Abstract
Anteroinferior glenohumeral instability can be treated by variants of the Bankart repair, remplissage, and the Latarjet procedure, although all options remain associated with complications, including recurrence, stiffness, persistent pain, apprehension, and dislocation arthropathy. The authors therefore thought of a concept of dynamic anterior stabilization to treat anteroinferior glenohumeral instability by transferring the long head of the biceps within a subscapularis split to the anterior glenoid margin, thereby creating a “sling effect” by using a conservative technique. A standard Bankart repair is then to re-establish the labral damper effect. The main benefit of the dynamic anterior stabilization procedure is that it grants the “sling effect,” but is easier and safer than arthroscopic Latarjet. It does not require screws nor traction of the coracoid process, and should therefore reduce the risks of neurologic damage. Furthermore, the procedure can be performed with only 3 small incisions, because it does not require coracoid transfer, which eliminates risks of nerve dissection, graft overhang, and cortical resorption, hence reducing the probability for dislocation arthroplasty. Lastly, the pectoralis minor remains intact, which would avoid scapular dyskinesis.
Anteroinferior glenohumeral instability can be treated by various surgical techniques, depending on whether the underlying etiology is labral tear (Bankart),1 humeral head lesion (Malgaigne or Hill-Sachs),2, 3 or glenoid bone defect.4 The treatment options include variants of the Bankart repair, which may be combined with remplissage,5 as well as the Latarjet procedure,6 all of which are associated with complications.7, 8, 9, 10, 11, 12
The Bankart repair reattaches the torn labrum to the glenoid rim,13 and is usually combined with a capsular shift in the inferosuperior direction that Neer and Foster14 described for multidirectional instability. The outcomes of isolated Bankart repairs have been mediocre, with recurrence rates up to 67%,4 leading surgeons to supplement them with other protective procedures.
Remplissage is performed in the presence of humeral head lesions, by tightening the infraspinatus tendon and/or the teres minor muscle8 and posterior capsule within the defect, rendering it extra-articular. Common complications of remplissage include shoulder stiffness,15, 16, 17, 18 persistent pain,11 and failure of tendon healing.19
When traditional arthroscopic Bankart repair is not possible due to severe capsulolabral deficiency, different types of open or arthroscopic subscapularis tendon augmentation or capsular reconstruction have been described.20, 21, 22, 23, 24, 25
The Latarjet procedure transfers the coracoid process to the anterior portion of the glenoid creating a “triple effect”: (1) osseous, extending the glenoid articular surface; (2) ligamentous, by coracoacromial ligament reinforcement of the inferior glenohumeral ligament; and (3) muscular, through conjoined tendon transfer that lowers the inferior portion of the subscapularis and acts as a sling on the inferior subscapularis and the anteroinferior capsule with the arm abducted and externally rotated.26
The procedure is arthroscopically challenging, however, due to difficulties of screw positing,7 risks of nerve damage,9 and the need to fuse cortical bone to the glenoid.7 The Latarjet procedure is also associated with complications due to bone overhang,27 superior graft resorption,27 persistent apprehension, and recurrent dislocation.7, 28
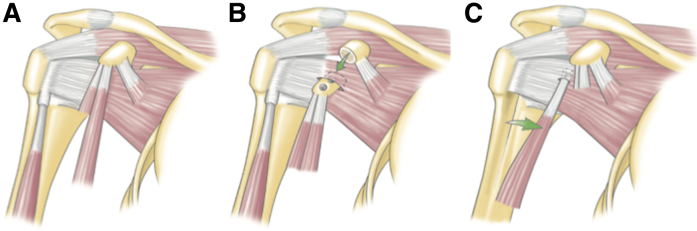
The purpose of this Technical Note is therefore to present a dynamic anterior stabilization (DAS) to treat anteroinferior glenohumeral instability, by transferring the long head of the biceps (LHB) to the anterior glenoid margin, thereby creating a “sling effect” by using a conservative technique (Fig 1). Indications for DAS are anteroinferior glenohumeral instability with limited bone defects, associated with SLAP, or in overhead athletes and throwers. Conversely, contraindication for DAS would include the following: greater bone defects, presence of LHB lesions or spontaneous rupture, associated subscapularis lesion, and previous LHB tenotomy or tenodesis.
Fig 1.
