Abstract
Background
The Centers for Medicare and Medicaid Services publicly reports hospital risk-standardized readmission rates (RSRRs) as a measure of quality and performance; mischaracterizations may occur because observation stays are not captured by current measures.
Objectives
To describe variation in hospital use of observation stays, the relationship between hospitals observation stay use and RSRRs.
Methods
Cross-sectional analysis of Medicare fee-for-service beneficiaries discharged after acute myocardial infarction (AMI), heart failure, or pneumonia between July 2011 and June 2012. We calculated three hospital-specific 30 day outcomes: 1) observation rate, the proportion of all discharges followed by an observation stay without a readmission; 2) observation proportion, the proportion of observation stays among all patients with an observation stay or readmission; and 3) RSRR.
Results
For all 3 conditions, hospitals’ observation rates were < 2.5% and observation proportions were < 12%, although there was variation across hospitals, including 28% of hospital with no observation stay use for AMI, 31% for heart failure, and 43% for pneumonia. There were statistically significant, but minimal, correlations between hospital observation rates and RSRRs: AMI (r=−0.02), heart failure (r=−0.11), and pneumonia (r=−0.02) (p<0.001). There were modest inverse correlations between hospital observation proportion and RSRR: AMI (r=−0.34), heart failure (r=−0.26), and pneumonia (r=−0.21) (p<0.001). If observation stays were included in readmission measures, <4% of top performing hospitals would be recategorized as having average performance.
Conclusions
Hospitals’ observation stay use in the post-discharge period is low, but varies widely. Despite modest correlation between the observation proportion and RSRR, counting observation stays in readmission measures would minimally impact public reporting of performance.
Keywords: Patient Readmission, Quality Indicators, Healthcare, Observation Services, Medicare
Background
Between 2007 and 2012, the use of hospital observation stays for short-term acute care treatment and assessment grew by 57% among Medicare beneficiaries.1 While observation care was initially designed to provide an efficient alternative to inpatient hospitalization for patients with select diagnoses requiring a brief evaluation, such as chest pain or asthma, observation stays are now used for a wide variety of diagnoses.2,3 Concurrent with broader use of observation stays, recent work has also demonstrated wide geographic and hospital-level variation in the use of observation stays.1,3-5
As use of observation stays continues to grow, concerns have been raised about their implications for hospital quality and performance measurement,6-8 particularly the measurement of hospital readmission rates, which is now a principal part of national public reporting and accountability programs administered by the Centers for Medicare and Medicaid Services (CMS). These measures do not count observation stays within 30 days of inpatient discharge as readmissions. Although observation stays are expected to last no more than 24 hours, 40% are for longer durations of observation, suggesting that these stays may reflect ineffective care transitions, and may be very similar to short-stay inpatient readmissions.4,9 Previous evaluations of variation in hospitals’ use of observation stays have neither distinguished between general observation stays and those occurring after hospital discharge nor explicitly focused on the medical conditions which are the focus of the CMS's Hospital Readmission Reduction Program. Moreover, although recent data have suggested a modest but notable decline in hospital readmission rates that were not offset by an equivalent increase in post-discharge observation stays nationally,1,10,11 these findings did not explore the degree to which individual hospital's use of observation stays could impact performance measurement of hospital readmission rates.
Accordingly, we sought to characterize the use of post-discharge observations stays and the relevance for hospital readmission measurement. Specifically, we describe hospital-level variation in the use of observation stays among Medicare beneficiaries in the post-discharge period after hospitalization for acute myocardial infarction (AMI), heart failure, and pneumonia. In addition, we examined whether these post-discharge observation stays were similar in diagnosis and length of stay to hospital readmissions and whether hospital characteristics were associated with use of observation stays. We also evaluate the association between observation stay use and hospital-level estimates of readmission rates, including an assessment of the impact of including observation stays as a readmission measure outcome on the classification of hospital performance.
Methods
Design and Dataset
This study is a cross-sectional analysis of Medicare beneficiaries hospitalized and discharged alive for AMI, heart failure, and pneumonia. We used Medicare hospital inpatient, outpatient, and physician Standard Analytic Files to identify admissions, readmissions, observation stays as well as the inpatient and outpatient diagnosis codes necessary to assign each hospitalization to a disease cohort based on principal discharge diagnosis. The cohort is consistent with CMS's readmission measures, using International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes to identify AMI, heart failure, and pneumonia discharges between July 2011 and June 2012.12-14 We restricted the sample to patients enrolled in fee-for-service Medicare Parts A and B for 12 months prior to index hospitalization, in order to maximize our ability to capture diagnoses for risk adjustment, and who were discharged alive and maintained fee-for-service coverage for at least 30 days following hospital discharge. We excluded patients discharged against medical advice and considered contiguous admissions in a transfer chain as a single admission. Only short-term acute care hospitals with 25 condition-specific index hospital admissions were included in this analysis for consistency with publicly reported measures.12-15
Measurement of Observation Stays
We measured observation stays in the 30 days post-discharge from index hospitalization. Observation stays were defined as any hospital outpatient claim for observation services using billing code G0378 concurrent with hospital outpatient revenue center codes 0760 or 0762. This definition is similar to prior work and was developed based on expert input to be specific to the use of observation stays for acute, unscheduled hospital care. Observation stay length of stay was measured in hours based on the number of G0378 units billed.
