Abstract
The Fragile X Syndrome (FXS) is one of the most common forms of inherited intellectual disability in all human societies. Caused by the transcriptional silencing of a single gene, the fragile x mental retardation gene FMR1, FXS is characterized by a variety of symptoms, which range from mental disabilities to autism and epilepsy. More than 20 years ago, a first animal model was described, the Fmr1 knock-out mouse. Several other models have been developed since then, including conditional knock-out mice, knock-out rats, a zebrafish and a drosophila model. Using these model systems, various targets for potential pharmaceutical treatments have been identified and many treatments have been shown to be efficient in preclinical studies. However, all attempts to turn these findings into a therapy for patients have failed thus far. In this review, I will discuss underlying difficulties and address potential alternatives for our future research.
Keywords: Fragile X Syndrome, mouse model, FMR1, microsatellite instability, E/I balance, behavior and cognition, primates, autism spectrum disorders
Introduction
The tremendous advance that has taken place in life sciences during the last decades has opened a variety of options and opportunities for research as well as for human societies, in particular in the field of genetics. One of these advances was the invention of the Crispr-Cas system (Crispr; reviewed in Donohoue et al., 2017; Huang et al., 2017; Petersen, 2017). The technique allows for a fast and relatively precise gene editing in a variety of different organisms ranging from plants and insects to vertebrates and primates including human cell lines and embryos. Being relatively efficient and easy to use, the system promises much progress not only for our understanding of complex biological systems, but also for the treatment of genetic disorders.
Of foremost interest in this context are monogenetic diseases with limited treatment options for patients, such as the Fragile X Syndrome (FXS), a nonetheless strikingly complex autism spectrum disorder (ASD). Combined with the advance of genetic screening methods for persons at risk (reviewed in Rajan-Babu and Chong, 2016) and assisted reproduction services, the Crispr technique opens not only new horizons, but also raises many ethical concerns, although there is no common agreement on ethical standards among mankind and not all people are sharing the concerns.
For our future research, it will therefore be important to critically evaluate what we are able to achieve, what we have achieved, and, on a society based level, what we do want to achieve. This article will review and discuss important results as well as ideas from the FXS field, and in particular address underlying difficulties arising from the current mouse models.
The Fragile X Syndrome — of Men
Phenotype
Affecting approximately 1 in 7000 males and 11,000 females (meta-analysis: Hunter et al., 2014), FXS represents one of the most frequent forms of monogenetically determined mental retardation in all human populations and ethnic groups (reviewed in Tzschach and Ropers, 2007). In the vast majority of cases, the disease is caused by the transcriptional silencing of a single gene on the X chromosome, the Fragile X Mental Retardation gene FMR1. In consequence, expression of the encoded protein FMRP is lost (reviewed in Saldarriaga et al., 2014; Usdin and Kumari, 2015).
FXS patients display a variety of intellectual deficits ranging from mild learning impairments to severe cognitive disabilities, but also autistic behaviors such as aggression, social anxiety and stereotypic acting characterize the disease (reviewed in Saldarriaga et al., 2014; Gross et al., 2015b; Figure 1). Men are in general more severely affected than women, achieving only average IQs1 of 40–50, whereas women mainly present with mild to moderate cognitive impairments and an average IQ of about 80, though their abilities may range from severe deficits to superior performances (Freund et al., 1993; de Vries et al., 1996; Lewis et al., 2006; Chaste et al., 2012, reviewed in Huddleston et al., 2014). However, even men can be high functioning (Basuta et al., 2015).
Figure 1.
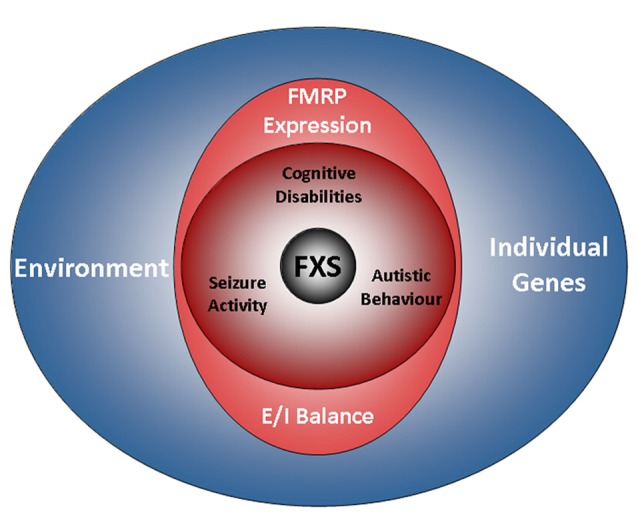
The FXS world. The drawing illustrates factors influencing the disease. A characteristic of FXS is the presence of a broad range of deficits with a high degree of individual variation. The phenotype of the disorder includes cognitive disabilities as well as autistic behaviors and epilepsy. Aside from a loss of FMRP expression, the genetic background and environmental factors are emerging as determinants of the disease. However, while residual FMRP expression is known to correlate with the cognitive performance of FXS patients, the impact of individual genes and the relevance of the environment are less well understood (also see the section “Phenotype”). Recent findings indicate that autistic behaviors and epilepsy are influenced by the E/I balance, but not by residual FMRP expression. FXS, Fragile X Syndrome; FMRP, Fragile X Mental Retardation Protein; E/I balance, balance of excitation and inhibition in neuronal networks.