(A) Native shoulder. (B) Latarjet procedure. The coracoid graft including the conjoint tendon is secured to the anterior glenoid by means of two 4.5-mm screws. (C) Dynamic anterior stabilization. The long head of the biceps is transferred to the anterior glenoid margin.
Surgical Technique
Preoperative Patient Positioning
The operation, illustrated in Video 1, is performed in the semi-beach chair position under general anesthesia with an interscalene block. An examination under anesthesia is performed before prepping and draping the arm. Table 1 explains the tips, pitfall, and key points of this technique.
Table 1.
Pearls and Pitfalls
| Pearls |
|
| Pitfalls |
|
Initial Exposure and Portal Placement
An intra-articular approach is used through a standard posterior portal (soft spot); a standard diagnostic arthroscopy is performed with a 30° arthroscope and a pump maintaining pressure at 60 mm Hg. Anterolateral and anterior portals are then established by an outside-in technique using a spinal needle as a guide. The rotator interval is opened, and the internal structures (glenoid defects, humeral defects, etc.) are further assessed with the probe (VAPR, DePuy Mitek, Raynham, MA).
Anterior Glenoid Preparation
From a lateral viewing portal, the labrum, if necessary, is detached from the glenoid, and a suture is passed around the labrum and pulled through the posterior portal to increase access for preparation of the anterior glenoid (Fig 2). The glenoid neck is cleaned from soft tissues at around 3 o'clock with a burr (Omnicut, DePuy Mitek).
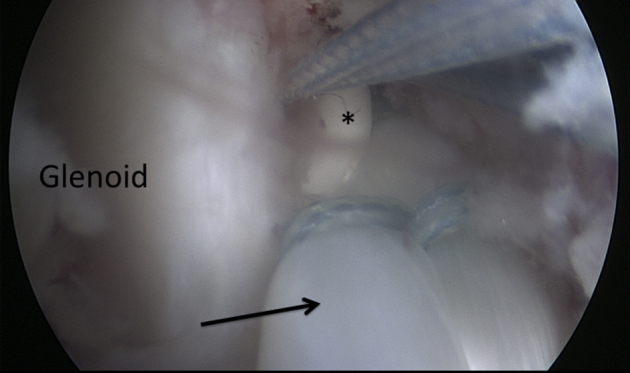
Fig 2.
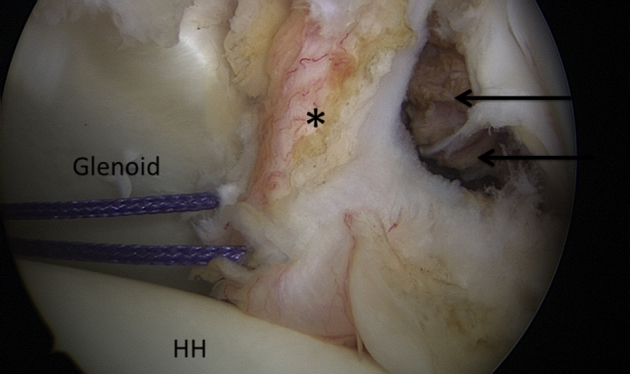
Intra-articular view of a right shoulder, anterolateral viewing portal. A suture is passed around the detached labrum and pulled through the posterior portal to increase access for preparation of the anterior glenoid. ∗ indicates the labrum, the black arrows the access to the glenoid neck, and HH the humeral head.
Addressing the LHB and Subscapularis Split
The LHB is then tenotomized and the biciptal groove is opened laterally and distally to avoid detaching the subscapularis (Fig 3).29 The biceps is then exteriorized, secured using a SpeedWhip technique with No. 2 FiberLoop 20 mm from the proximal tendon. From a lateral viewing portal the subscapularis is exposed on 3 sides,30 together with the lateral margin of the conjoint tendon. Two options exist to create a split in the middle of the subscapularis31 above the junction of the superior two-thirds used in the standard Latarjet procedure32: From a lateral viewing portal, either a switching stick (Wissinger Rod) can be passed across the glenohumeral joint through a posterior approach at the level of the inferior glenoid (Fig 4), or an outside-in approach can be used.33 The switching stick is now found in the retrocoracoid space and maintained lateral to the conjoint tendon to avoid damaging the nerve plexus. The probe is then introduced through the anterior portal to complete the split.
Fig 3.
