Abstract
Large to massive rotator cuff tears are challenging to repair, although there are several options for dealing with them. Among them, superior capsular reconstruction was recently introduced as an effective procedure for retaining the static stability of the shoulder joint and preventing the progression to cuff tear arthropathy. The purpose of this technique-based article is to describe a surgical option, called arthroscopic in situ superior capsular reconstruction, for large to massive rotator cuff tears using the long head of the biceps tendon.
Large to massive tears of rotator cuff tendons usually cause atrophy and fatty degeneration of the rotator cuff muscles and painful loss of shoulder function. Several treatment options for large to massive rotator cuff tears (RCTs) exist; they include arthroscopic partial repair,1, 2, 3 tuberoplasty,4, 5 debridement3, 6 with possible biceps tenotomy, tenodesis or augmentation,7, 8 tendon transfer,9, 10, 11 superior capsular reconstruction,12, 13, 14, 15, 16 patch augmentation,17, 18, 19, 20 bridging rotator cuff reconstruction with a graft,21 and reverse total shoulder arthroplasty.22, 23, 24 Despite all of these options, large to massive RCTs are still difficult to manage and treat effectively.
The superior capsule of the shoulder joint plays an important role as a static stabilizer of the glenohumeral joint. In patients with large to massive RCTs, the superior shoulder capsule is concomitantly torn. Biomechanically superior capsular defects have been shown to increase glenohumeral translation, particularly with superior translation at 5° and 30° of abduction.14 Mihata et al.15 enrolled 24 RCTs (11 large, 13 massive) and studied the clinical outcomes from superior capsular reconstruction (SCR) using the tensor fascia lata. The minimum follow-up was 2 years postsurgery. Range of motion (ROM) and acromiohumeral distance of the shoulder joint significantly increased, and functional scores also improved significantly. The results of this study indicated that arthroscopic superior capsular reconstruction could be an efficient tool to manage large to massive rotator cuff tears.
Also, because of the proximity of the long head of the biceps tendon (LHBT) to the rotator cuff, many trials have used the LHBT to support RTC repair.7, 8, 25 This Technical Note describes an arthroscopic in situ SCR with the LHBT by using a rerouting technique for large to massive RCTs (Video 1, Table 1).
Table 1.
Order of Steps With Pitfalls and Pearls
| Surgical Steps | Pitfalls | Pearls |
|---|---|---|
| Debridement of the soft tissue around the LHBT | Removal of the transverse humeral ligament catches the LHBT in the biceps groove | Removes synovitis, which can be a pain source, and makes the LHBT more mobile and easy to handle |
| Decortication of bone bed of footprint for rerouting the LHBT | With insufficient debridement, remnant bone can damage rerouted LHBT postoperatively and make poor biological healing | Has a tuberoplasty effect and can make posterior LHBT movement easier, Makes enough of a bone bed for LHBT and RC to be fixated biologically |
| Lateral insertion of anchor to fix the LHBT | Malpositioning of the anchor, anchor pullout, and greater tuberosity fracturing | Posteriorly re-routed LHBT can be an efficient static stabilizer for the GH joint and sutures finishing the LHBT fixation can be used again for RCR |
| One lasso-loop and two wrap-around ties were made at the lateral anchor | Insufficent suture technique, resulting in loss of LHBT fixation | Makes one lasso-loop first to grip the LHBT more powerfully so that the LHBT has enough fixation power, resulting in a downward press of the humeral head |
| Medial insertion of another anchor and fixation of the medial LHBT | Malpositioning of the anchor, anchor pullout, and humeral head fracture in the GH joint | Additional power for fixation of the LHBT and downward pressure on the humeral head |
| Insertion of an additional anchor just posterior to the lateral LHBT anchor | Malpositioning of the anchor, anchor pullout, and greater tuberosity fracture | Enough sutures can be provided for rotator cuff repair |
| Rotator cuff repair is performed with sutures from 3 anchors | Too tight repair of the less reducible rotator cuff can lead to poor outcome, including retear | Can perform a separate repair for the delaminated tear, and the LHBT can be used for articular side remnant cuff repair; LHBT can be used for RCR and provides a space-occupying effect |
GH, glenohumeral; LHBT, long head of biceps tendon; RC, rotator cuff; RCR, rotator cuff repair; SCR, superior capsular reconstruction.