Shyness, poor eye contact and attention difficulties are particularly characteristic to young women with FXS (FMR1−/–), whereas increased aggression and the use of rote phrases are more typical to men (Murphy and Abbeduto, 2007; Hartley et al., 2011). In their adult life, women are mostly affected by deficits in interpersonal skills, while weak functional skills primarily concern men, though reduced social interaction skills are also prominent in men (Hartley et al., 2011). As a result, only 9% of the men affected by FXS achieve a high or very high level of independence in adult life, whereas 44% of the FXS women reach such a level. Contrary to most other X-linked diseases, approximately 35% of the women carrying a single mutated allele only (FMR1–/+) also demonstrate cognitive disabilities (Hagerman et al., 1992).
The impairments observed in FXS patients are not uniform though, but rather specific to certain capabilities: several studies demonstrated that FXS patients perform particularly weak in tasks requiring abstract item reasoning, attention, the solution of new problems and goal-directed actions, as well as in tasks relying on short-term memory and visual-motor coordination. By contrast, FXS patients usually demonstrate normal skills in vocabulary knowledge, although they show a cluttered and less complex speech (Hanson et al., 1986; Dykens et al., 1987; Maes et al., 1994; Loesch et al., 2004; Lewis et al., 2006; Roberts et al., 2007; Van der Molen et al., 2010).
Recent research has linked some of the variability observed in the cognitive phenotype of FXS patients to residual FMRP expression and mosaic expression patterns (Kaufmann et al., 1999; Dyer-Friedman et al., 2002; Loesch et al., 2003, 2004; Pretto et al., 2014; Basuta et al., 2015). For instance, the cognitive abilities of FXS patients were shown to strongly correlate with FMRP expression levels, even when full-scale IQ scores are used. Although this holds true for most of the cases, exceptions exist: Govaerts and colleagues reported a case, in which residual FMRP expression could not explain the good cognitive performance observed (Govaerts et al., 2007), thus implying a role for individual genetic factors and/or environmental effects (cp.2 Figure 1).
Further studies indeed support the significance of environmental factors in FXS (Dyer-Friedman et al., 2002; Kuo et al., 2002; Glaser et al., 2003): in particular maternal warmth and responsivity were demonstrated to ameliorate maladaptive as well as autistic behaviors, whereas maternal depression and criticism were indicated to increase FXS symptoms in children (Greenberg et al., 2012; Robinson et al., 2016; Smith et al., 2016). Contrary to cognitive deficits, autistic behaviors display no correlation with residual FMRP expression (Glaser et al., 2003; Pretto et al., 2014).
Particularly in children, seizures are frequent as well, affecting about 45% of the adolescent patients between 1 year and 14 years of age (Cowley et al., 2016; Figure 1). After the age of 20, seizure activity decreases, resulting in an overall prevalence of about 24% (Sabaratnam et al., 2001), although there is considerable variation among studies. Interestingly, some data suggest that the attention deficits observed in FXS patients are related to seizure activity (Cowley et al., 2016).
Just like autistic behaviors, seizure activity was found not to correlate with residual FMRP expression (Pretto et al., 2014). Although an imbalance of excitatory and inhibitory neuronal activity has been associated with seizure activity and autistic behaviors in several ASDs as well as in corresponding animal models (reviewed in Frye et al., 2016; Uzunova et al., 2016; Lee et al., 2017), data on FXS patients are rare. Using EEG3 electrodes, increases in event related potentials were found in the auditory cortex of FXS children, suggesting enhanced excitability (Castrén et al., 2003). EEG-studies of oscillatory dynamics in males with FXS identified impaired theta oscillations indicative of an imbalance in excitatory and inhibitory neuronal circuit activity (Van der Molen and Van der Molen, 2013; Van der Molen et al., 2014) and implied a lack of coordination in information processing. Notably, two studies also found decreased activations, one in prefrontal regions and one in the fusiform gyrus (Dalton et al., 2008; Holsen et al., 2008). These findings suggest that FXS patients experience brain-region and most likely circuit-specific imbalances in neuronal excitation.
