Abstract
Background
This study provides a comprehensive, population-based examination of tobacco use among both career and volunteer firefighters.
Methods
Data are from a population-based cohort study of randomly selected career (N = 11) and volunteer (N = 13) departments comprised of 677 male firefighters.
Results
Unadjusted rates of smoking were 13.6% and 17.4% for career and volunteer firefighters, respectively. Smoking rates were less than a comparable occupational group (military personnel) and adult males in the states represented. Smokers were more likely to have been diagnosed with an anxiety disorder (OR = 5.8; P = 0.010), have an elevated CAGE alcohol problem score (OR = 2.9; P = 0.040), and more likely to report driving after drinking too much (OR = 4.5; P = 0.020) compared to never-smokers. Large percentages of career (18.4%) and volunteer (16.8%) firefighters used smokeless tobacco.
Conclusions
Smoking among firefighters is associated with other significant health and safety risks. High rates of smokeless tobacco use suggest that the fire service is an important target for intervention. Thus, despite strong statements against smoking by the fire service, the need to maintain high levels of health and fitness and relatively low smoking rates, a significant proportion of firefighters continue to use tobacco products.
Keywords: firefighters, fire service, tobacco, smoking, cigarettes, cigar, smokeless
INTRODUCTION
Firefighters are a vital component of our nation’s emergency and disaster response system and are charged with protecting the citizens and property in the communities they serve. The nature of this profession makes fire-fighting a physically and mentally demanding occupation. Firefighters must respond to emergencies on a moment’s notice and often face dangerous and challenging work conditions. Because of this, there has been a strong emphasis on health promotion in the fire service, including encouraging firefighters to be tobacco free. For instance, the Fire Service Joint Labor Management Wellness Fitness Initiative [WFI, 2008], the national model for health promotion in fire departments, suggests that all departments adopt the following policies toward tobacco use:
All new fire department candidates shall be tobacco free upon appointment and throughout their length of service to the department.
Current fire department uniformed personnel shall not use tobacco products (cigarettes, cigars, and/or chewing tobacco) inside the work-site, within or on fire department apparatus, or inside training facilities.
and
A fire department sanctioned tobacco cessation program shall be made available to incumbent tobacco users. Tobacco cessation programs must be non-punitive and must include both short and long term goals.
National fire services organizations have been proactive in promoting a tobacco-free fire service. For instance, the National Fallen Firefighters Everyone Goes Home Life Safety Initiatives include the call for all firefighters to “Stop using tobacco products—period!” [EGH, 2010]. The labor union representing firefighters, the International Association of Fire Fighters (IAFF), formed a partnership with Pfizer, a pharmaceutical company, to create the “Campaign for a Smoke-Free Union” which includes advice and help on quitting tobacco [IAFF, 2010]. In addition to the health effects of tobacco use on firefighters, smoking is the leading cause of fatal fires in the United States (US), resulting in 700–800 deaths each year and hundreds of millions of dollars in property loss [NFPA, 2010]. Furthermore, given the fire service provides much of the emergency medical response in the US, firefighters often witness the end results of tobacco use in the citizens they serve. Thus, it is not surprising that the national fire service has been a strong voice against tobacco use in its ranks and the hazards posed by smoking to lives and property.
Given the fire service’s stance against tobacco use, it is surprising that little research has been conducted on tobacco use among firefighters. We could find no comprehensive, large-scale epidemiological studies of tobacco use in the fire service. Nearly all national studies of smoking prevalence among occupational groups [e.g., NIOSH, 2011] report data in broad groups such as “police and fire-fighters” or “protective services” making it impossible to determine the unique rates among firefighters. One study reported the trends in smoking rates among occupational groups in the United States, including firefighters, from 1987 to 1994 [Lee et al., 2004] based on the National Health Interview Survey. They estimated that the average prevalence over that period was 26.9 (±3.7), although this estimate was based on a small sample of firefighters (n = 233).
While we could find no large-scale epidemiological studies of tobacco use in the fire service, there have been a few studies that provide evidence of historically high rates of smoking from self-selected health screenings or risk studies among small, convenience populations of firefighters or where firefighters were included as an occupational category in a larger population survey or longitudinal study [e.g., Dibbs et al., 1982; Large et al., 1990; Glueck et al., 1996; Lee et al., 2004; Yoo and Franke, 2009]. For example, Dibbs et al. [1982] found that the overall rate of smoking among firefighters who were screened for participation in the Normative Aging Study (which was based out of the Veterans Administration clinic in Boston, MA) was approximately 51.3%. Large et al. [1990] found that smokers represented 42% of their sample of firefighters from one municipal department. However, there have been no population-based studies systematically examining the prevalence of different forms of tobacco (e.g., cigarettes, cigars, and smokeless tobacco) or factors that may be associated with its use. Thus, there is a critical need for systematic epidemiological research on tobacco use among firefighters to guide prevention and treatment efforts. This study represents the first such effort among both career and volunteer firefighters and it is the first study to biochemically verify smoking status.
METHODS
Participating Fire Departments
The data reported are from the baseline evaluation of an ongoing longitudinal cohort study examining risk factors for injury in both career and volunteer firefighters (“A prospective evaluation of health behavior risk for injury among firefighters—the Firefighter Injury Risk Evaluation [FIRE] study”; EMW-2007-FP-02571) in the International Association of Fire Chief’s (IAFC) Missouri Valley Region (Colorado, Iowa, Kansas, Missouri, North Dakota, Nebraska, South Dakota, and Wyoming).
Fire departments in the IAFC Missouri Valley region were randomly selected using a one-stage randomized cluster sampling approach, stratified by department type (Volunteer/Mostly Volunteer vs. Career/Mostly Career). Departments were drawn from the US Fire Administration’s (USFA) Fire Department Census Database for each of the eight Missouri Valley States using a computerized random selection program. One additional volunteer department that was involved in piloting our measures also was included even though it was not randomly selected. Our participating career departments ranged in size from 1 to 18 stations, with a mix of settings ranging from urban inner city, suburban, and rural. Our volunteer departments were primarily in small to medium rural towns and cities and ranged from 1 to 3 stations.
