Abstract
Medial meniscal root tears have been repaired using various methods. Arthroscopic all-inside repair using a suture anchor is one of the popular methods. However, insertion of the suture anchor into the proper position at the posterior root of the medial meniscus is technically difficult. Some methods have been reported to facilitate suture anchor insertion through a high posteromedial portal, a posterior trans-septal portal, or a medial quadriceptal portal. Nevertheless, many surgeons still have difficulty during anchor insertion. We introduce a technical tip for easy suture anchor insertion using a 25° curved guide and a soft suture anchor through a routine posteromedial portal.
Keywords: Medial meniscus, Root tear, Curved guide, Soft suture anchor
The circumferential hoop tension and load transmissibility of the menisci are impaired by a posterior root tear of the medial meniscus; consequently, the meniscus tends to be displaced anteriorly and posteriorly, altering the biomechanics and possibly the kinematics of the knee. This causes degenerative changes of the articular cartilage. Repair of the meniscal root is thus critical to restore normal to near-normal contact pressure and decrease progression to clinical osteoarthritis.1)
To repair the posterior root of the medial meniscus directly, the arthroscopic all-inside repair technique using a suture anchor was introduced.2,3,4) However, the suture anchor repair technique is technically difficult and carries a risk of damage to the soft tissue around the joint capsule during approach to the footprint of the posterior root of the medial meniscus through a high posteromedial (PM) portal, a posterior trans-septal portal, or a medial quadriceptal portal in deep flexion of the knee joint.
We introduce a technical tip to repair posterior root tears of the medial meniscus. Our technique enables easy fixation of the suture anchor at the appropriate position in a more vertical direction using a soft suture anchor with a 25° curved guide through a routine PM portal. All images were approved from the patient to be submitted for publication.
TECHNIQUE
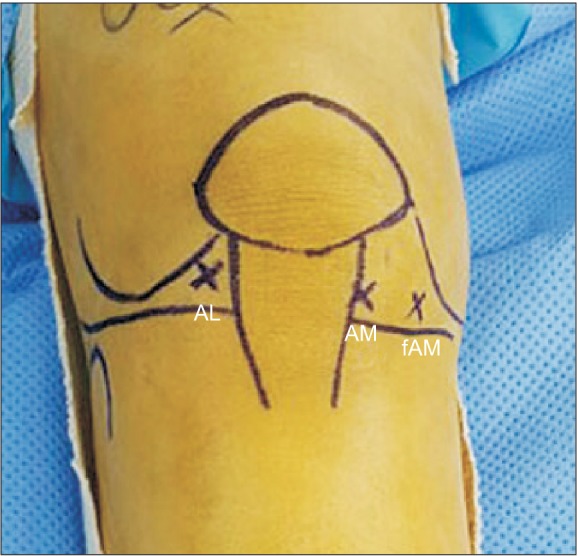
A complete tear of the posterior root of the medial meniscus with medial translation was confirmed by preoperative magnetic resonance imaging. An anterolateral (AL) portal was created as a viewing portal, and the torn posterior root of the medial meniscus was identified. An anteromedial (AM) portal was created as a working portal just medial to the patellar tendon and above the anterior horn of the medial meniscus. An additional far AM portal was created to prevent suture limb entanglement and soft tissue catching during shuttle relay (Fig. 1).
Fig. 1. Preoperative planning of portal positions in the right knee. Anterolateral (AL) portal as viewing portal, anteromedial (AM) portal as a main working portal located just medial to the patella tendon, and far anteromedial (fAM) portal used for shuttle relay.
