Abstract
Objective
Reduced resilience, a construct associated with maladaptive stress coping and a predisposing vulnerability for Functional Neurological Disorders (FND), has been under-studied compared to other neuropsychiatric factors in FND. This prospective case-control study investigated self-reported resilience in patients with FND compared to controls and examined relationships between resilience and affective symptoms, personality traits, alexithymia, health status and adverse life event burden.
Methods
50 individuals with motor FND and 47 healthy controls participated. A univariate test followed by a logistic regression analysis investigated group-level differences in Connor-Davidson Resilience Scale (CD-RISC) scores. For within-group analyses performed separately in patients with FND and controls, univariate screening tests followed by multivariate linear regression analyses examined factors associated with self-reported resilience.
Results
Adjusting for age, gender, education status, ethnicity and lifetime adverse event burden, patients with FND reported reduced resilience compared to controls. Within-group analyses in patients with FND showed that individual-differences in mental health, extraversion, conscientiousness, and openness positively correlated with CD-RISC scores; post-traumatic stress disorder symptom severity, depression, anxiety, alexithymia and neuroticism scores negatively correlated with CD-RISC scores. Extraversion independently predicted resilience scores in patients with FND. In control subjects, univariate associations were appreciated between CD-RISC scores and gender, personality traits, anxiety, alexithymia and physical health; conscientiousness independently predicted resilience in controls.
Conclusion
Patients with FND reported reduced resilience, and CD-RISC scores covaried with other important predisposing vulnerabilities for the development of FND. Future research should investigate if the CD-RISC is predictive of clinical outcomes in patients with FND.
Keywords: conversion disorder, psychogenic nonepileptic seizures, functional movement disorders, resilience, personality
1. Introduction
Functional Neurological Disorder (FND)/Conversion Disorder (CD), a common neuropsychiatric condition, is characterized by unexplained limb weakness, gait difficulties, non-epileptic seizures, abnormal movements and sensory deficits(1). Despite its prevalence and significant healthcare costs, many clinicians are uncomfortable treating FND(2). Advancements in the assessment of FND emphasize the evaluation of predisposing vulnerabilities, acute precipitants and perpetuating factors(3). Predisposing vulnerabilities, the focus of this article, include maladaptive stress coping strategies, personality traits, psychiatric co-morbidities, alexithymia, and adverse life events among other variables(4–7). While studies have documented the importance of these factors, limited research to date has investigated relationships between resilience and other predisposing vulnerabilities associated with the development of FND.
Though initially conceptualized as an individual trait, resilience is recognized as a dynamic construct involving adaptability, sustainability, and recovery in the face of stress or trauma over the lifespan(8, 9). To date, few studies in FND have specifically investigated group-level differences in resilience. One study used the Connor-Davidson Resilience Scale (CD-RISC), a widely used and validated psychometric measure of stress coping abilities(10), to record that patients with psychogenic nonepileptic seizures (PNES) exhibiting altered ictal responsiveness reported lower resilience compared to individuals showing preserved ictal responsiveness(11). Another study showed that patients with mixed FND compared to those with general medical conditions reported lower resilience(12). Importantly, no studies to our knowledge have previously investigated within-group associations between self-reported resilience and other predisposing vulnerabilities across the spectrum of motor FND, which includes not only PNES but also functional movement disorders and functional limb weakness(13, 14).
Studies in FND populations have demonstrated the importance of impaired stress coping using several distinct psychometric instruments(5, 15–20). Patients with PNES, for example, consistently report using emotion-focused coping strategies such as distancing or escape-avoidance, while relying less on active problem-solving approaches(5, 15, 16). The use of emotion-focused coping strategies in patients with PNES correlates with depression, trauma-related intrusive experiences, alexithymia, and anger(17). In FND, men may use avoidant coping more often than women, indicating potential gender differences in coping styles(18). Patients with functional movement disorders and/or functional paralysis also report using active coping strategies less frequently than controls(19). Similarly, individuals with other medically unexplained somatic symptoms report using maladaptive emotion-focused coping strategies at higher frequencies compared to healthy individuals(20).
Additional insights into neuropsychiatric and psychosocial factors associated with resilience may be gained through studies conducted in other clinical and healthy populations. Several studies have demonstrated that personality traits such as neuroticism are negatively associated with resilience, while extraversion and consciousness have been connected to enhanced resilience(21, 22). In individuals faced with adverse life events, reduced resilience is associated with increased rates of depression, post-traumatic stress disorder (PTSD), and poor prognosis(23, 24). Other factors commonly associated with resilience include attachment style, spirituality, the tendency to experience positive emotions, and family and social support structures(25, 26).
This prospective case-control study investigated group-level differences in resilience in 50 patients with motor FND compared to 47 control subjects. Thereafter, univariate tests followed by multivariate linear regression analyses examined relationships between CD-RISC scores and self-reported mood/anxiety, PTSD symptoms, personality traits, alexithymia, adverse life event burden and health status in patients with FND. Within-group analyses were also performed separately in healthy subjects to determine which factors represented markers of perceived resilience across populations and which variables were specifically linked to resilience in patients with FND. We hypothesized that patients with FND would report decreased resilience compared to controls, and that maladaptive personality traits, increased affective and trauma-related symptoms, and impaired health status would be associated with reduced resilience in patients with FND.
2. Methods
2.1 Subjects
50 patients with motor FND (mean age=40.8±12.5; 37 women, 13 men; illness duration=3.4±3.8) were prospectively recruited from the Massachusetts General Hospital FND Clinic(13). Patients met criteria for clinically-established functional movement disorder (n=26)(27), PNES (18 documented; 1 clinically-established; 2 probable)(28), and/or functional limb weakness (n=18 with positive exam findings, 1 with probable paroxysmal functional weakness based on history and longitudinal follow-up) (Supplemental Table 1). 16 of 50 had mixed-motor FND; 15 also showed functional speech symptoms and 12 exhibited splitting of the midline sensory deficits. To be representative of the FND population, patients with major neurologic comorbidities (n=6) and/or co-morbid epileptic seizures (n=4) were also included (Supplemental Table 2). Exclusion criteria included illiteracy, history of mania or psychosis, active suicidality, current illicit drug abuse or alcohol dependence. 47 control subjects (mean age=37.7±11.8; 34 women, 13 men) were also recruited by internet advertisements from the greater Boston metropolitan area. All subjects provided written informed consent as approved by the Institutional Review Board of Partners HealthCare.
2.2 Psychometric Measures
As the primary study measure, subjects completed the CD-RISC(10). As part of a detailed psychometric battery, all subjects also completed the following self-report measures: Patient Health Questionnaire-15 (PHQ-15)(29), Screening for Somatoform Symptoms Conversion Disorder Subscale (SOMS:CD)(30), Dissociative Experience Scale (DES)(31), Somatoform Dissociation Questionnaire-20 (SDQ)(32), Short Form Health Survey (SF-36)(33), Beck Depression Inventory-II (BDI)(34), Spielberger State-Trait Anxiety Inventory (STAI-T)(35), NEO Five-Factor Inventory-3 (NEO)(36), Toronto Alexithymia Scale (TAS)(37), Childhood Trauma Questionnaire (CTQ)(38), Life Events Checklist-5 (LEC)(39) and PTSD Checklist-5 (PCL)(40).