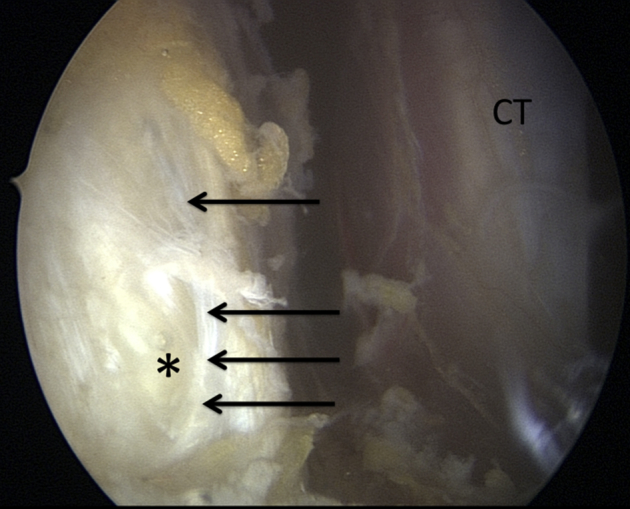
Retrocoracoid space of a right shoulder, anterolateral viewing portal. After LHB tenotomy, the bicipital sheath (black arrows) is opened laterally and the LHB (∗) is found. (CT, conjoint tendon; LHB, long head of the biceps.)
Fig 4.
Intraoperative view of a right shoulder with passage of the switching stick (∗) across the glenohumeral joint at the level of the inferior glenoid to the subscapularis. (HH, humeral head.)
LHB Tenodesis to Anterior Glenoid
A drill is then used to prepare a hole at 3 o'clock from anterior to posterior within the neck of the glenoid, 1.5 to 2.0 cm deep, depending on the length of the interference screw. The LHB tendon is then passed through the subscapularis split into the predrilled hole, to establish the “sling effect,” and fixed using a SwiveLock Tenodesis screw (Arthrex, Naples, FL) (Fig 5).
Fig 5.
Intraoperative view of a right shoulder through the subscapularis split, anterolateral viewing portal. The long head of the biceps tendon (black arrow) is fixed using a tenodesis screw (∗) to establish the “sling effect.”
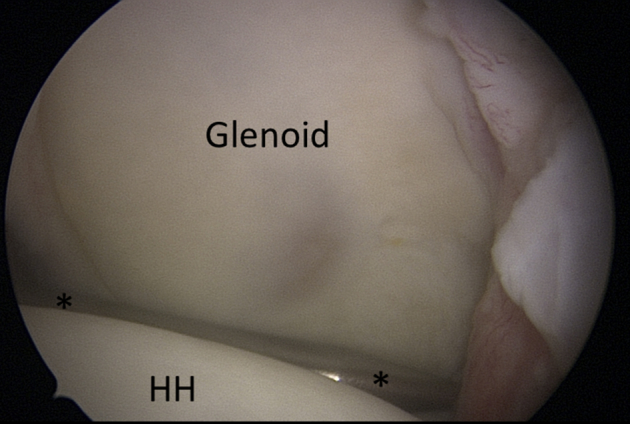
Labral Repair
With the arthroscope through the posterior portal, a standard Bankart repair is performed using 2 to 3 suture anchors. The anchors are placed on the glenoid rim at 3, 4, and 5 o'clock to enable the retension of the capsuloligamentous structures and to re-establish the labral damper effect (Video 1 and Fig 6).
Fig 6.
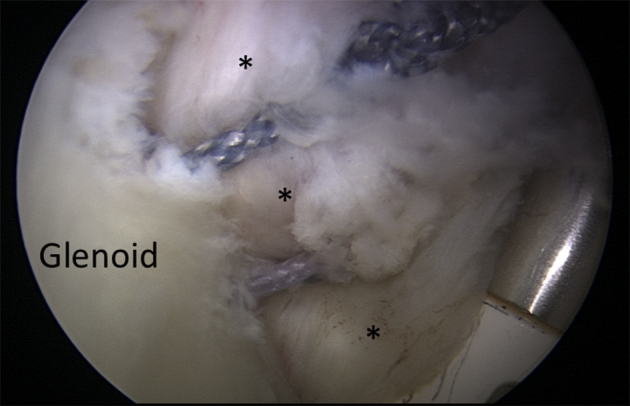
Intra-articular view through the posterior portal. Associated capsulolabral repair using 2 to 3 anchors recreates normal articular concavity (bumper effect). The anchors are placed on the glenoid rim between 3 and 6 o'clock, depending on the lesion. ∗ indicates the labrum.