Surgical Technique
Positioning and Examination of Glenohumeral Joint and Subacromial Space
Our patient was prepared in the usual manner—in the left lateral decubitus position with general endotracheal anesthesia. The operative arm was placed at 30° abduction and 20° forward flexion. Diagnostic arthroscopy was performed with 30° arthroscope viewing through a standard arthroscopic portal to examine the glenohumeral joint of the right shoulder. The posterior portal is used as the viewing portal and anterior portal is used as the working portal. The joint was routinely examined to detect any articular lesions on the supraspinatus tendon. The integrity of the LHBT was also checked. If the LHBT was completely torn, we could not perform this technique. The arthroscope was moved into the subacromial space through the posterior portal, which was similarly used for the examination of the glenohumeral joint and a bursectomy was performed by a shaver (Advantage Turbo; ConMed, Largo, FL) through the anterolateral portal. An acromioplasty was performed only for large sharp spurs. We used a laser-marked probe to assess the tear extent (Fig 1A).
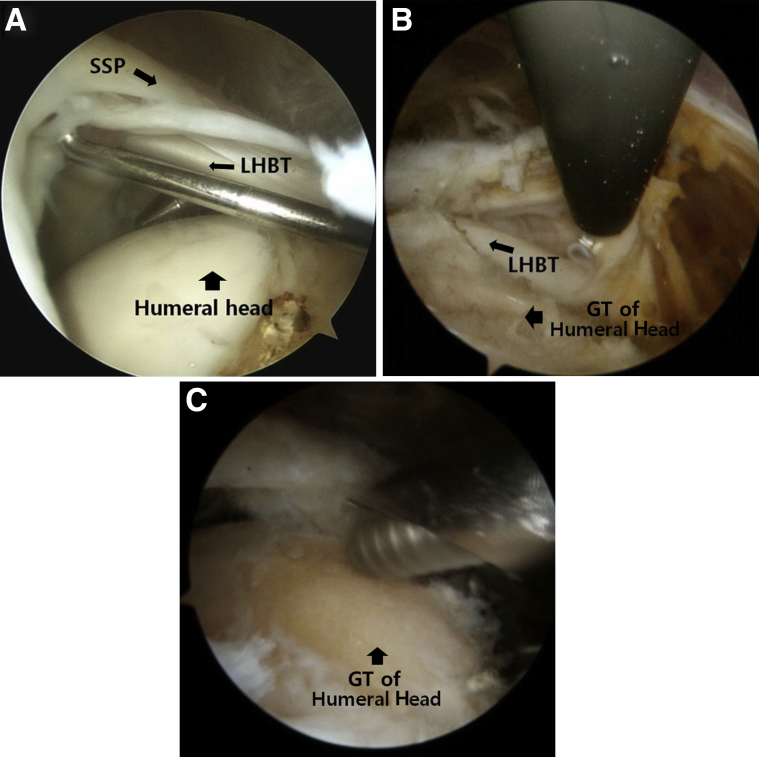
Fig 1.
Subacromial space of right shoulder viewing from the posterior portal (A). The extent of the tear was measured by a laser-marked probe. (B) To make the LHBT mobile and reroute the tendon posterolaterally, removal of the soft tissue around the LHBT, including the transverse humeral ligament, was performed with an electrocautery device (Vapr Suction Electrodes; Depuy Synthes Mitek). (C) The bone bed of the greater tuberosity of the humeral head was prepared through the anterolateral portal with careful use of a bone cutter blade (4.2-mm Tiger Sterling Arthroscopy blade; ConMed). (LHBT, long head of biceps tendon; SSP, supraspinatus tendon.)
Preparation of LHBT for Rerouting and Bone Bed of the Greater Tuberosity of the Humeral Head
To ensure muscle mobility and re-route the LHBT posterolaterally, we removed the soft tissue around the LHBT, including the transverse humeral ligament, using an electrocautery device (Vapr Suction Electrodes; DePuy Synthes Mitek, Raynham, MA; Fig 1B). The decortication of bone bed of the footprint was performed through the anterolateral portal with careful use of a bone-cutter blade (4.2-mm Tiger Sterling Arthroscopy blade; ConMed, Largo, FL; Fig 1C), until the cancellous bone of the general tuberosity (GT) of the humeral head is exposed enough. This bone bed of the GT of the humeral head is used for the biologic fixation of LHBT and rotator cuff to the bone. The mobility and integrity of the LHBT should be checked with a tendon grasper (Fig 2A). We used a retriever to posteriorly reposition the LHBT to the GT of the humeral head (Fig 2B).