Procedures
The protocol for the protection of human subjects for this study was approved by the NDRI Institutional Review Board. Among career departments, a total of 14 career departments were contacted with 2 declining participation because of competing priorities and 1 department not meeting inclusion criteria of at least 20 personnel.
Recruitment of departments
Based on the logistics and staffing patterns of volunteer departments, contacting a department’s administration was more difficult. Therefore, for each department selected, phone calls were made to the listed department number in the National Fire Department Census Database, as well as any number located through extensive internet searches. Phone calls were made during the day, in the evening and on a weekend day. If an address was provided, a letter also was sent to the station to the attention of the chief with a brief description of the study and a request for them to contact the research team. If no response was received within 2 weeks of attempted contact, a replacement department was selected. In addition to the challenges of contacting the volunteer personnel, the database did not always have current census numbers and, therefore, some departments were ruled out because of a low number of volunteer personnel. Thus, of 47 volunteer departments contacted, 13 were enrolled; 17 were unreachable; 8 did not meet the inclusion criteria of having at least 20 personnel; and 9 declined participation. In total, 11 career and 13 volunteer departments were enrolled and contributed data to this study.
Recruitment of firefighters
A core team of investigators traveled to each fire department for 2–5 days depending on the type of department (career vs. volunteer) and shift structure of career departments in order to solicit potential study participants from all available firefighters. In order to solicit participation from firefighters in selected departments, each data collection session included refreshments and/or participant incentives such as study t-shirts. Firefighters who agreed to participate in the study were provided an overview of the study, its specific aims, and the risks and benefits involved in study participation. They were then provided a survey to complete and moved through different assessment stations. Measures used in this article are described below.
For volunteer fire departments, we typically recruited participants during their regular monthly personnel meetings. The total number of volunteer firefighters across all departments included in this study is an estimated N = 385 and we enrolled 55.6% of potential participants. However, most volunteer fire chiefs indicated that their total list of firefighters was not an accurate representation of the number of firefighters they had who were “active” and engaged in the department. The number of engaged firefighters (e.g., who regularly attend monthly meetings) often is lower than the number listed in personal records. Thus, with volunteer departments it is difficult to know the number of active firefighters and, therefore, it is difficult to calculate a meaningful participation rate when based on the department personnel records. However, we enrolled 98.2% of the volunteers who attended the monthly meeting and were available for solicitation for participation in the study.
For career firefighters, there were approximately 929 career firefighters on the personnel files of the departments we visited and we consented 52.8% of them. Capturing the population of a fire department is particularly challenging given career firefighters work 24-hr shifts, often trade shifts, and some have “Kelly days” (i.e., a rotating day off). In some instances, we were unable to conduct scheduled data collection because crews were called out for extended periods of time and were not available during the days we traveled to their department. We attempted to capture at least 1 day for each shift but the population we captured varied a great deal by department. On average, our capture rate for the population of a department was 69% and was as high as 93.3% but our recruitment of career firefighters who were available during our visit was very high. Of all volunteer and career firefighters solicited, 97% agreed to participate in the research and provided signed informed consent.
Measures
Cigarette smoking status
Smoking status questions were modeled after national surveys such as the BRFSS [CDC, 2010b] and the Department of Defense Survey of Health Related Behaviors Among Active Duty Military Personnel [Department of Defense (DoD) Survey; Bray et al., 2009]. Three questions were used to determine smoking status: (1) Have you ever smoked a cigarette, even a puff?; (2) Have you smoked at least 100 cigarettes in your entire life?; and (3) Have you smoked a cigarette, even a puff, in the past 30 days? Participants who answered “no” to question 1 were defined as never smokers. Those who answered “yes” to question 1 but “no” to question 2 were designated as experimental smokers. Those who answered yes to questions 1 and 2 but “no” to 3 were defined as ex-smokers while participants who answered “yes” to all three questions were current smokers.
Verification of self-reported smoking status
Smoking status was validated through breath carbon monoxide (CO) testing using the Bedront Micro III Smokerlyzer (Bedfont, 2011). A CO ≥10 ppm was used to indicate possible false negatives. A total of 363 career and 155 volunteer firefighters were tested. There were no refusals for CO testing among study participants; however, it was not possible to calibrate the CO monitor in some departments due to high ambient CO levels. For career firefighters, the potential false negative rate was 1.3% while for volunteers it was 3.2%. Given the potential exposure of firefighters to CO while on the job (resulting in elevated CO in nonsmokers), this suggests that their self-reports of smoking were generally valid.
Cigar use
Cigar use was assessed with the item: “Have you smoked a cigar in the past 30 days?” Participants who answered yes to this item were asked how many days they smoked in the past 30 days and how many cigars they smoked on these days. The product of these two items was used to estimate level of use. Current users also were asked whether they smoked cigars while on duty.
Smokeless tobacco use
Using items similar to the assessment of cigarette and cigar use, participants were asked whether they had used chewing tobacco, snuff, or dip in the last 30 days and if yes, the amount (tins per week). Finally, smokeless users were asked to report their preferred brand.
Alcohol use
Items assessing alcohol use were modeled after common substance use questions in the civilian population on surveys such as the National Household Survey on Drug Abuse and on surveys of military members [Vander Weg, 2006]. Binge drinking was assessed with the item: “Considering all types of alcoholic beverages, how many times during the past 30 days did you have 5 drinks or more on an occasion (4 drinks for female firefighters)?” Driving while drinking was measured with the following item: “During the past 30 days, did you drive a car or other vehicle on any occasion when you perhaps had too much to drink?” Participants responded either “Yes” or “No.” Potential alcohol abuse was assessed with the CAGE questionnaire [O’Brien, 2008]. Participants were asked whether they (1) felt the need to cut down their drinking, (2) felt annoyed by criticism of their drinking, (3) had guilty feelings about drinking, and (4) had taken a morning eye opener. Each affirmative response contributes 1 point to an overall score of 0–4. Scores equal to or above 2 are considered indicating potential problem drinking [O’Brien, 2008].
