30-, and 36-month time points between September 2015 and March 2020. The initiative worked within the existing PPAU clinical infrastructure to
coordinate removal of cost to all contraception;
increase clinic capacity (staffing and stocking devices);
ensure clients’ ability to discontinue and switch methods without out-of-pocket cost;
conduct a targeted electronic outreach and education campaign; and
collect prospective data and link health data to the Utah Population Database.
Study Population
We have reported data for 2 populations: the “all-served” cohort and the “survey arm” participants. The all-served cohort included females aged 16 to 45 years who went to the 4 participating health centers in Salt Lake County, Utah, for new contraceptive services. A new client seeking any contraceptive service or an existing client seeking a new contraceptive method qualified for the all-served cohort. We differentiated the all-served cohort into three 6-month study periods on the basis of the timing of the client’s first visit. Study staff informed all qualifying clients of the study and invited them to participate in the survey arm. Interested clients completed the informed consent process and the baseline survey in a private room. Survey arm participants, who consented to 3 years of follow-up surveys, are a subset of the all-served cohort. Eligibility requirements for the survey arm included being aged 18 to 45 years, being fluent in English or Spanish, desiring to prevent pregnancy for at least 1 year, having a functioning mobile telephone, and having an income under 300% federal poverty level as determined in 2015 by the US Department of Health and Human Services.
We use the term “women” throughout this article but acknowledge that not all individuals who are in need of contraceptive services (or who were served by this initiative) identify as women. Transgender men and gender-nonconforming individuals were eligible for all aspects of participation.
All-Served Cohort Development
Before initiation of observation and enrollment.
Before project initiation, a community advisory board of local contraceptive champions raised awareness and financial support. We conducted a community engagement studio with 10 individuals representing diverse Salt Lake County communities to inform the initiative.19
Before the study, PPAU trained their staff statewide on a standardized client-centered “contraceptive conversation.” The conversation included semistructured open-ended prompts to discuss personal user preferences and a standardized handout emphasizing ease of use and effectiveness. The conversation was on the basis of the shared decision-making model20–22 and incorporated studio input as well as the 10 best practices.23
Control period.
During the control period, clients at 4 Salt Lake County HER-participating health centers and 5 non-HER health centers (outside Salt Lake County) received standard contraceptive counseling and care. During the control period, some health centers did not have an advanced practice clinician onsite daily and were limited by pharmacy stocking. The out-of-pocket costs of contraceptive services were the same as before the control period. This included Title X–supported care for individuals below 100% of the federal poverty level and the use of sliding-scale fees to provide needs-based reduction of contraceptive costs for individuals between 101% and 250% of the federal poverty level. All methods, except the implant, were available on a sliding scale during the precontrol and the control periods. Of note, a low-cost levonorgestrel IUD (Liletta Medicine 360, Allergan, Madison, NJ) became available in May 2015. This was available at all PPAU clinics both before and throughout the control period.24
Intervention 1.
Intervention 1 implemented 2 evidence-based family planning practices: (1) removal of out-of-pocket costs for all reversible contraception, and (2) increased capacity to provide same-day IUDs and implants. To remove cost as a factor in contraceptive decision-making staff informed qualifying clients of the no-cost contraception before the contraceptive conversation. Clients were also informed that they could switch methods at any time over the next 3 years at no cost. Staff invited clients to enroll in the survey arm but confirmed that enrollment was not necessary to receive no-cost contraception. To enhance clinic capacity for same-day insertions, all HER-participating health centers had an ample stock of hormonal and nonhormonal IUDs and implants onsite. The ability to stock IUDs and implants was supported both by pharmaceutical companies supplying devices and study operations regularly managing inventory. The HER-participating health centers increased the number of days an advanced practice clinician attended the clinic and added time slots for IUD and implant insertions at HER-participating centers during the interventions. During intervention 1, PPAU conducted additional provider trainings on device insertions and removals.
Intervention 2.