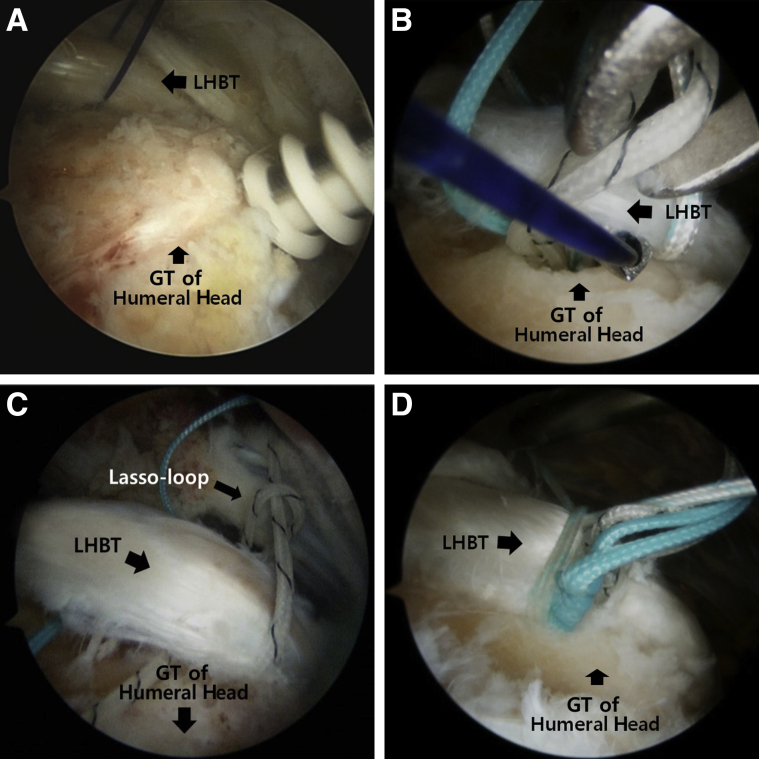
Fig 2.
(A) The mobility and integrity of the LHBT should be checked by a tendon grasper. (B) Trial to reposition the LHBT posteriorly to the greater tuberosity of the humeral head was performed by a retriever. (LHBT, long head of biceps tendon.)
Fixation of LHBT
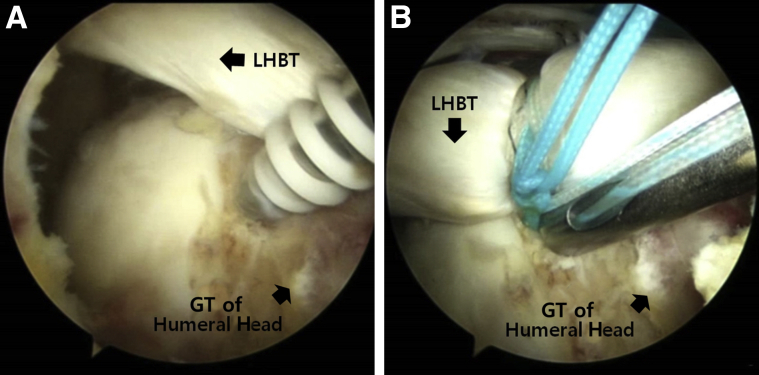
After anchor insertion (5.5-mm Healicoil; Smith & Nephew, Andover, MA; Fig 3A) at the midlateral aspect of footprint, we preloaded a suture hook (Linvatec, Largo, FL) with a No. 1 PDS (Ethicon, Somerville, NJ) and introduced the hook through the anterior portal to make a lasso-loop tie.26 The tip of the hook should pass through the body of the LHBT to make a lasso-loop around the LHBT to capture the tendon at the anchor site. The shuttle of the suture that is used to make the lasso-loop should not pass the tendon completely to make a loop at the body of the LHBT (Fig 3B). After making of the loop at the body of the LHBT, the end of the suture that formed the loop should pass through the loop to complete the lasso-loop (Fig 3C). And with the opposite part of the suture, ties are made 4 to 5 times to fix the LHBT. After making a lasso-loop tie, we made two more wrap-around ties to ensure successful fixation of the LHBT (Fig 3D). Similarly, the medial side of the LHBT was fixated by another anchor suture. At the junction of joint cartilage and the footprint, the medial suture anchor was inserted (Fig 4A). Then, the LHBT is securely fixed again at the medial site of the footprint in the same manner using one lasso-loop tie, and two wrap-around ties were also made (Fig 4B). All the strands should remain uncut for further suture of the torn rotator cuff tendon. This is the final procedure of arthroscopic in situ SCR using an LHBT procedure via a re-routing technique. A tenotomy of the LHBT can be performed at the distal aspect of the lateral anchor if tendon integrity is not sufficient to maintain itself.
