Abstract
Objective
Clinical symptoms of diabetic nephropathy patients and non-diabetic nephropathy are compared and analyzed, hemodialysis effect and quality of life of two kinds of nephrotic patients are analyzed.
Methods
Respectively extract 1300 cases of diabetic nephropathy and non-diabetic nephropathy patients admitted to different hospitals during December 2011-December 2014. Based on whether the patient suffers from diabetes, they were divided into diabetic group and control group. Hemodialysis of two groups of patients were followed up to observe effectiveness of blood treatment, and complications were observed after one year of follow-up.
Results
Hematodialysis effectiveness of diabetic nephropathy patients is significantly lower than that of non-diabetic nephropathy group. After 1 year’s follow-up, it can be found that survival rate of diabetic nephropathy patients is much lower than that of control group. In statistical comparison of data involved in the two groups of patients, P < 0.05, the difference is statistically significant.
Conclusion
Treatment effect of diabetic nephropathy patients is relatively poor compared to that of non-diabetic patients. In clinics, management and prevention of diabetic patients should be strengthened to avoid complication of nephropathy which brings serious injury to patients.
Keywords: Diabetic nephropathy, Non-diabetic nephropathy, Hemodialysis, Survival rate, Comparison
1. Introduction
Diabetic nephropathy is a frequent complication of diabetes, which grows with rise in incidence of diabetes, causing a serious impact on physical health and life safety of patients. Diabetic nephropathy can also cause a serious increase in the number of end-stage nephritic patients, which seriously endangers patient’ life safety. Hemodialysis is an effective means to treat end-stage nephropathy, and hemodialysis quality will directly affect physical health of patients. Because of their original diabetes, diabetic nephropathy patients will suffer from decline in resistance. In this case, hemodialysis treatment effect will be greatly reduced. Moreover, because of multiple complications of diabetes, patients’ quality of life are greatly impacted. Therefore, emphasis on diabetes should be strengthened in clinics to avoid disease deterioration of diabetic patients and development into diabetic nephropathy. The author selected data of 2600 cases of nephrotic patients admitted in different hospitals during December 2011-December 2014, to be divided into diabetic group and control group based on whether patients have diabetes, each group with 1300 cases. Therapeutic effects and complications were studied, with research results reported. Fig. 1 shows B-ultrasound diagnosis picture of a nephritic patient. (see Table 1, Table 2).
Fig. 1.

The B-ultrasound diagnosis picture of a patient (male, 34 years old, polycystic kidney disease).
Table 1.
Comparison of survival rate of the two groups of patients (n,%).
| Group | Total case | Survive (person) | Die (person) |
|---|---|---|---|
| Diabetic group | 1300 | 726 (55.8) | 574 (44.2) |
| Control group | 1300 | 1018 (78.3) | 282 (21.7) |
| P value | <0.05 | ||
Table 2.
Comparison of incidence of complication during treatment of the two groups of patients (n,%).
| Group | Total case | Occurred | Un-occurred |
|---|---|---|---|
| Diabetic group | 1300 | 1124 (86.5) | 176 (13.5) |
| Control group | 1300 | 762 (58.6) | 538 (41.4) |
| P value | <0.05 | ||
2. Method
2.1. General information
Among the 2600 patients selected in this study, 1300 patients are with diabetic nephropathy, while the other 1300 cases are non-diabetic nephropathy patients. Diabetic group: Male: 580 cases, female 720 cases, age: between 32 and 79 years, mean age (50.7 ± 5.2) years. Control group: Male: 601 cases; female: 699 cases, age: between 35 and 78 years, mean age (51.1 ± 4.9) years. There is no statistical difference between general information of the two groups of patients, and it is worth comparing the two groups of patients. All patients were treated with maintenance hemodialysis and did not suffer from contagious, hereditary diseases and evil nature disease of other forms. Before treatment, all patients themselves and their families expressed their willingness to cooperate with follow-up investigation. After the end of treatment, a period of 1 year of follow-up was done. Fig. 2 shows hematodialysis treatment picture of a nephrotic patient.
Fig. 2.

Hematodialysis treatment picture of a nephrotic patient.