During intervention 2, we launched a targeted online media campaign. The campaign used banners to advertise the availability of no-cost contraception on social media (Facebook and Instagram) and link potential clients to HERsaltlake.org. HERsaltlake.org was promoted as a Google search result when individuals in Salt Lake County searched for contraceptive-related words (i.e., “free birth control” or “IUD”). HERsaltlake.org provided a portal for appointment requests for contraceptive services at HER-participating health centers. Additionally, during intervention 2, when women living in Salt Lake County visited Bedsider.org directly, they received a pop-up window informing them about no-cost contraception through HERsaltlake.org. The campaign used creative content from whoopsproof.org, information gathered by our community engagement studio, and digital optimization to tailor advertisements to local women of reproductive age.
Data Sources
Electronic health records.
PPAU uses NextGen Healthcare, an electronic client management and electronic health records system. The electronic health record includes medical history and demographic information. We used the PPAU electronic health record to prospectively track the all-served cohort during interventions 1 and 2. During the control period, we obtained PPAU electronic health record data retrospectively, using the same qualifying visit codes for new contraceptive services and chart review (Table A, available as a supplement to the online version of this article at http://www.ajph.org). To control for baseline and trend changes in contraceptive method mix, we used the PPAU electronic health record to compare average monthly contraceptive use at the 4 HER-participating health centers to the 5 non-HER health centers (January 2014 through March 2017).
Survey arm data.
We administered surveys through a secure Web-based research electronic data capture (REDCap, Vanderbilt University, Nashville, TN) system at 9 specific time points from enrollment through 36 months after.25 Participants completed surveys via e-mail or telephone (and could receive reminder text messages) depending on their preference. Survey arm participants received a $20 gift card for a local supermarket at enrollment and were sent a $20 Amazon.com gift code at 6 months and at the end of each 12-month period for a total of $100 compensation.
Statistical Analysis
Descriptive statistics.
Variables described here are age, race, ethnicity, payer type, federal poverty level, parity, and health center location. We explored several comparisons using the χ2 test, including characteristics of the all-served cohort versus survey arm participants and client’s timing at first visit. We also assessed differences in contraceptive method mix during each phase of the study for the all-served cohort and the survey arm participants. We used Stata 14.0 or higher (StataCorp LP, College Station, TX) for all analyses.
Logistic regression analysis.
We used logistic regression to compare method use during intervention 1 and intervention 2 to the control period. We specifically report on changes in IUD and implant use. We also examined shorter-acting methods, including depot medroxyprogesterone acetate (DMPA) and pills, patches, and rings. We adjusted for sociodemographic variables known to affect contraceptive use: age, race, ethnicity, insurance status, federal poverty level, parity, and clinic location.26
Interrupted time series analysis (January 2014–March 2017).
To better understand current trends in regional contraceptive use and to control for trends and seasonality in contraceptive method mix preceding and during the study period, we evaluated 3.25 years of data on contraceptive use within all HER and non-HER PPAU health centers. We used billing data and Current Procedural Terminology, 4th edition codes from the PPAU electronic health record to generate aggregate counts for method type at each health center by month from January 2014 through completion of HER Salt Lake enrollment in March 2017. To explore monthly contraceptive prevalence, we weighted methods on the basis of the difference of provision frequency. We divided the DMPA counts by 4 and the pills, patches, and rings by 12.
In this analysis, we used an interrupted time series ordinary least squares regression analysis (ITSA) to compare trends in contraceptive use, specifically monthly averages (level) and changes during the periods (slope) at HER-participating and non-HER health centers before, during, and after the initiative and seasonally adjusted use by calendar month.27 We explored changes in level and slope of both IUD and implant insertions, DMPA, and pills, patches, and rings separately and collapsed them into contraceptive categories. The single group ITSA model estimating treatment effects for multiple intervention periods equation is as follows27:
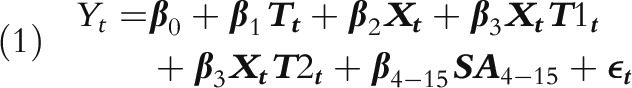 |
Where  represents the initial number of clients selecting method,
represents the initial number of clients selecting method,  estimates the average monthly change in the number over the preintervention period,
estimates the average monthly change in the number over the preintervention period,  represents the time since the beginning of the preintervention period,
represents the time since the beginning of the preintervention period,  represents the time since the beginning of the study period at intervention 1,
represents the time since the beginning of the study period at intervention 1,  represents the change in the level that occurred in the period immediately following intervention 1,
represents the change in the level that occurred in the period immediately following intervention 1,  is an indicator variable representing the pre–post intervention,
is an indicator variable representing the pre–post intervention,  represents the difference between pre–post-intervention trends for each method,
represents the difference between pre–post-intervention trends for each method,  is seasonal adjustment by calendar month using dummy variables, and εt is the term accounting for random error and autocorrelation. After examining the Cumby-Huizinga general test for time series autocorrelation, we did not see any significant lags (P < .05) and therefore did not include them in the analysis.