Fig 3.
(A) Lateral anchor insertion (5.5-mm Healicoil; Smith & Nephew) at the midlateral portion of the footprint for LHBT fixation was performed. (B) A suture hook (Linvatec) which was preloaded with No. 1 PDS (Ethicon) was introduced through the anterior portal to make a lasso-loop tie26 and then was passed through the body of the LHBT. (C) One lasso-loop tie was made at the lateral anchor. (D) Two more wrap-around ties were made to ensure LHBT fixation after making the lasso-loop tie. (LHBT, long head of biceps tendon.)
Fig 4.
(A) At the junction of joint cartilage and the footprint, the insertion of medial side anchor was performed. (B) One lasso-loop tie and two wrap-around ties were then made for the medial fixation of the LHBT. (LHBT, long head of biceps tendon.)
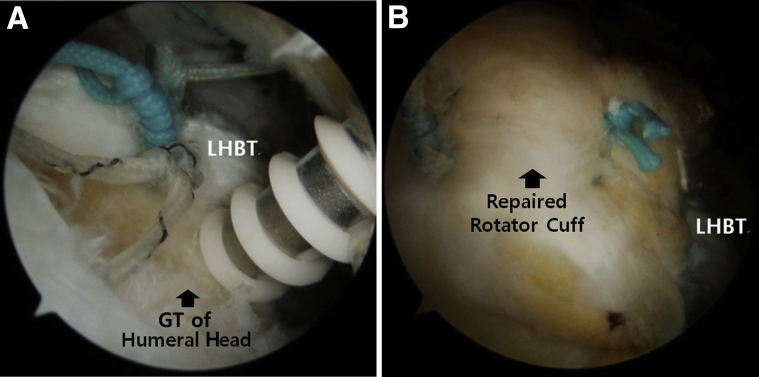
Rotator Cuff Repair
After finishing the arthroscopic in situ SCR with the LHBT, rotator cuff repair should be performed. Rotator cuff repair can be performed using the sutures from the two previously inserted anchors used to fix the LHBT and an additional anchor that can be inserted into the posterolateral aspect of the GT of the humeral head just behind the LHBT for posterior RCT (Fig 5). In the case of delaminated rotator cuff tear, the articular side rotator cuff can be repaired with sutures from the previously medially inserted anchor for LHBT fixation. For delaminated tears, separate double-row repair or separate bridge repair can be performed.27 And for massive rotator cuff tears, which cannot be covered by remnant cuff tissue, partial repair is acceptable through arthroscopic in situ SCR with the LHBT.
Fig 5.
(A) An additional anchor can be inserted posterolaterally into the greater tuberosity of the humeral head just behind the LHBT for repair of the posterior rotator cuff. (B) The sutures from the two previously inserted anchors that serve to fix the LHBT can be used to repair the rotator cuff. (LHBT, long head of biceps tendon.)