Postoperative Rehabilitation
Patients are instructed to wear a simple sling for 10 days encouraging rest and reducing the risk of postoperative hematoma formation. Rehabilitation with self-mobilization in elevation and external rotation is allowed from day 0. At 10 days, activities of daily living are allowed and self-mobilization in elevation and external rotation continued. Return to low-risk sports (e.g., jogging, cycling, and swimming) is allowed at 6 weeks, and high-risk (throwing and collision) sports at 3 months only after satisfactory clinical and radiographic evaluations confirm satisfactory healing of the coracoid graft. Initially, no physiotherapy is recommended. Nevertheless, if persistent apprehension is observed,34, 35, 36 a multidisciplinary approach can be recommended. This can include (1) a “reafferentation” of the shoulder based on a neuromuscular and proprioceptive work,37 (2) a neurofeedback therapy,38 (3) a cognitive behavioral approach to decondition the pathological residual apprehension by highlighting to the patients that residual micromotion does not necessarily lead to recurrent instability,39 and finally with (4) a rotator cuff reinforcement to avoid further dysfunction due to muscle fatigue.
Discussion
Bankart, remplissage, and Latarjet procedures are proven treatments for anteroinferior glenohumeral instability. Each procedure has its set of limitations related to technical difficulties, recurrence of dislocation, and/or complications, which is why the authors sought other concepts for simplified techniques.
Several investigations have shown that an important stabilizing factor results from the “sling effect.”40, 41, 42 Furthermore, Giles et al.40 demonstrated in a biomechanical study that the “sling effect” is unlikely to limit internal-external rotation ROM beyond the native physiologic level. Therefore the main benefit of the DAS procedure is that it not only grants the “sling effect,” but is also easier and safer than arthroscopic Latarjet. Moreover, it does not require screws nor traction of the coracoid process, and should consequently reduce the risks of neurologic damage.9, 43 Furthermore, the procedure can be performed with only 3 small incisions (Video 1), because it does not require coracoid transfer, which eliminates risks of nerve dissection, graft overhang, and cortical resorption, hence reducing the probability for dislocation arthroplasty.10, 44 Lastly, the pectoralis minor remains intact, which would avoid scapular dyskinesis.45
The potential drawbacks of DAS are that it relies on the LHB tendon, which has smaller diameter than the conjoint tendon, and could therefore have a weaker “sling effect” than that of the standard Latarjet. Also, there are, like in the Latarjet procedure, the risks of biceps pain, and secondary iatrogenic factors. Furthermore, it does not involve bony reconstruction, and may therefore be inadequate for cases with massive bone loss.4 Table 2 summarizes the advantages and disadvantages of this technique. We believe that the indications and limitations (Table 3) are yet to be defined and it is recommended that future studies are carried out with a more long-term follow-up.
Table 2.
Advantages and Disadvantages
| Advantages |
|
| Disadvantages |
|
LHB, long head of the biceps.
Table 3.
Indications and Contraindications
| Indications | Anteroinferior glenohumeral instability with limited bone defects (<20%) |
| Relative contraindications | Anteroinferior glenohumeral instability with intermediate bone defects (20% to 30%), instability in pitchers without SLAP lesions, subscapularis lesions |
| Absolute contraindications | Anteroinferior glenohumeral instability with important bone defects (>30%), presence of biceps lesions or spontaneous rupture, and previous LHB tenotomy or tenodesis |
LHB, long head of the biceps.
In view of the aforementioned pros and cons, the most suitable indications for DAS would be anteroinferior glenohumeral instability with limited bone defects (<20%). Conversely, contraindication for DAS would include the following: greater bone defects, presence of biceps lesions or spontaneous rupture, and previous LHB tenotomy or tenodesis.
Encouraged by the successes of previous techniques, it is believed that DAS presented here will provide a promising alternative to the surgical treatments for anteroinferior glenohumeral instability.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: P.C. receives consultancy fees from Wright Medical and Smith & Nephew; and receives royalties from Wright Medical, Storz, and Advanced Medical Applications. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Dynamic anterior stabilization in a 17-year-old patient. After preparing the anterior glenoid, a tenotomy of the long head of the biceps (LHB) is performed. The LHB is then calibrated outside the body. After subscapularis split, the LHB is fixed in the anterior glenoid with a tenodesis screw to create the sling effect. Finally, a standard Bankart repair is realized.