is seasonal adjustment by calendar month using dummy variables, and εt is the term accounting for random error and autocorrelation. After examining the Cumby-Huizinga general test for time series autocorrelation, we did not see any significant lags (P < .05) and therefore did not include them in the analysis.
RESULTS
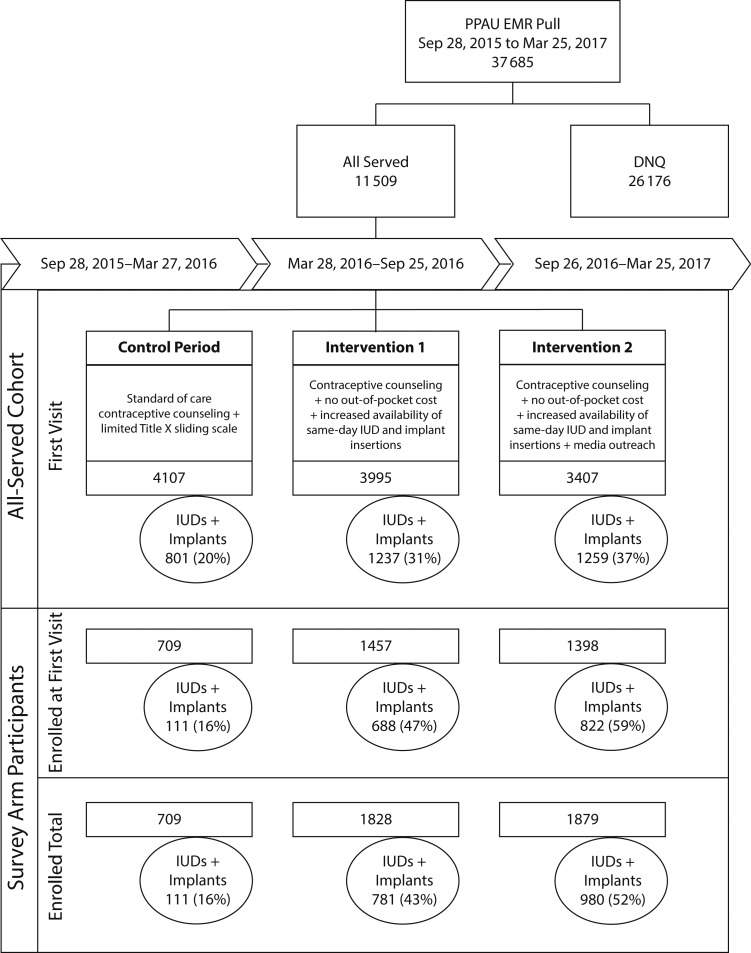
Over 18 months, 11 509 unique individuals presented to receive new contraceptive services at HER-participating health centers. Overall, 38% of the all-served cohort enrolled in the survey arm (n = 4427) and 81% of these participants enrolled at their first qualifying visit (Figure A, available as a supplement to the online version of this article at http://www.ajph.org). Figure 1 details the initiative and describes IUD and implant use at the time of first visit for the all-served cohort and the survey arm participants across each period. Demographic distributions were mostly similar between the all-served cohort clients who chose not to enroll and the all-served cohort clients who enrolled in the survey arm (Table 1). Age distribution was meaningfully different; those aged 16 or 17 years qualified for free contraception but were not eligible to enroll in the survey arm, because of limitations placed by the institutional review board. The survey arm cohort had higher proportions of women who were aged 18 to 24 years, parous, non-Hispanic White, and self-paying. Women who had their first visit during the interventions were also more likely to enroll in the survey arm.