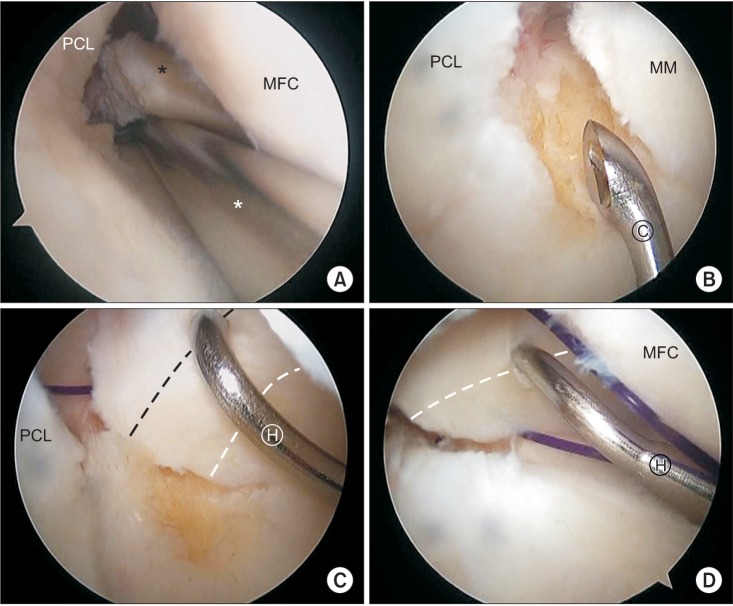
Under visualization through the AL portal with a 30° arthroscope, the torn edge of the posterior root of the medial meniscus was debrided using a motorised shaver through the AM portal. Cartilage at the insertion area of the posterior root of the medial meniscus was removed using a curved curette to improve the healing environment. A suture hook (Linvatec, Largo, FL, USA) loaded with a no. 0 polydioxanone suture (PDS; Ethicon, Somerville, NJ, USA) was inserted through the AM portal, and the tip of the hook penetrated the posterior one-third of the meniscus from superior to inferior in a vertical direction, 7–8 mm medial to the torn edge. The loaded PDS was advanced, and then two limbs of the PDS were retrieved through the far AM portal using a suture retriever (Arthrex, Naples, FL, USA). This process was repeated to suture the anterior one-third of the meniscus (Fig. 2).
Fig. 2. (A) The tear margin of the posterior root of medial meniscus (MM; black asterisk) is debrided using a motorized shaver (white asterisk). (B) Preparation of the insertion site using a curved curette (Ⓒ). (C) Posterior one-third of the meniscus (black dotted line), 7–8 mm medial to the torn edge, is penetrated using a curved suture hook (Ⓗ). (D) The anterior one-third of the meniscus (white dotted line) is penetrated in the same manner. PCL: posterior cruciate ligament, MFC: medial femoral condyle.
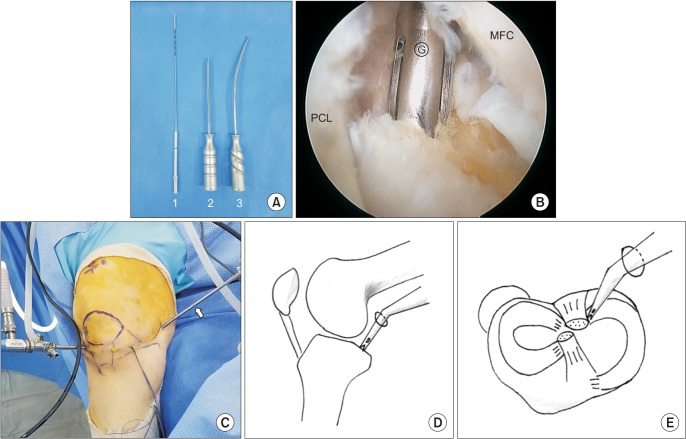
Transillumination of the saphenous nerve and vein was performed with an arthroscope placed between the posterior cruciate ligament and the medial femoral condyle through the AL portal. Then, a routine PM portal was created 1–1.5 cm proximal to the joint line and 1 cm posterior to the medial femoral condyle to avoid neurovascular injury (Fig. 3). The tip of a 25° curved guide was placed at the prepared insertion site of the footprint of the posterior root of the medial meniscus through the PM portal, and a pilot hole was created at an appropriate angle using a flexible drill with the knee flexed at less than 90°. A 2.3-mm ICONIX soft suture anchor (Stryker Endoscopy, San Jose, CA, USA) double loaded with no. 2 Force Fiber (Teleflex Medical OEM, Gurnee, IL, USA) was inserted along the 25° curved guide (Fig. 4).