References
- 1.Bankart A.S. Recurrent or habitual dislocation of the shoulder-joint. Br Med J. 1923;2:1132–1133. doi: 10.1136/bmj.2.3285.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hill H., Sachs M. The grooved defect of the humeral head. A frequently unrecognized complication of dislocations of the shoulder joint. Radiology. 1940;35:690–700. [Google Scholar]
- 3.Malgaigne J. J.-B. Baillière; Paris: 1855. Traité des fractures et des luxations. [Google Scholar]
- 4.Burkhart S.S., De Beer J.F. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: Significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16:677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 5.Wolf E., Pollack M. Hill-Sachs “remplissage”: An arthroscopic solution for the engaging Hill-Sachs lesion. Arthroscopy. 2004;20:e14–e15. doi: 10.1016/j.arthro.2008.03.015. [DOI] [PubMed] [Google Scholar]
- 6.Latarjet M. Treatment of recurrent dislocation of the shoulder. Lyon Chir. 1954;49:994–997. [PubMed] [Google Scholar]
- 7.Cunningham G., Benchouk S., Kherad O., Lädermann A. Comparison of arthroscopic and open Latarjet with a learning curve analysis. Knee Surg Sports Traumatol Arthrosc. 2016;24:540–545. doi: 10.1007/s00167-015-3910-3. [DOI] [PubMed] [Google Scholar]
- 8.Lädermann A., Arrigoni P., Barth J. Is arthroscopic remplissage a tenodesis or capsulomyodesis? An anatomic study. Knee Surg Sports Traumatol Arthrosc. 2016;24:573–577. doi: 10.1007/s00167-015-3756-8. [DOI] [PubMed] [Google Scholar]
- 9.Lädermann A., Denard P.J., Burkhart S.S. Injury of the suprascapular nerve during Latarjet procedure: An anatomic study. Arthroscopy. 2012;28:316–321. doi: 10.1016/j.arthro.2011.08.307. [DOI] [PubMed] [Google Scholar]
- 10.Lädermann A., Lubbeke A., Stern R., Cunningham G., Bellotti V., Gazielly D.F. Risk factors for dislocation arthropathy after Latarjet procedure: A long-term study. Int Orthop. 2013;37:1093–1098. doi: 10.1007/s00264-013-1848-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nourissat G., Kilinc A.S., Werther J.R., Doursounian L. A prospective, comparative, radiological, and clinical study of the influence of the “remplissage” procedure on shoulder range of motion after stabilization by arthroscopic Bankart repair. Am J Sports Med. 2011;39:2147–2152. doi: 10.1177/0363546511416315. [DOI] [PubMed] [Google Scholar]
- 12.Shah A.A., Butler R.B., Romanowski J., Goel D., Karadagli D., Warner J.J. Short-term complications of the Latarjet procedure. J Bone Joint Surg Am. 2012;94:495–501. doi: 10.2106/JBJS.J.01830. [DOI] [PubMed] [Google Scholar]
- 13.Bankart A. The pathology and treatment of the recurrent dislocation of the shoulder joint. Br J Surg. 1938;26:23–29. [Google Scholar]
- 14.Neer C.S., II, Foster C.R. Inferior capsular shift for involuntary inferior and multidirectional instability of the shoulder. A preliminary report. J Bone Joint Surg Am. 1980;62:897–908. [PubMed] [Google Scholar]
- 15.Boileau P., O'Shea K., Vargas P., Pinedo M., Old J., Zumstein M. Anatomical and functional results after arthroscopic Hill-Sachs remplissage. J Bone Joint Surg Am. 2012;94:618–626. doi: 10.2106/JBJS.K.00101. [DOI] [PubMed] [Google Scholar]
