Abstract
We present a case of cerebral venous sinus thrombosis (CVST) as a rare complication of herpes simplex virus (HSV) encephalitis. A young man with no pertinent medical history was diagnosed with HSV encephalitis. After initial treatment, he showed improvement in symptomatology until day 6 when he acutely developed new neurological deficits. An urgent MRI brain showed changes in left temporal lobe consistent with HSV encephalitis and lack of flow void in superior sagittal sinus. Subsequent magnetic resonance venography confirmed the diagnosis of superior sagittal sinus thrombosis along with thrombosis of bilateral frontoparietal cortical draining veins. Anticoagulation was immediately initiated and oral anticoagulation was continued for 1 year. He made complete recovery subsequently. Our case serves as a reminder for the treating clinicians to consider CVST in patients with HSV encephalitis who develop an unexpected new neurological deficits during early phase of appropriate treatment.
Keywords: meningitis, infection (neurology), neuroimaging, stroke, radiology
Background
Cerebral venous sinus thrombosis (CVST) is an uncommon cause of venous stroke due to conditions such as infections, trauma, surgery, drugs, thrombophilic disorders and cancers.1–3 CVST is less common than other types of strokes and could be more challenging to diagnose due to its varying presentation. Thrombosis of the intracranial venous drainage system produces array of symptoms. Intracranial infection can trigger a cascade of biochemical changes that can alter patient’s clinical condition. These biochemical changes may also lead to concurrent development of complications that can modify the clinical progression. Herpes simplex virus (HSV) encephalitis is not an uncommon intracranial infection, with acyclovir being the treatment of choice.4 Viral encephalitis is found to be the most common cause of encephalitis in large case series.5 6 The general outcome for the patient with timely and appropriate treatment is promising. Early initiation of acyclovir increases chances of promising recovery and extent of brain parenchyma involvement on the MRI has a prognostic value.7 We report a rare presentation of HSV encephalitis complicated by CVST in a patient with no other risk factors.
Case presentation
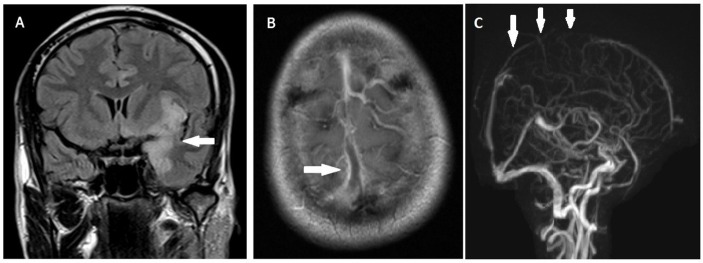
A 31-year-old man was brought to the hospital after his first ever episode of a generalised tonic-clonic seizure. Other symptoms were 3 days of fever, generalised headache and photophobia. He did not have a history of seizure, drug abuse, alcohol or other significant illness. He had no pertinent medical history and was not on any long-term medications. He was a lifelong non-smoker with no family history of seizures, cancers or thrombophilias. Neurological examination revealed mild drowsiness and neck rigidity. Initial CT of the brain and laboratory tests showed no abnormality, including a normal white cell count. Cerebrospinal fluid (CSF) analysis showed a lymphocyte predominant pleocytosis, with normal glucose and protein. Gram stain did not show any organisms, but a CSF PCR was positive for HSV. He was treated for acute meningoencephalitis with intravenous acyclovir. He became more alert, and the headache resolved gradually. However, on day 6, the patient developed bilateral upper limb weakness, incoordination and worsening headache. An urgent MRI brain showed changes in the left temporal lobe consistent with HSV encephalitis (figure 1A) and flow void in the superior sagittal sinus (figure 1B) consistent with superior sagittal sinus thrombosis. Subsequent magnetic resonance venography (MRV) confirmed a superior sagittal sinus thrombosis (figure 1C). Further workup revealed no other abnormalities predisposing him to a prothrombotic state, including a normal thrombophilia screen.
Figure 1.
(A) Fluid-attenuated inversion recovery (FLAIR) MRI coronal view shows hyperintensity in the left temporal lobe, consistent with herpes simplex virus (HSV) encephalitis. (B) T1-weighted image axial view after contrast with filling defect, consistent with thrombus in the superior sagittal sinus. (C) Magnetic resonance venography (MRV) shows superior sagittal sinus thrombosis.