The CD-RISC is a widely used and validated measure of adaptive stress coping consisting of 25-items scored on a 5-point Likert scale ranging from “not true at all” (0) to “true nearly all the time”(4). Higher scores reflect greater levels of perceived resilience. The PHQ-15 is a 15-item measure of somatic symptoms within the past 4 weeks, while the SOMS:CD is a measure of functional neurological symptom severity within the past 7 days. The DES and SDQ are measures of psychological and somatoform dissociation respectively. The SF-36 is a 36-item index of health status, which consists of two summary composite domains: mental health and physical health. The STAI-T is a 40-item questionnaire of trait and state anxiety, and the BDI is a 21-item self-report measure for depression. The TAS is a measure of difficulty identifying and describing feelings (alexithymia) consisting of 20 items rated on a 5-point scale. The NEO consists of 60 items assessing 5 personality domains including neuroticism, extraversion, openness, agreeableness, and conscientiousness. To assess childhood/adolescent trauma and lifetime adverse event burden, the CTQ and LEC-5 “happened to me” indices were used. In addition, patients and controls participated in a Structured Clinical Interview for DSM-IV-TR Axis I Disorders (SCID). See Supplemental Table 1 for psychiatric diagnoses in FND patients. All control subjects denied a clinical history of psychiatric diagnoses on telephone screens, however, 6 met SCID criteria for mild lifetime psychiatric co-morbidities (2 with current anxiety not otherwise specified) (Supplemental Table 3).
2.3 Statistical Analyses
Since CD-RISC scores were not normally distributed in controls (Shapiro-Wilks normality test p=0.004), a Mann-Whitney U test was performed to evaluate group-level differences between patients with FND and controls. Thereafter, a multivariate logistic regression analysis assessed if group-level differences remained significant adjusting for age, gender, education status, ethnicity and LEC “happened to me” scores.
For within-group analyses examining associations between CD-RISC scores and demographic, clinical and psychometric variables, we first performed univariate screening tests (Pearson correlations or unpaired two-tailed t-tests in FND patients with normally distributed CD-RISC scores or Mann-Whitney U tests and Spearman correlations in controls). Thereafter, variables showing a statistically significant relationship with the dependent variable (CD-RISC score) (p<0.05) were included in second-level linear regression analyses to examine independent predictors of self-reported resilience in patients with FND and controls separately. The percent variance explained by the models is shown using R2 values. All analyses were performed in IBM SPSSv23 (Chicago).
3. Results
3.1 Between Group Findings
In univariate tests, patients with FND reported lower CD-RISC scores (p<0.001; mean score 63.2±16.5) compared to controls (mean score 78.7±12.1); 24 of 50 patients with FND were within one standard deviation of the mean score observed in the control group. In a logistic regression analysis adjusting for age, gender, education status, ethnicity and LEC “happened to me” trauma burden, CD-RISC scores independently predicted having a diagnosis of FND compared to controls (odds ratio (OR)=0.95; 95% confidence interval (CI)=0.90–0.99; p=0.032). Note, this finding remained statistically significant if trauma burden was removed as a covariate of non-interest from the model (p<0.001).
3.2 Within-Group FND Findings
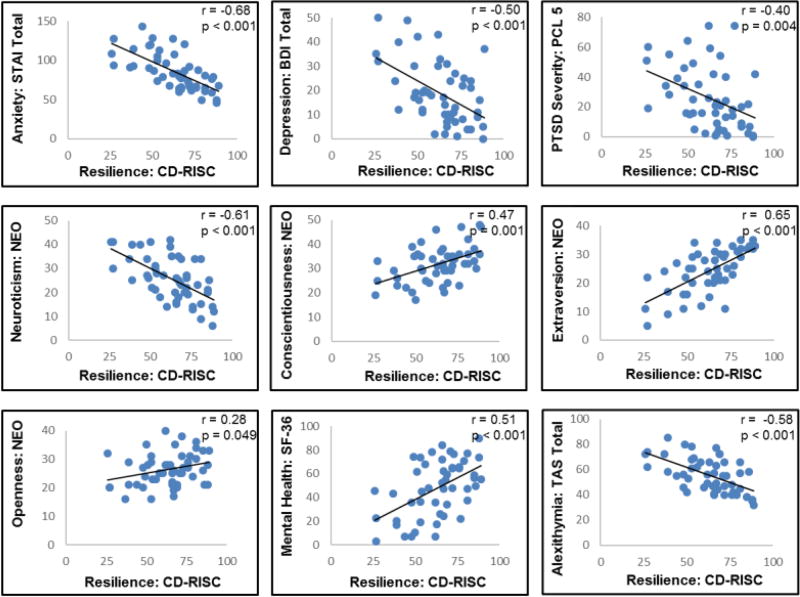
In univariate tests, four variables showed positive associations with CD-RISC scores: SF-36: mental health (Pearson correlation coefficient=0.51, p<0.001); NEOextraversion (Pearson correlation coefficient=0.65, p<0.001); NEO-conscientiousness (Pearson correlation coefficient=0.47, p=0.001); and NEO-openness (Pearson correlation coefficient=0.28, p=0.049) (Table 1, Figure 1). Five distinct variables demonstrated negative associations with CD-RISC scores: PCL-5: PTSD severity (Pearson correlation coefficient=-0.40, p=0.004); BDI-II (Pearson correlation coefficient=−0.50, p<0.001); STAI-total (Pearson correlation coefficient=−0.68, p<0.001); NEO-neuroticism (Pearson correlation coefficient=−0.61, p<0.001) and TAS (Pearson correlation coefficient=−0.58, p<0.001). There were no univariate associations between motor FND subtypes and CD-RISC scores. In a single linear regression analysis including the 9 statistically significant variables, only NEO-extraversion independently predicted CD-RISC scores (standardized beta= 0.35; p=0.006) (Table 2). 66.7% of the data variance was explained by the model. In a post hoc regression analysis including history of epileptic seizures and/or major neurological comorbidities as separate covariates-of-noninterest, the relationship between CD-RISC scores and NEO-extraversion remained statistically significant (standardized beta=0.39; p=0.004).
Table 1.
Within Group Univariate Associations with Self-Reported Resilience (CD-RISC) in Motor Functional Neurologic Disorders
| FND (n=50) | Test Statistics | P-Value | |
|---|---|---|---|
|
| |||
| Age | 40.8±12.5 | 0.05 | 0.75 |
|
| |||
| Male (n=13) vs. Female (n=37) | 63.3±19.4 | 0.02 | 0.98 |
| 63.2±15.7 | |||
|
| |||
| White (n=46) vs. non-white (n=4) | 64.0±16.0 | 1.04 | 0.30 |
| 55.0±23.1 | |||
|
| |||
| College graduate (n=18) vs. non-college graduate (n=32) | 68.7±12.8 | 1.81 | 0.077 |
| 60.1±17.7 | |||
|
| |||
| PNES (n=21) vs. other FND (n=29) | 59.5±14.5 | −1.37 | 0.18 |
| 65.9±17.5 | |||
|
| |||
| FMD (n=26) vs. other FND (n=24) | 65.6±16.8 | 1.07 | 0.29 |
| 60.6±16.1 | |||
|
| |||
| FW (n=19) vs. other FND (n=31) | 66.1±15.4 | 0.97 | 0.33 |
| 61.5±17.2 | |||
|
| |||
| SOMS: CD | 8.6±7.4 | −0.007 | 0.96 |
|
| |||
| PHQ-15 | 13.2±5.2 | −0.14 | 0.34 |
|
| |||
| SDQ | 32.2±10.5 | 0.002 | 0.99 |
|
| |||
| SF-36 mental | 47.8±23.6 | 0.51 | <0.001 |
|
| |||
| SF-36 physical | 47.1±23.2 | 0.052 | 0.72 |
|
| |||
| DES | 19.3±14.8 | −0.28 | 0.050 |
|
| |||
| PTSD: PCL 5* | 25.7±20.7 | −0.40 | 0.004 |
|
| |||
| CTQ-abuse | 29.0±13.5 | −0.071 | 0.62 |
|
| |||
| CTQ- neglect | 20.4±8.4 | −0.033 | 0.82 |
|
| |||
| LEC | 4.4±2.8 | −0.18 | 0.22 |
|
| |||
| BDI-II | 18.9±12.9 | −0.50 | <0.001 |
|
| |||
| STAI-total | 85.4±23.5 | −0.68 | <0.001 |
|
| |||
| TAS | 55.5±13.6 | −0.58 | <0.001 |
|
| |||
| NEO-neuroticism | 25.5±9.3 | −0.61 | <0.001 |
|
| |||
| NEO-extraversion | 24.4±7.6 | 0.65 | <0.001 |
|
| |||
| NEO-conscientiousness | 31.7±7.5 | 0.47 | 0.001 |
|
| |||
| NEO-agreeableness | 35.6±4.7 | −0.012 | 0.94 |
|
| |||
| NEO-openness | 26.3±5.7 | 0.28 | 0.049 |
Test statistic refers to independent sample t-test for continuous variables or Pearson correlation coefficient for dichotomous group comparisons.