We identified observations stays that occurred after an index admission and in the absence of a readmission in order to only identify a return to the hospital not already captured by CMS readmission measures. Consistent with the current measures, only one observation stay was counted towards the outcome in patients with multiple observation stays within the 30 days following hospital discharge. Therefore, each index admission was found to have a readmission, an observation stay (and no readmission) or neither. For descriptive purposes, the principal diagnosis for observation stays were grouped into meaningful clinical categories using the Clinical Classification Software (CCS) developed by the Agency for Healthcare Research and Quality.16
Hospital-level use of observation stays was measured by calculating two measures: the post-discharge observation stay rate and the post-discharge observation stay proportion. Both measures have been previously used to describe hospital observation use, but not applied to the post-discharge period.2,5 The post-discharge observation stay rate is the percentage of index admissions followed by an observation stay without readmission (hereafter referred to as the observation rate). The post-discharge observation proportion is the hospital-level proportion of post-discharge observation stays among the sum of post-discharge observation stays and inpatient readmissions (hereafter referred to as the observation proportion). This metric was constructed to describe the relative use of hospital-level observation stays compared to inpatient readmissions among post-discharge returns to the hospital. In addition, measurement of the hospital observation proportion also ensures that hospitals with low post-discharge observation rates and readmission rates as a result of lower-admission propensity, transfer decisions, or lower hospitalization volumes are not assumed to have low observation stay use.
Measurement of Readmissions
Consistent with current CMS measures, readmissions were defined as the first unplanned inpatient hospitalization within the 30-day period following discharge.12-14 Subsequent inpatient hospitalizations following 30 days from discharge were considered as distinct index admissions if they met inclusion criteria. For descriptive analyses of discharge diagnosis only, we defined short-stay inpatient readmission as having a hospital length of stay of 0 or 1 days to identify inpatient hospitalizations most comparable to observation.
Each hospital's Risk-Standardized Readmission Rate (RSRR) was calculated using the same methodology used for measures that have been endorsed by the National Quality Forum and used by CMS for public reporting and payment programs.12-14 Briefly, the hospital RSRR is estimated using hierarchical generalized linear models (HGLM) using a logit link with the first level adjusted for age, sex, and 29 clinical covariates for AMI, 35 clinical covariates for heart failure, and 38 clinical covariates for pneumonia. Clinical covariates are identified using inpatient and outpatients claims during the 12 months prior to the index hospitalization. The second level of the model includes a random hospital-level intercept to account for the clustering of patients within the same hospital.12-14
Analytic Approach
In order to characterize the degree to which post-discharge observation stays are similar to inpatient readmission, we first describe the clinical conditions (by CCS category) most frequently evaluated in observation and short-stay readmission. We also calculated observation stay length of stay in 24-hour increments consistent with previous work studying prolonged observation stays.4,17 We report hospital-level observation rates and observation proportions for AMI, heart failure, and pneumonia.
We evaluated the relationship between hospital observation use and hospital readmission measure performance in several ways. First, we report Spearman correlation coefficients between both the hospital observation rate or observation proportion, and the hospital RSRR. Second, we report hospital-level variation in RSRR performance between strata of the observation rate and the observation proportion that were empirically defined after evaluating the distribution of both measures across the study cohorts. For the observation rate we grouped hospitals as having rates of: 0%, >0%-1%, >1%-2%, >2%-4%, and >4%. For the observation proportion, we grouped hospitals by rates of: 0%, >0%-10%, >10%-25%, and >25%. Third, we recalculated RSRR performance identically for each hospital but modified the outcome definition to count observation stays in addition to readmissions. We report this reclassification analysis as the number and proportion of hospitals that moved between pre-defined strata: top (>95th percentile), above average (75th-95th percentile), average (25th-75th percentile), below average (5th-25th percentile), and bottom (<5th percentile).