2.2. Treatment methods
The two groups of patients were treated with basic medical treatment methods (Liang Yindi, 2013). During treatment, medical staff should make necessary control of the patient’s diet, and simultaneously adjust the patient’s diet structure to avoid excessive fat intake (Meicai et al., 2013). During hemodialysis treatment, medical staff should help patients to establish necessary venous vascular access, take positive and effective measures during treatment cycle to strengthen patients’ calcium foliate supplement, and take heparin as an anticoagulant agent for treatment of patients without bleeding (Peng Bin et al., 2014).
At the same time, apply central venous indwelling catheter for patients. To improve patient compliance and facilitate patient treatment, intermittent hemodialysis method should be used to control blood flow of hemodialysis within 300 ml per minute. Perform 4 hours’ dialysis treatment every day (August et al., 2016).
2.3. Evaluation method
Compare hemodialysis effect and survival rate 1 year after follow-up to generate sound clinical observation index.
2.4. Statistical methods
For diabetic patients in experimental study, obtained clinical data is tested with software package SPSS15.0. Among them, obtained clinical count data is denoted by (n,%) and tested by chi-square test. After statistics, two sets of obtained experimental data P < 0.05, which indicates significant difference after grouping therapy.
3. Results
3.1. Comparison of survival rate after follow-up
After one year of follow-up of the two groups of patients, it can be found that: survival rate of diabetic nephropathy patients is 55.8% (726/1300), well below 78.3% in the control group (1018/1300). After statistical comparison, P < 0.05, difference is statistically significant.
3.2. Comparison of incidence of complications
Complications that occur during treatment of diabetic nephropathy patients and complications of non-diabetic nephropathy patients were compared: Incidence of complications of diabetic nephropathy patients is 86.5%, far higher than 58.6% of control group. After comparison, difference is obvious, P < 0.05, with significant statistical difference. Fig. 3 shows complication (proteinuria) of diabetic nephropathy patients.
Fig. 3.

A diabetic nephropathy patient with complication of proteinuria.
3.3. Disease research of diabetic nephropathy patients
Currently, the number of diabetic patients has started to increase greatly, and diabetic patients worldwide have grown to a certain number (Yi et al., 2014), which makes incidence of a serious complication of diabetes - diabetic nephropathy also significantly increase (Zhang Xiaoling et al., 2013). Diabetic nephropathy patients will suffer from serious kidney failure, with probability of kidney failure much higher than that of normal nephritic patients (Yang Xiaohua et al., 2012). Necessary hemodialysis treatment for diabetic patients can effectively improve health status of patients, which, however, can not restore patients’ health and even more, serious complications may occur, thus causing multiple organ failure and resulting in kidney failure. Compared to other types of kidney diseases, diabetic nephropathy will cause greater harm to patients and thus should attract enough attention from medical staff in clinical practice. In final stage, diabetic patients will have lowered insulin sensitivity. In this period, in order to better ensure patients’ blood glucose level, patients’ diet condition should be improved during hemodialysis treatment, and clinical use of insulin should be increased (Mellotte et al., 2015). However, at current stage, mostly sugar-free dialysis apparatus is adopted for hemodialysis of nephritic patient and each dialysis treatment will cause necessary loss of the body’s sugar. As a result, usage amount of insulin needs to be increased. There also exists difference between prognosis of diabetic nephropathy patients after hemodialysis and non-diabetic nephropathy patients (Lina et al., 2011). For diabetic nephropathy patients, intensity of hemodialysis needs to be strengthened. During treatment of patients, medical staff should strengthen supervision and control of such indexes as blood, blood glucose and blood lipids, etc. in order to better improve anemic condition of patients, effectively control impact on patients, and maintain patients’ nutritional balance. At the same time, complications of diabetic nephropathy patients during hemodialysis should also be effectively controlled, in order to better improve survival rate and effectively improve patients’ performance of clinical symptoms (Gu Bo et al., 2011). Fig. 4 shows CT image of a patient with kidney failure.
Fig. 4.
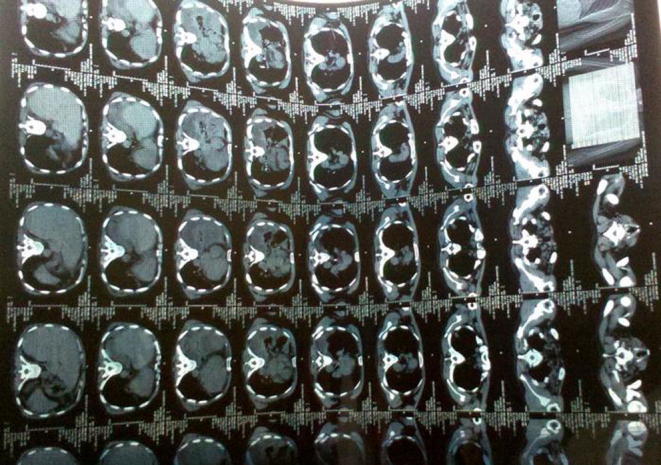
CT image of kidney failure.
