Abstract
Background
Physical symptoms and depression in heart failure (HF) are key drivers of health-related quality of life (HRQOL). Heart failure self-care behaviors are believed to influence how symptoms affect HRQOL.
Objective
Determine if HF self-care behaviors moderate the relationships between physical and depressive symptoms and HRQOL.
Methods
In a cohort of adults with moderate to advanced HF, multivariate linear regression was used to evaluate the interaction between self-care behaviors (Self-Care of HF Index maintenance and management scales) and physical HF symptoms (HF Somatic Perception Scale) on emotional HRQOL (emotional dimension of Minnesota Living with HF Questionnaire). The interaction between self-care behaviors and depression (9-item Patient Health Questionnaire) was evaluated on physical HRQOL (physical dimension of Minnesota Living with HF Questionnaire).
Results
The mean age of the sample (n=202) was 57±13 years, 50% were women, and 61% had NYHA class III/IV HF. Controlling for age, Seattle HF Score, functional ability and co-morbidities, self-care maintenance and management moderated the relationship between physical HF symptoms and emotional HRQOL. Only self-care maintenance moderated the relationship between depression and physical HRQOL.
Conclusions
In HF, HRQOL is dependent upon both the severity of physical and depressive symptoms and the level of engagement in HF self-care behaviors. Future research should consider both self-care behaviors and symptoms when examining patient HRQOL.
Keywords: Heart failure, Symptoms, Self-care, Health-related quality of life
Introduction/Background
Heart failure (HF) is a prevalent cardiovascular syndrome characterized by distressing symptoms and high mortality.1–3 The clinical hallmark of dyspnea is the most frequent physical symptom of HF4 and is the primary reason for HF hospitalization.5 Depression is also common in patients with HF, contributing significantly to increased mortality and poor health-related quality of life (HRQOL).6 Understanding how physical symptoms and depression influence patient outcomes is a priority for clinicians since these HF symptoms predict mortality and are the primary drivers of HRQOL.7–10 A modifiable factor that may influence the strength and direction of the relationship between symptoms and HRQOL is HF self-care.11,12 Self-care in HF entails adherence behaviors to prevent and monitor symptoms (i.e. maintenance) and behaviors to recognize and self-treat symptoms (i.e. management).12 The Situation-specific Theory of HF Self-care proposes physical and emotional symptoms influence self-care and that moderate-to-high levels of self-care are needed to influence outcomes.12 Additionally, a number of studies have shown physical and depressive symptoms to be associated with HRQOL in HF,3,13,14 and HF self-care behaviors have been shown to be positively associated with HRQOL.15,16 In these studies, however, HF symptoms and self-care were examined as independent predictors of HRQOL. But, symptoms and self-care in HF are likely not independent. For example, fewer episodes of pulmonary congestion, a common reason for dyspnea in HF, are associated better HF self-care,17 and higher levels of self-care have been associated with lower odds of having elevated HF biomarkers suggesting that engagement in self-care may influence HF progression resulting in fewer symptoms and better HRQOL.18,19 No studies to date, however, have examined how HRQOL is a function of symptoms, HF self-care, and the interaction between the two. This is a significant gap in our knowledge of HF symptomology and self-care since a primary goal of interventions focused on HF self-care is to mitigate the frequency and/or severity of HF symptoms leading to improved HRQOL. A more complete understanding of how HF self-care behaviors (i.e. maintenance and management) and physical HF symptoms and depression interact to influence HRQOL will provide much needed information to develop tailored interventions to reduced symptom burden and improve patient quality of life. The goal of this study was to determine if HF self-care behaviors alter the strength and/or direction of the relationship between symptoms and HRQOL.
Method
Procedure
A secondary analysis was completed on data collected between 2010 and 2013 during a prospective cross-sectional study examining gender differences in symptoms in adults with moderate to advanced HF. The study was conducted at an advanced HF clinic associated with an academic medical center in Pacific Northwest, United States.20 By design, data were collected on 101 men and 101 women with NYHA class II-IV HF. Additional inclusion criteria included age 21 years or older, willingness to provide informed consent, ability to read at least 5th grade English and receiving optimized HF treatment by a cardiologist. Exclusion criteria included a diagnosis of a major cognitive disorder (e.g. Alzheimer’s disease), having received a heart transplant or ventricular-assist device or being unable to complete study requirements. Written and informed consent was obtained from all participants and the study was approved by our institutional review board.