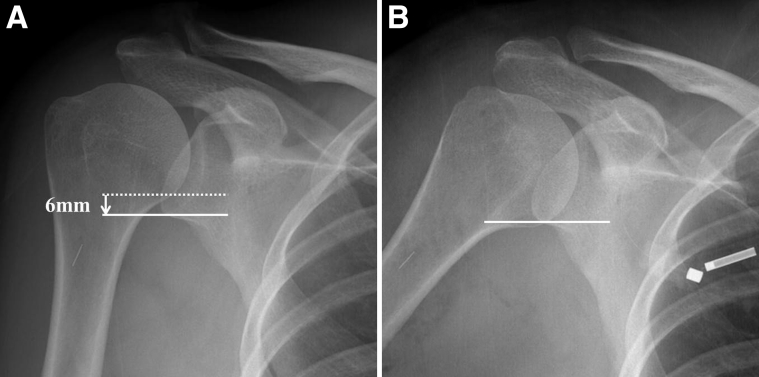
Compared with preoperative radiographs (Fig 6A), our patient's immediate postoperative radiograph (Fig 6B) showed significantly increased acromiohumeral distance. This suggests that arthroscopic in situ SCR using the LHBT may improve static stability for the glenohumeral joint of the shoulder with large to massive RCTs.
Fig 6.
Compared with preoperative radiograph (A), immediate postoperative radiograph (B) showed that humeral head migrated inferiorly about 7 mm.
Postoperative Care
Postoperative pain is usually controlled by an interscalene block or interscalene nerve catheter. Postoperative rehabilitation initially focuses on limited and protected passive range of motion, with an abduction brace. Because of the re-routing and anchoring of the LHBT, even passive motion of the elbow is prohibited during the entire brace application period. Passive motion starts 4 to 6 weeks postoperatively after removal of the brace. Pendulum and pulley exercises start just after brace removal. Active range of motion typically starts after 8 weeks, and external rotation strengthening exercises start after 12 weeks. The main rehabilitation goals are to improve active shoulder motion and to facilitate and maintain the biomechanics of glenohumeral joints.
Discussion
SCR was recently introduced and has become popular in many centers.12, 13, 15, 16 The superior capsule is important for stability of the glenohumeral joint. The rotator cuff is a dynamic stabilizer; it helps to reinforce the capsule and gives strength to overhead movements. On the other hand, the superior capsule is considered to be a key static stabilizer. This concept explains why the SCR can relieve severe pain and improve disability from irreparable massive rotator cuff tears. In a cadaver study, Ishihara et al.14 suggested that a defect in the superior capsule, as seen in massive cuff tears, can increase glenohumeral translations in all directions. This means that alterations in the static stability of the shoulder joint due to the absence of a superior capsule can cause progression to cuff tear arthropathy. In their original description, Mihata et al.15 reported good short-term results from this reconstructive procedure. They found this to be a safe and reproducible procedure.
We demonstrated an arthroscopic SCR technique using the LHBT instead of the autologous tensor fascia lata15 in this report. We prefer the LHBT to the fascia lata autograft, which Mihata et al.15 originally reported. There are many advantages of using LHBT instead of the autologous tensor fascia lata15 or dermal allograft.12, 13, 16 It can be used very easily during arthroscopic shoulder surgery because of the proximity of this tendon and because donor-site morbidity can be avoided. Furthermore, our technique of re-routing the LHBT creates a downward force to the humeral head; thus, postoperative radiographs show down-migration of the humeral head after our procedure (Fig 6). Also, because this procedure is performed just in the shoulder joint, the risk of infection can be reduced and the operation time is reduced by skipping the harvesting of a graft tendon or trimming the interposition tissues. Most importantly, we expect that our technique is quite effective for preventing progression into cuff tear arthropathy for large to massive RCTs, not only because our technique includes coincident repair of the rotator cuff but also because of the downward force induced by the rerouted LHBT and the space-occupying effect of the SCR. The LHBT is fixated with a medial and lateral anchor and has an LHB tenodesis effect as a result. Therefore, this technique yields additional therapeutic effects for patients who have biceps pathologies, such as biceps tendinitis or instabilities. On the other hand, because of rerouting of LHBT, the biceps tendon would be a little bit stretched and increase the tension. This might cause the pain along the biceps muscle at the early stage after the surgery. Further evaluation is needed to distinguish the origin of postoperative pain. And another limitation of this technique is that in the case of completely torn LHBT, this procedure cannot be indicated. So, to perform this technique, preoperative evaluation of LHBT by MRI or intraoperative thorough glenohumeral joint examination should be done (Table 2).
Table 2.