Genotype
Microsatellites — Sources of Complexity
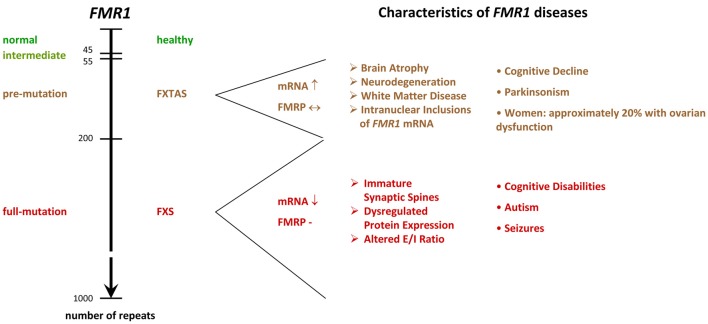
The molecular mechanisms leading to the silencing of the FMR1 gene during embryonic development are complex and result from expansions in the length of a microsatellite located in the 5′UTR4 of FMR1 (Fu et al., 1991; Pieretti et al., 1991; Verkerk et al., 1991; Eiges et al., 2007; Bar-Nur et al., 2012). In healthy individuals, the sequence consists of CGG/CCG tandem tracts and includes approximately 6–44 repeats, whereas FXS patients show more than 200 repeats. FMR1 alleles containing 45–54 repeats are classified as intermediate, and 55–200 repeats as pre-mutation alleles (Figure 2). Contrary to regular tandem tracts, pre-mutation alleles are meiotically as well as mitotically unstable and may turn into full-mutation alleles within one generation, if transmitted by a female (Fu et al., 1991; Heitz et al., 1992; Yu et al., 1992).
Figure 2.
FMR1−/y diseases. The scheme shows the relation between microsatellite length (number of repeats) and phenotype. While healthy individuals show 6–44 tandem tracts in the 5′ UTR of their FMR1 gene, FXS patients display more than 200 repeats. Alleles containing 45–54 repeats are classified as intermediate, and 55–200 repeats as pre-mutation alleles. Premutation alleles give rise to a neurodegenerative disorder called FXTAS, which presents with parkinsonism and brain atrophy. FXTAS typically manifests in individuals over the age of 50. FMR1: Fragile X Mental Retardation gene. FMRP: Fragile X Mental Retardation Protein. FXS: Fragile X Syndrome. FXTAS: Fragile X-associated Tremor/Ataxia Syndrome. E/I balance: balance of excitation and inhibition in neuronal networks, UTR: untranslated region. ↓: decreased levels in the diseased condition. ↔ similar levels in normal and diseased conditions. ↑ increased levels in diseased conditions.
Although microsatellites are often associated with diseases (reviewed in Nelson et al., 2013; Zhang and Ashizawa, 2017), they turned out to play crucial roles in many species, but in particular in humans. Due to their high variability, tandem tracts are thought to serve as a substrate for evolution (reviewed in Kashi and King, 2006; Hannan, 2012; Plohl et al., 2012). Most microsatellites are nonetheless only maintained by chance and total microsatellite numbers are rather species or clade specific than related to vertebrate evolution (Buschiazzo and Gemmell, 2010; Adams et al., 2016). Yet, tract length polymorphism turned out to be a major source for the emergence of variability and complexity in species: recent research revealed that tandem tracts located in regulatory regions contribute to the genesis of complexity (Liu H. et al., 2012; Namdar-Aligoodarzi et al., 2015). By triggering the formation of secondary structures in DNA as well as RNA molecules in a length dependent manner, these repeats redress the transcription and translation efficiency and, in doing so, control the expression level of their proteins (reviewed in Kashi and King, 2006; Pezer et al., 2012; Sawaya et al., 2012; also see e.g., Zumwalt et al., 2007; Halder et al., 2009; Vinces et al., 2009; Quilez et al., 2016). In consequence, the protein stoichiometry is altered, leading to modifications in a variety of protein interactions, while the functionality of the protein itself is preserved. It is therefore no surprise that tandem tracts are preferentially located in the proximity of transcription starts (Vinces et al., 2009; Sawaya et al., 2013; Liang K. C. et al., 2015), that human promoter regions are particularly rich in microsatellites (Sawaya et al., 2013) and that the polymorphism and complexity of tandem tracts significantly increase in primates and humans (Zhang et al., 2004; Mohammadparast et al., 2014; Sabino et al., 2014; Bilgin Sonay et al., 2015; Namdar-Aligoodarzi et al., 2015; Ohadi et al., 2015; Rezazadeh et al., 2015).
Moreover, tandem tract polymorphism turned out to be astonishingly abundant in genes involved in the development of the nervous system (Riley and Krieger, 2009). Indeed, some studies even associated repeat variations with individual differences in behavioral traits—not only in humans (Gerra et al., 2005; Larsen et al., 2010; Simmons and Roney, 2011; Berry et al., 2013; Durdiaková et al., 2013; Valomon et al., 2014; Votinov et al., 2015), but also in birds (Stuber et al., 2016) and other mammals (Hammock and Young, 2005; Lucarelli et al., 2017). In addition, Bagshaw and colleagues showed that polymorphic microsatellites of genes involved in human personality traits and social behavior are able to integrate interactions with the environment, in this case maternal smoking, which caused anti-social acts in carriers of certain TBR1 alleles (Bagshaw et al., 2017). Their finding is in line with an earlier study showing that a CGG repeat variant of the glutathion peroxidase 1 gene is protective for autism (Ming et al., 2010). Indeed, it has been found that prenatal oxidative stress, such as caused by environmental toxicants, is involved in the establishment of autism, in particular when occurring in certain sensitive stages of embryogenesis (reviewed in Chauhan and Chauhan, 2006; Landrigan, 2010; Wells et al., 2016; Heyer and Meredith, 2017).