Measurement
A questionnaire was used to obtain participant’s sociodemographic and clinical data including age, gender, marital/partnership status, race/ethnicity, employment, and adequacy of financial resources. Comorbid conditions were evaluated with the Charlson Comorbidity Index.21 Clinical and treatment characteristic were collected through an in-depth review of the electronic health record. The Seattle HF Model Score was calculated using data collected from the patient electronic medical record at the time of enrollment. The calculation for the Seattle HF Score was derived from the model developed by Levy et al.22 The model includes demographic (i.e. age-per decade, gender), clinical factors related to HF (i.e. HF etiology, New York Heart Association functional class, systolic blood pressure, left ventricular ejection fraction, hemoglobin, lymphocyte percent, uric acid, total cholesterol, and sodium) and HF treatment (β-blockers, angiotensin converting enzyme inhibitors, allopurinol, diuretic dose, statin use, and device therapy). A composite of the model factors creates a mortality risk-prediction score from −0.16 to 3.85 in this sample, with higher scores indicating greater mortality risk. Self-reported functional ability was assessed using the Duke Activity Status Index (DASI).23
Physical symptoms
Physical HF symptoms were measured with the 18-item HF Somatic Perception Scale (HFSPS).24 The HFSPS asks about the presence of HF symptoms and how much the participant was bothered by those symptoms during the last week and provides six response options ranging from 0 (not at all) to 5 (extremely bothersome). The HFSPS has excellent internal consistency (alpha = 0.90) with higher scores on the HFSPS indicating more physical symptom burden.24
Depressive symptoms
Depression was measured using the 9-item Patient Health Questionnaire (PHQ9). The PHQ9 provides 4 response options 0 (not at all) to 3 (nearly every day) based on the Diagnostic and Statistical Manual, 4th Edition.25 Scores range from 0 – 27 with higher scores indicating more depression. The PHQ9 is sensitive and specific for detecting major depression with excellent internal consistency (alpha = 0.86 – 0.89).26 Scores on the PHQ9 indicate mild, moderate, moderately severe and severe depression with values of 5, 10, 15 and 20, respectively.26
Self-care Behaviors
Heart failure self-care behaviors were measured with the Self-Care of HF Index (SCHFI v.6) self-care maintenance and self-care management scales; responses are standardized scores (0–100; higher values indicate better self-care).27 The 10 items of the self-care maintenance scale use a 4-point scale with sufficient internal consistency (global reliability index = 0.82 and model-based internal consistency coefficient = 0.83).28 The SCHFI self-care management scale is comprised of 6 items with 4 to 5 response options.27 The SCHFI management score has sufficient internal consistency (global reliability index = 0.77 and model-based internal consistency coefficient = 0.76).28 The SCHFI scores of 70 or greater are considered adequate self-care.12
Health-related Quality of Life
Heart failure-specific HRQOL was measured using the Minnesota Living with HF Questionnaire (MLHFQ), a 21 item scale that quantifies the physical (8 items), emotional (5 items), and social (8 items) impact of HF and treatment on patients’ lives. Items are rated on a 6 point scale ranging from 0 (no effect) to 5 (very much).29 The MLHFQ has been shown to be a valid and reliable instrument and has been used extensively to assess disease-specific HRQOL in HF research.29–31 The score for the MLHFQ physical dimension and the MLHFQ emotional dimension can range from 0 – 40 and 0 – 25 respectively, with a higher score indicating worse HRQOL. A total MLHFQ score > 45 represents poor HF-specific HRQOL and a score < 24 denotes good HRQOL.32
Analysis
Means, standard deviations, frequency, and percentages were used to describe the sample using Stata/IC v14.2. Multivariate linear regression was used to model whether HF self-care moderates the relationship between physical symptoms and HRQOL (Figure 1). The emotional dimension of the MLHFQ (dependent variable) score was regressed on the physical symptom measure (HFSPS), one self-care behavior (management or maintenance) and an interaction term combining physical symptoms and the specified self-care behavior. Using hierarchical regression, change in R2 and F-values were examined between models with and without the interaction term of physical symptoms and self-care behaviors. The same method was used to assess the moderation of self-care behaviors on the relationship between depression (PHQ9) and physical HRQOL (physical dimension of the MLHFQ). The purpose of selecting an emotional HRQOL metric in association with physical symptoms, and selecting a physical HRQOL metric in association with depressive symptoms was to avoid inherent measurement overlap. To account for the effect of other factors associated with HF, each model was adjusted for the Seattle HF Model Score (gender, HF clinical and treatment variables). Analyses were also adjusted for additional covariates known to significantly influence HF-specific HRQOL in previous research, namely age, comorbidities and functional ability.33–35 Although age per decade is a factor in the Seattle HF model, the full distribution of patient age per year was used as a covariate in this analysis to more directly control for the potential confounding effects of age. Formal moderation testing was used with an a priori alpha of 0.05. The moderation of self-care on physical symptoms or depression and HRQOL was represented with 1) contour plots generated across the complete observed range of physical and depressive symptoms, self-care behaviors and HRQOL and 2) by plotting the predicted values of HRQOL by physical or depressive symptoms with and without the moderation of self-care behaviors.
Figure 1. Moderation Testing Analysis Plan.