Advantages and Disadvantages of Arthroscopic In Situ SCR Using LHBT Compared With Using Original SCR
| Advantages | Disadvantages |
|---|---|
| 1. No outside joint procedure 2. Reduces operation time and the risk of infection due to intra–shoulder joint procedure 3. LHBT tissue can be used as a scaffold during RCR 4. Technically easier than SCR with TFL or allodermal patch 5. No donor site morbidity 6. LHB tenodesis effect |
1. Possible pain from stretched LHBT 2. Not feasible for patients whose LHBT is completely torn |
LHBT, long head of biceps tendon; RCR, rotator cuff tear; SCR, superior capsular reconstruction; TFL, tensor fascia lata.
To summarize, SCR is considered a reasonable treatment option for younger patients with posterosuperior large to massive RCTs who want to avoid tendon transfer or reverse total shoulder arthroplasty. Finally, our technique, arthroscopic in situ SCR using LHBT, can be an effective procedure for patients to avoid progression to cuff tear arthropathy. Further clinical trials are needed to investigate the long-term benefits of this technique, as well as to determine the best indications for this procedure.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Our patient was in the left lateral decubitus position with general endotracheal anesthesia. The right arm was placed at 30° abduction and 20° forward flexion. Diagnostic arthroscopy was performed with 30° arthroscope viewing through a standard arthroscopic portal to examine the glenohumeral joint. The integrity of the LHBT was checked. The arthroscope was moved into the subacromial space. To ensure muscle mobility and reroute the LHBT posterolaterally, we removed the soft tissue around the LHBT, including the transverse humeral ligament, using an electrocautery device. The decortication of bone bed of the greater tuberosity of the humeral head was performed through the anterolateral portal with careful use of a bone-cutter blade. The mobility and integrity of the LHBT should be checked with a tendon grasper for rerouting of the LHBT. After the suture anchor insertion on the lateral portion of the footprint, we introduced the hook through the anterior portal to make a lasso-loop tie. After making a lasso-loop tie, we made two more wrap-around ties to ensure successful fixation of the LHBT. Similarly, at the junction of the joint cartilage and the footprint, the additional suture anchor is inserted for the medial secure fixation of LHBT. One lasso-loop tie and two wrap-around ties were also made. All the strands should remain uncut for further suture of the torn rotator cuff tendon. This is the final procedure of arthroscopic in situ SCR using an LHBT procedure via a rerouting technique. A tenotomy of the LHBT can be performed at the distal aspect of the lateral anchor if tendon integrity is not sufficient to maintain itself. After finishing the arthroscopic in situ SCR with the LHBT, rotator cuff repair should be performed. Rotator cuff repair can be performed using the sutures from the two previously inserted anchors used to fix the LHBT and an additional anchor that can be inserted into the posterolateral aspect of the greater tuberosity of the humeral head just behind the LHBT for posterior RCT. And for massive rotator cuff tears, which cannot be covered by remnant cuff tissue, partial repair is acceptable through arthroscopic in situ SCR with the LHBT. (LHBT, long head of biceps tendon; RCT, rotator cuff tear; SCR, superior capsular reconstruction.)
