Abstract
Immune checkpoint blockade (CPB) utilizing such agents as ipilimumab, nivolumab, or pembrolizumab has revolutionized melanoma therapy and has seen continued utilization in numerous other malignancies in recent years. However, these agents come at the price of inflammatory immune-related adverse events. Despite the increasing recognition of biochemical thyroid dysfunction associated with CPB, information regarding potential imaging findings is sparse. We describe the first 2 cases of acute thyroiditis following CPB presenting as diffuse thyromegaly documented by computed tomography, ultrasound, and iodine uptake imaging. Given the rise in the use of CPB, it is important for radiologists to recognize potential imaging manifestations of therapy immune-related adverse events to avoid erroneous diagnosis and to prompt the biochemical investigation of thyroid function.
Keywords: Thyroiditis, Ipilimumab, Nivolumab, Monoclonal antibodies, Hyperthyroidism
Introduction
Immune checkpoint blockade (CPB) targeting CTLA-4 with ipilimumab or PD1 with nivolumab or pembrolizumab has revolutionized advanced melanoma therapy. Durable responses and prolonged survival come at the price of inflammatory immune-related adverse events (irAEs), including dermatitis, colitis, thyroiditis, hypophysitis, hepatitis, pneumonitis, and nephritis. Serious irAEs collectively affect approximately 20% of patients receiving anti-PD1 therapy, 30% of patients receiving ipilimumab, and 55% of patients receiving ipilimumab and nivolumab combination therapy [1]. Thyroiditis, associated with hypothyroidism de novo or following transient hyperthyroidism, affects approximately 9% and 15% of patients receiving anti-PD1 alone or in combination with ipilimumab, respectively [1]. Despite the increasing recognition of biochemical thyroid dysfunction associated with CPB, information regarding potential imaging findings is sparse. Herein, we describe the first 2 cases of acute thyroiditis following CPB presenting as diffuse thyromegaly documented by computed tomography (CT), ultrasound, and iodine uptake imaging.
Case reports
Case 1
A 51-year-old woman underwent wide local excision and left cervical lymphadenectomy for a BRAF V600E-mutated left frontal scalp melanoma involving 1 preauricular lymph node (stage IIIA). Two years later, metastases to the lungs, the liver, and the brain were initially treated with dabrafenib and trametinib kinase inhibitors. After 4 months, these drugs were discontinued for progression in the brain treated with single-fraction radiotherapy followed by combination immune CPB with ipilimumab at 3 mg/kg and nivolumab at 1 mg/kg. Three days after the first dose, the patient experienced neck swelling, tenderness, and fatigue without palpitations, anxiety, or other thyroid storm symptoms. Thyroid function testing revealed a free T4 increase from 1.48 ng/dL at baseline to 2.95 ng/dL (normal ≤1.57 ng/dL), a free T3 of 4.4 pg/mL (normal ≤4.2 pg/mL, baseline unavailable), and a thyroid stimulating hormone (TSH) decrease from 0.503 to 0.065 µIU/mL (normal ≥0.35 µIU/mL) consistent with transient hyperthyroidism from immune necrosis.
CT of the neck with iodinated intravenous contrast (Fig. 1A and B) revealed a significantly enlarged thyroid gland with a heterogeneous enhancement and discrete areas of hypodensity with marginal enhancement. The right lobe of the thyroid measured 4.0 × 3.7 × 6.6 cm and the left lobe measured 3.4 × 3.3 × 6.5 cm. Comparison with a chest CT from less than 4 months earlier (Fig. 1C) showed these areas of hypoattenuation to be new, and the gland had more than tripled in volume. Ultrasound (Fig. 2A) showed a heterogeneous thyroid gland with a slight increase in vascularity. One month later, a radioactive iodine (I-131) uptake test (Fig. 2B) demonstrated only a faint uptake of radiotracer within the thyroid gland with a 4-hour thyroid uptake of 0.82%. Repeat CT of the neck with contrast 3 months later showed a near-complete resolution of thyroid heterogeneity and a significant reduction in the size of the gland.