FIGURE 1—
Participant Flow Diagram: Community-Wide HER Salt Lake Contraceptive Initiative, Salt Lake City, UT, January 2014—March 2017
Note. DNQ = did not qualify; EMR = electronic medical record; IUD = intrauterine device; PPAU = Planned Parenthood Association of Utah.
TABLE 1—
Demographic Characteristics Comparing Survey Arm Participants With the All-Served Cohort: HER Salt Lake Contraceptive Initiative, Salt Lake City, UT, September 2015–March 2017
| Variable | Not Enrolled, No. (%) | Survey Arm Participants, No. (%) | All-Served Cohort, No. (%) | P |
| Total | 7 082 (62) | 4 427 (38) | 11 509 (100) | |
| Age, y | < .001 | |||
| < 18 | 587 (8) | 18 (0) | 605 (5) | |
| 18–24 | 3 078 (43) | 2 551 (58) | 5 629 (49) | |
| 25–34 | 2 358 (33) | 1 541 (35) | 3 899 (34) | |
| ≥ 35 | 1 059 (15) | 317 (7) | 1 376 (12) | |
| Parity | .029 | |||
| Nulliparous | 4 496 (63) | 2 721 (61) | 7 217 (63) | |
| Parous | 2 586 (37) | 1 706 (39) | 4 292 (37) | |
| Federal poverty levela | .64 | |||
| ≤ 100% | 6 957 (98) | 4 354 (98) | 11 311 (98) | |
| > 100% | 125 (2) | 73 (2) | 198 (2) | |
| Race/ethnicity | < .001 | |||
| Non-Hispanic White | 4 267 (60) | 2 926 (66) | 7 193 (62) | |
| Hispanic non-White | 2 045 (29) | 1 028 (23) | 3 073 (27) | |
| Other | 770 (11) | 473 (11) | 1 243 (11) | |
| Insurance status | < .001 | |||
| Self-pay | 4 625 (65) | 3 240 (73) | 7 865 (68) | |
| Public | 529 (7) | 224 (5) | 753 (7) | |
| Private | 1 928 (27) | 963 (22) | 2 891 (25) | |
| Clinic location | < .001 | |||
| Metro health center | 400 (6) | 472 (11) | 872 (8) | |
| Salt Lake clinic | 2 275 (32) | 1 503 (34) | 3 778 (33) | |
| South Jordan | 1 449 (20) | 856 (19) | 2 305 (20) | |
| West Valley | 2 958 (42) | 1 596 (36) | 4 553 (40) | |
| Salt Lake County resident | .74 | |||
| No | 1 627 (23) | 1 029 (23) | 2 656 (23) | |
| Yes | 5 455 (77) | 3 398 (77) | 8 853 (77) | |
| Timing of first qualifying visit | < .001 | |||
| Control period | 2 730 (39) | 1 377 (31) | 4 107 (36) | |
| Intervention 1 | 2 346 (33) | 1 649 (37) | 3 995 (35) | |
| Intervention 2 | 2 006 (28) | 1 401 (32) | 3 407 (30) |
Defined by the US Census.
The all-served cohort had a higher use of barrier methods (condoms, diaphragms) and emergency contraception and a higher proportion of clients walking away from the clinic with no documented contraception. Survey arm participants had a higher use of more effective methods across periods. Figure B (available as a supplement to the online version of this article at http://www.ajph.org) presents the contraceptive method mix for the all-served cohort (part a) and the survey arm participants (part b) across periods. These figures demonstrate a significant rise in IUD and implant use during interventions 1 and 2, with a corresponding decrease in less effective methods.