Indicates that one subject had missing data for the PTSD: PCL 5.
CD-RISC, Connor-Davidson Resilience Scale; PNES, Psychogenic Non-Epileptic Seizures; FMD, Functional Movement Disorder; FW, Functional Weakness; FND, motor Functional Neurological Disorder; SOMS: CD, Conversion Disorder Subscale of the Screening for Somatoform Symptoms-7 scale; PHQ-15, Patient Health Questionnaire-15; SDQ, Somatoform Dissociation Questionnaire; SF-36; Short Form Health Survey-36; DES, Dissociative Experience Scale; PTSD: PCL 5, Post-Traumatic Stress Disorder Checklist for DSM-5; CTQ, Childhood Trauma Questionnaire; LEC, Life Events Checklist happened to me score; BDI, Beck Depression Inventory-II; STAI, Spielberger State Trait Anxiety Inventory; TAS, Toronto Alexithymia Score; NEO, NEO Five Factor Inventory.
Figure 1. Univariate Relationships Between Resilience and Other Predisposing Vulnerabilities in Motor Functional Neurologic Disorders.
Displayed are the nine statistically significant psychometric correlations with Connor-Davidson Resilience Scale (CD-RISC) scores in patients with functional neurological disorders. STAI Total, Spielberger State Trait Anxiety Inventory; BDI, Beck Depression Inventory-II; PCL 5, Post-Traumatic Stress Disorder Checklist for DSM-5; NEO, NEO Five-Factor Inventory 3; TAS, Toronto Alexithymia Scale.
Table 2.
Linear Regression Factors Associated with Self-Reported Resilience (CD-RISC) in Functional Neurologic Disorders
| Significant variables identified by univariate tests |
Standardized beta |
95% Confidence Interval |
P-Value |
|---|---|---|---|
| BDI-II | 0.054 | −0.37–0.51 | 0.75 |
| STAI-total | −0.35 | −0.52–0.02 | 0.071 |
| PTSD: PCL 5 | −0.10 | −0.32–0.15 | 0.49 |
| TAS | −0.16 | −0.52–0.13 | 0.23 |
| SF-36 mental | −0.033 | −0.28–0.23 | 0.86 |
| NEO-neuroticism | 0.024 | −0.58–0.66 | 0.89 |
| NEO-extraversion | 0.35 | 0.24–1.28 | 0.006 |
| NEO-conscientiousness | 0.20 | −0.02–0.91 | 0.059 |
| NEO-openness | 0.16 | −0.20–1.09 | 0.17 |
CD-RISC, Connor-Davidson Resilience Scale; BDI, Beck Depression Inventory-II; STAI, Spielberger State Trait Anxiety Inventory; PTSD: PCL 5, Post-Traumatic Stress Disorder Checklist for DSM-5; TAS, Toronto Alexithymia Score; SF-36; Short Form Health Survey-36; NEO, NEO Five Factor Inventory.
3.3 Within-Group Control Subject Findings
In univariate tests, women reported greater resilience (CD-RISC mean=81.8±11.7) compared to men (CD-RISC mean=70.5±9.5; p=0.002). In addition, CD-RISC scores were positively associated with three variables: SF-36: physical health (Spearman correlation coefficient=0.35, p=0.015); NEO-extraversion (Spearman correlation coefficient=0.48, p=0.001); and NEO-conscientiousness (Spearman correlation coefficient=0.65, p<0.001). Three variables were also negatively associated with CD-RISC scores: STAI-total (Spearman correlation coefficient=−0.49, p<0.001); NEO-neuroticism (Spearman correlation coefficient=−0.34, p=0.020); and TAS scores (Spearman correlation coefficient=−0.37, p<0.011) (Supplemental Table 4). In a single linear regression analysis including these 7 statistically significant variables, only NEO-conscientiousness independently predicted CD-RISC scores (standardized beta=0.38; p=0.005) (Table 3). 61.5% of the data variance was explained by the model.
Table 3.
Linear Regression Factors Associated with Self-Reported Resilience (CD-RISC) in Control Subjects
| Significant variables identified by univariate tests |
Standardized beta |
95% Confidence Interval |
P- Value |
|---|---|---|---|
| Gender | 0.17 | −1.48–10.85 | 0.13 |
| SF36 physical health | 0.095 | −0.17–0.44 | 0.37 |
| STAI-total | −0.069 | −0.39–0.27 | 0.70 |
| TAS | −0.094 | −0.42–0.18 | 0.42 |
| NEO-neuroticism | −0.13 | −0.85–0.37 | 0.43 |
| NEO-extraversion | 0.21 | −0.07–0.76 | 0.10 |
| NEO-conscientiousness | 0.38 | 0.26–1.31 | 0.005 |
CD-RISC, Connor-Davidson Resilience Scale; STAI, Spielberger State Trait Anxiety Inventory; SF-36; Short Form Health Survey-36; TAS, Toronto Alexithymia Score; NEO, NEO Five Factor Inventory.
4. Discussion
This case-control study investigated between-group and within-group associations with self-reported resilience in patients with FND and controls. We confirmed the hypothesis that patients with FND would report lower CD-RISC scores compared to controls. In addition, CD-RISC scores in patients with FND correlated with individual differences in personality traits, depression/anxiety, trauma-related symptoms, alexithymia, and mental health. In a multivariate regression analysis, extraversion independently predicted increased resilience in patients with FND. In controls, relationships were observed between CD-RISC scores and gender, personality traits, alexithymia, anxiety and physical health. Notably, personality dimensions, anxiety and alexithymia were associated with perceived resilience across FND and control subjects. There were no differences in CD-RISC scores across motor FND subtypes, highlighting the utility of a trans-diagnostic approach to research in this population.
Our between-group finding of decreased reported resilience in patients with FND compared to non-clinical control subjects has not been previously described using the CD-RISC. However, the concept of impaired resilience is consistent with theories that predisposing vulnerabilities for the development of functional neurologic symptoms in some patients relate to maladaptive stress responses, often in an indirect, nuanced fashion(4). Proposed models for the pathogenesis of FND offer multiple stages where resilience may play an important role(3, 14). For example, low resilience may act as a predisposing and/or perpetuating factor, interacting dynamically with remote and ongoing psychosocial stressors. Furthermore, poor prognosis in FND has been linked to maladaptive personality characteristics, depression, and anxiety(41), which resembles the relationships between resilience and neuropsychiatric variables observed in our FND cohort.