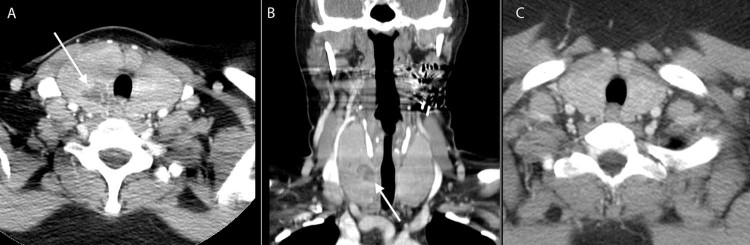
Fig. 1.
Case 1: Axial (A) and coronal (B) computed tomographies of the neck with intravenous iodinated contrast show a diffuse enlargement of the thyroid gland with internal areas of necrosis (arrow). Noncontrast chest computed tomography from less than 4 months earlier (C) shows a normal appearance of the thyroid gland.
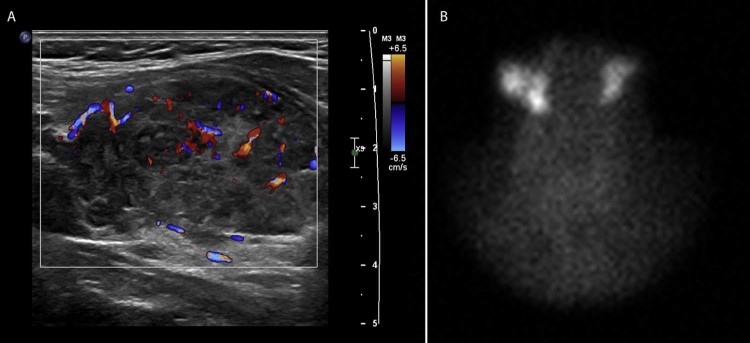
Fig. 2.
Case 1: Follow-up thyroid ultrasound (A) shows increased vascularity within a heterogeneous and enlarged thyroid gland. Radioactive iodine (I-131) uptake test (B) performed 1 month later shows an uptake within normal salivary tissue and virtually no uptake within the thyroid gland.
Symptoms gradually improved over a few weeks despite continued ipilimumab and nivolumab without steroids. Repeat thyroid function testing at 1 month revealed that FT4 decreased to 0.61 ng/dL, FT3 decreased to 1.2 pg/mL, and TSH increased to 57.4 µIU/mL, signaling a conversion to hypothyroidism requiring levothyroxine. The patient remained alive with excellent performance status 8 months after starting immunotherapy.
Case 2
A 46-year-old woman underwent a wide local excision and right axillary lymphadenectomy for a BRAF wild-type right anterior chest melanoma involving a single sentinel lymph node (stage IIIA). The patient received 1 month of high-dose adjuvant interferon and did well for 8 years until pulmonary metastases were discovered. Immune CPB was initiated with ipilimumab at 3 mg/kg, nivolumab at 1 mg/kg, and granulocyte macrophage colony-stimulating factor subcutaneously. Three days after the first dose, the patient presented to the emergency department with painless neck swelling and no other symptoms. Neck CT with iodinated intravenous contrast (Fig. 3A and B) showed a diffuse enlargement and a slight diffuse hypoattenuation of the thyroid gland with no areas of suspected necrosis. The thyroid gland measured 2.2 × 3.1 × 6.0 cm on the right and 2.2 × 3.0 × 5.0 cm on the left, more than doubling in volume compared with a CT from 10 days earlier (Fig. 3C).
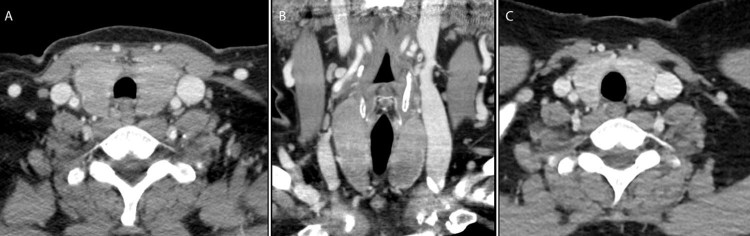
Fig. 3.