Fig. 3. A posterior medial portal (asterisk) is established by the transillumination technique at the center of soft spot, 1–1.5 cm proximal to the joint line and 1 cm posterior to the medial femoral condyle.
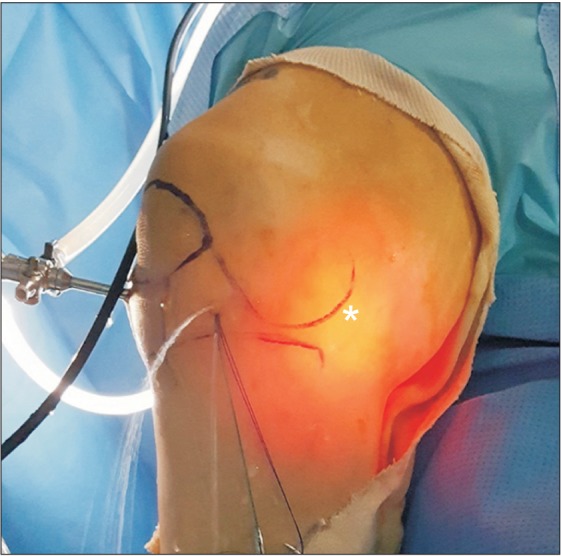
Fig. 4. (A) Comparison of a flexible reamer (1) and a 25° curved suture anchor guide (3) with a straight guide (2). (B) The tip of a 25° curved guide (Ⓖ) is placed on the footprint of the posterior root of the medial meniscus vertically. (C) Under visualization through an anterolateral portal, a soft suture anchor along the curved guide (arrow) is inserted through a posteromedial portal at an angle of 30° with the knee flexed at 60°. (D, E) Schematic diagram showing the knee position and insertion of the curved guide through the posteromedial portal. PCL: posterior cruciate ligament, MFC: medial femoral condyle.
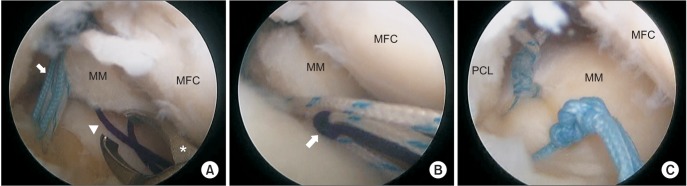
A plastic cannula was then placed through the AM portal to prevent the fibers from entangling the soft tissue during shuttle relay and sliding knot creation. A suture retriever was inserted through the AM portal, and one strand of the Force Fiber and one limb of the PDS from the inferior side were retrieved. The strand of PDS was twisted to make a shuttle relay, and the strand of the Force Fiber was hooked to the shuttle relay. The other limb of the PDS placed at the far AM portal was pulled to pass the Force Fiber from inferior to superior. Another Force Fiber was passed through the substance of the meniscus by the same process. The two limbs of the Force Fiber were retrieved through the AM portal, a SMC knot was made and slid with a knot pusher under adequate reduction and tension, and four additional reversed half-hitches on alternating posts were made. Another knot was made via the same process (Fig. 5).
Fig. 5. (A) One limb of the polydioxanone suture (PDS, arrowhead) from the inferior side and one strand of Force Fiber (arrow) are retrieved using a suture retriever (asterisk) along a cannula through an anteromedial portal. (B) Shuttle relay by pulling a PDS (arrow) at far anteromedial portal is made to pass the Force Fiber through the meniscus from inferior to superior. (C) Two sutures are tied securely, and the posterior root of the medial meniscus (MM) is repaired to the insertion site. MFC: medial femoral condyle, PCL: posterior cruciate ligament.