In FND patients, we observed positive associations between resilience scores and extraversion, conscientiousness, and openness, and a negative relationship between resilience and neuroticism. Higher extraversion scores were the only independent predictor of resilience. In psychiatric populations, personality characteristics such as extraversion and openness have positively correlated with adaptive coping, while neuroticism is a consistently identified risk factor for the development of psychopathology(42). The positive association between extraversion and CD-RISC scores may relate to the tendency of extroverts to experience more interpersonal interactions, positive affect and social support(43). These factors can promote social networks and encourage individuals to seek out support in times of need(43).
While patients with FND exhibit heterogenous personality profiles, some exhibit maladaptive traits(44–47). One recent study of functional movement disorder and PNES cohorts investigated NEO-based personality dimensions, demonstrating that both FND sub-groups exhibited significantly higher levels of neuroticism compared to controls(48). This study also found that childhood emotional abuse correlated with neuroticism and inversely correlated with extraversion, openness to experiences and agreeableness. A study utilizing the Minnesota Multiphasic Personality Inventory (MMPI) and NEO proposed a clustering of personality sub-types in patients with PNES: “depressed neurotics”, “somatic defenders” and “activated neurotics”(47). Of note, extraversion was low in the “depressed neurotics” and average in the other two groups. Our results support the notion that extraverts with FND may have greater perceived resilience.
In patients with FND, higher resilience was also associated with lower depression, anxiety and PTSD symptom severity. Patients with FND exhibit high rates of depression, anxiety, and PTSD(4, 13, 49, 50). The negative association between psychiatric disorders and resilience has been described using the CD-RISC(10, 51, 52). Moreover, resilience correlates with lower mental health symptoms, favorable outcome in PTSD, and mediates treatment response in patients with depression(24, 51, 53–56). Studies also show that resilience is a potential protective factor against developing psychopathology after trauma(56, 57). A longitudinal study examining the protective effect of resilience as measured by the intersection of stressful life events and somatic/affective symptoms showed that individuals with greater baseline resilience were less likely to develop mood or anxiety disorders(58). Given the role of psychiatric co-morbidities as predisposing factors for FND, as well as links between health-related quality of life and affective symptoms(59, 60), it is notable that self-reported resilience co-varies with depression and anxiety in patients with FND.
Alexithymia, the reduced ability to identify and describe emotions, was also negatively associated with resilience in both patients with FND and controls. Alexithymic individuals have difficulty distinguishing between emotion-driven and other physical sensations and show deficits in the ability to recognize emotional distress(61). Furthermore, alexithymia is associated with poor health, other somatic symptom disorders, and increased rates of mood and anxiety disorders(62). While individual differences are present, associations between alexithymia and FND are well described(7, 48, 63–65). For example, in patients with PNES, alexithymia correlated with trauma symptoms, emotion-oriented coping strategies, demoralization, low positive emotion, and cynicism(17, 66). Patients with functional movement disorders in comparison to other movement disorders and healthy controls have reported elevated rates of alexithymia, which was also associated with obsessive-compulsive personality disorder(7). These findings highlight the close relationship between impairments in verbalizing emotional distress and reduced adaptive stress coping abilities.
In this study, mental health-related quality of life was associated with increased resilience in patients with FND, while higher physical health-related quality of life correlated with increased resilience in controls. These observations are notable given the absence of associations between CD-RISC scores, indices of functional neurological symptom severity, and trauma burden in the FND cohort. The lack of a clear relationship between CD-RISC scores and functional neurological symptoms is in striking contrast to the multiplicity of associations between resilience in personality dimensions, depression/anxiety, trauma symptoms, and alexithymia observed in patients with FND. Additional work is necessary to further disentangle the relationships between resilience, other psychiatric symptoms and physical health, particularly given robust associations between affective symptoms and health-related quality of life reported in FND(59).
In control subjects, we observed similar correlations between resilience and extraversion, conscientiousness, neuroticism, anxiety, and alexithymia. However, we also identified findings not appreciated in patients with FND, including a positive relationship between physical health and resilience, as well as increased reported resilience in women compared to men. The overlap of findings in the FND and control cohorts suggests that certain characteristics, particularly personality dimensions, are likely involved in resilience regardless of clinical status(67). While there has been considerable research at the intersection of personality and resilience, the relationship between gender and resilience is under-studied(68). Analyses of resilience, as well as related concepts such as post-traumatic growth, have been inconsistent with some studies demonstrating no differences between men and women(43, 69, 70), and others showing modest gender differences(71–73). Additional research is needed to investigate potential relationships between adaptive coping, gender, and physical health.
In recent years, mind-body therapies have received increased attention in Western medicine and these interventions show efficacy in patients with depression(74), PTSD(75), and chronic pain(76) among other stress-related non-communicable disorders. It has been hypothesized that interventions designed to both decrease stress through meditative practices and to enhance resilience through social support, positive psychology training, and life-style modifications can reduce vulnerability to stress-related conditions(77). For example, mindfulness-based relaxation response and stress-management training programs are linked to improved coping and a heightened sense of self-efficacy, along with reduced depression and anxiety(78). Given that a subset of patients with FND remain symptomatic despite receiving an updated standard of care(79), future studies should investigate the utility of adjunctive mind-body interventions in the management of FND.
Limitations of this study include the use of self-report measures and the relatively low number of male subjects. The CD-RISC is a validated scale, however, there may be a mismatch between patient self-report and objective markers of resilience, indicating that more research is needed. Future research should combine self-report measures of resilience with laboratory-based stress provocation paradigms measuring autonomic and neuroendocrine reactivity to further disentangle these issues. Also, our FND cohort spans the spectrum of motor FND framed as including functional movement disorders, functional limb weakness and PNES. We used this trans-diagnostic approach given the commonly encountered overlap across subtypes(13, 14, 80), although we acknowledge that this remains debated in the field(81). It is important to highlight that there were no observed relationships between CD-RISC scores and motor FND subtypes. A strength of the study is the inclusion of patients with neurologic comorbidities as is common in FND, while also adjusting for the presence of neurologic comorbidities in within-group regression analyses. In addition, 6 out of 47 controls had mild psychiatric co-morbidities as detected by the SCID (all screened negative for a history of psychiatric diagnoses on telephone interviews); this mild degree of psychopathology would, if relevant, likely reduce the magnitude of group-level differences in CD-RISC scores across patients with FND and controls. Future research should also investigate between-group differences in resilience in patients with FND compared to a random sample of the general population, trauma controls and those with other neurologic and psychiatric conditions. More research is also needed to investigate if some of the within-group correlations with CD-RISC scores are specific to patients with FND or largely common across neuropsychiatric conditions. Notably, 48% of patients with FND were within one standard deviation of the mean CD-RISC score in controls, further highlighting the importance of individual differences in the study of FND(82). Lastly, longitudinal treatment studies should investigate if baseline resilience profiles predict clinical outcomes(83, 84), as well as the extent to which resilience may be enhanced therapeutically.
In conclusion, patients with FND reported lower rates of resilience as measured by the CD-RISC compared to controls. We also demonstrated that CD-RISC scores in patients with FND covaried with several important predisposing vulnerabilities for the development of FND, including maladaptive personality traits, depression/anxiety, PTSD, and alexithymia. Future studies should examine the relationship between self-reported resilience and clinical outcomes in FND.