As a secondary analysis, we examined the relationship between hospital characteristics and the observation rate, observation proportion and RSRR including observation stays in the outcome. We used the American Hospital Association Annual Survey to identify hospital characteristic including: safety-net status, teaching status, and urban/rural status. Hospital safety-net status was defined consistent with prior work as a hospital Medicaid caseload greater than 1 standard deviation above the mean Medicaid caseload in their respective state.18 We calculate chi-square statistics to compare hospital characteristics groups.
All analyses were conducted using SAS 9.1 (SAS Institute, Cary, NC). Institutional Review Board approval was obtained through the Yale University Human Investigations Committee.
Results
Prevalence and Characteristics of Post-Discharge Observation Stays
During the study year, we included a total of 157,035 patients hospitalized at 1,656 hospitals for AMI; 391,209 at 3,044 hospitals for heart failure; and 342,376 at 3,484 hospitals for pneumonia in our analyses. After hospitalization for AMI, there were 3,506 observation stays (2.2%) and 27,214 readmissions (17.3%) within 30 days of discharge; 6,145 (1.6%) and 88,106 (22.5%), respectively, after hospitalization for heart failure; and 4,231 (1.2%) and 59,352 (17.3%), respectively, after hospitalization for pneumonia.
The ten most common reasons for post-discharge observation stays were largely similar to the discharge diagnoses for short-stay inpatient readmissions. Appendix Tables 1,2,3. The average length of stay for observation stays following index hospital admission for AMI was 32 hours (Interquartile range (IQR): 18 to 43), 36 hours for heart failure (IQR: 19 to 47), and 35 hours for pneumonia (IQR: 19 to 46). Of all post-discharge observation stays, 14.0% among AMI patients were longer than 48 hours, 17.7% among heart failure patients, and 16.0% for pneumonia, exceeding the CMS's recommended length of observation stays. Appendix Figure 1 and eTable 4.
Hospital use of Post-Discharge Observation Stays for Patients with AMI, Heart Failure and Pneumonia
At the hospital level, many hospitals had no observation stays in the post-discharge period, including 28% of hospitals that had discharged patients after AMI, 31% after heart failure, and 43% after pneumonia. Across all hospitals, there was high hospital-level variation for the observation rate and observation proportion. The median hospital's observation rate was 1.9% for AMI (5th/95th percentile: 0.0% to 5.7%), 1.3% for heart failure (5th/95th: 0.0% to 4.4%) and 0.9% for pneumonia (5th/95th: 0.0% to 3.7%, Appendix Figure 2). The median hospital's observation proportion was 10.2% for AMI (5th/95th: 0.0% to 28.6%), 5.4% for heart failure (5th/95th: 0.0% to 17.4%), and 5.3% for pneumonia (5th/95th: 0.0% to 20.0%, Appendix Figure 2).
Relationship Between Hospital Post-Discharge Observation Use and RSRR Performance
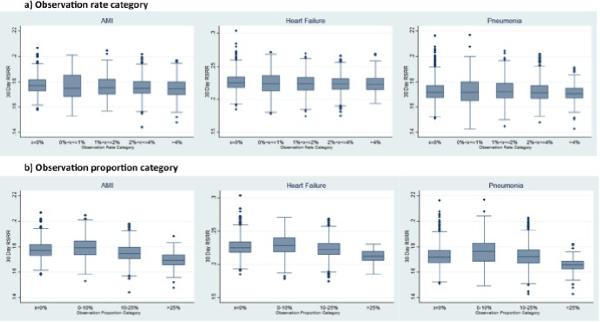
Across all three conditions, hospitals with high and low use of post-discharge observation stays had similar RSRRs. For AMI, the 471 hospitals with no use (observation rate=0%) of post-discharge observation stays had a median RSRR of 17.7% (5th/95th percentile: 16.6% to 19.1%) while the 301 hospitals with the highest use of post discharge observation stays (observation rate>4%) had a median RSRR of 17.6% (5th/95th: 16.3% to 18.8%). For heart failure and pneumonia, there was similarly little difference in RSRR performance between hospitals in the lowest and highest observation rate categories (Table 1, Figure 1). For all conditions, the median hospital in the highest observation proportion group (observation proportion >25%) had a lower RSRR than the median hospital with no use of observation for all three conditions (AMI: 17.0% vs. 17.7%; heart failure: 21.2% vs. 22.5%; pneumonia: 16.6% vs. 17.2%; Table 2, Figure 1). However, the range of RSRR performance was similar across all observation proportion categories. For each condition cohort, very few hospitals used observation stays in the highest proportion category: 174 (11%) of hospitals measured for AMI performance, 92 (3%) of hospitals for heart failure, and 162 (5%) of hospitals for pneumonia.