Logistic Regression Results
Method use also differed between the all-served cohort and survey arm participants. Changes in method mix will be described in more detail in subsequent analyses; however, the contraceptive mix changed significantly for both the all-served and survey arm participants following the interventions. At the HER-participating health centers, the odds of getting an IUD or implant during intervention 1 increased by a factor of 1.6 (95% confidence interval [CI] = 1.5, 1.6), compared with the control period, and a factor of 2.5 (95% CI = 2.2, 2.8) during intervention 2, compared with the control period in the all-served cohort. Compared with the all-served cohort, survey arm participants were more than twice as likely to obtain an IUD or implant at their first visit (odds ratio [OR] = 2.5; 95% CI = 2.4, 2.7) in all periods.
Interrupted Time Series Results
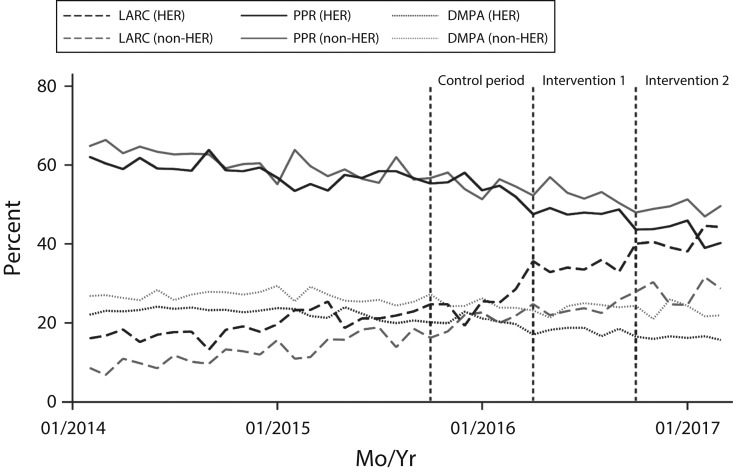
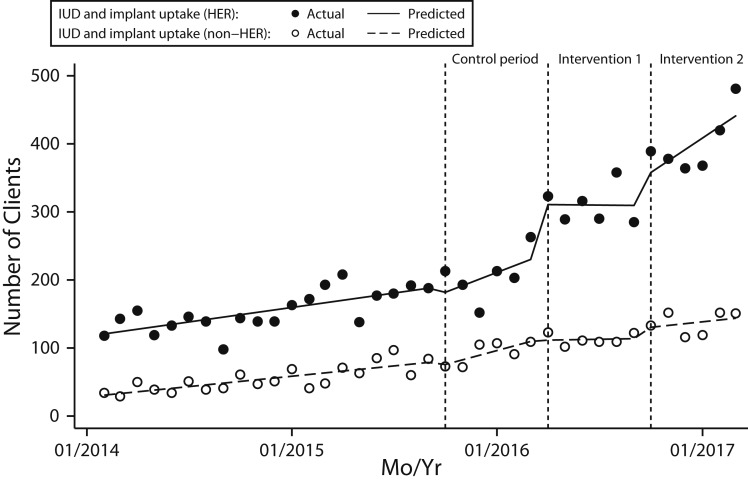
Figure 2 shows the time series analysis of contraceptive use at HER-participating health centers and non-HER health centers during the 21 months before the control period through the initiative. Leading up to the initiative and through the control period, overall trends of all methods were similar for HER-participating and non-HER health centers. Figure 3 depicts the results from an ITSA assessing IUD and implant use with seasonal adjustment. The results demonstrate that there was no level or slope effect of the control period for either the HER-participating or non-HER health centers. Between January 1, 2014, and March 27, 2016, both participating and non-HER health centers had similar upward trends in IUD and implant use (ITSA results for pills, patches, and rings and DMPA are not shown but are available upon request).
FIGURE 2—
Contraceptive Method Distribution in All Planned Parenthood Association of Utah Health Centers: HER Salt Lake Contraceptive Initiative, Salt Lake City, UT, January 2014—March 2017
Note. DMPA = depot medroxyprogesterone acetate; IUD = intrauterine device; LARC = long-acting reversible contraception; PPR = pills, patches, and rings.