These findings illustrate that microsatellite polymorphism is an important component of individuality, complexity, neuronal development and gene-environment interactions. Since FMRP itself is developmentally regulated (Hinds et al., 1993) and was found to function in neuronal migration, differentiation and dendritic spine maturation (Hinton et al., 1991; Irwin et al., 2001; Saffary and Xie, 2011; Telias et al., 2013; La Fata et al., 2014; Khalfallah et al., 2017), it seems therefore possible that the microsatellite of FMR1 might have currently unrecognized functions in the individual peculiarities characteristic to FXS.
To Silence or Not to Silence Expanded FMR1?
Transcript toxicity in humans
Mirroring the results on microsatellites and protein expression, the different FMR1 alleles indeed give rise to different expression patterns: pre-mutation carriers are characterized by enhanced mRNA, but normal or slightly reduced protein levels, since the elongated transcripts are inefficiently translated, but heavily transcribed (Tassone et al., 2000a,b; Kenneson et al., 2001; Primerano et al., 2002; Ludwig et al., 2014), whereas full-mutations cause FMRP deficiency due to DNA hypermethylation, Histone modification and subsequent heterochromatin formation (Pieretti et al., 1991; Sutcliffe et al., 1992; Hornstra et al., 1993; Coffee et al., 1999, 2002; Kumari and Usdin, 2010). Some residual mRNA is nonetheless still present in many men with FXS, but the mRNA is not translated (Tassone et al., 2001), probably due to secondary structure formation in the tandem tract.
It is noteworthy that pre-mutation carriers often develop a neurodegenerative disorder called the Fragile X-associated Tremor/Ataxia Syndrome (FXTAS, Figure 2), which presents with neurodegeneration, parkinsonism and brain atrophy, and which is associated with primary ovarian insufficiency in females (reviewed in Botta-Orfila et al., 2016; Hagerman and Hagerman, 2016). FXTAS is believed to arise from a toxicity of elongated mRNA transcripts and/or of a cryptic FMR1 protein derived from CGG repeat triggered non-ATG translation (Handa et al., 2005; Hashem et al., 2009; Chen et al., 2010; Todd et al., 2013). Since the transcript levels are markedly reduced in FXS patients, these findings suggest that the silencing of full-mutation alleles in FXS serves to prevent from toxic effects, however, clear evidence for a toxicity of the full-mutation mRNA or the cryptic protein is missing. Indeed, the identification of several healthy and non-mosaic individuals carrying unmethylated, normally expressing full-mutation alleles (Smeets et al., 1995; Pietrobono et al., 2005; Tabolacci et al., 2008) argues against the idea of mutation-triggered toxicity in humans. Nonetheless, two cases were identified, where expression of a full-mutation gene caused severe FXTAS (Loesch et al., 2012; Santa Maria et al., 2014), thus supporting the idea that a fully mutated FMR1 transcript can have toxic effects and that elongated transcripts are causative for FXTAS, but not for FXS, although some mRNA is present in many FXS patients (Tassone et al., 2001).
These apparently conflicting cases illustrate that individual genes and/or environmental effects may overcome the typical mechanisms and phenotypes observed in FXS. The relevance of the latter is further emphasized by the fact that alcohol abuse seemed to be involved in the case of severe FXTAS reported by Loesch and colleagues (Loesch et al., 2012). Recent studies revealed that alcohol is in fact exaggerating behavioral problems such as aggression and impulsivity in FXS patients (Salcedo-Arellano et al., 2016) and accelerating neurological deterioration in FXTAS (Muzar et al., 2014). It might be for these negative effects that, in contrast to cases of high-functioning autism, where patients used drinking to cope with social anxiety (Lalanne et al., 2015), alcoholism is at least in FXS patients rare (cp. Salcedo-Arellano et al., 2016).
For our future research, it will therefore be important to address questions such as: Why may fully mutated FMR1 transcripts have toxic effects in one case, but not in the other? How does the environment influence the underlying mechanisms? Why may it be better to have a fully mutated gene silenced, and thus FXS, than unsilenced, and eventually FXTAS — from an evolutionary point of view? A deeper understanding of the relevance of genetic individuality is required before attempting a reactivation of FMR1 in patients (reviewed in Tabolacci et al., 2016b) — in particular, since full-mutation mRNA is not necessarily translated (Tassone et al., 2001; Dolskiy et al., 2017) and since transcribed alleles are able to cause FXTAS under circumstances currently unknown (Loesch et al., 2012; Santa Maria et al., 2014).
A question of secondary structures?