4. Discussion
Treatment effect and quality of life of diabetic nephropathy patients and non-diabetic nephropathy patients are studied in this paper. The results indicate that diabetic nephropathy patients are with low resistance, great treatment difficulty, and the treatment process also easily leads to other complications, which causes a serious impact on physical health and life safety of patients. With the increasing number of diabetes, incidence of diabetic nephropathy has gradually increased, and prevention and treatment of diabetic nephropathy has become very important. On the one hand, observation of diabetic patients should be strengthened, and accurate diagnosis in the first time of diabetic nephropathy is needed, allowing patients to receive timely treatment. Also, strict control is needed to avoid serious complications. On the other hand, for diabetic nephropathy patients with complications, medical staff should strengthen blood glucose control, find important factors affecting quality of life of diabetic nephropathy patients, and then effectively improve quality of life of diabetic patients. In addition, other renal replacement therapy can be adopted for treatment of end stage renal disease, and kidney transplant can be carried out to effectively improve quality of life of patients. With the development and progress of medical level, the medical community will certainly find more effective methods for treatment of diabetic nephropathy, and thus effectively promote health of patients, improve quality of life and survival quality of diabetic patients, so that prognosis life of diabetic patients becomes happier and more colorful.
Footnotes
Peer review under responsibility of King Saud University.
References
- August D.A., Kallogjeri D., Lewison G., Chen X. Nutrition support in surgical oncology. Asian Pac. J. Surg. Oncol. 2016;2(3):153–162. [Google Scholar]
- Gu Bo Lu., Jianrao Yi Yang, Hanqing Wang, Xuan Yi. Bone metabolism of elderly 2 type diabetic nephropathy patients with maintenance hemodialysis. Chinese J. Blood Purificat. 2011;26(08):440–443. [Google Scholar]
- Lina Li., Xiang Li., Yan Xu. ultrasound evaluation of vascular endothelial function of diabetic nephropathy patients with hemodialysis. Chinese J. Med. Imag. Tech. 2011;31(07):1422–1425. [Google Scholar]
- Meicai Yang, Sufen Li, Min Tian. Application of Comprehensive Nursing Intervention in Hemodialysis of Diabetic Nephropathy Patients. China Med. Pharmacy. 2013;2(13):146–147. [Google Scholar]
- Mellotte G., Maher V., Devitt P.G., Shin V.Y., Leung C.P. Minimally invasive surgical oncology: state of the art. Asian Pac. J. Surg. Oncol. 2015;1(2):101–112. [Google Scholar]
- Peng Bin Xu., Tao Wang Niansong, Xiaohua Sheng. Impact of hemodialysis combined with hemodiafiltration on cardiac structure and function of diabetic nephropathy patients with maintenance hemodialysis. Chinese J. Integrat. Tradit. Western Nephrol. 2014;14(02):129–133. [Google Scholar]
- Xiaohua Yang, Xiaojun Han, Chong Yan. Effects of high flux hemodialysis on prognosis of diabetic nephropathy patients with hemodialysis. J. Pract. Med. 2012;1(2):2009–2010. [Google Scholar]
- Yi Li, Chen Rui Wu., Guofeng Lou Aiju. Anemia treatment comparison of diabetic nephropathy patients and hemodialysis patient with chronic glomerulonephritis. Guangzhou Med. 2014;4(05):31–33. [Google Scholar]
- Yindi Liang. Nursing measures to improve quality of life of diabetic nephropathy patients with hematodialysis. Contemporary Med. 2013;33(18):131–132. [Google Scholar]
- Zhang Xiaoling, Bai Jiuxu, Han Jingming, Wang Donghui, Cui Hanmin, Cao Ning. Blood Clcium, Serum Phosphate and Parathyroid Hormone Levels of Diabetic Nephropathy and Non-Diabetic Nephropathy Patients with Maintenance Hemodialysis. Progress in Modern Biomedicine, 2013, 4 (30): 5896-5899 + 5928.