General health assessment and likelihood of developing serious disease
Participants were asked to rate their current health with the item: “In general, would you say your health is:” Possible responses were “excellent,” “very good,” “good,” “fair,” and “poor.” Similar to studies of self-rated health in related occupations [Haddock et al., 2006], responses were categorized into “fair” or “good” versus the other responses to determine which firefighters rated their health relatively low. Likelihood of developing a serious disease was assessed with the item: “Compared to others your age, how likely do you believe it is that you will develop a serious disease, such as heart disease or cancer, in the future?” Participants responded on a 1–5 scale from “Not at all Likely” to “Very Likely.” To determine which firefighters believed they were at higher risk than average, those who responded either “Likely” or “Very Likely” were compared to other participants.
Depression
The Center for Epidemiological Studies Short Depression Scale (CES-D 10) was used to assess depression. The survey includes questions about the frequency of both feelings and behaviors during the past week. Response options included: rarely or none of the time (<1 day), some or a little of the time (1–2 days), occasionally or a moderate amount of time (3–4 days), all of the time (5–7 days). Total scores are then calculated by adding the points for each question. Those endorsing four or more items in the negative direction are considered to be in the range of concern for depression [Irwin et al., 1999] The CESD has been found to be highly reliable among the general population (Spearman–Brown, split halves r = 0.85) and in patient samples (r = 0.90; 74).
Previous diagnosis of anxiety or depressive disorder
Participants were asked to report whether they had ever been diagnosed with an anxiety or depressive disorder. History of anxiety was assessed with: “Has a doctor or other healthcare provider EVER told you that you had an anxiety disorder (including acute stress disorder, anxiety, generalized anxiety disorder, obsessive–compulsive disorder, panic disorder, phobia, posttraumatic stress disorder, or social anxiety disorder)? History of depressive disorder was determined with: “Has a doctor or other healthcare provider EVER told you that you have a depressive disorder (including depression, major depression, dysthymia, or minor depression)?”
The self-report of physical activity (SRPA) questionnaire, estimated maximal oxygen consumption (VO2max), and NFPA fitness standard
The SRPA questionnaire provides a global, self-rating of physical activity patterns. Indicators of the questionnaire’s validity in adult populations (significant correlation between SRPA ratings and measured maximal oxygen consumption) have been established [Jackson et al., 1990]. For our study, participants were instructed to select a value from the questionnaire that best described their physical activity pattern during the past 30 days [Jackson and Ross, 1997]. These values, along with BMI, age, and gender were used to estimate VO2max. This method has been tested by comparing it to measured VO2max and has demonstrated equal, if not better accuracy than methods using submaximal exercise heart rate to estimate aerobic capacity [Jackson et al., 1990, 1995, 1996; Jackson and Ross, 1997; Jurca et al., 2005; Wier et al., 2006], making it an ideal field measure. Aerobic capacity sufficient to exceed the National Fire Protection Association (NFPA) fitness standard was judged by comparing the estimated VO2max with the suggested cutpoint of ≥12 METS (VO2max ≥ 42 ml/kg/min) [NFPA, 2006; Donovan et al., 2009]. Estimated VO2max levels were converted to METS using the standard conversion of dividing VO2max by 3.5 ml/kg/min.
Statistical Analyses
Prevalence rates were computed for cigarette smoking status, cigar use, and smokeless tobacco use stratified by career versus volunteer firefighters. Women were excluded from analyses given their small numbers (n = 21 for career; n = 15 for volunteers). Comparisons are often made between the fire service and the military, as the fire service operates under a paramilitary structure, shares several traditions with the military, and has a relatively high rate of former military members among its ranks [USFA, 2010]. Thus, rates for smoking and smokeless tobacco were compared to the most recent age-adjusted sample of military members [DoD Survey; Bray et al., 2009]. The methods used to measure tobacco use in the DoD Survey were nearly identical to the ones used in this study, enhancing the validity of the comparisons. There was not sufficient data to make comparisons on cigar use. Population estimates stratified by age from the DoD Survey [Bray et al., 2009] were used for the standard population and StatsDirect Statistical Software version 2.7.8 (StatsDirect Ltd, 2010) was used to compute the age-standardized rates in our sample using the direct method of standardization [Hennekens and Buring, 1987].
A host of previous studies, some conducted in similar occupation groups such as the military [e.g., Haddock et al., 1998, 2004, 2007; Lando et al., 1999], have found that smokers underestimate their health risks, are at risk for problems with mood, are less physically fit, and are more likely to have other health risks than nonsmokers. To explore potential differences in measures of these parameters among firefighters based on their cigarette use, descriptive statistics (means or proportions) were computed separately for the four smoking status categories. In addition, among career firefighters, SAS PROC MIXED (for continuous variables) or SAS PROC GLIMMIX (for discrete variables) was used to test these differences in statistical models. To account for the unique sampling strategy used in this study, the clustering effect of department was included as a random effect in each model. Models for volunteer firefighters were not conducted because of their lower sample size and the relatively low statistical power of models based on cluster designs [Murray, 1998].
RESULTS
A total of 677 male career and volunteer firefighters were enrolled into the cohort and completed a baseline health evaluation. Demographic characteristics of all enrolled firefighters (including women) are presented in Table I.
TABLE I.