Table 1.
Hospital-level RSRR Performance based on observation rate following discharge for acute myocardial infarction (AMI), heart failure, and pneumonia
| Risk-Standardized Readmission Rate (RSRR) Performance | ||||||
|---|---|---|---|---|---|---|
| AMI | Heart Failure | Pneumonia | ||||
| Observation Rate Category | Hospitals (n) | Median RSRR (5th, 95th percentile) | Hospitals (n) | Median RSRR (5th, 95th percentile) | Hospitals (n) | Median RSRR (5th, 95th percentile) |
| 0% | 471 | 17.7% (16.6, 19.1) | 953 | 22.5% (20.6, 25.4) | 1,500 | 17.2% (16.1, 18.7) |
| 0%-1% | 78 | 17.5% (16.1, 19.6) | 367 | 22.4% (19.6, 25.4) | 370 | 17.2% (15.5, 19.1) |
| 1%-2% | 294 | 17.50% (16.1, 19.1) | 658 | 22.4% (19.9, 24.9) | 705 | 17.2% (15.8, 18.8) |
| 2%-4% | 512 | 17.5% (16.3, 18.8) | 756 | 22.3% (20.1, 24.9) | 696 | 17.1% (16.0, 18.6) |
| >4% | 301 | 17.5% (16.3, 18.8) | 310 | 22.3% (20.5, 24.5) | 213 | 17.1% (16.0, 18.2) |
| Total | 1,656 | 17.6% (16.3, 18.9) | 3,044 | 22.4% (20.1, 25.0) | 3,484 | 17.2% (15.9, 18.7) |
Figure 1. Hospital RSRR Performance based on observation rate use following discharge for AMI, heart failure and pneumonia.
Figure subtitle: AMI; Heart Failure; Pneumonia above each graph
y-axis: 30 day RSRR
x-axis top row of figures(a): Observation Rate Category
x-axis bottom row of figures(b): Observation Proportion Category
footnote: *all hospitals with volume of index admissions <25; RSRR: 30 day risk-standardized readmission rate
Table 2.
Hospital-level RSRR Performance based on Observation Proportion following discharge for AMI, heart failure and Pneumonia
| Risk-Standardized Readmission Rate (RSRR) Performance | ||||||
|---|---|---|---|---|---|---|
| AMI | Heart Failure | Pneumonia | ||||
| Observation Proportion Category | Hospitals (n) | Median (5th, 95th percentile) | Hospitals (n) | Median (5th, 95th percentile) | Hospitals (n) | Median (5th, 95th percentile) |
| 0% | 471 | 17.7% (16.6, 19.1) | 953 | 22.5% (20.6, 25.3) | 1,500 | 17.2% (16.1, 18.7) |
| 0%-10% | 383 | 17.9% (16.6, 19.3) | 504 | 22.8% (20.2, 25.4) | 329 | 17.6% (15.8, 19.3) |
| 10%-25% | 628 | 17.5% (16.2, 18.8) | 1,495 | 22.3% (20.1, 24.6) | 1,493 | 17.2% (15.8, 18.6) |
| >25% | 174 | 17.0% (15.9, 17.9) | 92 | 21.2% (19.8, 22.5) | 162 | 16.6% (15.6, 17.4) |
| Total | 1,656 | 17.6% (16.3, 18.9) | 3,044 | 22.4% (20.1, 25.0) | 3,484 | 17.2% (15.9, 18.7) |
We assessed correlations between hospital-level observation measures and RSRR performance. There was a statistically significant but weak correlation between the observation rate and hospital RSRRs (AMI: r=−0.1092, p<0.001; heart failure: −0.0886, p<0.001; pneumonia r=−0.0366, p=0.031). The correlation between hospital observation proportions and RSRRs were moderate (AMI: r=−0.3390, p<0.001; heart failure: r=−0.2621, p<0.001; pneumonia: r=−0.2114, p<0.001).
Inclusion of Observation Stays in the RSRR Measurement
We conducted several analyses to assess the impact of counting post-discharge observation stays as outcomes in the readmission measures. First, the correlation between hospital RSRR performance and hospital RSRR performance counting observation stays as an outcome was consistently high across all three conditions (AMI: r=0.89; heart failure: r=0.94; pneumonia: r=0.95). Table 3. Except for hospitals with an observation rate >4%, the Spearman correlation was >0.98 across all other observation rate categories for all three conditions indicating that inclusion of observation stays in the RSRR outcome may only impact a select number of hospitals. Second, we created a reclassification table to evaluate this change in RSRR outcome assessment. Appendix Table 3 a,b,c. For AMI, 3 out of 81(3.7%) hospitals in the top 5th percentile of RSRR performance moved to average performance (25th to 75th percentile), while 54 hospitals still remained in the top 5th percentile and 24 remained in the top quartile. Similarly for heart failure, inclusion of observation stays in the outcome would only move 2 of 155 (1.3%) hospitals from the top 5th percentile of performance to average performance and 2 of 134 (1.5%) hospitals for pneumonia. Notably, differences (or the lack of) in RSRR performance based on hospital ownership or safety-net status were not changed by the inclusion of hospital observation stays in the RSRR outcome.