FIGURE 3—
Intrauterine Device (IUD) and Implant Uptake at HER Participating and Non-HER Participating Health Centers, Seasonally Adjusted: HER Salt Lake Contraceptive Initiative, Salt Lake City, UT, January 2014—March 2017
When looking at the initiative as a whole, HER-participating Salt Lake County health centers placed an average of 90 more devices per month (95% CI = 72, 108) than did non-HER clinics. Following the removal of cost and increasing clinic capacity, there was a significantly increased level change in IUD and implant use in the HER-participating health centers compared with non-HER health centers by an average of 59 IUDs and implants per month (95% CI = 13, 105). Participating centers had a postintervention linear trend that was 32% (95% CI = 12%, 53%) steeper than was the nonparticipating centers (coefficient = 0.44 vs 0.11; P = .003). When breaking the initiative out further and assessing control period, intervention 1, and intervention 2 as separate events, statistical power reduces, yet there is still a post–intervention 1 increase of 76 device per month (95% CI = 8, 143) but no difference in the slope of use of IUDs and implants between HER and non-HER health centers (coefficient = −0.02; 95% CI = −0.49, 0.45). At intervention 2, there was not a statistically significant level increase in the number of devices compared with intervention 1 (16; 95% CI = −10, 42) but change in slope was steeper (coefficient = 0.46; 95% CI = −0.10, 1.03) after seasonal adjustment.
DISCUSSION
Regardless of enrollment status, HER Salt Lake demonstrated statistically significant shifts in method mix toward more effective methods. We observed increased IUD and implant use when out-of-pocket costs were removed and provider and device availability improved in an environment using client-centered counseling. Further shifts occurred with the addition of a public-facing media campaign. Although survey arm participants differed from those not enrolled, the detailed information collected from enrolled individuals will be critical in assessing social and economic impact and other long-term assessments. This selection bias is not unique to this study; recruitment to research studies in general have demonstrated self-selection bias in enrollment patterns.28 However, the use of contraceptive service data from HER-participating and non-HER health centers allowed us to put the intervention in a multiyear context, which strengthens this study’s conclusions. Additionally, a strength of the ITSA is that it differentiates the intervention effect from changes that would have happened over time without the interventions.29
HER Salt Lake was initiated with 5 primary innovations:
Using existing clinical infrastructure;
Initiating standardized client-centered contraceptive counseling before the control period;
Confirming community support for the project;
Coordinating funding sources that included local supporters promoting sustainability; and
Performing long-term follow-up at the population level using the Utah Population Database.
Limitations and Strengths
The large, longitudinal nature of this study and its having multiple sites, outcomes, and data sources pose operational and analytical challenges. Crossover occurred between the 3 periods; specifically, 19% of women who received care at a participating health center during the control period returned during intervention 1 or 2 and enrolled in the survey arm (Figure C, available as a supplement to the online version of this article at http://www.ajph.org). Moving forward, we will analyze data on the basis of both treatment at initial presentation and a per-protocol approach to explore method switching over time and the impact on outcomes. The findings we have presented assess only use at the first visit. Despite some limitations, HER Salt Lake offers a unique opportunity to assess the individual and community outcomes of expanding contraceptive access using existing family planning infrastructure in environments that provide client-centered counseling.
Public Health Implications
The development of safe and effective contraception is widely accepted as 1 of the 10 most important public health achievements of the 20th century.30 However, even in the 21st century, access to these essential services is still not universal, and federal- and state-level policies can either support or hinder women’s access to contraception. These findings and forthcoming work from HER Salt Lake provide local-level data that will inform clinical care, policy, and future translational research. These data provide an example of the critical role that Planned Parenthood plays as a Title X health center in expanding access to a broad range of contraceptive methods and integrating best practices in a state with limited publicly funded support. This project will now prospectively follow participants to track the collective dimension of universal access to family planning services, including maternal and infant health outcomes and the social, economic, sexual, and emotional health of individuals served.