Baseline Demographic and Tobacco Use of Career and Volunteer Firefighters in the FIRE Study
| Demographics | Career (N = 500) | Volunteer (N = 214) |
|---|---|---|
| Age (SD) | 38.0 (9.9) | 39.7 (12.0) |
| Gender (% male) | 95.6 | 93.0 |
| Race (% white) | 86.2 | 97.2 |
| Marital status (% married or living with partner) | 70.8 | 74.3 |
| Education (% at least some college or college graduate) | 82.8 | 77.1 |
| Years in the fire service (SD) | 13.8 (9.4) | 11.1 (10.2) |
| Rank (%) | ||
| Firefighter | 32.8 | 58.5 |
| Firefighter/paramedic | 17.7 | 7.1 |
| Driver/operator | 19.8 | 8.5 |
| Officer | 22.2 | 10.8 |
| Chief | 6.4 | 9.4 |
| Other | 1.0 | 5.7 |
SD, standard deviation.
Percentages may not add to100 due to rounding.
Cigarette Use
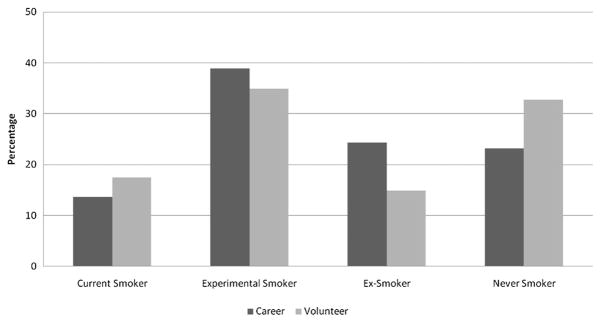
As can be seen in Figure 1, a relatively small percentage of firefighters were current cigarette users; unadjusted rates were 13.6% for career firefighters and 17.4% for volunteer firefighters. This compares to a national unadjusted prevalence rate of 23.4% for males [CDC, 2010a]. Age-standardized rates of current smoking for career (16.2%) and volunteer (16.2%) firefighters were substantially lower than the recently reported DoD prevalence of current smoking (30.5% unadjusted, 29.2% adjusted) among males. There were no significant differences among the smoking status categories on either age or years in the fire service for either the career or volunteer service. On average, career firefighters who smoked consumed 10.0 (SD = 9.03) cigarettes per day while volunteer smoked 15.2 (SD = 9.8) cigarettes per day. Over half of all career (54.1%) and volunteer (55.9%) firefighters who smoked had attempted to quit in the past year. Large percentages of both career (62.3%) and volunteer (70.6%) of fire-fighters who smoked reported that they planned to make another quit attempt in the next 6 months.
FIGURE 1.
Smoking status.
Table II presents descriptive statistics for differences in important health indices for the fire service among smoking status categories. Adjusted analyses demonstrated that there were significant differences between never and ex-smokers on meeting the NFPA fitness standard (odds ratio (OR) = 2.2, P < 0.01) and the number of binge drinking episodes (F = 7.3; P = 0.008) among career firefighters. Compared to never smokers, current smokers were nearly five times more likely to rate their health as fair or poor (OR = 4.9; P = 0.005), six times more likely to have been diagnosed with an anxiety disorder (OR = 5.8; P = 0.010), three times as likely to have a clinically significant CAGE alcohol problem score (OR = 2.9; P = 0.040), were over four times as likely to report driving while having too much alcohol to drink (OR = 4.5; P = 0.020), and reported significantly more binge drinking episodes (F = 21.1; P < 0.001). Although the rate of meeting the NFPA fitness standard was higher for never smokers (44.4%) compared to current smokers (31.8%) the test for this contrast was not statistically significant. Despite the fact that smoking is a powerful risk factor for both heart disease and cancer, current smokers did not rate themselves as having a significantly higher risk of heart disease or cancer compared to other firefighters.
TABLE II.
Unadjusted Associations Between Smoking Status and Health Beliefs and Practices
| Career firefighters
|
Volunteer firefighters
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Never | Experimental | Ex | Current | Never | Experimental | Ex | Current | |
| General healthfairor poor(%) | 4.5 | 6.5 | 7.0 | 18.5 | 9.9 | 9.5 | 0.3 | 16.7 |
| Likelyor very likely to developserious disease (%) | 15.7 | 16.1 | 18.0 | 19.0 | 16.9 | 17.6 | 20.7 | 13.9 |
| Meets NFPAfitness standard (%) | 44.4 | 44.6 | 31.3 | 31.8 | 25.4 | 20.3 | 29.6 | 16.7 |
| CESD10 ≥ 4 (%) | 13.1 | 13.3 | 14.5 | 18.2 | 11.8 | 19.2 | 25.0 | 26.5 |
| Depressive disorderdiagnosis (%) | 9.0 | 6.5 | 12.2 | 12.1 | 2.8 | 6.8 | 3.4 | 13.9 |
| Anxiety disorderdiagnosis (%) | 2.7 | 5.4 | 7.8 | 15.2 | 8.5 | 5.4 | 6.9 | 5.6 |
| CAGE ≥ 2 (%) | 6.4 | 12.2 | 10.7 | 16.7 | 5.6 | 8.5 | 13.8 | 11.4 |
| Drovewhen hadtoo muchto drink (%) | 3.7 | 7.7 | 7.9 | 16.9 | 2.8 | 8.2 | 10.3 | 14.3 |
| Numberof Binge drinkingepisodes past 30 days (mean (SD)) | 1.3 (2.7) | 2.8 (4.2) | 2.7 (3.9) | 4.2 (4.6) | 3.3 (6.8) | 2.8 (5.0) | 2.4 (3.0) | 4.8 (7.6) |
Figure 2 presents cigar use among firefighters and the percent of current users who smoke cigars while on duty. Current cigar use was higher among career (12.1%) compared to volunteer firefighters (3.7%). This compares to a national unadjusted prevalence rate of 9% for adult males [SAMSA, 2008]. Among current cigar smokers, about half (50.1%) of the career firefighters and approximately one-fourth (22.2%) of volunteers smoked while on duty. There were no significant differences between those who reported smoking cigars and nonusers on either age or years in the fire service for either the career or volunteer service. The mean number of cigars smoked per day in the past 30 days was 11.6 (SD = 27.7) career and 17.7 (SD = 32.5) for volunteer firefighters. However, a large group of cigar smokers among both groups (60.7% for career; 55.5% for volunteer) had smoked only 1–2 cigars in the previous 30 days, suggesting occasional use. The range of consumption in the previous 30 days for other fire-fighters who smoked cigars was 3–150 cigars for career and 3–90 for volunteers.