Table 3.
Correlation of Hospital RSRR performance with Hospital RSRR performance including observation stays*
| Observation Rate Category | AMI | Heart Failure | Pneumonia |
|---|---|---|---|
| 0% | 0.9755 | 0.9876 | 0.9914 |
| 0%-1% | 0.9859 | 0.9939 | 0.9959 |
| 1%-2% | 0.9909 | 0.9958 | 0.9963 |
| 2-4% | 0.983 | 0.9836 | 0.9808 |
| >4% | 0.9376 | 0.9358 | 0.9283 |
| Overall | 0.8925 | 0.9394 | 0.9502 |
Spearman Correlation Coefficient
Hospital Characteristics Associated with Post-Discharge Observation Stay Use
In our secondary analysis of hospital characteristics, we found several that were associated with observation stay use (Table 4). Non-teaching and rural hospitals had statistically higher observation rates for AMI and heart failure and statistically higher observation proportions for all three conditions. Safety-net hospitals’ observation rate and observation proportion did not differ from non-safety-net hospitals for AMI or heart failure. Rural hospitals had consistently higher observation rates and observation proportions than urban hospitals for AMI (observation rate: 3.1% vs. 2.2%, p<0.001; observation proportion: 15.9% vs. 11.5%, p<0.001), heart failure (2.1% vs. 1.6%, p<0.001; 8.9% vs. 6.6%, p<0.001) and pneumonia (1.5% vs. 1.2%, p<0.001; 8.9% vs. 6.5%, p<0.001).
Table 4.
Hospital characteristics associated with post-discharge observation rate and observation proportion for acute myocardial infarction (AMI), heart failure, and pneumonia
| AMI | Heart Failure | Pneumonia | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hospital Type |
Hospitals | Observation Rate |
Observation Proportion |
RSRR | RSRR-O | Hospitals | Observation Rate |
Observation Proportion |
RSRR | RSRR-O | Hospitals | Observation Rate |
Observation Proportion |
RSRR | RSRR-O |
| (N) | Mean (SD) | Mean (SD) | Mean (SD) |
Mean (SD) |
(N) | Mean (SD) | Mean (SD) | Mean (SD) |
Mean (SD) |
(N) | Mean (SD) | Mean (SD) | Mean (SD) |
Mean (SD) |
|
| Non-profit | 1,155 | 0.024 (0.02) | 0.12 (0.11) | 0.18 (0.01) | 0.20 (0.01) | 1,897 | 0.018 (0.02) | 0.074 (0.08) | 0.22 (0.02) | 0.24 (0.02) | 2,142 | 0.013 (0.02) | 0.073 (0.09) | 0.17 (0.01) | 0.19 (0.01) |
| Private | 241 | 0.025 (0.03) | 0.12 (0.12) | 0.18 (0.01) | 0.20 (0.01) | 496 | 0.017 (0.02) | 0.070 (0.07) | 0.23 (0.01) | 0.24 (0.01) | 506 | 0.013 (0.02) | 0.066 (0.90) | 0.17 (0.01) | 0.19 (0.01) |
| Public | 168 | 0.024 (0.02) | 0.13 (0.13) | 0.18 (0.01) | 0.20 (0.01) | 446 | 0.020 (0.02) | 0.082 (0.09) | 0.22 (0.1) | 0.24 (0.15) | 618 | 0.015 (0.02) | 0.090 (0.13) | 0.17 (0.01) | 0.18 (0.01) |
| p-value | 0.82 | 0.62 | 0.0025 | 0.009 | 0.037 | 0.064 | <0.0001 | 0.0002 | 0.017 | 0.0002 | 0.052 | 0.42 | |||
| Non-teaching | 973 | 0.025 (0.03) | 0.13 (0.13) | 0.18 (0.01) | 0.20 (0.01) | 2,139 | 0.019 (0.02) | 0.077 (0.09) | 0.22 (0.01) | 0.24 (0.01) | 2,585 | 0.014 (0.02) | 0.078 (0.11) | 0.17 (0.01) | 0.18 (0.01) |
| Teaching | 591 | 0.022 (0.02) | 0.11 (0.10) | 0.18 (0.01) | 0.20 (0.01) | 700 | 0.016 (0.02) | 0.067 (0.07) | 0.22 (0.02) | 0.24 (0.02) | 681 | 0.013 (0.02) | 0.064 (0.07) | 0.17 (0.01) | 0.19 (0.01) |
| p-value | 0.0046 | 0.0026 | 0.26 | 0.61 | 0.0012 | 0.005 | 0.10 | 0.0032 | 0.12 | 0.0012 | 0.026 | 0.12 | |||
| Non-safety net | 1,254 | 0.024 (0.02) | 0.12 (0.11) | 0.18 (0.01) | 0.20 (0.01) | 2,138 | 0.018 (0.02) | 0.074 (0.08) | 0.22 (0.02) | 0.24 (0.02) | 2,369 | 0.013 (0.02) | 0.072 (0.09) | 0.17 (0.01) | 0.18 (0.01) |
| Safety net | 310 | 0.024 (0.02) | 0.12 (0.12) | 0.18 (0.01) | 0.20 (0.01) | 701 | 0.019 (0.02) | 0.075 (0.09) | 0.23 (0.01) | 0.24 (0.02) | 897 | 0.015 (0.02) | 0.083 (0.12) | 0.17 (0.01) | 0.18 (0.01) |