- 16.Garcia G.H., Wu H.H., Liu J.N., Huffman G.R., Kelly J.D., IV Outcomes of the remplissage procedure and its effects on return to sports: Average 5-year follow-up. Am J Sports Med. 2016;44:1124–1130. doi: 10.1177/0363546515626199. [DOI] [PubMed] [Google Scholar]
- 17.Ko S.H., Cha J.R., Lee C.C., Hwang I.Y., Choe C.G., Kim M.S. The influence of arthroscopic remplissage for engaging Hill-Sachs lesions combined with Bankart repair on redislocation and shoulder function compared with Bankart repair alone. Clin Orthop Surg. 2016;8:428–436. doi: 10.4055/cios.2016.8.4.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Merolla G., Paladini P., Di Napoli G., Campi F., Porcellini G. Outcomes of arthroscopic Hill-Sachs remplissage and anterior Bankart repair: A retrospective controlled study including ultrasound evaluation of posterior capsulotenodesis and infraspinatus strength assessment. Am J Sports Med. 2015;43:407–414. doi: 10.1177/0363546514559706. [DOI] [PubMed] [Google Scholar]
- 19.Bonnevialle N, Azoulay V, Faraud A, Elia F, Swider P, Mansat P. Results of arthroscopic Bankart repair with Hill-Sachs remplissage for anterior shoulder instability [published online May 11, 2017]. Int Orthop. doi:10.1007/s00264-017-3491-5. [DOI] [PubMed]
- 20.Denard P.J., Narbona P., Lädermann A., Burkhart S.S. Bankart augmentation for capsulolabral deficiency using a split subscapularis tendon flap. Arthroscopy. 2011;27:1135–1141. doi: 10.1016/j.arthro.2011.02.032. [DOI] [PubMed] [Google Scholar]
- 21.Maiotti M., Massoni C., Russo R., Schroter S., Zanini A., Bianchedi D. Arthroscopic subscapularis augmentation of Bankart repair in chronic anterior shoulder instability with bone loss less than 25% and capsular deficiency: Clinical multicenter study. Arthroscopy. 2017;33:902–909. doi: 10.1016/j.arthro.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 22.Maiotti M., Russo R., Zanini A., Schroter S., Massoni C., Bianchedi D. Arthroscopic Bankart repair and subscapularis augmentation: An alternative technique treating anterior shoulder instability with bone loss. J Shoulder Elbow Surg. 2016;25:898–906. doi: 10.1016/j.jse.2015.09.025. [DOI] [PubMed] [Google Scholar]
- 23.Russo R., Della Rotonda G., Cautiero F. Arthroscopic Bankart repair associated with subscapularis augmentation (ASA) versus open Latarjet to treat recurrent anterior shoulder instability with moderate glenoid bone loss: Clinical comparison of two series. Musculoskelet Surg. 2017;101:75–83. doi: 10.1007/s12306-016-0446-8. [DOI] [PubMed] [Google Scholar]
- 24.Warner J.J., Marks P.H. Reconstruction of the antero-superior shoulder capsule with the subscapularis tendon: A case report. J Shoulder Elbow Surg. 1993;2:260–263. doi: 10.1016/S1058-2746(09)80087-6. [DOI] [PubMed] [Google Scholar]
- 25.Warner J.J., Venegas A.A., Lehtinen J.T., Macy J.J. Management of capsular deficiency of the shoulder. A report of three cases. J Bone Joint Surg Am. 2002;84:1668–1671. doi: 10.2106/00004623-200209000-00023. [DOI] [PubMed] [Google Scholar]
- 26.Patte D, Debeyre J. [Luxations récidivantes de l'épaule]. Paris: Tech Chir Orthop. Encycl Med Chir 1980;44265:4.4-02.