Supplementary Material
Supplemental Table 1. Demographic characteristics of patients with functional neurological disorders. †Indicates that these patients had splitting of the midline functional numbness. ††Indicates that patient also had a functional cognitive disorder. *Indicates that these patients also had functional speech. **Psychiatric diagnoses made by chart review, as structured psychiatric interview not performed. M, male; F, female; PNES, Psychogenic Nonepileptic Seizures; FW, Functional Weakness; FMD, Functional Movement Disorders; NOS, not otherwise specified; MDD, Major Depressive Disorder; PD_Ag+, Panic Disorder with Agoraphobia; PD_Ag−, Panic Disorder without Agoraphobia; GAD, Generalized Anxiety Disorder; Undiff Somatoform, Undifferentiated Somatoform Disorder; PTSD, Post-Traumatic Stress Disorder; OCD, Obsessive Compulsive Disorder; Ag, Agoraphobia without Panic Disorder; LOC, Loss of Consciousness; APM, Amphetamine; APZ, Aripiprazole; ATP, Amitriptyline; BSP, Buspirone; BUP, Bupropion; BZP, Benztropine; CLN, Clonidine; CLP, Clonazepam; CTP, Citalopram; CZP, Carbamazepine; DLX, Duloxetine; DNZ, donepezil; DOX, Doxepin; DVX, Desvenlafaxine; DXAM, Dextroamphetamine; DZP, Diazepam; ECP, Escitalopram; FLX, Fluoxetine; GBP, Gabapentin; LRZ, Lorazepam; LSD, Lysergic Acid Diethylamide; LTG, Lamotrigine; LXAM, Lisdexamfetamine; MIR, Mirtazapine; NRT, Nortriptyline; PGN, Pregabalin; PZN, Prazosin; QTP, Quetiapine; ROP, Ropinirole; SERT, Sertraline; THP, Trihexyphenidyl; TPM, Topiramate; TZD, Trazodone; VEN, Venlafaxine; VPA, Valproic Acid; VTX, Vortioxetine; ZLP, Zolpidem.
Supplemental Table 2. Major brain scan abnormalities in patients with functional neurological disorders. FND, functional neurological disorder; s/p, status-post, MCA, middle cerebral artery; TBI, traumatic brain injury; VP, ventriculoperitoneal.
Supplemental Table 3. Control subjects with psychiatric co-morbidities on structured psychiatric interview. Note: all other control subjects were without any psychiatric comorbidities as evaluated by a structured psychiatric interview. M, male; F, female; NOS, not otherwise specified; PD_Ag−, Panic Disorder without Agoraphobia.
Supplemental Table 4. Within group univariate associations with self-reported resilience (CD-RISC) in control subjects. Test statistic refers to Spearman correlation coefficients or z-scores derived from Mann Whitney U tests. HC, healthy controls; CD-RISC, Connor-Davidson Resilience Scale; SOMS: CD, Conversion Disorder Subscale of the Screening for Somatoform Symptoms-7 scale; PHQ-15, Patient Health Questionnaire-15; SDQ, Somatoform Dissociation Questionnaire; SF-36; Short Form Health Survey-36; DES, Dissociative Experience Scale; PTSD: PCL 5, Post-Traumatic Stress Disorder Checklist for DSM-5; CTQ, Childhood Trauma Questionnaire; LEC, Life Events Checklist happened to me score; BDI-II, Beck Depression Inventory-II; STAI, Spielberger State Trait Anxiety Inventory; TAS, Toronto Alexithymia Score; NEO, NEO Five-Factor Inventory 3.
Highlights.
Decreased self-reported resilience in Functional Neurological Disorders (FND).
Reduced resilience linked to mood/anxiety, PTSD, neuroticism and alexithymia in FND.
Extraversion independently predicted increased resilience in patients with FND.
Acknowledgments
D.L.P. was supported by the National Institute of Mental Health Grant 1K23MH111983-01A1, Sidney R. Baer Jr. Foundation, and the Massachusetts General Hospital Physician-Scientist Development Award.
M.S.K., consultant at Forum Pharmaceuticals; editor for Schizophrenia Research.
W.C.L., has served on the editorial boards of Epilepsia, Epilepsy & Behavior and Journal of Neuropsychiatry and Clinical Neurosciences; receives editor's royalties from the publication of Gates and Rowan's Nonepileptic Seizures, 3rd ed. (Cambridge University Press, 2010) and 4th ed. (2017); author’s royalties for Taking Control of Your Seizures: Workbook and Therapist Guide (Oxford University Press, 2015); has received research support from the NIH (NINDS 5K23NS45902 [PI]), Department of Defense, Rhode Island Hospital, the American Epilepsy Society (AES), the Epilepsy Foundation (EF), Brown University and the Siravo Foundation; serves on the Epilepsy Foundation Professional Advisory Board; has received honoraria for the American Academy of Neurology Annual Meeting Annual Course; has served as a clinic development consultant at University of Colorado Denver, Cleveland Clinic, Spectrum Health and Emory University; and has provided medico legal expert testimony.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures/Conflicts of Interest:
All other authors report no disclosures or conflicts of interest.
References
- 1.Stone J, LaFrance WC, Jr, Brown R, Spiegel D, Levenson JL, Sharpe M. Conversion disorder: current problems and potential solutions for DSM-5. J Psychosom Res. 2011;71(6):369–76. doi: 10.1016/j.jpsychores.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 2.McMillan KK, Pugh MJ, Hamid H, Salinsky M, Pugh J, Noel PH, et al. Providers' perspectives on treating psychogenic nonepileptic seizures: frustration and hope. Epilepsy Behav. 2014;37:276–81. doi: 10.1016/j.yebeh.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 3.Reuber M. The etiology of psychogenic non-epileptic seizures: toward a biopsychosocial model. Neurol Clin. 2009;27(4):909–24. doi: 10.1016/j.ncl.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 4.Roelofs K, Keijsers GP, Hoogduin KA, Naring GW, Moene FC. Childhood abuse in patients with conversion disorder. Am J Psychiatry. 2002;159(11):1908–13. doi: 10.1176/appi.ajp.159.11.1908. [DOI] [PubMed] [Google Scholar]
- 5.Goldstein LH, Drew C, Mellers J, Mitchell-O'Malley S, Oakley DA. Dissociation, hypnotizability, coping styles and health locus of control: characteristics of pseudoseizure patients. Seizure. 2000;9(5):314–22. doi: 10.1053/seiz.2000.0421. [DOI] [PubMed] [Google Scholar]
- 6.Kaplan MJ, Dwivedi AK, Privitera MD, Isaacs K, Hughes C, Bowman M. Comparisons of childhood trauma, alexithymia, and defensive styles in patients with psychogenic non-epileptic seizures vs. epilepsy: Implications for the etiology of conversion disorder. J Psychosom Res. 2013;75(2):142–6. doi: 10.1016/j.jpsychores.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 7.Demartini B, Petrochilos P, Ricciardi L, Price G, Edwards MJ, Joyce E. The role of alexithymia in the development of functional motor symptoms (conversion disorder) J Neurol Neurosurg Psychiatry. 2014;85(10):1132–7. doi: 10.1136/jnnp-2013-307203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rutter M. Resilience as a dynamic concept. Development and psychopathology. 2012;24(2):335–44. doi: 10.1017/S0954579412000028. [DOI] [PubMed] [Google Scholar]
- 9.Davydov DM, Stewart R, Ritchie K, Chaudieu I. Resilience and mental health. Clinical psychology review. 2010;30(5):479–95. doi: 10.1016/j.cpr.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 10.Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC) Depress Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 11.Baslet G, Tolchin B, Dworetzky BA. Altered responsiveness in psychogenic nonepileptic seizures and its implication to underlying psychopathology. Seizure. 2017;52:162–8. doi: 10.1016/j.seizure.2017.10.011. [DOI] [PubMed] [Google Scholar]