| p-value | 0.87 | 0.64 | 0.025 | 0.048 | 0.19 | 0.65 | 0.061 | 0.023 | 0.0078 | 0.0046 | 0.26 | 0.89 | |||
| Rural | 220 | 0.031 (0.03) | 0.16 (0.15) | 0.18 (0.01) | 0.20 (0.01) | 989 | 0.022 (0.02) | 0.089 (0.10) | 0.22 (0.01) | 0.24 (0.01) | 1,402 | 0.015 (0.02) | 0.089 (0.13) | 0.17 (0.01) | 0.18 (0.01) |
| Urban | 1,344 | 0.023 (0.02) | 0.12 (0.11) | 0.18 (0.01) | 0.20 (0.01) | 1,850 | 0.016 (0.02) | 0.066 (0.07) | 0.22 (0.02) | 0.24 (0.02) | 1,864 | 0.012 (0.01) | 0.065 (0.07) | 0.17 (0.01) | 0.18 (0.01) |
| p-value | <0.0001 | <0.0001 | 0.36 | 0.17 | <0.0001 | <0.0001 | 0.15 | 0.0003 | <0.0001 | <0.0001 | 0.013 | 0.30 | |||
RSRR: Risk-Standardized Readmission Rate
RSRR-O: Risk-standardized Readmission Rate including observation stays as an outcome
Discussion
In this national analysis of hospital use of post-discharge observation stays, we found little evidence to support the concern that hospital use of observation stays was substantially impacting the assessment of hospital performance on national quality measures. Nearly 40% of hospitals in the US did not have any Medicare fee-for-service beneficiaries return to the hospital for an observation stay without inpatient readmission within 30 days of hospital discharge after AMI, heart failure, or pneumonia. In addition, hospital use of observation services in the post-discharge period for Medicare beneficiaries occurs at a frequency that is one-ninth that of inpatient hospital readmissions, suggesting that most patients requiring hospitalization within 30 days of discharge from these three conditions largely require more intensive services, particularly in the older Medicare population, than afforded by traditional observation stays.
Our findings demonstrate that over half of patients admitted to observation following hospital discharge spend over 24 hours in the hospital and are observed for conditions very similar to inpatient readmissions, suggesting that a portion of patients may be returning to the hospital for observation stays for reasons similar to readmissions. We also found wide variation in the use of post-discharge observation stays between hospitals, which both supports a recent study demonstrating that observation use varies by geographic region,1 and demonstrates the importance of describing the relationship between observation service use and readmission performance benchmarks.
Although hospital-level observation rates were quite low, a small percentage of hospitals demonstrated a higher observation proportion and lower RSRRs as evidenced by moderate correlations. This may either suggest some marginal substitution between observation stays and inpatient readmissions that could subtly distort readmission measures or the incremental use of observation stays for other purposes. These select hospitals with the highest observation proportion (less than 175 hospitals per condition) may use observation stays as an alternative to prolonged emergency department visits or as a “release valve” for emergency department overcrowding, neither of which may reflect the same care transition outcome as an inpatient readmission.3 Furthermore, because fairly small increases or decreases in the number of readmissions can impact individual hospital RSRR performance, we tested the hypothetical impact of including observation stays in the RSRR outcome and found little change in performance classification. As such, it appears that differences found between hospitals’ readmission rates are less likely to reflect “gaming” of the performance measure through observation stay use.