FIGURE 2.
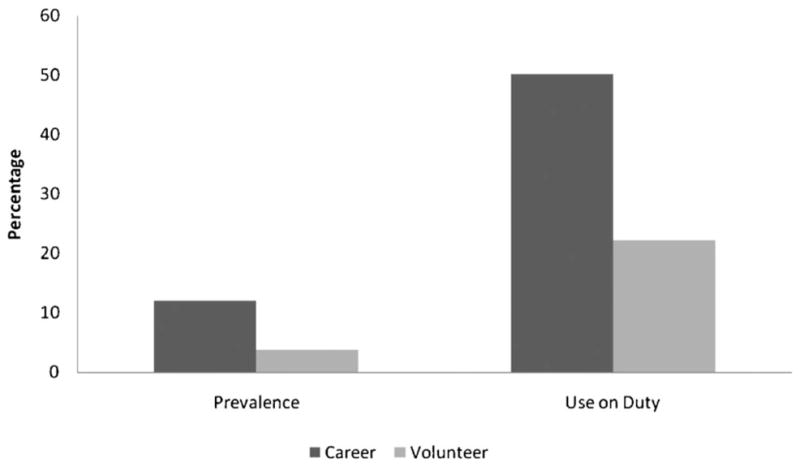
Cigar use prevalence and on-duty cigar smoking. Note: “Use on Duty” rates based on current users only.
Smokeless Tobacco
Rates of smokeless tobacco use and use on duty are presented in Figure 3. A surprisingly large percentage of career (18.4%) and volunteer (16.8%) firefighters were current users of smokeless tobacco. This compares to a national unadjusted use rate among adult males of 7.0% (CDC, 2011). Firefighters also demonstrated substantially higher rates of smokeless tobacco use when compared to males in the DoD overall and had rates comparable to the service with the highest rate of use, males in the US Marine Corps. For example, the age-standardized rate for career firefighters was 21.2% while the rate for all males in the DoD was 15.6% and for male Marines was 22.7% [Bray et al., 2009]. The volunteer age-standardize rate also were higher (20.8%) than the overall DoD prevalence for men and similar to that for males in the US Marine Corps.
FIGURE 3.
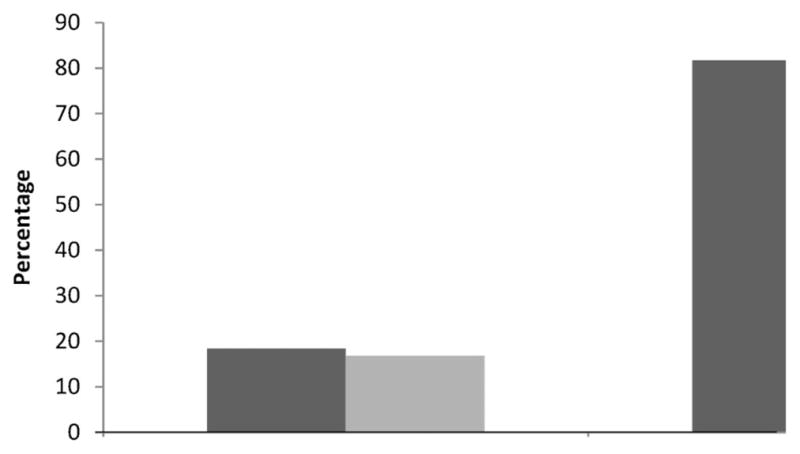
Prevalence of smokeless tobacco use and percent of current users who use on duty. Note: “On-duty” use rates based on current users only.
Smokeless users were slightly younger (35.1 years vs. 39.2 years; P = 0.001 for career and 35.2 vs. 41.2; P = 0.009 for volunteers) and among career firefighters had fewer years in the fire service (11.1 years vs. 14.6 years; P = 0.001) than other firefighters. Level of use was 2.8 (SD = 3.5) tins per week for career and 2.9 (SD = 3.6) tins per week for volunteer firefighters. A small percentage (15.7%) of career firefighters who used smokeless tobacco reported doing so because of restrictions on smoking in their department.
Polyuse
Among career firefighters who were current cigarette smokers, 30.5% also used smokeless tobacco while 22.0% also were current cigar users. There were fewer polyusers among volunteer firefighters. Among volunteers who smoked cigarettes, 17.3% also used chew while only 3.0% were current cigar users.
DISCUSSION
This study is the first systematic epidemiological study of the prevalence of different forms of tobacco use and factors associated with its use in the fire service and the first to biochemically verify smoking status. The prevalence of cigarette smoking among firefighters was relatively low compared to the general public and to the DoD and lower than historical rates suggested by studies that included firefighters [Dibbs et al., 1982; Large et al., 1990; Glueck et al., 1996; Lee et al., 2004; CDC, 2010b]. For instance, in the seven states covered by this study the rates of current cigarette use among adult males ranges from 16.9% in South Dakota to 24.3% in Missouri [CDC, 2010b]. In addition, the low rates of smoking found in our population-based cohort are consistent with the rate (10%) reported by Kales et al. [2003] in their control sample of active firefighters from Massachusetts who participated in their study of risk factors for coronary heart disease. A high proportion of current smokers had made a quit attempt in the previous year and were planning another quit attempt in the near future. Thus, smokers in the fire service appear to be motivated to quit. Given that smoking is not normative, the emphasis on being tobacco free in the fire service, and self-reports of quit attempts and plans to quit, firefighters appear to be an ideal population for smoking cessation efforts.