- 12.Bokharey IZ. Resilience and Coping Strategies in the Patients with Conversion Disorder and General Medical Conditions: A Comparative Study. Malaysian Journal of Psychiatry. 2013;22(1) 22. [Google Scholar]
- 13.Matin N, Young SS, Williams B, LaFrance WCJ, King JN, Caplan D, et al. Neuropsychiatric Associations with Gender, Illness Duration, Work Disability and Motor Subtype in a US Functional Neurological Disorders Clinic Population. J Neuropsychiatry Clin Neurosci. 2017;29(4):375–82. doi: 10.1176/appi.neuropsych.16110302. [DOI] [PubMed] [Google Scholar]
- 14.Perez DL, Dworetzky BA, Dickerson BC, Leung L, Cohn R, Baslet G, et al. An integrative neurocircuit perspective on psychogenic nonepileptic seizures and functional movement disorders: neural functional unawareness. Clin EEG Neurosci. 2015;46(1):4–15. doi: 10.1177/1550059414555905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Frances PL, Baker GA, Appleton PL. Stress and avoidance in Pseudoseizures: testing the assumptions. Epilepsy Res. 1999;34(2–3):241–9. doi: 10.1016/s0920-1211(98)00116-8. [DOI] [PubMed] [Google Scholar]
- 16.Testa SM, Krauss GL, Lesser RP, Brandt J. Stressful life event appraisal and coping in patients with psychogenic seizures and those with epilepsy. Seizure. 2012;21(4):282–7. doi: 10.1016/j.seizure.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 17.Myers L, Fleming M, Lancman M, Perrine K, Lancman M. Stress coping strategies in patients with psychogenic non-epileptic seizures and how they relate to trauma symptoms, alexithymia, anger and mood. Seizure. 2013;22(8):634–9. doi: 10.1016/j.seizure.2013.04.018. [DOI] [PubMed] [Google Scholar]
- 18.Myers L, Trobliger R, Bortnik K, Lancman M. Are there gender differences in those diagnosed with psychogenic nonepileptic seizures? Epilepsy Behav. 2017 doi: 10.1016/j.yebeh.2017.10.019. [DOI] [PubMed] [Google Scholar]
- 19.van Beilen M, Griffioen BT, Leenders KL. Coping strategies and IQ in psychogenic movement disorders and paralysis. Mov Disord. 2009;24(6):922–5. doi: 10.1002/mds.22428. [DOI] [PubMed] [Google Scholar]
- 20.Nater UM, Wagner D, Solomon L, Jones JF, Unger ER, Papanicolaou DA, et al. Coping styles in people with chronic fatigue syndrome identified from the general population of Wichita, KS. J Psychosom Res. 2006;60(6):567–73. doi: 10.1016/j.jpsychores.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 21.Park S, Naliboff B, Shih W, Presson A, Videlock E, Ju T, et al. Resilience is decreased in irritable bowel syndrome and associated with symptoms and cortisol response. Neurogastroenterology & Motility. 2017 doi: 10.1111/nmo.13155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Campbell-Sills L, Cohan SL, Stein MB. Relationship of resilience to personality, coping, and psychiatric symptoms in young adults. Behav Res Ther. 2006;44(4):585–99. doi: 10.1016/j.brat.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 23.Kukihara H, Yamawaki N, Uchiyama K, Arai S, Horikawa E. Trauma, depression, and resilience of earthquake/tsunami/nuclear disaster survivors of Hirono, Fukushima, Japan. Psychiatry and clinical neurosciences. 2014;68(7):524–33. doi: 10.1111/pcn.12159. [DOI] [PubMed] [Google Scholar]
- 24.Wingo AP, Wrenn G, Pelletier T, Gutman AR, Bradley B, Ressler KJ. Moderating effects of resilience on depression in individuals with a history of childhood abuse or trauma exposure. Journal of affective disorders. 2010;126(3):411–4. doi: 10.1016/j.jad.2010.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gloria CT, Steinhardt MA. Relationships among positive emotions, coping, resilience and mental health. Stress and Health. 2016;32(2):145–56. doi: 10.1002/smi.2589. [DOI] [PubMed] [Google Scholar]
- 26.Shibue Y, Kasai M. Relations between attachment, resilience, and Earned Security in Japanese University students. Psychological reports. 2014;115(1):279–95. doi: 10.2466/21.02.PR0.115c14z7. [DOI] [PubMed] [Google Scholar]
- 27.Williams DT, Ford B, Fahn S. Phenomenology and psychopathology related to psychogenic movement disorders. Adv Neurol. 1995;65:231–57. [PubMed] [Google Scholar]
- 28.LaFrance WC, Jr, Baker GA, Duncan R, Goldstein LH, Reuber M. Minimum requirements for the diagnosis of psychogenic nonepileptic seizures: a staged approach: a report from the International League Against Epilepsy Nonepileptic Seizures Task Force. Epilepsia. 2013;54(11):2005–18. doi: 10.1111/epi.12356. [DOI] [PubMed] [Google Scholar]
- 29.Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64(2):258–66. doi: 10.1097/00006842-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 30.Rief W, Hiller W. A new approach to the assessment of the treatment effects of somatoform disorders. Psychosomatics. 2003;44(6):492–8. doi: 10.1176/appi.psy.44.6.492. [DOI] [PubMed] [Google Scholar]
- 31.Bernstein EM, Putnam FW. Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis. 1986;174(12):727–35. doi: 10.1097/00005053-198612000-00004. [DOI] [PubMed] [Google Scholar]
- 32.Nijenhuis ER, Spinhoven P, Van Dyck R, Van der Hart O, Vanderlinden J. The development and psychometric characteristics of the Somatoform Dissociation Questionnaire (SDQ-20) J Nerv Ment Dis. 1996;184(11):688–94. doi: 10.1097/00005053-199611000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–83. [PubMed] [Google Scholar]
- 34.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 35.Spielberger CD, Gorsuch RL, Lushene RE. Manual for the state-trait anxiety inventory. 1970 [Google Scholar]
- 36.Costa PT, MacCrae RR. Revised NEO personality inventory (NEO PI-R) and NEO five-factor inventory (NEO-FFI): Professional manual: Psychological Assessment Resources, Incorporated. 1992 [Google Scholar]
- 37.Bagby RM, Taylor GJ, Parker JD. The twenty-item Toronto Alexithymia Scale—II. Convergent, discriminant, and concurrent validity. Journal of psychosomatic research. 1994;38(1):33–40. doi: 10.1016/0022-3999(94)90006-x. [DOI] [PubMed] [Google Scholar]
- 38.Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry. 1994;151(8):1132–6. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- 39.Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, Keane TM. The Life Events Checklist for DSM-5 (LEC-5) 2013 [Google Scholar]
- 40.Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. J Trauma Stress. 2015;28(6):489–98. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- 41.Gelauff J, Stone J, Edwards M, Carson A. The prognosis of functional (psychogenic) motor symptoms: a systematic review. J Neurol Neurosurg Psychiatry. 2014;85(2):220–6. doi: 10.1136/jnnp-2013-305321. [DOI] [PubMed] [Google Scholar]