Should the hospital-level trend in the use of observation stays continue to rise, the importance of capturing observation stays as potential signals of poor transitions may warrant the development of a potential composite measure of both observation stays and inpatient readmissions. Any policy change now may be premature, however, without a better understanding of the types and purpose of observation care. Our analyses are limited by current administrative claims data, which cannot distinguish between efficient observation care that is delivered in a dedicated unit using coordinated clinical pathways from observation stays that may closely mimic inpatient readmissions.17,19 Future research should better characterize the relationship between the type of observation care and readmission rates in order to assess the efficiency and quality of care transitions.
We also found that Medicare beneficiaries were generally more likely to be admitted to post-discharge observation stays based on certain hospital characteristics suggesting that observation stay use may be a function of several market characteristics. While most hospital characteristics conferred either no or minimal statistical differences, rural hospitals demonstrated consistently higher observation stay use. In addition to confirming previous work,20 our work also suggests that inclusion of observation stays in the RSRR outcome would generate significantly higher readmission rates for rural hospitals in the case of heart failure patients, but the opposite in the case of pneumonia patients. This difference suggests that post-discharge observation use, like hospital admission and readmission rates,19 may be either a condition-specific phenomenon or that rural hospitals use observation services as an alternative to outpatient follow-up care in a clinic due to local workforce and access limitations.
Several limitations of our work must be considered. First, the observation care policy environment is dynamic, and the recently proposed “two midnight rule,” which distinguishes between observation and inpatient hospitalizations based on hospital length of stay, could impact the assignment of outcomes for this work. However, our conclusions are likely conservative as inclusion of the 50-60% of post-discharge observation stays that are currently longer than 24 hours, and therefore potentially hospitalized for 2 midnights, in the readmission outcome did not alter RSRR performance. Our analyses only evaluated the post-discharge use of observation stays and cannot account for index use of hospital observation stays. We believe index use of observation services to minimally impact our results for two reasons: first, few patients admitted to the hospital for AMI, heart failure, or pneumonia would meet observation status admission guidelines, and second, current financial incentives would favor index inpatient admission for favorable reimbursement.
Conclusion
Hospital use of observation stays in the post-discharge period for AMI, heart failure, and pneumonia is quite low in comparison to inpatient readmissions. There is wide variation among hospitals in the use of post-discharge observation stays and only a modest relationship between hospital observation stay use and readmission rates. Current hospital use of observation stays does not impact performance measurement of hospital readmission rates; however, continued surveillance is necessary to ensure that select hospitals with disproportionately higher use of observation stays are accurately classified for public reporting and payment programs.
Supplementary Material
Acknowledgments
All authors of this work received support from the Centers for Medicare and Medicaid Service, an agency of the U.S. Department of Health and Human Services, under Contract Number HHSM-500-2013-13018I-T0001 to conduct this work. AKV also reports the support of the Emergency Medicine Foundation Health Policy Scholar Award for the study of observation services and a one-time consulting fee from QuantiaMD for the development of observation care related Continuing Medical Education. JSR also report support from the National Institute of Aging (K08 AG032886) and by the American Federation of Aging Research through the Paul B. Beeson Career Development Award Program. JSR is also supported from the FDA, the Pew Charitable Trust, Johnson & Johsnon, and Medtronic Inc. and serves as a member of the Scientific Advisory Board of FAIR Health Inc. for work not related to this manuscript. LGS is also supported in part by the VA Connecticut Healthcare System.
Footnotes
Conflicts of Interest: No other authors (CW, FKS, SV, JG, SB) report any other potential conflicts of interest in the previous three years.