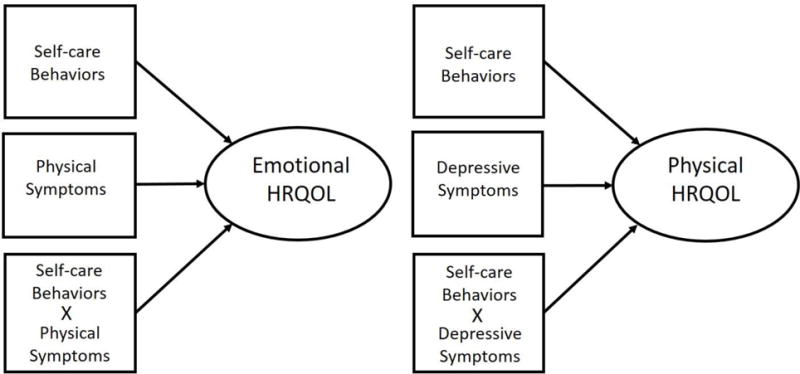
The analytic approach involves using hierarchical regression to examine whether the interaction of symptoms (physical and depressive) and self-care behaviors significantly influence HRQOL (emotional and physical) above and beyond the independent contributions of symptoms and self-care. Emotional HRQOL was regressed on physical symptoms, each self-care behavior (maintenance and management) and an interaction term combining physical symptoms and a self-care behavior. The same approach was used examine the influence of depression and self-care behaviors on physical HRQOL. The reason a metric of emotional HRQOL was analyzed in relation to physical symptoms and physical HRQOL in relation to emotional symptoms was to avoid inherent measurement overlap.
Abbreviations: HRQOL – health-related quality of life
Results
The mean age of the sample (n=202) was 57 years old, half were women, a majority (60%) of subjects had Class III–IV HF, and most (65%) had non-ischemic HF (Table 1). The average overall HRQOL was low.32 On average, self-care maintenance was adequate and self-care management inadequate using the common cut-point of 70 (Table 1).
Table 1.
Characteristics of the Sample (n= 202)
| mean ± SD or n (%) | |
|---|---|
| Age (in years) | 57 ± 13.3 |
| Female | 101 (50.0) |
| Self-Identified Race | |
| White | 173 (85.6) |
| Marital Status | |
| Married or living with partner | 129 (63.9) |
| Functional Ability (DASI) | 13.2 ± 12.8 |
| Charlson Co-morbidity Category | |
| Low (score of 1 or 2) | 124 (61.4) |
| Medium (score of 3 or 4) | 66 (32.6) |
| High (score of 5 or more) | 12 (6.0) |
| Heart Failure Characteristics: | |
| NYHAIII/IV | 122 (60.4) |
| EF % | 28.5 ± 12.5 |
| Primary Etiology | |
| Ischemic | 71 (35.3) |
| Seattle HF Score | 1.8 ± 0.7 |
| Systolic BP | 109.5 ± 17 |
| Aldosterone Agonist | 96 (47.5) |
| ACE/ARB | 162 (80.2) |
| Beta Blocker | 183 (90.6) |
| Hemoglobin | 12.81 ± 2.1 |
| Serum Sodium | 137.5 ± 3.3 |
| Symptoms: | |
| Physical | 24.6 ± 16.4 |
| Depressive | 7.02 ± 5.9 |
| Health-related Quality of Life: | |
| Total HRQOL Score | 46.9 ± 25.4 |
| Emotional Dimension | 10.1 ± 7.4 |
| Physical Dimension | 20 ± 11.2 |
| Self-care Behaviors: | |
| Self-care Management | 65.7 ± 19.9 |
| Self-care Maintenance | 70.2 ± 15.1 |
Abbreviations: ACE - angiotensin converting enzyme; ARB - angiotensin receptor blocker; BP - blood pressure; DASI - Duke Activity Status Index; EF - ejection fraction; HF - heart failure; HRQOL - health-related quality of life; NYHA - New York Heart Association
Better self-care maintenance and management were both independently associated with worse emotional HRQOL in adjusted models (Table 2). Worse physical symptoms were independently associated with worse emotional HRQOL (β = 0.409 ± 0.081, p < 0.001). Self-care maintenance and self-care management moderated the relationship between physical HF symptoms and emotional HRQOL (Table 2). As a key example, when symptoms are severe and self-care is high, HRQOL is better than when symptoms are high and self-care is low. (Figures 2A & 2C). Conversely, when physical symptom burden is low and self-care is high, HRQOL is worse than when symptom burden is low and self-care is low. The relationship between worse physical symptoms and worse emotional HRQOL was not constant across all levels of engagement with self-care (Figure 2B & 2D). That is, the better the self-care the less physical symptoms affect emotional HRQOL.
Table 2.