- 27.Barth J., Neyton L., Metais P. Is the two-dimensional computed tomography scan analysis reliable for coracoid graft positioning in Latarjet procedures? J Shoulder Elbow Surg. 2017;26:e237–e242. doi: 10.1016/j.jse.2016.12.067. [DOI] [PubMed] [Google Scholar]
- 28.Metais P., Clavert P., Barth J. Preliminary clinical outcomes of Latarjet-Patte coracoid transfer by arthroscopy vs. open surgery: Prospective multicentre study of 390 cases. Orthop Traumatol Surg Res. 2016;102:S271–S276. doi: 10.1016/j.otsr.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 29.Godenèche A., Nové-Josserand L., Audebert S. Relationship Between Subscapularis Tears and Injuries to the Biceps Pulley. Knee Surg Sports Traumatol Arthrosc. 2017;25:2114–2120. doi: 10.1007/s00167-016-4374-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Denard P.J., Lädermann A., Burkhart S.S. Arthroscopic management of subscapularis tears. Sports Med Arthrosc Rev. 2011;19:333–341. doi: 10.1097/JSA.0b013e31822d41c6. [DOI] [PubMed] [Google Scholar]
- 31.Lafosse L., Boyle S., Gutierrez-Aramberri M., Shah A., Meller R. Arthroscopic Latarjet procedure. Orthop Clin North Am. 2010;41:393–405. doi: 10.1016/j.ocl.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 32.Young A.A., Maia R., Berhouet J., Walch G. Open Latarjet procedure for management of bone loss in anterior instability of the glenohumeral joint. J Shoulder Elbow Surg. 2011;20:S61–S69. doi: 10.1016/j.jse.2010.07.022. [DOI] [PubMed] [Google Scholar]
- 33.Lädermann A, Denard P, Arrigoni P, Narbona P, Burkhart S, Barth J. Level of the subscapularis split during arthroscopic Latarjet [published online August 16, 2017]. Arthroscopy. doi:10.1016/j.arthro.2017.06.013. [DOI] [PubMed]
- 34.Haller S., Cunningham G., Lädermann A. Shoulder apprehension impacts large-scale functional brain networks. AJNR Am J Neuroradiol. 2014;35:691–697. doi: 10.3174/ajnr.A3738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zanchi D., Cunningham G., Lädermann A., Ozturk M., Hoffmeyer P., Haller S. Brain activity in the right-frontal pole and lateral occipital cortex predicts successful post-operatory outcome after surgery for anterior glenohumeral instability. Sci Rep. 2017;7:498. doi: 10.1038/s41598-017-00518-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zanchi D., Cunningham G., Lädermann A., Ozturk M., Hoffmeyer P., Haller S. Structural white matter and functional connectivity alterations in patients with shoulder apprehension. Sci Rep. 2017;7:42327. doi: 10.1038/srep42327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fyhr C., Gustavsson L., Wassinger C., Sole G. The effects of shoulder injury on kinaesthesia: A systematic review and meta-analysis. Man Ther. 2015;20:28–37. doi: 10.1016/j.math.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 38.deCharms R.C., Maeda F., Glover G.H. Control over brain activation and pain learned by using real-time functional MRI. Proc Natl Acad Sci USA. 2005;102:18626–18631. doi: 10.1073/pnas.0505210102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lädermann A., Denard P.J., Tirefort J. Does surgery for instability of the shoulder truly stabilize the glenohumeral joint? A prospective comparative cohort study. Medicine (Baltimore) 2016;95:e4369. doi: 10.1097/MD.0000000000004369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Giles J.W., Boons H.W., Elkinson I. Does the dynamic sling effect of the Latarjet procedure improve shoulder stability? A biomechanical evaluation. J Shoulder Elbow Surg. 2013;22:821–827. doi: 10.1016/j.jse.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 41.Wellmann M., Petersen W., Zantop T. Open shoulder repair of osseous glenoid defects: Biomechanical effectiveness of the Latarjet procedure versus a contoured structural bone graft. Am J Sports Med. 2009;37:87–94. doi: 10.1177/0363546508326714. [DOI] [PubMed] [Google Scholar]
- 42.Yamamoto N., Muraki T., An K.N. The stabilizing mechanism of the Latarjet procedure: A cadaveric study. J Bone Joint Surg Am. 2013;95:1390–1397. doi: 10.2106/JBJS.L.00777. [DOI] [PubMed] [Google Scholar]
- 43.Clavert P., Lutz J.C., Wolfram-Gabel R., Kempf J.F., Kahn J.L. Relationships of the musculocutaneous nerve and the coracobrachialis during coracoid abutment procedure (Latarjet procedure) Surg Radiol Anat. 2009;31:49–53. doi: 10.1007/s00276-008-0426-2. [DOI] [PubMed] [Google Scholar]
- 44.Lädermann A., Benchouk S., Denard P. Traumatic anterior shoulder instability: General concepts & proper management. In: Park J., editor. Vol 1. Springer; Berlin/Heidelberg: 2015. (Sports injuries to the shoulder and elbow). [Google Scholar]
- 45.Carbone S., Moroder P., Runer A., Resch H., Gumina S., Hertel R. Scapular dyskinesis after Latarjet procedure. J Shoulder Elbow Surg. 2016;25:422–427. doi: 10.1016/j.jse.2015.08.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Dynamic anterior stabilization in a 17-year-old patient. After preparing the anterior glenoid, a tenotomy of the long head of the biceps (LHB) is performed. The LHB is then calibrated outside the body. After subscapularis split, the LHB is fixed in the anterior glenoid with a tenodesis screw to create the sling effect. Finally, a standard Bankart repair is realized.