- 42.Ormel J, Jeronimus BF, Kotov R, Riese H, Bos EH, Hankin B, et al. Neuroticism and common mental disorders: meaning and utility of a complex relationship. Clinical psychology review. 2013;33(5):686–97. doi: 10.1016/j.cpr.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Campbell-Sills L, Cohan SL, Stein MB. Relationship of resilience to personality, coping, and psychiatric symptoms in young adults. Behaviour research and therapy. 2006;44(4):585–99. doi: 10.1016/j.brat.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 44.Kranick S, Ekanayake V, Martinez V, Ameli R, Hallett M, Voon V. Psychopathology and psychogenic movement disorders. Movement Disorders. 2011;26(10):1844–50. doi: 10.1002/mds.23830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bodde NM, Bartelet DC, Ploegmakers M, Lazeron RH, Aldenkamp AP, Boon PA. MMPI-II personality profiles of patients with psychogenic nonepileptic seizures. Epilepsy & Behavior. 2011;20(4):674–80. doi: 10.1016/j.yebeh.2011.01.034. [DOI] [PubMed] [Google Scholar]
- 46.Reuber M, Pukrop R, Bauer J, Derfuss R, Elger C. Multidimensional assessment of personality in patients with psychogenic non-epileptic seizures. Journal of Neurology, Neurosurgery & Psychiatry. 2004;75(5):743–8. doi: 10.1136/jnnp.2003.013821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cragar DE, Berry DT, Schmitt FA, Fakhoury TA. Cluster analysis of normal personality traits in patients with psychogenic nonepileptic seizures. Epilepsy Behav. 2005;6(4):593–600. doi: 10.1016/j.yebeh.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 48.Ekanayake V, Kranick S, LaFaver K, Naz A, Frank Webb A, LaFrance WC, Jr, et al. Personality traits in psychogenic nonepileptic seizures (PNES) and psychogenic movement disorder (PMD): Neuroticism and perfectionism. J Psychosom Res. 2017;97:23–9. doi: 10.1016/j.jpsychores.2017.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stone J, Warlow C, Sharpe M. The symptom of functional weakness: a controlled study of 107 patients. Brain. 133(Pt 5):1537–51. doi: 10.1093/brain/awq068. [DOI] [PubMed] [Google Scholar]
- 50.Kranick S, Ekanayake V, Martinez V, Ameli R, Hallett M, Voon V. Psychopathology and psychogenic movement disorders. Mov Disord. 2011;26(10):1844–50. doi: 10.1002/mds.23830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hjemdal O, Vogel PA, Solem S, Hagen K, Stiles TC. The relationship between resilience and levels of anxiety, depression, and obsessive–compulsive symptoms in adolescents. Clinical psychology & psychotherapy. 2011;18(4):314–21. doi: 10.1002/cpp.719. [DOI] [PubMed] [Google Scholar]
- 52.Tan-Kristanto S, Kiropoulos LA. Resilience, self-efficacy, coping styles and depressive and anxiety symptoms in those newly diagnosed with multiple sclerosis. Psychology, health & medicine. 2015;20(6):635–45. doi: 10.1080/13548506.2014.999810. [DOI] [PubMed] [Google Scholar]
- 53.Hoge EA, Austin ED, Pollack MH. Resilience: research evidence and conceptual considerations for posttraumatic stress disorder. Depression and anxiety. 2007;24(2):139–52. doi: 10.1002/da.20175. [DOI] [PubMed] [Google Scholar]
- 54.Min J-A, Lee N-B, Lee C-U, Lee C, Chae J-H. Low trait anxiety, high resilience, and their interaction as possible predictors for treatment response in patients with depression. Journal of affective disorders. 2012;137(1):61–9. doi: 10.1016/j.jad.2011.12.026. [DOI] [PubMed] [Google Scholar]
- 55.Fava GA, Tomba E. Increasing psychological well-being and resilience by psychotherapeutic methods. Journal of personality. 2009;77(6):1903–34. doi: 10.1111/j.1467-6494.2009.00604.x. [DOI] [PubMed] [Google Scholar]
- 56.Wrenn GL, Wingo AP, Moore R, Pelletier MT, Gutman AR, Bradley B, et al. The effect of resilience on posttraumatic stress disorder in trauma-exposed inner-city primary care patients. Journal of the National Medical Association. 2011;103(7):560. doi: 10.1016/s0027-9684(15)30381-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pietrzak RH, Johnson DC, Goldstein MB, Malley JC, Rivers AJ, Morgan CA, et al. Psychosocial buffers of traumatic stress, depressive symptoms, and psychosocial difficulties in veterans of Operations Enduring Freedom and Iraqi Freedom: the role of resilience, unit support, and postdeployment social support. Journal of affective disorders. 2010;120(1):188–92. doi: 10.1016/j.jad.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 58.Sheerin CM, Lind MJ, Brown EA, Gardner CO, Kendler KS, Amstadter AB. The impact of resilience and subsequent stressful life events on MD and GAD. Depression and anxiety. 2017 doi: 10.1002/da.22700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jones B, Reuber M, Norman P. Correlates of health-related quality of life in adults with psychogenic nonepileptic seizures: A systematic review. Epilepsia. 2016;57(2):171–81. doi: 10.1111/epi.13268. [DOI] [PubMed] [Google Scholar]
- 60.LaFrance WC, Jr, Syc S. Depression and symptoms affect quality of life in psychogenic nonepileptic seizures. Neurology. 2009;73(5):366–71. doi: 10.1212/WNL.0b013e3181b04c83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Taylor GJ, Bagby RM, Parker JD. Disorders of affect regulation: Alexithymia in medical and psychiatric illness. Cambridge University Press; 1999. [Google Scholar]
- 62.Duddu V, Isaac M, Chaturvedi S. Alexithymia in somatoform and depressive disorders. Journal of psychosomatic research. 2003;54(5):435–8. doi: 10.1016/s0022-3999(02)00440-3. [DOI] [PubMed] [Google Scholar]
- 63.Gulpek D, Kelemence Kaplan F, Kesebir S, Bora O. Alexithymia in patients with conversion disorder. Nordic journal of psychiatry. 2014;68(5):300–5. doi: 10.3109/08039488.2013.814711. [DOI] [PubMed] [Google Scholar]
- 64.Kaplan MJ, Dwivedi AK, Privitera MD, Isaacs K, Hughes C, Bowman M. Comparisons of childhood trauma, alexithymia, and defensive styles in patients with psychogenic non-epileptic seizures vs. epilepsy: implications for the etiology of conversion disorder. Journal of psychosomatic research. 2013;75(2):142–6. doi: 10.1016/j.jpsychores.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 65.Brown RJ, Bouska JF, Frow A, Kirkby A, Baker GA, Kemp S, et al. Emotional dysregulation, alexithymia, and attachment in psychogenic nonepileptic seizures. Epilepsy Behav. 2013;29(1):178–83. doi: 10.1016/j.yebeh.2013.07.019. [DOI] [PubMed] [Google Scholar]
- 66.Myers L, Matzner B, Lancman M, Perrine K, Lancman M. Prevalence of alexithymia in patients with psychogenic non-epileptic seizures and epileptic seizures and predictors in psychogenic non-epileptic seizures. Epilepsy & Behavior. 2013;26(2):153–7. doi: 10.1016/j.yebeh.2012.11.054. [DOI] [PubMed] [Google Scholar]
- 67.Schneider TR, Rench TA, Lyons JB, Riffle RR. The influence of neuroticism, extraversion and openness on stress responses. Stress and Health. 2012;28(2):102–10. doi: 10.1002/smi.1409. [DOI] [PubMed] [Google Scholar]
- 68.Hirani S, Lasiuk G, Hegadoren K. The intersection of gender and resilience. Journal of psychiatric and mental health nursing. 2016;23(6–7):455–67. doi: 10.1111/jpm.12313. [DOI] [PubMed] [Google Scholar]
- 69.Ahmad S, Feder A, Lee EJ, Wang Y, Southwick SM, Schlackman E, et al. Earthquake impact in a remote South Asian population: Psychosocial factors and posttraumatic symptoms. Journal of traumatic stress. 2010;23(3):408–12. doi: 10.1002/jts.20535. [DOI] [PubMed] [Google Scholar]