Multivariate models with interaction of HF self-care and physical symptoms on emotional HRQOL
| n= 201 | β ± Standard Error | t | p value |
|---|---|---|---|
| HFSPS | 0.409 ± 0.081 | 5.03 | <0.001 |
| SCMAIN | 0.130 ± 0.029 | 4.45 | <0.001 |
| HFSPS × SCMAIN | −0.003 ± 0.001 | −2.71 | 0.007 |
|
| |||
| n= 196 | |||
| HFSPS | 0.38 ± 0.08 | 5.02 | <0.001 |
| SCMGT | 0.07 ± 0.03 | 2.70 | 0.008 |
| HFSPS × SCMGT | −0.003 ± 0.001 | −2.37 | 0.019 |
For SCMAIN model: ΔR2 = 0.022, ΔF(1, 194) = 5.98, p < 0.001. For SCMGT model: ΔR2 = 0.015, ΔF(1, 189) = 3.82, p < 0.001. The main effects of physical symptoms and self-care as well as the interaction of self-care (maintenance and management) and physical symptoms were all significant at a p value < 0.05. In addition, a significant change in R2 was observed with the inclusion of the interaction term indicating self-care behaviors moderate the relationship between physical symptoms and emotional HRQOL. Each model was adjusted for age, Seattle HF Score, functional ability and co-morbidities. Albeit minimal, there was some marginal reduction in sample size due to missingness in model covariates.
Abbreviations: HF – heart failure; HFSPS - Heart Failure Somatic Perception Scale; HRQOL - health-related quality of life; SCMAIN- self-care maintenance; SCMGT- self-care management
Figure 2. Self-care as a Moderator of Physical Symptoms and Emotional HRQOL.
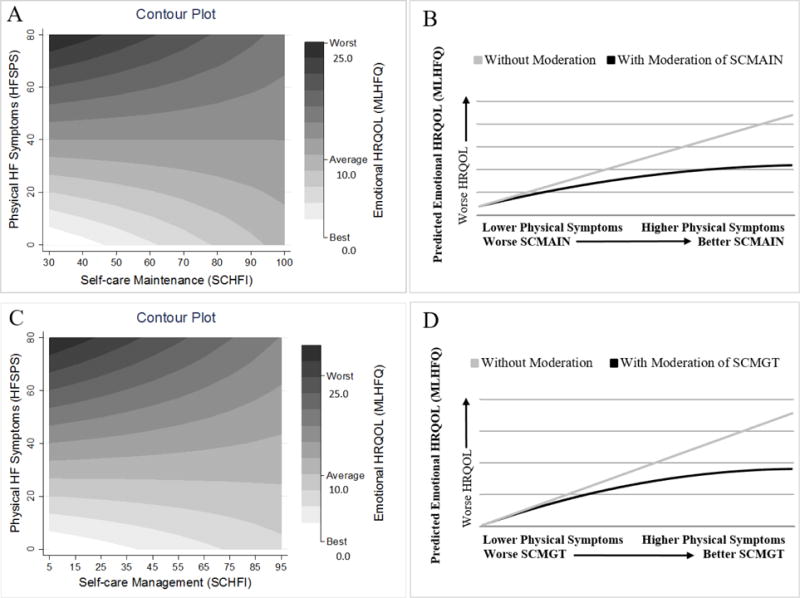
Plots A & C: The contour plots show that emotional HRQOL was dependent upon both the level of physical symptoms and self-care (maintenance and management) at all levels. For example, the best emotional HRQOL (white color) was reported when both symptoms and self-care are low, and the worst emotional HRQOL (black color) was reported when symptom were high but self-care was low. Plots B & D: Linear regression was used to estimate emotional HRQOL with and without the moderation of self-care (maintenance and management) on the relationship between physical symptoms and emotional HRQOL. The better the self-care, the less physical symptoms affect emotional HRQOL. Note: Plots B & D represent a simplified moderation for economy of presentation whereas Plots A & C represent the full complexity of moderation.
Abbreviations: HFSPS – Heart Failure Somatic Perceptions Scale; HRQOL – health-related quality of life; MLHFQ – Minnesota Living with Heart Failure Questionnaire; SCMAIN – self-care Maintenance; SCMGT – self-care Management.
Better self-care maintenance and management were independently associated with worse physical HRQOL in adjusted models (Table 3). In addition, more severe depression was independently associated with worse physical HRQOL (β = 1.64 ± 0.341, p < 0.001). Self-care maintenance but not self-care management significantly moderated the relationship between depression and physical HRQOL (Table 3). For example, worse physical HRQOL was associated with poor self-care maintenance and more severe depression (Figure 3A). In contrast, better physical HRQOL was observed when both depression and self-care maintenance were low. As seen with physical symptoms and emotional HRQOL, the relationship between depressive symptoms and physical HRQOL was not constant across all levels of self-care maintenance (Figure 3B). The better the self-care maintenance the less depressive symptoms affect physical HRQOL.
Table 3.
Multivariate models with interaction of HF self-care and depression on physical HRQOL
| n= 196 | β ± Standard Error | t | p value |
|---|---|---|---|
| PHQ9 | 1.64 ± 0.341 | 4.81 | <0.001 |
| SCMAIN | 0.20 ± 0.039 | 5.30 | <0.001 |
| PHQ9 × SCMAIN | −0.01 ± 0.005 | −2.14 | 0.034 |
|
| |||
| n= 191 | |||
| PHQ9 | 1.3 ± 0.237 | 5.49 | <0.001 |
| SCMGT | 0.20 ± 0.033 | 6.16 | <0.001 |
| PHQ9 × SCMGT | −0.006 ± 0.004 | −1.68 | 0.094 |
For SCMAIN model: ΔR2 = 0.009, ΔF(1, 189) = 2.87, p = 0.007; For SCMGT model: ΔR2 = 0.005, ΔF(1, 184) = 1.21, p = 0.11. The main effects of depression and self-care and the interaction of self-care maintenance but not self-care management and depression were significant at a p-value < 0.05. Additionally, a significant change in R2 was observed with the inclusion of the interaction term (PHQ9 × SCMAIN) indicating self-care maintenance moderates the relationship between depressive symptoms and physical HRQOL. Each model was adjusted for age, Seattle HF Score, functional ability and co-morbidities. Albeit minimal, there was some marginal reduction in sample size due to missingness in model covariates.