An alternative explanation for the silencing of full-mutation alleles is DNA stability. During germ cell generation as well as during early phases of embryogenesis and prior to the silencing of FMR1, CGG repeats may expand or contract through mechanisms under debate (reviewed in Mor-Shaked and Eiges, 2016; Gerhardt, 2017). Despite some uncertainty about the exact molecular events that cause repeat instability, it is believed that the formation of secondary DNA structures during recombination, DNA replication and DNA repair leads to the addition or deletion of repeats. Since no repeat instability has been observed in FMR1 postnatally (Reyniers et al., 1993, 1999; Wöhrle et al., 1993), it is thought that the instability is related to events of the embryogenesis.
Little is known about the factors that could contribute to the instability of the CGG repeats in FMR1. It has been noticed that the number of repeats, the content of interspersed AGG and the haplotype are able to influence the stability of FMR1 (Oberlé et al., 1991; Eichler et al., 1994; Gunter et al., 1998; Hirst and White, 1998; Taylor et al., 1999; Larsen et al., 2000; Dombrowski et al., 2002; Nolin et al., 2003, 2013, 2015; Yrigollen et al., 2012, 2013, 2014; Avitzour et al., 2014; Weiss et al., 2014). AGG interruptions, for instance, have been indicated to support the stability of FMR1 by reducing secondary structure formation (Weisman-Shomer et al., 2000; Jarem et al., 2010) and promoting appropriate DNA conformations (Jarem et al., 2010) as well as adequate DNA packing (Mulvihill et al., 2005; Volle and Delaney, 2013). Furthermore, the number of repeats was shown to directly correlate with the instability of the tandem tracts (Oberlé et al., 1991; Eichler et al., 1994; Taylor et al., 1999; Avitzour et al., 2014): it is assumed that the size of G-rich tracts directly correlates with the formation of secondary structures and polymerase slippage during replication (Mornet et al., 1996; Freudenreich et al., 1997; Weitzmann et al., 1997; Hirst and White, 1998). In line with this idea, the total length of the CGG repeat allele turned out to be the best predictor for the risk of transmission (Yrigollen et al., 2014).
Aside from internal genetic properties, trans-acting factors have also been postulated to affect the stability of FMR1 during mitosis and meiosis (Mornet et al., 1996; Nolin et al., 1996, 1999), but although it seems plausible that other genes might impact on the stability of FMR1, studies are rare. In an attempt to identify such trans-acting factors, Xu et al. (2013) analyzed two microarray sets containing data on the transcript expression in FXS patients and controls, and found a significant down-regulation of DNA damage/repair pathway transcripts, thus implying that impaired DNA repair pathways may support FMR1 instability in FXS patients.
Remarkably, environmental factors have also been found to influence the instability of FMR1: maternal age was recently related to increased instability (Yrigollen et al., 2014) and oxidative stress was demonstrated to interfere with the stability of FMR1 (Adihe Lokanga et al., 2014). The latter finding is in line with other studies showing that different kinds of stress can induce instability in microsatellites (Chatterjee et al., 2015; Wu et al., 2017) and that oxidized DNA can trigger repeat expansion or contraction (Lai et al., 2013; Cilli et al., 2016). Given that chronic alcoholism causes oxidative stress (reviewed in Wu et al., 2006; Hernández et al., 2016), the data imply that alcohol abuse could contribute to the consolidation of FMR1 diseases. Interestingly, a study conducted by Kogan and colleagues found alcoholism to be significantly more common in families of pre-mutation carriers than in control families (Kogan et al., 2008). Although this association does not tell whether the disease (FXTAS) is causing the alcoholism, for example by overcharging family members who care for their affected relatives, or whether the alcoholism is causing the disease (or both), the facts that maternal alcoholism seems to increase the risk for FXS (mentioned in Hagerman et al., 2010) and that foetuses are particularly vulnerable to alcohol (reviewed in Henderson et al., 1999; Dennery, 2007) support a role for alcohol abuse in the emergence of FXS. Much more research is needed to establish the relation of toxins, such as derived from smoking or drinking, oxidative stress, microsatellite instability and the consolidation of FMR1 diseases.
Repeat numbers exceeding 200 tandems trigger the epigenetic silencing of FMR1 by initiating an abnormal 5′-C-phosphate-G-3′ methylation and repressive Histone modifications in the promoter region (e.g., Coffee et al., 1999, 2002; Chandler et al., 2003; Kumari and Usdin, 2010; Brasa et al., 2016). As a consequence, CpG5 islands flanking the repeats as well as the repeats itself, which also function as a CpG island, become hypermethylated and render the gene inactive (Hansen et al., 1992). Studies in human FXS cell lines aiming to reactivate FMR1 by either changing repressive Histone modifications (Kumari and Usdin, 2016; Dolskiy et al., 2017) or decreasing CpG methylation (Chiurazzi et al., 1998; Coffee et al., 2002; Tabolacci et al., 2005, 2016a), suggest that DNA methylation is the primary cause for gene inactivity, while repressive Histone methylations have a supportive function.