As in other, similar occupational groups, smoking was a marker for important health and safety risk factors [Haddock et al., 1998, 2004, 2007; Lando et al., 1999]. Statistical models conducted with career firefighters suggested that smokers had significantly more problems with mood and alcohol compared to never smokers and some of those differences were strikingly large. For instance, current smokers were nearly six times as like to have been diagnosed with an anxiety disorder and four and one-half times as likely to report driving while intoxicated. Also consistent with previous literature, there were fewer significant differences between never and ex-smokers on health and safety factors. This pattern of results was consistent with descriptive data from volunteer firefighters. Fortunately, smokers who quit experience numerous health benefits and often make positive changes in other health parameters [NCI, 2010].
Prevalence of cigar use among career firefighters was slightly higher than national prevalence rates. In contrast, volunteer firefighters had relatively low rate of cigar use. Even among those who reported smoking a cigar in the past 30 days, consumption was low; typically one or two cigars in the past 30 days. It is possible that, because many cigar smokers reported smoking on duty, these infrequent users only smoked socially with their crews. A small number of firefighters in both career and volunteer departments had higher consumption, up to the equivalent of five cigars per day. Given that heavy cigar use has been linked to both coronary heart disease and respiratory disease [NCI, 1998; ACS, 2009], efforts to encourage cigarette smokers to quit should extend to cigar smokers.
We found high rates of smokeless tobacco use compared to national norms. In fact, the prevalence rate for males in the career fire service was almost three times that found in national surveys of men and was higher than prevalence rates from states represented in this study [i.e., current rates range from 7.2% in Colorado to 11.9% in South Dakota, CDC, 2010b]. Smokeless tobacco contains at least 28 carcinogens and is a known cause of human cancer [NCI, 1992; WHO, 1998, 2007]. Thus, the high prevalence of smokeless use among firefighters should be addressed by both researchers and fire service organizations. In particular, researchers should examine the potential role of targeting of the fire service by tobacco companies. A large number of studies have demonstrated how the tobacco industry marketed products to military members and attempted to influence tobacco policy in the U.S. DoD [Smith et al., 2007; Arvey and Malone, 2008; Smith and Malone, 2009a,b]. It is possible that that the high rates of smokeless tobacco use in the fire service may be partially due to target marketing by industry. For example, since 2002 the U.S. Smokeless Tobacco Company has donated utility vehicles to fire departments as part of Operation Polaris Ranger and advertisements for Copenhagen have featured firefighters engaged in emergency operations [Adiocracy, 2010; FDNN, 2010]. Also, it is possible that occupational factors, such as prohibitions against cigarette smoking in fire houses, leads to smokeless tobacco use which, in turn, maintains nicotine addiction. Research into social and industry influences on smokeless tobacco use in the fire service is needed.
A significant percentage of cigarette smokers also were found to use other forms of tobacco. Polyusers, or those who use multiple forms of tobacco, have been found to be at particularly high health risk compared to other tobacco users [Lando et al., 1999; Rigotti et al., 2000]. For instance, Lando et al. [1999] compared polyusers (combined cigarette and smokeless use) with other tobacco users in a military population. Military members who were polyusers reported higher risk-taking, the least frequent seat belt use, the highest use of alcohol and binge drinking, and had a poorer quality diet than those who either smoked or chewed. Thus, firefighters who use multiple form of tobacco are in particular need of research on best methods to encourage cessation and deliver treatment.
In summary, despite strong statements against smoking by the fire service and the need to maintain high levels of health and fitness, a significant proportion of firefighters continue to use tobacco. This study was conducted in only one of the IAFC’s regions, therefore, it is unknown whether rates of tobacco use will differ in other regions given this was the first surveillance study of its kind. Thus, future studies should examine tobacco use in other IAFC regions to determine whether the findings of this study generalize to firefighters nationally. Future research also should examine social and industry factors which support tobacco use and test occupationally tailored interventions to help firefighters to successfully quit.
Acknowledgments
Contract grant sponsor: Federal Emergency Management Agency in the Department of Homeland Security; Contract grant number: EMW-2007-FP-02571.
This study was funded by a grant from the Assistance to Firefighters Grants program managed by the Federal Emergency Management Agency in the Department of Homeland Security (“A prospective evaluation of health behavior risk for injury among firefighters—the Firefighter Injury Risk Evaluation [FIRE] study”; EMW-2007-FP-02571). We would like to thank the departments that participated in this study.
References
- Adiocracy. [Accessed December 1, 2010];Smokeless tobacco features firemen engulfed in smoke. 2010 URL: http://www.adiocracy.com/2009/05/13/smokeless-tobacco-features-firemen-engulfed-in-smoke/
- American Cancer Society. Prevention and early detection: Cigar smoking. Atlanta: ACS; 2009. [Accessed December 1, 2010]. URL: http://www.cancer.org/Cancer/CancerCauses/TobaccoCancer/CigarSmoking/index. [Google Scholar]
- Arvey SR, Malone RE. Advance and retreat: Tobacco control policy in the U.S. military. Mil Med. 2008;173:985–991. doi: 10.7205/milmed.173.10.985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray RM, Pemberton MR, Hourani LL, Witt M, Rae-Olmsted KL, Brown JM, Weimer B, Lane ME, Marsden ME, Scheffler S, Vandermaas-Peeler R, Aspinwall KR, Anderson E, Spagnola K, Close K, Gratton JL, Calvin S, Bradshaw M. 2008 Department of Defense Survey of Health Related Behaviors among Active Military Personnel: A Component of the Defense Lifestyle Assessment Program. Research Triangle Park, NC: RTI International; 2009. [Google Scholar]
- Bedfont. [Accessed May 16, 2011];Smokerlyzer: Breath Carbon Monoxide (CO) Monitor. 2011 http://www.bedfont.com/smokerlyzer.