Abbreviations: HF – heart failure; HRQOL - health-related quality of life; PHQ9 - 9-item Patient Health Questionnaire; SCMAIN - self-care maintenance; SCMGT - self-care management
Figure 3. Self-care Maintenance as a Moderator of Depression and Physical HRQOL.
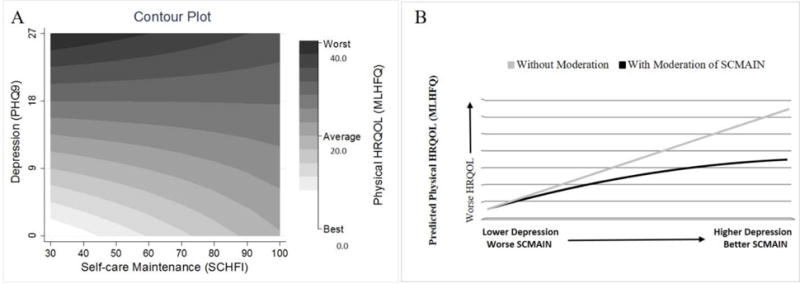
Plot A: The contour plot shows physical HRQOL as a function of both depression and self-care maintenance at all levels. The best physical HRQOL was reported when depression was low and self-care maintenance was low, and the worst physical HRQOL was reported when depression was high and self-care was low. Not surprisingly, when depression was high, more engagement in self-care maintenance had little association with better physical HRQOL. This suggests when depression is high, physical HRQOL is poor regardless of the level of self-care. Plot B: Linear regression was used to estimate physical HRQOL with and without the moderation of self-care maintenance on the relationship between depression and physical HRQOL. The better the self-care maintenance, the less depression affects physical HRQOL. Note: Plot B represents a simplified moderation for economy of presentation whereas Plot A depicts the full complexity of moderation.
Abbreviations: HRQOL - health-related quality of life; MLHFQ - Minnesota Living with Heart Failure Questionnaire; PHQ9 - 9-item Patient Health Questionnaire; SCMAIN – self-care maintenance.
Discussion
In this study of 101 women and 101 men with symptomatic HF, we observed that HRQOL is dependent upon both symptomatology and engagement in HF self-care. The worst HRQOL was reported when physical and depressive symptoms were severe and self-care was poor while, interestingly, the best HRQOL was associated with few symptoms and low levels of self-care engagement. Additionally, better emotional HRQOL was reported when both physical symptom and self-care behaviors were high. These findings provide new insights into the complex interaction among self-care behaviors, common HF symptoms and HRQOL.
Heo et al.2,13 and others3,14 have shown that more severe physical HF symptoms and depression are associated with worse HRQOL. The relationship between self-care behaviors and HRQOL is not clear. In a review of self-care interventions aimed at improving HRQOL in adults with HF, Grady31 reported a possible positive association between self-care and HRQOL. However, small sample sizes and heterogeneity in the study designs and measurement of HRQOL prevented unequivocal conclusions from the review. Additionally, Jonkman et al.,16 in a meta-analysis of 20 HF self-management studies, demonstrated self-management interventions had a small but positive effect on HRQOL. The relationship between self-care behaviors and the severity of physical symptoms and depression is also uncertain. Lee et al.36 and others37 have shown that worse physical HF symptoms or depression in relatively young HF patients were associated with better self-care suggesting HF symptoms are key drivers of self-care.38,39 Alternatively, Graven et al.40 found that among older adults worse physical HF symptoms were associated with lower levels of self-care and with no association between depression and HF self-care. In sum, the relationships between self-care behaviors and symptoms in influencing HRQOL in HF are inconclusive based on prior research. Although the effect sizes are relatively small (ΔR2 ~ 1–2%), the current study provides new information regarding these complicated relationships that enhances our understanding of how differences in self-care behaviors and symptoms affect HRQOL in patients with HF.