The molecular mechanisms by which CGG expansions trigger the epigenetic silencing of FMR1 are currently not well understood though (for a review, please see Usdin and Kumari, 2015). It is thought that transient unpairing of the DNA during replication, transcription or repair provides an opportunity for the repeat region of FMR1 to form secondary structures such as hairpins or G-quadruplexes (Fry and Loeb, 1994; Kettani et al., 1995; Mitas et al., 1995; Usdin and Woodford, 1995; Patel et al., 2000; Loomis et al., 2014). Similar structures occur in FMR1 transcripts (Handa et al., 2003; Napierala et al., 2005; Zumwalt et al., 2007; Malgowska et al., 2014). Studies showed that these secondary structures hinder replication, transcription and translation (Fry and Loeb, 1994; Nadel et al., 1995; Usdin and Woodford, 1995; Subramanian et al., 1996) and that structure-disrupting proteins are able to alleviate the situation (Fukuda et al., 2005; Khateb et al., 2007), thus suggesting that the formation of secondary structures is troubling the cells.
Not all structures are alike though: R-loops, a DNA-RNA hybrid formed during transcription, were recently indicated to prevent gene silencing by protecting DNA from de novo methylation (Ginno et al., 2012). Moreover, R-loops were shown to cause chromosome decondensation and transcription activation (Powell et al., 2013). Since FMR1 has been observed to give rise to R-loops (Groh et al., 2014; Loomis et al., 2014), this data could nicely explain the enhanced expression of pre-mutation alleles observed in FXTAS, but experimental evidence is missing. In fact, Groh and colleagues found that the formation of R-loops on FMR1 impedes gene expression (Groh et al., 2014), thus suggesting that R-loop formation is involved in the silencing of FMR1. Their data are in line with another study demonstrating that promoter-bound FMR1 transcripts containing tandem tracts induce the silencing of FMR1 (Colak et al., 2014).
The relevance of the number of repeats required to build R-loops and the role of the respective loop size are not yet clear though, since R-loops were found to form on normal, pre-mutation and full-mutation alleles (Colak et al., 2014; Groh et al., 2014; Loomis et al., 2014). It seems therefore possible that the role of R-loops in transcription regulation depends on the loop size: Loomis and colleagues provided evidence that the expansion of FMR1 repeats causes an enhanced formation of aggrandized loops, which tend to form higher-order structures. These structures distinguish FMR1 from other CpG islands containing promoters (Ginno et al., 2012, 2013) and could finally trigger repeat instability and hypermethylation (Loomis et al., 2014). Hence, R-loops formed on FMR1 could enhance gene expression until they exceed a specific size and form secondary structures. Previous research on the methylation of different loci indeed indicated that it is the higher-order structures that trigger DNA methylation (Smrzka et al., 1995; Paoloni-Giacobino et al., 2007; Gentry and Meyer, 2013).
These findings imply that CpG methylation could serve to limit the formation of secondary structures. Nuclear magnetic resonance analyses revealed CpG methylations to decrease the dynamics of the DNA backbone (Geahigan et al., 2000), while molecular dynamic investigations illustrated DNA methylation to increase the rigidity of the DNA by steric hinderance and hydrophobicity (Derreumaux et al., 2001). Using density functional theory and nuclear magnetic resonance measurements, Taqi and colleagues further demonstrated that cytosine methylation impairs the conformational flexibility of short ssDNA6 molecules and their ability to form secondary structures (Taqi et al., 2012). Although these data support the idea that hypermethylation of FMR1 could serve to prevent the formation of secondary structures, more evidence is required.
Further studies showed that the hypermethylation of FMR1 indeed correlates with enhanced tract stability during mitosis (Gläser et al., 1999; Wöhrle et al., 2001; Nichol Edamura et al., 2005). Remarkably, Zhou and colleagues observed that cells carrying fully mutated and hypermethylated alleles outcompete those carrying alleles with less repeats and no methylation when co-cultured, resulting in a loss of these cells (Zhou et al., 2016). Since no differences were seen in the viability of both cell lines, toxic effects are unlikely to account for the disappearing of cells with unsilenced alleles. The reasons for this effect remain to be investigated though.
The data imply that hypermethylation of FMR1 should occur when cells start to divide a lot. Studies using fetal tissues showed that hypermethylation is established between the 10th and 12th week of gestation, but FMR1 may remain partly active for some time (Devys et al., 1992; Sutcliffe et al., 1992; Suzumori et al., 1993; Iida et al., 1994; Willemsen et al., 2002; reviewed in Mor-Shaked and Eiges, 2018). Models of cell division in human embryos do not support high rates of mitosis during this time though, they rather show a decline in division rates (Luecke et al., 1999). Looking at the brain in specific, the situation is yet different: By the 9th week of gestation, neuronal tube formation is completed and shortly after, at the 12th week of gestation, neurogenesis as well as neuronal migration will reach their first peak (reviewed in Linderkamp et al., 2009). Nerve cells will then be proliferating at rates of about 15 million per hour (reviewed in Ackerman, 1992), thus implying that the silencing of FMR1 could be related to cell line-specific changes serving in neurogenesis. Such a mechanism could be important to maintain the correct timing and pace during neuronal development, which is essential to establish the complex connections that characterize the brain.