ACKNOWLEDGMENTS
This project is funded by the Society of Family Planning Research Fund, the William and Flora Hewlett Foundation, and an anonymous foundation. The following companies contributed contraceptive products for the project: Bayer Women’s Healthcare, Merck & Co. Inc., and Teva Pharmaceuticals. Use of REDCap was provided by the Eunice Kennedy Shriver National Institute of Child Health and Development (grant 8UL1TR000105 [formerly UL1RR025764] National Center for Advancing Translational Sciences/National Institutes of Health [NIH]). Team members receive support from the Eunice Kennedy Shriver National Institute of Child Health & Human Development and the Office of Research on Women’s Health of the NIH (awards K12HD085852 to J. N. S. and K24HD087436 to D. K. T.).
We are grateful for the community support for HER Salt Lake from the Willard L. Eccles Foundation, the Intermountain Community Care Foundation, private contributions, and our community advisory board (lead by Annette Cumming and Kim Wirthlin). The authors acknowledge the exceptional execution of HER Salt Lake by our research team (Jasmin Alcantara, Eduardo Galindo, Amy Orr, Corinne Sexsmith); administrative support of the University of Utah Obstetrics and Gynecology Network; research and statistical consultations from the HER Data Advisory Committee (Bethany Everett, Daniel Adkins, Claudia Geist); the incredible clinical and research partnership of the Planned Parenthood Association of Utah; and work of our colleagues who generously provided advice on the basis of their previous successful execution of large-scale reproductive health interventions.
Note. This content is solely the responsibility of the authors and does not necessarily represent the official view of any of the funding agencies or participating institutions, including the NIH, the University of Utah, and the Planned Parenthood Federation of America, Inc.
HUMAN PARTICIPANT PROTECTION
The University of Utah institutional review board approved the HER Salt Lake study.
REFERENCES
- 1.Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. N Engl J Med. 2016;374(9):843–852. doi: 10.1056/NEJMsa1506575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kost K, Lindberg L. Pregnancy intentions, maternal behaviors, and infant health: investigating relationships with new measures and propensity score analysis. Demography. 2015;52(1):83–111. doi: 10.1007/s13524-014-0359-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hellerstedt WL, Pirie PL, Lando HA et al. Differences in preconceptional and prenatal behaviors in women with intended and unintended pregnancies. Am J Public Health. 1998;88(4):663–666. doi: 10.2105/ajph.88.4.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abajobir AA, Maravilla JC, Alati R, Najman JM. A systematic review and meta-analysis of the association between unintended pregnancy and perinatal depression. J Affect Disord. 2016;192:56–63. doi: 10.1016/j.jad.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 5.Axinn WG, Barber JS, Thornton A. The long-term impact of parents’ childbearing decisions on children’s self-esteem. Demography. 1998;35(4):435–443. [PubMed] [Google Scholar]
- 6.Cheng D, Schwarz EB, Douglas E, Horon I. Unintended pregnancy and associated maternal preconception, prenatal and postpartum behaviors. Contraception. 2009;79(3):194–198. doi: 10.1016/j.contraception.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 7.Gipson JD, Koenig MA, Hindin MJ. The effects of unintended pregnancy on infant, child, and parental health: a review of the literature. Stud Fam Plann. 2008;39(1):18–38. doi: 10.1111/j.1728-4465.2008.00148.x. [DOI] [PubMed] [Google Scholar]
- 8.Logan CH, Holcombe E, Manlove J, Ryan S. The Consequences of Unintended Childbearing: A White Paper. Bethesda, MD: Child Trends; 2007. [Google Scholar]
- 9.Parks C, Peipert JF. Eliminating health disparities in unintended pregnancy with long-acting reversible contraception (LARC) Am J Obstet Gynecol. 2016;214(6):681–688. doi: 10.1016/j.ajog.2016.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.US Office of Disease Prevention and Health Promotion. 2020 Topics and objectives. Available at: http://www.healthypeople.gov/2020/topicsobjectives2020/default. Accessed Jan 20, 2015.