Investigations
complete blood count: normal;
serum chemistry: normal;
thrombophilia workup including protein C, protein S, antithrombin III, lupus anticoagulant, Leiden factor V mutation: normal;
antiphospholipid and anticardiolipin antibodies for antiphospholipid syndrome: normal;
autoimmune workup including anti-DNA antibodies, antineutrophil cytoplasmic antibodies, antinuclear antibody: normal;
urine analysis: negative for proteinuria to rule out nephrotic syndrome;
CSF analysis: lymphocyte-predominant pleocytosis;
CSF herpes simplex PCR: positive;
MRI brain: showed changes consistent with HSV encephalitis in the left temporal lobe and flow void in the superior sagittal sinus, consistent with superior sagittal sinus thrombosis;
MRV brain: confirmed superior sagittal sinus thrombosis.
Differential diagnosis
HSV encephalitis complicated by hydrocephalus;
worsening of HSV infection (failure of treatment).
Treatment
The patient was continued on acyclovir (antiviral, treatment for HSV encephalitis), started on intravenous heparin and bridged with warfarin (treatment of CVST), and continued for 1 year.
Outcome and follow-up
The patient’s neurological deficits recovered completely with treatment. At 1-year follow-up, the patient was asymptomatic with no neurological deficits or long-term sequel from HSV encephalitis or CVST.
Discussion
CVST is a rare complication of HSV. While parameningeal infections are common causes of cerebral venous thromboses, HSV is not recognised as such.8 9 HSV encephalitis has been identified as a cause of arterial stroke and cerebral haematoma but there is no reported association of CVST and HSV encephalitis to the best of our knowledge and literature search.10–12 Data available from sizeable case series have established thrombophilic disorders, oral contraceptive use, otitis media and active malignancy to be common causes, although a significant proportion of cases remained idiopathic.13 14 Interestingly, Behcet’s disease is known to present as both encephalitis and CVST.15 Headache is the most common feature of CVST reported in up to 40%–90% of the patients, followed by seizures, altered mental status and motor deficits, but these overlap with HSV encephalitis which was the primary pathological condition in our patient.8 Cases have been described when patients were treated as for HSV encephalitis due to overlapping clinical presentation and CT scan appearance; however, the diagnosis and treatment required revision after angiography confirmed cortical venous thrombosis.16 HSV infection is known to promote a thrombogenic environment by altering the endothelial cell surface properties by various mechanisms. Some of the better studied mechanisms by which HSV promotes intravascular thrombosis are: inhibition of natural anticoagulants and activation of procoagulants, causing an increase in the binding sites for inflammatory cells, further adding to the prothrombotic propensity.17 Early diagnosis and initiation of anticoagulation are vital to ensure better neurological outcome.9 Despite appropriate antiviral therapy, our patient with HSV encephalitis deteriorated following initial improvement in symptomatology. MRV confirmed segmental superior sagittal sinus thrombosis along with bilateral frontoparietal cortical draining vein thromboses. Anticoagulation with intravenous heparin was immediately initiated, followed by warfarin. Our patient achieved complete recovery and continued anticoagulation for 1 year, after which it was discontinued. HSV encephalitis has not been seen as a common association with CVST.12–14 Our case serves as a reminder for the treating clinician to consider CVST as a rare—although treatable—complication of HSV encephalitis. If a patient with HSV encephalitis develops a new neurological deficit after initial improvement during the early phase of treatment, this rare complication should be considered.
Learning points.
Worsening of symptoms, after good initial response, for the treatment of herpes simplex virus (HSV) encephalitis is unusual.
In case of new neurological deficits, while on appropriate treatment for HSV encephalitis, urgent neuroimaging should be pursued.
Cerebral venous sinus thrombosis is a rare complication associated with HSV encephalitis and should be considered.