Indeed, when Khalfallah and colleagues induced differentiation in a murine embryonic stem cell line lacking FMRP (shFmr1 ES), they found an accelerated generation of both, progenitor and neuronal cells during the first steps of neurogenesis (Khalfallah et al., 2017; reviewed in Bardoni et al., 2017; Westmark, 2017). Their experiments further revealed that this phenotype is due to enhanced expression of a target of FMRP, APP7, which is able to accelerate neurogenesis following cleavage into the A-beta peptide. This mechanism might also provide an alternative or additional explanation for the observation that embryonic stem cells carrying a hypermethylated FMR1 gene outcompete cells with the active gene as it was found by Zhou and colleagues (Zhou et al., 2016). It will be interesting to see how these changes affect neuronal maturation and signaling and how the findings of Khalfallah and colleagues relate to neuronal development in humans.
Notably, studies employing human embryonic stem cells (hESCs) showed that the epigenetic silencing of FMR1 may occur prior to differentiation (Avitzour et al., 2014; Zhou et al., 2016) or upon differentiation (Eiges et al., 2007): of 11 hESC lines, 7 showed some levels of stable hypermethylation prior to differentiation. It is not yet clear though, when and how the hypermethylation is established. Current models suggest that fully expanded genes first acquire abnormal methylation patterns before or during embryo implantation and that FMR1 silencing is achieved after the blastocyst stage. Microsatellites that escape the initial methylation changes are believed to remain unmethylated. Since standard reprogramming procedures serving to generate induced pluripotent stem cells (iPSCs) from skin fibroblasts are unable to remove the exaggerated methylation marks inactivating FMR1 (Urbach et al., 2010; Sheridan et al., 2011; Doers et al., 2014), hypermethylation is thought to be stable and irreversible once it is established.
This is not necessarily the case though: removing CGG repeats and the immediate 5′-flanking region from fully mutated microsatellites in the FMR1 gene of a male iPSC line by the CRISPR/Cas9 system, Park and colleagues were able to restore FMR1 gene expression as well as FMRP protein levels in a pair of clones (Park et al., 2015). The reactivation of FMR1 led to a stable expression of the gene throughout differentiation into mature neurons. These findings are further supported by the previously mentioned study of Zhou and colleagues, who showed that hypermethylation present in embryonic stem cells is dynamic (Zhou et al., 2016): alleles containing over 400 repeats may contract to smaller repeat numbers, resulting in a permanent reactivation even when more than 200 tandems are present. Moreover, de Esch and colleagues (de Esch et al., 2014) observed that the reprogramming of fibroblasts from an atypical individual carrying an active full mutation FMR1 gene with 330 repeats into iPSCs recurrently resulted in a complete inactivation of the gene. Taken together, these studies not only illustrate the dynamics of the system, but also suggest that repeat length is not the only factor influencing the silencing of FMR1 and that other factors, such as neurodevelopmental stage are involved. Indeed, the fact that the brother of the atypical individual also carried an unsilenced full-mutation implies that maternal-parental components, which were not present in fibroblasts or inactivated during the reprogramming procedure, and/or specific environmental factors caused their FMR1 genes to remain active despite the high repeat length.
Aside from tandem repeat polymorphism, mutations in the coding region of FMR1 have also been associated with the occurrence of FXS in patients (Quartier et al., 2017): a deletion of the last exon, which is giving rise to a truncated FMRP isoform, was recently identified in three brothers meeting FXS criteria (Hagerman’s scores = 15). Moreover, two splice variants were detected in two unrelated patients showing the same outcome in the test, and several missense mutations have been identified in FXS patients (Siomi et al., 1994; Handt et al., 2014; Myrick et al., 2014). Although these cases represent rare exemptions, they nonetheless demonstrate that the correct functioning of FMRP is central to FXS.
The Fragile X Syndrome — of Mice
The Genotype of Mice or the Charm of Simplicity
Mice are much different from humans, they are much smaller, live much shorter and have much less to learn. Nonetheless, mice and men are sharing almost 99% of their genes (Waterston et al., 2002) as well as most physiological functions and pathogenic mechanisms (see for example the reviews of Tecott, 2003; Elefteriou and Yang, 2011; Van der Weyden and Adams, 2013; Jacobs et al., 2013; Eilam, 2014; Hoehndorf et al., 2014; Vandamme, 2014; Lubojemska et al., 2016). Indeed, even their aging was recently shown to match human senescence surprisingly well (Dutta and Sengupta, 2016). Since mice are also easy to keep, they became the most widely used model organism in life sciences after their first documented employment almost 500 years ago (reviewed in Paigen, 2003; Goodman et al., 2015): of nearly 11.5 million animals used for scientific purposes in the European Union in 2011, 61% were mice (European Commission, 2010). Despite these massive research efforts, most attempts to translate the outcomes to humans have failed. In the FXS field for instance, more than 70 studies reporting rescues (excluding reviews) have been published on pubmed during the last 12 years, 63 clinical trials are registered on ClinicalTrials.gov, and not a single treatment is available for patients yet (2nd of October 2017; current state reviewed in Ligsay and Hagerman, 2016). Although several positive outcomes were observed during the trials, indicating at least some progress toward a better understanding of the disease and a treatment for patients, discrepancies between the data obtained in men and mice were common: benefits experienced by patients were often very subtle, limited to subgroups, outside the outcome measures or simply absent. How much wishful-thinking is involved in our mouse models?