- Centers for Disease Control and Prevention. State-specific prevalence of cigarette smoking and smokeless tobacco use among adults—United States, 2009. Morb Mortal Wkly Rep. 2010a;59:1400–1406. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. [Accessed November 23, 2010];Behavioral Risk Factor Surveillance System Questionnaire. 2010b URL: http://www.cdc.gov/brfss/questionnaires/pdf-ques/2010brfss.pdf.
- Centers for Disease Control and Prevention. [Accessed May 16, 2011];Smokeless Tobacco Facts. 2011 URL: http://www.cdc.gov/tobacco/data_statistics/fact_sheets/smokeless/smokeless_facts/index.htm.
- Dibbs E, Thomas HE, Weiss ST, Sparrow D. Fire fighting and cornary artery disease. Circulation. 1982;65:943–946. doi: 10.1161/01.cir.65.5.943. [DOI] [PubMed] [Google Scholar]
- Donovan R, Nelson T, Peel J, Lipsey T, Voyles W, Israel RG. Cardiorespiratory fitness and the metabolic syndrome in firefighters. Occup Med (Lond) 2009;59:487–492. doi: 10.1093/occmed/kqp095. [DOI] [PubMed] [Google Scholar]
- Everyone Goes Home. [Accessed December 1, 2010];Second of four key areas: Firefighter heart disease and cancer education and prevention. 2009 URL: www.everyonegoeshome.com/news/2009/safetyweek_2.html.
- Fire Department News Network. [Accessed December 1, 2010];Operation Ranger Provides First Response Organizations in Need with Polaris Ranger 6x6 Utility Vehicles. 2010 URL: http://www.fdnntv.com/news.asp_Q_articleID_E_4927_A_title_E_Operation_Ranger_Provides_First_Response_Organizations_in_Need_with_Polaris_Ranger_6x6_Utility_Vehicles.
- Glueck CJ, Kelley W, Wang P, Gartside PS, Black D, Tracy T. Risk factors for coronary heart disease among firefighters in Cincinnati. Am J Ind Med. 1996;30:331–340. doi: 10.1002/ajim.4700300313. [DOI] [PubMed] [Google Scholar]
- Haddock CK, Klesges RC, Talcott GW, Stein RJ, Lando H. Smoking prevalence and risk factors for smoking in a population of United States Air Force basic trainees. Tob Control. 1998;7:232–235. doi: 10.1136/tc.7.3.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddock CK, Lando H, Klesges RC, Peterson AL, Scarinci IC. Modified tobacco use and lifestyle change in risk reducing beliefs about smoking. Am J Prev Med. 2004;27:35–41. doi: 10.1016/j.amepre.2004.03.010. [DOI] [PubMed] [Google Scholar]
- Haddock CK, Poston WSC, Pyle SA, Klesges RC, VanderWeg M, Peterson A, Debon M. The validity of self-rated health as a measure of health status among young military personnel: Evidence from a cross-sectional survey. Health Qual Life Outcomes. 2006;4:57. doi: 10.1186/1477-7525-4-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddock CK, Pyle SA, Poston WSC, Bray R, Stein RJ. Smoking and body weight as markers of fitness for duty among U.S. Military personnel. Mil Med. 2007;172:527–532. doi: 10.7205/milmed.172.5.527. [DOI] [PubMed] [Google Scholar]
- Hennekens CH, Buring JE. Epidemiology in medicine. Philadelphia, PA: Lippincott Williams & Wilkins; 1987. [Google Scholar]
- International Association of Fire Fighters (IAFF) [Accessed December 1, 2010];Campaign for a Smoke-Free Union. 2010 URL: http://www.iaff.org/smokefree/
- Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult. Criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D) Arch Intern Med. 1999;159:1701–1704. doi: 10.1001/archinte.159.15.1701. [DOI] [PubMed] [Google Scholar]
- Jackson A, Beard E, Wier L, Ross R, Stuteville J, Blair S. Changes in aerobic power of men ages 25–70 years. Med Sci Sports Exerc. 1995;27:113–120. [PubMed] [Google Scholar]
- Jackson A, Blair SN, Mahar MT, Wier L, Ross RM, Stuteville JE. Prediction of functional aerobic capacity without exercise testing. Med Sci Sports Exerc. 1990;22:863–870. doi: 10.1249/00005768-199012000-00021. [DOI] [PubMed] [Google Scholar]
- Jackson A, Ross RM. Understanding exercise for health and fitness. 3. Dubuque, IA: Kendall/Hunt; 1997. [Google Scholar]
- Jackson A, Wier L, Ayers G, Beard E, Stuteville J, Blaire S. Changes in aerobic power of women, ages 20–64 yr. Med Sci Sports Exerc. 1996;28:884–891. doi: 10.1097/00005768-199607000-00016. [DOI] [PubMed] [Google Scholar]
- Jurca R, Jackson AS, LaMonte MJ, et al. Assessing cardiorespiratory fitness without performing exercise testing. Am J Prev Med. 2005;29:185–193. doi: 10.1016/j.amepre.2005.06.004. [DOI] [PubMed] [Google Scholar]
- Kales SN, Soteriades ES, Christoudias SG, Christiani DC. Firefighters and on-duty deaths from coronary heart disease: A case control study. Environ Health. 2003;2:14. doi: 10.1186/1476-069X-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lando H, Haddock CK, Klesges RC, Talcott GW. Smokeless tobacco use in a population of young adults. Addict Behav. 1999;24:431–437. doi: 10.1016/s0306-4603(98)00058-6. [DOI] [PubMed] [Google Scholar]
- Large AA, Owens GR, Hoffman LA. The short-term effects of smoke exposure on the pulmonary function of firefighters. Chest. 1990;97:806–809. doi: 10.1378/chest.97.4.806. [DOI] [PubMed] [Google Scholar]