Footnotes
Contributors: AL: data collection, initial draft, review, revision of manuscript. MCD: data collection, review. ACFH: critical review. AA: conceiving idea, data collection, critical review.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Sriram N, Saifee TA. Cerebral venous sinus thrombosis. Br J Hosp Med 2017;78:C98–C102. 10.12968/hmed.2017.78.7.C98 [DOI] [PubMed] [Google Scholar]
- 2.Gazioglu S, Eyuboglu I, Yildirim A, et al. . Cerebral venous sinus Thrombosis: Clinical Features, Long-Term outcome and recanalization. J Clin Neurosci 2017;45:248–51. 10.1016/j.jocn.2017.07.028 [DOI] [PubMed] [Google Scholar]
- 3.Einhäupl K, Stam J, Bousser MG, et al. . EFNS guideline on the treatment of cerebral venous and sinus thrombosis in adult patients. Eur J Neurol 2010;17:1229–35. 10.1111/j.1468-1331.2010.03011.x [DOI] [PubMed] [Google Scholar]
- 4.Bradshaw MJ, Venkatesan A. Herpes Simplex Virus-1 Encephalitis in Adults: Pathophysiology, Diagnosis, and Management. Neurotherapeutics 2016;13:493–508. 10.1007/s13311-016-0433-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Çiftçi Kavaklioğlu B, Çoban E, Şen A, et al. . Review of Viral Encephalitis Cases Seen at a Tertiary Care Center in Turkey: Focus on Herpes Simplex Type 1. Noro Psikiyatr Ars 2017;54:209–15. 10.5152/npa.2016.12540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boucher A, Herrmann JL, Morand P, et al. . Epidemiology of infectious encephalitis causes in 2016. Med Mal Infect 2017;47:221–35. 10.1016/j.medmal.2017.02.003 [DOI] [PubMed] [Google Scholar]
- 7.Rabinstein AA. Herpes virus encephalitis in adults: current knowledge and old myths. Neurol Clin 2017;35:695–705. 10.1016/j.ncl.2017.06.006 [DOI] [PubMed] [Google Scholar]
- 8.Jha S, Jose M, Kumar V. Herpes simplex encephalitis: some interesting presentations. Neurol India 2003;51:399–400. [PubMed] [Google Scholar]
- 9.Saposnik G, Barinagarrementeria F, Brown RD, et al. . Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011;42:1158–92. 10.1161/STR.0b013e31820a8364 [DOI] [PubMed] [Google Scholar]
- 10.Takeuchi S, Takasato Y. Herpes simplex virus encephalitis complicated by intracerebral hematoma. Neurol India 2011;59:594–6. 10.4103/0028-3886.84344 [DOI] [PubMed] [Google Scholar]
- 11.Zis P, Stritsou P, Angelidakis P, et al. . Herpes Simplex Virus Type 2 Encephalitis as a Cause of Ischemic Stroke: Case Report and Systematic Review of the Literature. J Stroke Cerebrovasc Dis 2016;25:335–9. 10.1016/j.jstrokecerebrovasdis.2015.10.002 [DOI] [PubMed] [Google Scholar]
- 12.Modi S, Mahajan A, Dharaiya D, et al. . Burden of herpes simplex virus encephalitis in the United States. J Neurol 2017;264:1204–8. 10.1007/s00415-017-8516-x [DOI] [PubMed] [Google Scholar]
- 13.Bousser MG, Chiras J, Bories J, et al. . Cerebral venous thrombosis--a review of 38 cases. Stroke 1985;16:199–213. 10.1161/01.STR.16.2.199 [DOI] [PubMed] [Google Scholar]
- 14.Mak W, Mok KY, Tsoi TH, et al. . Cerebral venous thrombosis in Hong Kong. Cerebrovasc Dis 2001;11:282–3. 10.1159/000047652 [DOI] [PubMed] [Google Scholar]
- 15.Huss GP, Mattle H, Wessel K, et al. . [Neuro-Behçet’s syndrome: encephalitis and cerebral venous thrombosis--clinical aspects and neuroradiology of 5 cases]. Nervenarzt 1992;63:352–8. [PubMed] [Google Scholar]
- 16.Chan KH, Cheung RT, Liu WM, et al. . Cerebral venous thrombosis in a gentleman presenting with fever, convulsion and frontotemporal haemorrhages. J Clin Neurosci 2005;12:186–8. 10.1016/j.jocn.2004.03.013 [DOI] [PubMed] [Google Scholar]
- 17.Stam J. Thrombosis of the cerebral veins and sinuses. N Engl J Med 2005;352:1791–8. 10.1056/NEJMra042354 [DOI] [PubMed] [Google Scholar]