Our findings show that emotional HRQOL is influenced by both the engagement in self-care and the severity of physical symptoms. For example, more severe symptoms were associated with better emotional HRQOL when self-care maintenance and management were high compared to when self-care was low. One explanation for why patients with high levels of symptoms exhibit higher levels of self-care may be that worsening symptoms increase engagement with self-care.36,37 Another explanation for the interaction of self-care behaviors and symptoms on HRQOL may be patients with severe physical symptoms are receiving more frequent contact from family members or their healthcare team, who may provide additional teaching or feedback enhancing self-care behaviors and in turn improving emotional HRQOL.18
Contrasting our results of better HRQOL with severe physical symptoms and better self-care, we found low physical symptom burden was associated with worse emotional HRQOL when self-care was high compared to when self-care was low. This result is consistent with data reported by Peters-Klimm et al.41 who also found better self-care related to worse HRQOL in a community-dwelling sample with predominantly less severe symptoms (60% NHYA class I-II). The observation of worse emotional HRQOL in participants with better self-care who were experiencing a low level of physical symptom severity may suggest that some aspect of good self-care is influencing worse HRQOL in these patients. Perhaps excellent self-care in the setting of mild physical symptoms may be perceived by some patients as burdensome, influencing worse emotional HRQOL.12 Continued research, particularly of longitudinal design, is needed to elucidate the temporal relationships and other factors associated with self-care, physical symptom severity and emotional HRQOL.
Advancing the understanding of self-care, depression and physical HRQOL, our results indicate that self-care maintenance but not self-care management significantly influenced the association of depression on physical HRQOL. Our analysis demonstrated the worst physical HRQOL was observed with the highest levels of depression and poor self-care maintenance. This results is consistent with recent research by Graven et al.40 that demonstrated worse physical HF symptoms (similar to the physical dimension of the MLHFQ) were associated with more depression and poor adherence behaviors (self-care maintenance). Furthermore, our results demonstrated better self-care maintenance did not affect HRQOL at high levels of depression. Simply put, with severe depression poor quality of life is a given irrespective of the level of self-care maintenance. Additionally, we found that the best physical HRQOL was associated with low levels of depression and the poorest self-care maintenance. This finding supports research showing less depression is associated with better HRQOL13,14 and substantiates the idea that less severe symptoms are associated with lower levels of self-care. In other words, mild to absent depression may result in better physical HRQOL for patients with HF creating less motivation to engage in frequent self-care maintenance behaviors.
Our research has several strengths. First, the study sampled equal numbers of men and women; the original study was designed to address gender inequalities in sampling prevalent in the majority of HF literature. Second, our study examined both physical and emotional symptoms in HF providing a broader picture of HF symptomology. Third, the analysis was designed to mitigate the measurement overlap between the physical HF symptoms, depression and the MLHFQ. There are also important limitations that should be taken into consideration when interpreting the results. First, the cross-sectional design of the study prevents drawing conclusions about temporal or causal relationships. Future studies with longitudinal and/or experimental designs are needed to better understand how symptoms, self-care and quality of life are associated over time. Second, the sample was obtained from a clinic associated with a large academic medical center where patients tend to be younger, sicker, and more have HF of non-ischemic etiology that may limit the generalizability of our findings to all HF populations.
Conclusion
In our sample, HRQOL was dependent upon both the level of symptom burden and level of engagement in self-care such that the better the self-care the less physical symptoms and depression affect HRQOL. Furthermore, knowing that self-care behaviors influence the relationship between HF symptoms and HRQOL differently depending on the patient’s symptom severity may inform strategies to teach adherence and symptom monitoring skills that minimize negative impacts on HRQOL. The results of this study highlight the need to focus further research, patient education and clinical practice on both HF symptoms and HF self-care in order to optimize outcomes for patients.
Acknowledgments
This work was supported by the National Institute of Nursing Research (F31NR016660) and by the Office of Research on Women’s Health and the National Institute of Child Health and Human Development through the Oregon Building Interdisciplinary Research Careers in Women’s Health program (HD043488-08). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research, the Office of Research on Women's Health or the National Institute of Child Health and Human Development.
Contributor Information
Jonathan P. Auld, Oregon Health & Science University School of Nursing, Portland, OR.
James O. Mudd, Oregon Health & Science University, Knight Cardiovascular Institute, Portland, OR.
Jill M. Gelow, Oregon Health & Science University, Knight Cardiovascular Institute, Portland, OR.
Shirin O. Hiatt, Oregon Health & Science University School of Nursing, Portland, OR.