- 11.Secura GM, Allsworth JE, Madden T, Mullersman JL, Peipert JF. The Contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol. 2010;203(2):115.e111–115.e117. doi: 10.1016/j.ajog.2010.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Biggs MA, Rocca CH, Brindis CD, Hirsch H, Grossman D. Did increasing use of highly effective contraception contribute to declining abortions in Iowa? Contraception. 2015;91(2):167–173. doi: 10.1016/j.contraception.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 13.Ricketts S, Klingler G, Schwalberg R. Game change in Colorado: widespread use of long-acting reversible contraceptives and rapid decline in births among young, low-income women. Perspect Sex Reprod Health. 2014;46(3):125–132. doi: 10.1363/46e1714. [DOI] [PubMed] [Google Scholar]
- 14.Peipert JF, Madden T, Allsworth JE, Secura GM. Preventing unintended pregnancies by providing no-cost contraception. Obstet Gynecol. 2012;120(6):1291–1297. doi: 10.1097/aog.0b013e318273eb56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Frost JJ, Frohwirth L, Zolna MR. Contraceptive Needs and Services, 2014 Update. New York, NY: Guttmacher Institute; 2016. [Google Scholar]
- 16.Centers for Disease Control and Prevention. Contraceptive use among nonpregnant and postpartum women at risk for unintended pregnancy, and female high school students, in the context of zika preparedness—United States, 2011–2013 and 2015. MMWR Morb Mortal Wkly Rep. 2016;65(30):780–787. doi: 10.15585/mmwr.mm6530e2. [DOI] [PubMed] [Google Scholar]
- 17.Ross L, Solinger R. Reproductive Justice: An Introduction. Oakland, CA: University of California Press; 2017. [Google Scholar]
- 18.Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot. 1996;10(4):282–298. doi: 10.4278/0890-1171-10.4.282. [DOI] [PubMed] [Google Scholar]
- 19.Joosten YA, Israel TL, Williams NA et al. Community engagement studios: a structured approach to obtaining meaningful input from stakeholders to inform research. Acad Med. 2015;90(12):1646–1650. doi: 10.1097/ACM.0000000000000794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Educ Couns. 2006;60(3):301–312. doi: 10.1016/j.pec.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 21.Dehlendorf C, Diedrich J, Drey E, Postone A, Steinauer J. Preferences for decision-making about contraception and general health care among reproductive age women at an abortion clinic. Patient Educ Couns. 2010;81(3):343–348. doi: 10.1016/j.pec.2010.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dehlendorf C, Krajewski C, Borrero S. Contraceptive counseling: best practices to ensure quality communication and enable effective contraceptive use. Clin Obstet Gynecol. 2014;57(4):659–673. doi: 10.1097/GRF.0000000000000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Levine D, Jaccard J, Kantor L, Levitz N. Ten best practice of contraceptive counseling, and integrating them into a counseling protocol. Paper presented at: American Public Health Association annual meeting; Chicago, IL; October 31–November 4, 2015. [Google Scholar]
- 24.Roth L, Sanders J, Simmons R, Bullock H, Jacobsen E, Turok D. Changes in use and cost of LARC devices following the introduction of a new, low-cost levonorgestrel IUD in Utah’s Title X clinics: a retrospective review. Contraception. doi: 10.1016/j.contraception.2018.03.029. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Frost JJ, Darroch JE. Factors associated with contraceptive choice and inconsistent method use, United States, 2004. Perspect Sex Reprod Health. 2008;40(2):94–104. doi: 10.1363/4009408. [DOI] [PubMed] [Google Scholar]
- 27.Lopez Bernal J, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348–355. doi: 10.1093/ije/dyw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grimes DA, Schulz KF. Bias and causal associations in observational research. Lancet. 2002;359(9302):248–252. doi: 10.1016/S0140-6736(02)07451-2. [DOI] [PubMed] [Google Scholar]
- 29.Taljaard M, McKenzie JE, Ramsay CR, Grimshaw JM. The use of segmented regression in analysing interrupted time series studies: an example in pre-hospital ambulance care. Implement Sci. 2014;9:77. doi: 10.1186/1748-5908-9-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. Ten great public health achievements—United States, 1900–1999. MMWR Morb Mortal Wkly Rep. 1999;48(12):241–243. [PubMed] [Google Scholar]