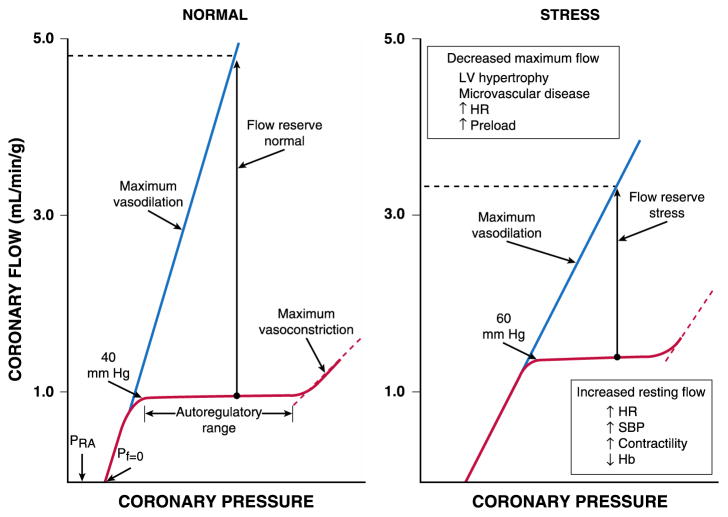
Fig. 1.
Autoregulatory relation under basal conditions and following metabolic stress (e.g., tachycardia). The normal heart maintains CBF constant (left panel) as regional coronary pressure is varied over a wide range when the global determinants of oxygen consumption are kept constant (red lines). Below the lower autoregulatory pressure limit (approximately 40 mm Hg), subendocardial vessels are maximally vasodilated and myocardial ischemia develops. During vasodilation (blue lines), flow increases four to five times above resting values at a normal arterial pressure. Coronary flow ceases at a pressure higher than right atrial pressure (PRA), called zero flow pressure (Pf = 0), which is the effective back pressure to flow in the absence of coronary collaterals. Following stress (right panel), tachycardia increases the compressive determinants of coronary resistance by decreasing the time available for diastolic perfusion and thus, reduces maximum vasodilated flow. Increases in myocardial oxygen demand or reductions in arterial oxygen content (e.g. from anemia or hypoxemia) increase resting flow. These changes reduce coronary flow reserve, the ratio between dilated and resting coronary flow, and cause ischemia to develop at higher coronary pressures. Abbreviations: LV, left ventricular; HR, heart rate; SBP, systolic blood pressure; Hb, hemoglobin. Reprinted from Canty and Duncker6 with permission.