- Lee DJ, LeBlanc W, Fleming LE, Gomez-Marin O, Pitman T. Trends in U.S. smoking rates in occupational groups: The National Health Interview Survey 1987–1994. J Occup Environ Med. 2004;46:538–548. doi: 10.1097/01.jom.0000128152.01896.ae. [DOI] [PubMed] [Google Scholar]
- Murray DM. Design and analysis of group-randomized trials. New York: Oxford University Press; 1998. [Google Scholar]
- Mustajbegovic J, Zuskin E, Schachter EN, Kern J, Vrcic-Keglevic M, Heimer S, Vitale K, Nada T. Respiratory function in active firefighters. Am J Ind Med. 2001;40:55–62. doi: 10.1002/ajim.1071. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute (NCI) Smoking and Tobacco Control Monograph No. 9. Bethesda, MD: National Institutes of Health, NCI; 1998. [Accessed December 1, 2010]. Cigars: Health Effects and Trends. URL: http://cancercontrol.cancer.gov/tcrb/monographs/9/index.html. [Google Scholar]
- National Cancer Institute (NCI) Smokeless Tobacco or Health: An International Perspective. Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health, NCI; 1992. [Accessed December 1, 2010]. URL: http://cancercontrol.cancer.gov/tcrb/monographs/2/index.html. [Google Scholar]
- National Cancer Institute (NCI) Harms of smoking and health benefits of quitting. Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health, NCI; 2010. [Accessed December 2, 2010]. URL: www.cancer.gov/cancerrtopics/factsheet/tobacco/cessation. [Google Scholar]
- National Fire Protection Association. NFPA 1582, Standards on comprehensive occupational medicine programs for fire departments. Quincy, MA: NFPA; 2006. [Google Scholar]
- US Fire Administration. Women’s History Month: Women in USFA. USFA; Emmitsburg, MD: 2010. [Accessed September 14, 2010]. URL: http://www.usfa.dhs.gov/media/press/2010releases/030510_mc.shtm. [Google Scholar]
- National Fire Protection Association. [Accessed December 1, 2010];Fire-safe cigarettes: The time has come. 2005 URL: www.nfpa.org/publicColumn.asp?categoryID=&itemID=25640&src=NFPAJournal.
- National Institute for Occupational Safety and Health. [Accessed March 30, 2011];Smoking prevalence by industry and occupation. 2008 URL: http://www2.cdc.gov/drds/worldreportdata/SectionDetails.asp?ArchiveID=1&SectionTitleID=17.
- O’Brien CP. The CAGE Questionnaire for detection of alcoholism: A remarkably useful but simple tool. JAMA. 2008;300:2054–2056. doi: 10.1001/jama.2008.570. [DOI] [PubMed] [Google Scholar]
- WFI. [Accessed December 1, 2010];The Fire Service Joint Labor Management Wellness Fitness Initiative. 2008 URL: http://www.iaff.org/hs/wfiresource/default.html.
- Vander Weg MW, DeBon M, Sherrill-Mittleman D, Klesges RC, Relyea GE. Binge drinking, drinking and driving, and riding with a driver who has been drinking heavily among Air National Guard and Air Force Reserve Personnel. Mil Med. 2006;171:177–183. doi: 10.7205/milmed.171.2.177. [DOI] [PubMed] [Google Scholar]
- Wier L, Jackson AS, Ayers GW, Arenare B. Nonexercise models for estimating VO2 max with waist girth, percent fat, or BMI. Med Sci Sports Exerc. 2006;38:555–561. doi: 10.1249/01.mss.0000193561.64152. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMSA) [Accessed December 1, 2010];National Survey on Drug Use and Health. 2008 URL: http://www.oas.samhsa.gov/NSDUH/2K8NSDUH/tabs/Sect2peTabs32to36.pdf. [PubMed]
- World Health Organization (WHO) Summaries and Evaluations: Tobacco Products, Smokeless (Group 1) Lyon, France: WHO, International Agency for Research on Cancer; 1998. [Accessed December 1, 2010]. URL: http://www.inchem.org/documents/iarc/suppl7/tobaccosmokeless.html. [Google Scholar]
- Rigotti NA, Lee JE, Wechsler H. US college students’ use of tobacco products: Results of a national survey. JAMA. 2000;284(6):699–705. doi: 10.1001/jama.284.6.699. [DOI] [PubMed] [Google Scholar]
- Smith EA, Blackman V, Malone RE. Death at a discount: How the tobacco industry thwarted tobacco control policies in U.S. military commissaries. Tob Control. 2007;16:38–46. doi: 10.1136/tc.2006.017350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith EA, Malone RE. “Everywhere the soldier will be”: Wartime tobacco promotion in the U.S military. Am J Public Health. 2009a;99:1595–1602. doi: 10.2105/AJPH.2008.152983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith EA, Malone RE. Tobacco promotion to military personnel: “The plums are here to be plucked”. Mil Med. 2009b;174(8):797–806. doi: 10.7205/milmed-d-04-4108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) International Agency for Research on Cancer Monographs on the Evaluation of Carcinogenic Risks to Humans. Vol. 89. Lyon, France: WHO; 2007. [Accessed December 1, 2010]. Smokeless tobacco and some tobacco-specific N-nitrosamines. URL: http://mono-graphs.iarc.fr/ENG/Monographs/vol89/mono89.pdf. [Google Scholar]
- Yoo HL, Franke WD. Prevalence of cardiovascular disease risk factors in volunteer firefighters. J Occup Environ Med. 2009;51:958–962. doi: 10.1097/JOM.0b013e3181af3a58. [DOI] [PubMed] [Google Scholar]