DISCUSSION
Some authors have treated posterior root tears of the medial meniscus via partial meniscectomy. However, it has been recognized that partial meniscectomy does not restore the normal biomechanical function of the meniscus. A torn medial meniscal root should be repaired to recover meniscal hoop tension even if the posterior horn attachment of the meniscus is covered with vascular synovial tissue and appears to have a good blood supply.5) Furthermore, a biomechanical study showed that repair of the torn medial meniscus restores normal to near-normal contact pressures.1) Therefore, numerous techniques to repair meniscal root tears have been reported. Recently, arthroscopic repair has been advocated, which can be divided into suture anchor repair and transtibial pull-out repair.
Ahn et al.6) introduced a pull-out suture repair technique using a trans-septal portal, which resulted in four cases of complete healing and eight cases of partial healing in 13 patients in a study by Cho and Song.7) However, the sutures in this technique are placed far from the native meniscal attachment. This causes potential abrasion of the suture material within the bony tunnel during range of motion of the knee and resultant loosening of the suture materials during rehabilitation.2) Additionally, the creation of a transtibial tunnel can be crowded or collide with other bone tunnels created during combined ligament surgery or high tibial osteotomy, and there is a possibility of cartilage damage on the medial femoral condyle to secure space for insertion of the anterior cruciate ligament guide.3) To reduce abovementioned risks, alternative arthroscopic all-inside repair techniques using a suture anchor through a high PM portal, a posterior trans-septal portal, or a quadriceps portal were introduced.2,3,4) However, the insertion of the posterior horn of the medial meniscus is attached to the anterior half of the posterior intercondylar fossa of the tibial plateau, directly anterior to the posterior cruciate ligament tibial insertion. Therefore, these techniques require the knee joint to be maintained in deep flexion intraoperatively to enable approach of the suture anchor to the appropriate position of the posterior horn of the medial meniscus. Deep flexion of the knee joint results in decreased joint space and suboptimal arthroscopic view, which makes it difficult to approach the appropriate position, especially in obese patients. Hence, there is a steep learning curve for the surgeon to be able to place the suture anchor at the appropriate insertion point in such an acute angle.2)
In an attempt to seek a method for easy insertion of the suture anchor, we tried out using a soft suture anchor with a curved guide, which was originally designed for more vertical insertion of a suture anchor in shoulder and hip surgery. Pullout force of the soft suture anchor used in our technique is rigid enough for a posterior root tear of the medial meniscus; the mean pullout force of the ICONIX 2 (Stryker Endoscopy) is 468 ± 45 N, which is at least four times stronger than the highest mean pullout failure strength of the posterior horn of the medial meniscus.8,9)
The soft suture anchor rod is flexible and can be passed through a curved guide. It is also possible to turn the direction of the tip of the curved guide to reach a wide range compared with a straight guide. So, it is easy to insert the anchor more vertically, and there is no need to flex the knee deeply to approach the footprint of the posterior root of the medial meniscus. Also, an optimal visual field can be secured during the procedure. Based upon our experience, the technique could be easy to perform in obese patients.
Our technique also enables insertion of the soft suture anchor though a routine PM portal, which could reduce the risk of soft tissue injury compared with a high PM portal, a posterior trans-septal portal, or a quadriceps portal. McGinnis et al.10) described in their cadaveric study that the use of a high PM portal always resulted in piercing of the gastrocnemius musculotendinous structure. The safety zone of a PM portal is located at the center of soft spot that is 1–2.5 cm proximal to the joint line, posterior to the medial femoral condyle, anterior to the gastrocnemius fold, and inferior to the adductor tendon.
There are some limitations of our technique. First, there is a risk of cartilage damage during insertion of the suture hook in the knee with medial tightness. AM portal positioning at a site just medial to the patellar tendon for securing sufficient working space at the intercondylar fossa and careful instrumentation during arthroscopic procedure are required. In some cases, the pie-crust technique for percutaneous medial collateral ligament lengthening could be used to avoid iatrogenic cartilage damage when the medial compartment is too narrow and tight. It is a safe and reliable technique and does not affect clinical and functional outcomes. Second, a degenerative meniscus can be injured during passing of the suture hook or suture strands, which can result in insecure fixation of the suture and a cutout. So, care should be taken to maintain proper tension during knot tying (Table 1).