Christopher S. Lee, Oregon Health & Science University School of Nursing and Knight Cardiovascular Institute, Portland, OR.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Executive Summary: Heart Disease and Stroke Statistics–2015 Update: A Report From the American Heart Association. Circulation. 2015;131(4):434–441. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 2.Heo S, Moser DK, Lennie TA, Zambroski CH, Chung ML. A comparison of health-related quality of life between older adults with heart failure and healthy older adults. Heart & lung: the journal of critical care. 2007;36(1):16–24. doi: 10.1016/j.hrtlng.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 3.Zambroski CH, Moser DK, Bhat G, Ziegler C. Impact of symptom prevalence and symptom burden on quality of life in patients with heart failure. European Journal of Cardiovascular Nursing. 2005;4(3):198–206. doi: 10.1016/j.ejcnurse.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 4.Jurgens CY. Somatic Awareness, Uncertainty, and Delay in Care-Seeking in Acute Heart Failure. Research in nursing & health. 2006;29:74–86. doi: 10.1002/nur.20118. [DOI] [PubMed] [Google Scholar]
- 5.Kociol RD, McNulty SE, Hernandez AF, et al. Markers of decongestion, dyspnea relief, and clinical outcomes among patients hospitalized with acute heart failure. Circ Heart Fail. 2013;6(2):240–245. doi: 10.1161/CIRCHEARTFAILURE.112.969246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in Heart Failure. A Meta-Analytic Review of Prevalence, Intervention Effects, and Associations With Clinical Outcomes. Journal of the American College of Cardiology. 2006;48(8):1527–1537. doi: 10.1016/j.jacc.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 7.Nohria A, Tsang SW, Fang JC, et al. Clinical assessment identifies hemodynamic profiles that predict outcomes in patients admitted with heart failure. Journal of the American College of Cardiology. 2003;41(10):1797–1804. doi: 10.1016/s0735-1097(03)00309-7. [DOI] [PubMed] [Google Scholar]
- 8.Negi S, Sawano M, Kohsaka S, et al. Prognostic Implication of Physical Signs of Congestion in Acute Heart Failure Patients and Its Association with Steady-State Biomarker Levels. PLoS ONE. 2014;9(5):e96325–e96325. doi: 10.1371/journal.pone.0096325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Drazner MH, Hellkamp AS, Leier CV, et al. Value of Clinician Assessment of Hemodynamics in Advanced Heart Failure: The ESCAPE Trial. Circulation: Heart Failure. 2008;1(3):170–177. doi: 10.1161/CIRCHEARTFAILURE.108.769778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee CS, Moser DK, Lennie TA, Riegel B. Event-free survival in adults with heart failure who engage in self-care management. Heart & lung: the journal of critical care. 2011;40(1):12–20. doi: 10.1016/j.hrtlng.2009.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Riegel B, Lee CS, Dickson VV. Self care in patients with chronic heart failure. Nature reviews Cardiology. 2011;8(11):644–654. doi: 10.1038/nrcardio.2011.95. [DOI] [PubMed] [Google Scholar]
- 12.Riegel B, Dickson VV, Faulkner KM. The Situation-Specific Theory of Heart Failure Self-Care. The Journal of Cardiovascular Nursing. 2015;31(3):226–235. doi: 10.1097/JCN.0000000000000244. [DOI] [PubMed] [Google Scholar]
- 13.Heo S, Moser DK, Pressler SJ, et al. Dose-dependent relationship of physical and depressive symptoms with health-related quality of life in patients with heart failure. Eur J Cardiovasc Nurs. 2013;12(5):454–460. doi: 10.1177/1474515112470996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bekelman DB, Havranek EP, Becker DM, et al. Symptoms, Depression, and Quality of Life in Patients With Heart Failure. Journal of Cardiac Failure. 2007;13(8):643–648. doi: 10.1016/j.cardfail.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 15.Lee CS, Mudd JO, Hiatt SO, Gelow JM, Chien C, Riegel B. Trajectories of heart failure self-care management and changes in quality of life. Eur J Cardiovasc Nurs. 2014 doi: 10.1177/1474515114541730. [DOI] [PubMed] [Google Scholar]
- 16.Jonkman NH, Westland H, Groenwold RHH, et al. Do Self-Management Interventions Work in Patients With Heart Failure? An Individual Patient Data Meta-Analysis. 2016;133(12):1189–1198. doi: 10.1161/CIRCULATIONAHA.115.018006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rathman LD, Lee CS, Sarkar S, Small RS. A critical link between heart failure self-care and intrathoracic impedance. The Journal of cardiovascular nursing. 2011;26(4):E20–E26. doi: 10.1097/JCN.0b013e3181ee28c8. [DOI] [PubMed] [Google Scholar]
- 18.Lee CS, Moser DK, Lennie TA, Tkacs NC, Margulies KB, Riegel B. Biomarkers of myocardial stress and systemic inflammation in patients who engage in heart failure self-care management. J Cardiovasc Nurs. 2011;26(4):321–328. doi: 10.1097/JCN.0b013e31820344be. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee CS, Tkacs NC, Riegel B. The Influence of Heart Failure Self-care on Health Outcomes Hypothetical Cardioprotective Mechanisms. J Cardiovasc Nurs. 2009;24(3):179–187. doi: 10.1097/JCN.0b013e31819b5419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee CS, Gelow JM, Denfeld QE, et al. Physical and Psychological Symptom Profiling and Event-Free Survival in Adults With Moderate to Advanced Heart Failure. The Journal of cardiovascular nursing. 2013;00(0):1–9. doi: 10.1097/JCN.0b013e318285968a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A New Method of Classifying Prognostic in Longitudinal Studies: Development and Validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 22.Levy WC. The Seattle Heart Failure Model: Prediction of Survival in Heart Failure. Circulation. 2006;113(11):1424–1433. doi: 10.1161/CIRCULATIONAHA.105.584102. [DOI] [PubMed] [Google Scholar]