- 70.Karaırmak Ö. Establishing the psychometric qualities of the Connor–Davidson Resilience Scale (CD-RISC) using exploratory and confirmatory factor analysis in a trauma survivor sample. Psychiatry research. 2010;179(3):350–6. doi: 10.1016/j.psychres.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 71.Eriksson M, Lindström B. Antonovsky’s sense of coherence scale and the relation with health: a systematic review. Journal of Epidemiology & Community Health. 2006;60(5):376–81. doi: 10.1136/jech.2005.041616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Stratta P, Capanna C, Patriarca S, de Cataldo S, Bonanni RL, Riccardi I, et al. Resilience in adolescence: gender differences two years after the earthquake of L’Aquila. Personality and Individual Differences. 2013;54(3):327–31. [Google Scholar]
- 73.Vishnevsky T, Cann A, Calhoun LG, Tedeschi RG, Demakis GJ. Gender differences in self-reported posttraumatic growth: A meta-analysis. Psychology of women quarterly. 2010;34(1):110–20. [Google Scholar]
- 74.D'Silva S, Poscablo C, Habousha R, Kogan M, Kligler B. Mind-body medicine therapies for a range of depression severity: a systematic review. Psychosomatics. 2012;53(5):407–23. doi: 10.1016/j.psym.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 75.Jindani F, Turner N, Khalsa SBS. A yoga intervention for posttraumatic stress: A preliminary randomized control trial. Evidence-Based Complementary and Alternative Medicine. 2015;2015 doi: 10.1155/2015/351746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lee C, Crawford C, Hickey A. Mind–body therapies for the self-management of chronic pain symptoms. Pain Medicine. 2014;15(S1):S21–S39. doi: 10.1111/pme.12383. [DOI] [PubMed] [Google Scholar]
- 77.Park ER, Traeger L, Vranceanu AM, Scult M, Lerner JA, Benson H, et al. The development of a patient-centered program based on the relaxation response: the Relaxation Response Resiliency Program (3RP) Psychosomatics. 2013;54(2):165–74. doi: 10.1016/j.psym.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 78.Sylvia LG, Bui E, Baier AL, Mehta DH, Denninger JW, Fricchione GL, et al. Resilient Warrior: A Stress Management Group to Improve Psychological Health in Service Members. Glob Adv Health Med. 2015;4(6):38–42. doi: 10.7453/gahmj.2015.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Glass SP, Matin N, Williams B, Mello J, Stephen CD, Young SS, et al. Neuropsychiatric Factors Linked to Adherence and Short-Term Outcome in a US Functional Neurological Disorders Clinic: A Retrospective Cohort Study. The Journal of neuropsychiatry and clinical neurosciences. 2017 doi: 10.1176/appi.neuropsych.17060117. appi. neuropsych. 17060117. [DOI] [PubMed] [Google Scholar]
- 80.McKenzie PS, Oto M, Graham CD, Duncan R. Do patients whose psychogenic non-epileptic seizures resolve, 'replace' them with other medically unexplained symptoms? Medically unexplained symptoms arising after a diagnosis of psychogenic non-epileptic seizures. J Neurol Neurosurg Psychiatry. 2011;82(9):967–9. doi: 10.1136/jnnp.2010.231886. [DOI] [PubMed] [Google Scholar]
- 81.Kanaan RAA, Duncan R, Goldstein LH, Jankovic J, Cavanna AE. Are psychogenic non-epileptic seizures just another symptom of conversion disorder? J Neurol Neurosurg Psychiatry. 2017;88(5):425–9. doi: 10.1136/jnnp-2017-315639. [DOI] [PubMed] [Google Scholar]
- 82.van der Hoeven RM, Broersma M, Pijnenborg GH, Koops EA, van Laar T, Stone J, et al. Functional (psychogenic) movement disorders associated with normal scores in psychological questionnaires: A case control study. J Psychosom Res. 2015;79(3):190–4. doi: 10.1016/j.jpsychores.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 83.Durrant J, Rickards H, Cavanna AE. Prognosis and outcome predictors in psychogenic nonepileptic seizures. Epilepsy Res Treat. 2011;2011:274736. doi: 10.1155/2011/274736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gelauff J, Stone J. Prognosis of functional neurologic disorders. Handb Clin Neurol. 2016;139:523–41. doi: 10.1016/B978-0-12-801772-2.00043-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1. Demographic characteristics of patients with functional neurological disorders. †Indicates that these patients had splitting of the midline functional numbness. ††Indicates that patient also had a functional cognitive disorder. *Indicates that these patients also had functional speech. **Psychiatric diagnoses made by chart review, as structured psychiatric interview not performed. M, male; F, female; PNES, Psychogenic Nonepileptic Seizures; FW, Functional Weakness; FMD, Functional Movement Disorders; NOS, not otherwise specified; MDD, Major Depressive Disorder; PD_Ag+, Panic Disorder with Agoraphobia; PD_Ag−, Panic Disorder without Agoraphobia; GAD, Generalized Anxiety Disorder; Undiff Somatoform, Undifferentiated Somatoform Disorder; PTSD, Post-Traumatic Stress Disorder; OCD, Obsessive Compulsive Disorder; Ag, Agoraphobia without Panic Disorder; LOC, Loss of Consciousness; APM, Amphetamine; APZ, Aripiprazole; ATP, Amitriptyline; BSP, Buspirone; BUP, Bupropion; BZP, Benztropine; CLN, Clonidine; CLP, Clonazepam; CTP, Citalopram; CZP, Carbamazepine; DLX, Duloxetine; DNZ, donepezil; DOX, Doxepin; DVX, Desvenlafaxine; DXAM, Dextroamphetamine; DZP, Diazepam; ECP, Escitalopram; FLX, Fluoxetine; GBP, Gabapentin; LRZ, Lorazepam; LSD, Lysergic Acid Diethylamide; LTG, Lamotrigine; LXAM, Lisdexamfetamine; MIR, Mirtazapine; NRT, Nortriptyline; PGN, Pregabalin; PZN, Prazosin; QTP, Quetiapine; ROP, Ropinirole; SERT, Sertraline; THP, Trihexyphenidyl; TPM, Topiramate; TZD, Trazodone; VEN, Venlafaxine; VPA, Valproic Acid; VTX, Vortioxetine; ZLP, Zolpidem.
Supplemental Table 2. Major brain scan abnormalities in patients with functional neurological disorders. FND, functional neurological disorder; s/p, status-post, MCA, middle cerebral artery; TBI, traumatic brain injury; VP, ventriculoperitoneal.
Supplemental Table 3. Control subjects with psychiatric co-morbidities on structured psychiatric interview. Note: all other control subjects were without any psychiatric comorbidities as evaluated by a structured psychiatric interview. M, male; F, female; NOS, not otherwise specified; PD_Ag−, Panic Disorder without Agoraphobia.
Supplemental Table 4. Within group univariate associations with self-reported resilience (CD-RISC) in control subjects. Test statistic refers to Spearman correlation coefficients or z-scores derived from Mann Whitney U tests. HC, healthy controls; CD-RISC, Connor-Davidson Resilience Scale; SOMS: CD, Conversion Disorder Subscale of the Screening for Somatoform Symptoms-7 scale; PHQ-15, Patient Health Questionnaire-15; SDQ, Somatoform Dissociation Questionnaire; SF-36; Short Form Health Survey-36; DES, Dissociative Experience Scale; PTSD: PCL 5, Post-Traumatic Stress Disorder Checklist for DSM-5; CTQ, Childhood Trauma Questionnaire; LEC, Life Events Checklist happened to me score; BDI-II, Beck Depression Inventory-II; STAI, Spielberger State Trait Anxiety Inventory; TAS, Toronto Alexithymia Score; NEO, NEO Five-Factor Inventory 3.