References
- 1.Gerhardt G, Yemane A, Apostle K, Oelschlaeger A, Rollins E, Brennan N. Evaluating Whether Changes in Utilization of Hospital Outpatient Services Contributed to Lower Medicare Readmission Rate. Medicare & medicaid research review. 2014;4(1) doi: 10.5600/mmrr2014-004-01-b03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Venkatesh AK, Geisler BP, Chambers JJG, Baugh CW, Bohan JS, Schuur JD. Use of observation care in US emergency departments, 2001 to 2008. PLoS One. 2011;6(9):e24326. doi: 10.1371/journal.pone.0024326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ross MA, Hockenberry JM, Mutter R, Barrett M, Wheatley M, Pitts SR. Protocol-driven emergency department observation units offer savings, shorter stays, and reduced admissions. Health Affairs. 2013;32(12):2149–2156. doi: 10.1377/hlthaff.2013.0662. [DOI] [PubMed] [Google Scholar]
- 4.Hockenberry JM, Mutter R, Barrett M, Parlato J, Ross MA. Factors associated with prolonged observation services stays and the impact of long stays on patient cost. Health services research. 2014;49(3):893–909. doi: 10.1111/1475-6773.12143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schuur JD, Venkatesh AK, Bohan JS. Variation in the use of observation status evaluation in Massachusetts acute care hospitals, 2003–2006. International journal of emergency medicine. 2010;3(4):367–372. doi: 10.1007/s12245-010-0188-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baugh CW, Schuur JD. Observation care—high-value care or a cost-shifting loophole? New England Journal of Medicine. 2013;369(4):302–305. doi: 10.1056/NEJMp1304493. [DOI] [PubMed] [Google Scholar]
- 7.Baugh CW, Venkatesh AK, Bohan JS. Emergency department observation units: a clinical and financial benefit for hospitals. Health care management review. 2011;36(1):28–37. doi: 10.1097/HMR.0b013e3181f3c035. [DOI] [PubMed] [Google Scholar]
- 8.Daughtridge GW, Archibald T, Conway PH. Quality improvement of care transitions and the trend of composite hospital care. JAMA. 2014;311(10):1013–1014. doi: 10.1001/jama.2014.509. [DOI] [PubMed] [Google Scholar]
- 9.Sheehy AM, Graf BK, Gangireddy S, Formisano R, Jacobs EA. “Observation status” for hospitalized patients: implications of a proposed Medicare rules change. JAMA internal medicine. 2013 Nov 25;173(21):2004–2006. doi: 10.1001/jamainternmed.2013.9382. [DOI] [PubMed] [Google Scholar]
- 10.Baier RR, Gardner RL, Coleman EA, Jencks SF, Mor V, Gravenstein S. Shifting the dialogue from hospital readmissions to unplanned care. The American journal of managed care. 2013 Jun;19(6):450–453. [PubMed] [Google Scholar]
- 11.Centers for Medicare Medicaid Services [October 3, 2014];Medicare Hospital Quality Chartbook 2013: Performance Report on Outcome Measures. 2013 http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Downloads/-Medicare-Hospital-Quality-Chartbook-2013.pdf.
- 12.Keenan PS, Normand S-LT, Lin Z, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circulation: Cardiovascular Quality and Outcomes. 2008;1(1):29–37. doi: 10.1161/CIRCOUTCOMES.108.802686. [DOI] [PubMed] [Google Scholar]
- 13.Krumholz HM, Lin Z, Drye EE, et al. An administrative claims measure suitable for profiling hospital performance based on 30-day all-cause readmission rates among patients with acute myocardial infarction. Circulation: Cardiovascular Quality and Outcomes. 2011;4(2):243–252. doi: 10.1161/CIRCOUTCOMES.110.957498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lindenauer PK, Normand SLT, Drye EE, et al. Development, validation, and results of a measure of 30-day readmission following hospitalization for pneumonia. Journal of Hospital Medicine. 2011;6(3):142–150. doi: 10.1002/jhm.890. [DOI] [PubMed] [Google Scholar]
- 15.Ash AS, Fienberg SF, Louis TA, Normand S-LT, Stukel TA, Utts J. Statistical issues in assessing hospital performance. 2012 [Google Scholar]
- 16.Elixhauser A, Pancholi M, Clancy CM. Using the AHRQ quality indicators to improve health care quality. Joint Commission journal on quality and patient safety/Joint Commission Resources. 2005;31(9):533–538. doi: 10.1016/s1553-7250(05)31069-5. [DOI] [PubMed] [Google Scholar]
- 17.Sheehy AM, Caponi B, Gangireddy S, et al. Observation and inpatient status: Clinical impact of the 2-midnight rule. Journal of Hospital Medicine. 2014;9(4):203–209. doi: 10.1002/jhm.2163. [DOI] [PubMed] [Google Scholar]
- 18.Ross JS, Bernheim SM, Lin Z, et al. Based on key measures, care quality for Medicare enrollees at safety-net and non-safety-net hospitals was almost equal. Health Affairs. 2012;31(8):1739–1748. doi: 10.1377/hlthaff.2011.1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Venkatesh AK, Suter LG. Observation “Services” and Observation “Care”—One Word Can Mean a World of Difference. Health services research. 2014;49(4):1083–1087. doi: 10.1111/1475-6773.12210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wright B, Jung HY, Feng Z, Mor V. Hospital, Patient, and Local Health System Characteristics Associated with the Prevalence and Duration of Observation Care. Health services research. 2014 doi: 10.1111/1475-6773.12166. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.