- 23.Hlatky MA, Boineau RE, Higginbotham MB, et al. A brief self-administered questionnaire to determine functional capacity (The Duke Activity Status Index) The American Journal of Cardiology. 1989;64(10):651–654. doi: 10.1016/0002-9149(89)90496-7. [DOI] [PubMed] [Google Scholar]
- 24.Jurgens CY, Lee CS, Riegel B. Psychometric Analysis of the Heart Failure Somatic Perception Scale as a Measure of Patient Symptom Perception. J Cardiovasc Nurs. 2015 doi: 10.1097/JCN.0000000000000320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spitzer RL, Kroenke K, Williams JDW. Validation and Utility of a Self-report Version of PRIME-MD: The PHQ Primary Care Study. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 26.Kroenke K, Spitzer RL, Willaims JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Riegel B, Lee CS, Dickson VV, Carlson B. An update on the self-care of heart failure index. The Journal of cardiovascular nursing. 2009;24(6):485–497. doi: 10.1097/JCN.0b013e3181b4baa0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barbaranelli C, Lee CS, Vellone E, Riegel B. Dimensionality and Reliability of the Self-Care of Heart Failure Index Scales: Further Evidence From Confirmatory Factor Analysis. Research in Nursing & Health. 2014;37(6):524–537. doi: 10.1002/nur.21623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bilbao A, Escobar A, Garcia-Perez L, Navarro G, Quiros R. The Minnesota living with heart failure questionnaire: comparison of different factor structures. Health Qual Life Outcomes. 2016;14:23. doi: 10.1186/s12955-016-0425-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rector TS, Cohn JN. Assessment of patient outcome with the Minnesota Living with Heart Failure questionnaire: Reliability and validity during a randomized, double-blind, placebo-controlled trial of pimobendan. American Heart Journal. 1992;124 doi: 10.1016/0002-8703(92)90986-6. [DOI] [PubMed] [Google Scholar]
- 31.Grady KL. Self-care and Quality of Life Outcomes in Heart Failure Patients. Journal of Cardiovascular Nursing. 2008;23(3):285–292. doi: 10.1097/01.JCN.0000305092.42882.ad. [DOI] [PubMed] [Google Scholar]
- 32.Behlouli H, Feldman DE, Ducharme A, et al. Identifying relative cut-off scores with neural networks for interpretation of the Minnesota Living with Heart Failure questionnaire. 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society; 3–6 Sept. 2009; 2009. [DOI] [PubMed] [Google Scholar]
- 33.Hwang SL, Liao WC, Huang TY. Predictors of quality of life in patients with heart failure. Jpn J Nurs Sci. 2014;11(4):290–298. doi: 10.1111/jjns.12034. [DOI] [PubMed] [Google Scholar]
- 34.Wu JR, Lennie TA, Frazier SK, Moser DK. Health-Related Quality of Life, Functional Status, and Cardiac Event-Free Survival in Patients With Heart Failure. J Cardiovasc Nurs. 2016;31(3):236–244. doi: 10.1097/JCN.0000000000000248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Comin-Colet J, Anguita M, Formiga F, et al. Health-related Quality of Life of Patients With Chronic Systolic Heart Failure in Spain: Results of the VIDA-IC Study. Rev Esp Cardiol (Engl Ed) 2016;69(3):256–271. doi: 10.1016/j.rec.2015.07.030. [DOI] [PubMed] [Google Scholar]
- 36.Lee CS, Gelow JM, Mudd JO, et al. Profiles of self-care management versus consulting behaviors in adults with heart failure. Eur J Cardiovasc Nurs. 2015;14(1):63–72. doi: 10.1177/1474515113519188. [DOI] [PubMed] [Google Scholar]
- 37.Holzapfel N, Lowe B, Wild B, et al. Self-care and depression in patients with chronic heart failure. Heart Lung. 2009;38(5):392–397. doi: 10.1016/j.hrtlng.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 38.Kessing D, Denollet J, Widdershoven J, Kupper N. Psychological Determinants of Heart Failure Self-Care: Systematic Review and Meta-Analysis. Psychosom Med. 2016;78(4):412–431. doi: 10.1097/PSY.0000000000000270. [DOI] [PubMed] [Google Scholar]
- 39.Lee KS, Lennie TA, Warden S, Jacobs-Lawson JM, Moser DK. A comprehensive symptom diary intervention to improve outcomes in patients with HF: a pilot study. J Card Fail. 2013;19(9):647–654. doi: 10.1016/j.cardfail.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 40.Graven LJ, Grant JS, Vance DE, Pryor ER, Grubbs L, Karioth S. Predicting depressive symptoms and self-care in patients with heart failure. Am J Health Behav. 2015;39(1):77–87. doi: 10.5993/AJHB.39.1.9. [DOI] [PubMed] [Google Scholar]
- 41.Peters-Klimm F, Freund T, Kunz CU, et al. Determinants of heart failure self-care behaviour in community-based patients: a cross-sectional study. Eur J Cardiovasc Nurs. 2013;12(2):167–176. doi: 10.1177/1474515112439964. [DOI] [PubMed] [Google Scholar]