Table 1. Advantages and Limitations.
| Advantage |
|---|
| · Vertical insertion allowing appropriate placement of an anchor using a curved guide |
| · Optimal visual field obtainment with the knee flexed to less than 90° |
| · Less risk of soft tissue damage with a curved guide through the routine posteromedial portal |
| · Applicable in patients with obesity |
| Limitation |
| · Cartilage damage during insertion of the suture hook in the knee with medial tightness |
| · Degenerative meniscus may not hold the suture securely, and a cutout may occur. |
In spite of some limitations, our technique using a soft suture anchor is easy to perform and could be an alternative rigid repair technique to previous techniques using a traditional suture anchor.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.LaPrade CM, Foad A, Smith SD, et al. Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am J Sports Med. 2015;43(4):912–920. doi: 10.1177/0363546514566191. [DOI] [PubMed] [Google Scholar]
- 2.Choi NH, Son KM, Victoroff BN. Arthroscopic all-inside repair for a tear of posterior root of the medial meniscus: a technical note. Knee Surg Sports Traumatol Arthrosc. 2008;16(9):891–893. doi: 10.1007/s00167-008-0581-3. [DOI] [PubMed] [Google Scholar]
- 3.Kim JH, Chung JH, Lee DH, Lee YS, Kim JR, Ryu KJ. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: a prospective comparison study. Arthroscopy. 2011;27(12):1644–1653. doi: 10.1016/j.arthro.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 4.Jung WH, Kim DH, Chun CW, Lee JH, Ha JH, Jeong JH. Arthroscopic, suture anchor repair through a novel medial quadriceptal portal for medial meniscal root tear. Knee Surg Sports Traumatol Arthrosc. 2012;20(12):2391–2394. doi: 10.1007/s00167-012-1895-8. [DOI] [PubMed] [Google Scholar]
- 5.Arnoczky SP, Warren RF. Microvasculature of the human meniscus. Am J Sports Med. 1982;10(2):90–95. doi: 10.1177/036354658201000205. [DOI] [PubMed] [Google Scholar]
- 6.Ahn JH, Wang JH, Yoo JC, Noh HK, Park JH. A pull out suture for transection of the posterior horn of the medial meniscus: using a posterior trans-septal portal. Knee Surg Sports Traumatol Arthrosc. 2007;15(12):1510–1513. doi: 10.1007/s00167-007-0310-3. [DOI] [PubMed] [Google Scholar]
- 7.Cho JH, Song JG. Second-look arthroscopic assessment and clinical results of modified pull-out suture for posterior root tear of the medial meniscus. Knee Surg Relat Res. 2014;26(2):106–113. doi: 10.5792/ksrr.2014.26.2.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barber FA, Herbert MA. Cyclic loading biomechanical analysis of the pullout strengths of rotator cuff and glenoid anchors: 2013 update. Arthroscopy. 2013;29(5):832–844. doi: 10.1016/j.arthro.2013.01.028. [DOI] [PubMed] [Google Scholar]
- 9.Kim YM, Joo YB. Pullout failure strength of the posterior horn of the medial meniscus with root ligament tear. Knee Surg Sports Traumatol Arthrosc. 2013;21(7):1546–1552. doi: 10.1007/s00167-012-2131-2. [DOI] [PubMed] [Google Scholar]
- 10.McGinnis MD, 4th, Gonzalez R, Nyland J, Caborn DN. The posteromedial knee arthroscopy portal: a cadaveric study defining a safety zone for portal placement. Arthroscopy. 2011;27(8):1090–1095. doi: 10.1016/j.arthro.2011.02.031. [DOI] [PubMed] [Google Scholar]