References
- 1.Pandey R., Tafazal S., Shyamsundar S., Modi A., Singh H.P. Outcome of partial repair of massive rotator cuff tears with and without human tissue allograft bridging repair. Shoulder Elbow. 2017;9:23–30. doi: 10.1177/1758573216665114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Castricini R., Galasso O., Riccelli D.A. Arthroscopic partial repair of irreparable, massive rotator cuff tears. Arthrosc Tech. 2017;6:e143–e147. doi: 10.1016/j.eats.2016.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Franceschi F., Papalia R., Vasta S., Leonardi F., Maffulli N., Denaro V. Surgical management of irreparable rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2015;23:494–501. doi: 10.1007/s00167-012-2317-7. [DOI] [PubMed] [Google Scholar]
- 4.Park J.G., Cho N.S., Song J.H., Baek J.H., Rhee Y.G. Long-term outcome of tuberoplasty for irreparable massive rotator cuff tears: Is tuberoplasty really applicable? J Shoulder Elbow Surg. 2016;25:224–231. doi: 10.1016/j.jse.2015.07.025. [DOI] [PubMed] [Google Scholar]
- 5.Lee B.G., Cho N.S., Rhee Y.G. Results of arthroscopic decompression and tuberoplasty for irreparable massive rotator cuff tears. Arthroscopy. 2011;27:1341–1350. doi: 10.1016/j.arthro.2011.06.016. [DOI] [PubMed] [Google Scholar]
- 6.Hawi N., Schmiddem U., Omar M. Arthroscopic debridement for irreparable rotator cuff tears. Open Orthop J. 2016;10:324–329. doi: 10.2174/1874325001610010324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cho N.S., Yi J.W., Rhee Y.G. Arthroscopic biceps augmentation for avoiding undue tension in repair of massive rotator cuff tears. Arthroscopy. 2009;25:183–191. doi: 10.1016/j.arthro.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 8.Rhee Y.G., Cho N.S., Lim C.T., Yi J.W., Vishvanathan T. Bridging the gap in immobile massive rotator cuff tears: Augmentation using the tenotomized biceps. Am J Sports Med. 2008;36:1511–1518. doi: 10.1177/0363546508316020. [DOI] [PubMed] [Google Scholar]
- 9.Elhassan B.T., Alentorn-Geli E., Assenmacher A.T., Wagner E.R. Arthroscopic-assisted lower trapezius tendon transfer for massive irreparable posterior-superior rotator cuff tears: Surgical technique. Arthrosc Tech. 2016;5:e981–e988. doi: 10.1016/j.eats.2016.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elhassan B.T., Wagner E.R., Werthel J.D. Outcome of lower trapezius transfer to reconstruct massive irreparable posterior-superior rotator cuff tear. J Shoulder Elbow Surg. 2016;25:1346–1353. doi: 10.1016/j.jse.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 11.Petriccioli D., Bertone C., Marchi G. Recovery of active external rotation and elevation in young active men with irreparable posterosuperior rotator cuff tear using arthroscopically assisted latissimus dorsi transfer. J Shoulder Elbow Surg. 2016;25:e265–e275. doi: 10.1016/j.jse.2015.12.011. [DOI] [PubMed] [Google Scholar]
- 12.Burkhart S.S., Denard P.J., Adams C.R., Brady P.C., Hartzler R.U. Arthroscopic superior capsular reconstruction for massive irreparable rotator cuff repair. Arthrosc Tech. 2016;5:e1407–e1418. doi: 10.1016/j.eats.2016.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hirahara A.M., Adams C.R. Arthroscopic superior capsular reconstruction for treatment of massive irreparable rotator cuff tears. Arthrosc Tech. 2015;4:e637–e641. doi: 10.1016/j.eats.2015.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ishihara Y., Mihata T., Tamboli M. Role of the superior shoulder capsule in passive stability of the glenohumeral joint. J Shoulder Elbow Surg. 2014;23:642–648. doi: 10.1016/j.jse.2013.09.025. [DOI] [PubMed] [Google Scholar]
- 15.Mihata T., Lee T.Q., Watanabe C. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 16.Petri M., Greenspoon J.A., Millett P.J. Arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthrosc Tech. 2015;4:e751–e755. doi: 10.1016/j.eats.2015.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ciampi P., Scotti C., Nonis A. The benefit of synthetic versus biological patch augmentation in the repair of posterosuperior massive rotator cuff tears: A 3-year follow-up study. Am J Sports Med. 2014;42:1169–1175. doi: 10.1177/0363546514525592. [DOI] [PubMed] [Google Scholar]
- 18.Petri M., Greenspoon J.A., Moulton S.G., Millett P.J. Patch-augmented rotator cuff repair and superior capsule reconstruction. Open Orthop J. 2016;10:315–323. doi: 10.2174/1874325001610010315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Petri M., Warth R.J., Horan M.P., Greenspoon J.A., Millett P.J. Outcomes after open revision repair of massive rotator cuff tears with biologic patch augmentation. Arthroscopy. 2016;32:1752–1760. doi: 10.1016/j.arthro.2016.01.037. [DOI] [PubMed] [Google Scholar]