Case 2: Axial (A) and coronal (B) computed tomographies of the neck with intravenous iodinated contrast also show a diffuse enlargement of the thyroid gland with a relatively decreased attenuation throughout, but no areas of visible necrosis. Axial postcontrast computed tomography of the neck obtained 10 days earlier (C) shows a normal appearance of the thyroid gland.
Laboratory testing was performed on suspicion of treatment-related thyroiditis, showing an increase in TSH from 1.68 µIU/mL at baseline to 2.82 µIU/mL. FT4 and FT3 were both normal. Additionally, the patient was noted to have a mild elevation of troponin I with a normal electrocardiogram. Neck swelling spontaneously improved, but high-dose prednisone was initiated 2 weeks later for apparent treatment-related myocarditis with rising troponin I and creatine kinase-MB, as well as intractable nausea. Further immunotherapy was withheld. Repeat neck CT 2 months after the onset of swelling showed a return of the gland to normal appearance, but after 2 additional months, TSH increased to 10.5 µIU/mL (nL ≤ 5.5), so levothyroxine was initiated. The patient remained clinically well 6 months after the initiation of immune CPB.
Discussion
Previous literature has documented the presence of biochemical thyroid abnormalities with immune CPB [1], [2]. We describe 2 cases of patients presenting with acute anterior neck swelling and radiographic evidence of thyroiditis within 3 days of initiating combination CPB. To our knowledge, this is the first report highlighting CT, ultrasound, and radioactive iodine uptake findings in patients with an acute autoimmune thyroiditis presenting as diffuse thyromegaly from CPB.
In our series of patients, the typical features on neck CT included a diffuse enlargement of the gland with associated hypoattenuation. One patient had areas of ring enhancement likely related to gland necrosis. On ultrasound, the gland was diffusely heterogeneous with an increase in vascularity. Radioactive iodine uptake was significantly reduced in the setting of thyrotoxicosis, consistent with subacute thyroiditis. The gland returned to a normal appearance on follow-up CT in 2-3 months.
PD-1 and CTLA-4 blockades continue to emerge as effective therapies against melanoma, Hodgkin lymphoma, and carcinomas of the lung, kidney, bladder, Merkel cells, and head and neck. These monoclonal antibodies boost the immune response against cancer cells by targeting T-cell proteins involved in immune tolerance. Unfortunately, irAEs against normal tissues, commonly the thyroid gland, are possible. Consistent with biochemical thyroiditis reports, steroid immune suppression is not required for acute thyromegaly. Swelling spontaneously resolves in weeks, although subsequent thyroid hormone supplementation may become necessary.
Given the rise in the use of CPB, it is important for radiologists to recognize potential imaging manifestations of therapy irAEs. Although the incidence of associated thyroid abnormalities on imaging is unknown, an awareness of this entity is important to avoid erroneous diagnosis and to prompt biochemical investigation of the thyroid function.
Footnotes
Ethical Standards: We declare that all human and animal studies have been approved by our institutional review board meeting institutional standards for a case series and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. For this type of study, formal consent is not required.
Competing Interests: The authors have declared that no competing interests exist.
Patient Consent: Requirement for informed consent was waived by the institutional review board for this retrospective case study.
Author Contributions: E.M.—conception, literature review, drafting of the article, critical revision, and final approval; B.W.—literature review, drafting of the article, critical revision, and final approval; R.C.—conception, literature review, critical revision, and final approval.
References
- 1.Abdel-Wahab N., Shah M., Suarez-Almazor M.E. Adverse events associated with immune checkpoint blockade in patients with cancer: a systematic review of case reports. PLoS ONE. 2016;11(7):e0160221. doi: 10.1371/journal.pone.0160221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morganstein D.L., Lai Z., Spain L., Diem S., Levine D., Mace C. Thyroid abnormalities following the use of cytotoxic T-lymphocyte antigen-4 and programmed death receptor protein-1 inhibitors in the treatment of melanoma. Clin Endocrinol (Oxf) 2017;86:614–620. doi: 10.1111/cen.13297. [DOI] [PubMed] [Google Scholar]