- 20.Yoon J.P., Chung S.W., Kim J.Y. Outcomes of combined bone marrow stimulation and patch augmentation for massive rotator cuff tears. Am J Sports Med. 2016;44:963–971. doi: 10.1177/0363546515625044. [DOI] [PubMed] [Google Scholar]
- 21.Lewington M.R., Ferguson D.P., Smith T.D., Burks R., Coady C., Wong I.H. Graft utilization in the bridging reconstruction of irreparable rotator cuff tears: A systematic review. Am J Sports Med. 2017 doi: 10.1177/0363546517694355. 363546517694355. [DOI] [PubMed] [Google Scholar]
- 22.Al-Hadithy N., Domos P., Sewell M.D., Pandit R. Reverse shoulder arthroplasty in 41 patients with cuff tear arthropathy with a mean follow-up period of 5 years. J Shoulder Elbow Surg. 2014;23:1662–1668. doi: 10.1016/j.jse.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 23.Hartzler R.U., Steen B.M., Hussey M.M. Reverse shoulder arthroplasty for massive rotator cuff tear: Risk factors for poor functional improvement. J Shoulder Elbow Surg. 2015;24:1698–1706. doi: 10.1016/j.jse.2015.04.015. [DOI] [PubMed] [Google Scholar]
- 24.Tokish J.M., Alexander T.C., Kissenberth M.J., Hawkins R.J. Pseudoparalysis: A systematic review of term definitions, treatment approaches, and outcomes of management techniques. J Shoulder Elbow Surg. 2017;26:e177–e187. doi: 10.1016/j.jse.2017.02.024. [DOI] [PubMed] [Google Scholar]
- 25.Obma P.R. Free biceps tendon autograft to augment arthroscopic rotator cuff repair. Arthrosc Tech. 2013;2:e441–e445. doi: 10.1016/j.eats.2013.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lafosse L., Van Raebroeckx A., Brzoska R. A new technique to improve tissue grip: “The lasso-loop stitch”. Arthroscopy. 2006;22:1246.e1241–1246.e1243. doi: 10.1016/j.arthro.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 27.Kim Y.S., Lee H.J., Jin H.K., Kim S.E., Lee J.W. Conventional en masse repair versus separate double-layer double-row repair for the treatment of delaminated rotator cuff tears. Am J Sports Med. 2016;44:1146–1152. doi: 10.1177/0363546516628869. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Our patient was in the left lateral decubitus position with general endotracheal anesthesia. The right arm was placed at 30° abduction and 20° forward flexion. Diagnostic arthroscopy was performed with 30° arthroscope viewing through a standard arthroscopic portal to examine the glenohumeral joint. The integrity of the LHBT was checked. The arthroscope was moved into the subacromial space. To ensure muscle mobility and reroute the LHBT posterolaterally, we removed the soft tissue around the LHBT, including the transverse humeral ligament, using an electrocautery device. The decortication of bone bed of the greater tuberosity of the humeral head was performed through the anterolateral portal with careful use of a bone-cutter blade. The mobility and integrity of the LHBT should be checked with a tendon grasper for rerouting of the LHBT. After the suture anchor insertion on the lateral portion of the footprint, we introduced the hook through the anterior portal to make a lasso-loop tie. After making a lasso-loop tie, we made two more wrap-around ties to ensure successful fixation of the LHBT. Similarly, at the junction of the joint cartilage and the footprint, the additional suture anchor is inserted for the medial secure fixation of LHBT. One lasso-loop tie and two wrap-around ties were also made. All the strands should remain uncut for further suture of the torn rotator cuff tendon. This is the final procedure of arthroscopic in situ SCR using an LHBT procedure via a rerouting technique. A tenotomy of the LHBT can be performed at the distal aspect of the lateral anchor if tendon integrity is not sufficient to maintain itself. After finishing the arthroscopic in situ SCR with the LHBT, rotator cuff repair should be performed. Rotator cuff repair can be performed using the sutures from the two previously inserted anchors used to fix the LHBT and an additional anchor that can be inserted into the posterolateral aspect of the greater tuberosity of the humeral head just behind the LHBT for posterior RCT. And for massive rotator cuff tears, which cannot be covered by remnant cuff tissue, partial repair is acceptable through arthroscopic in situ SCR with the LHBT. (LHBT, long head of biceps tendon; RCT, rotator cuff tear; SCR, superior capsular reconstruction.)