Some facts on men and mice (for more details, please see Table 1):
mice are 3000× smaller
mice and humans diverted 75 million years ago (Waterston et al., 2002)
laboratory mice are highly inbred
their genome is approximately 14% smaller, probably due to deletions (Waterston et al., 2002)
the DNA sequence identity is only 40% (Waterston et al., 2002)
the average substitution rate in mice is twofold higher than in humans (Waterston et al., 2002)
manipulations of their genome may induce mutations in their microsatellite sequences (Zuo et al., 2012; Du et al., 2013)
mouse-specific promoter and enhancer regions are significantly enriched in repetitive sequences (Yue et al., 2014)
only 12.6% of the murine DNA are associated with regulatory functions such as transcription factor binding, chromatin organization etc. (humans: 20%; Yue et al., 2014)
approximately 50% of the regulatory sequences have no identifiable orthologs in human (Cheng et al., 2014; Yue et al., 2014)
38.5% of mouse-specific transcription enhancers do not show activity in human ES cells (Yue et al., 2014)
mice have dozens of local gene family expansions related to reproduction, immunity and olfaction (Waterston et al., 2002)
Table 1.
Differences between men and mice.
| Category | Mice and men | Reference |
|---|---|---|
| Transposons | The mouse genome contains only 35.5% of transposon derived DNA (humans: >46%), but with 32.4% an higher amount of lineage-specific repeats (humans: 24.4%). | Waterston et al. (2002) |
| Breakpoint regions | Evolutionary breakpoint regions (intervals between segments of conserved gene order) of mice are mainly enriched for transposable elements of the SINE type (short interspersed nucleotide elements), whereas human breakpoint regions mainly contain the Alu type, a specific subtype of SINE elements. | Schibler et al. (2006) |
| Transcription | Only 22% of transcription factor footprints and 50% of transcription factor networks are conserved. | Yue et al. (2014) |
| Although the binding motifs of most sequence-specific transcription factors are conserved, the motifs for co-factors tend to be species specific. | Cheng et al. (2014) | |
| Immune system | Differences in the immune system include in the balance of leukocyte subsets, in defensins, Toll receptors, inducible NO synthase, Ig subsets, the B cell and T cell signaling pathways, cytokines and cytokine receptors, Th1/Th2 differentiation, co-stimulatory molecule expression and function, antigen-presenting function of endothelial cells, and chemokine and chemokine receptor expression. | reviewed in Mestas and Hughes (2004) |
| Physiology | Several differences in the physiology and morphology of organs have been reported recently. | e.g.,: Gharib et al. (2010), Tabata et al. (2012), Barak et al. (2013), Dolenšek et al. (2015), Schmidt et al. (2015) and Symonds et al. (2015) |
| Mice are indicated to have higher rates of reactive oxygen species production than humans, however, sufficient original evidence is missing. | Ku et al. (1993), reviewed in Finkel and Holbrook (2000) and Demetrius (2006) | |
| The fatty acid composition of the membrane is different in mice and men. | Hulbert (2005) |
The table summarizes genetic as well as physiological differences between mice and men, which may potentially affect the translation of research results between the two species. While genome studies in mice and humans showed that both mammals mainly differ in terms of gene regulation, differences in the physiology are not well characterized yet.
Table 2.
Fragile X Syndrome and Fragile X-associated Tremor/Ataxia Syndrome model mice.
| Fmr1 mouse model | MGI | Aliases | Strains | First publication | Further publications and information |
|---|---|---|---|---|---|
| Fmr1tm1Cgr | 1857169 | Fmr1 KO, Fmr1tm4Cgr, FMRP KO, fmr-tm1Cgr, FraX, FMR1- | FVB.129P-Fmr1tm1Cgr/J B6.129P2-Fmr1tm1Cgr/J FVB.129P2(B6)-Fmr1tm1Cgr/J | Bakker et al. (1994) | http://www.informatics.jax.org/reference/allele/MGI:1857169?typeFilter=Literature#myDataTable=results%3D100%26startIndex%3D0%26sort%3Dyear%26dir%3Ddesc%26typeFilter%3DLiterature |
| Fmr1tm1.1Cidz | 3808885 | Fmr1 KO2 | B6.129P2- Fmr1tm1.1Cidz/J | Mientjes et al. (2006) | http://www.informatics.jax.org/reference/allele/MGI:3808885?typeFilter=Literature |
| Fmr1tm1Cidz | 3603442 | Fmr1 CKO | Involves: 129S1/Sv* 129X1/SvJ | Koekkoek et al. (2005) | http://www.informatics.jax.org/reference/allele/MGI:3603442?typeFilter=Literature |
| Fmr1tm2Cgr | 2451086 | CGG(98) Fmr1 CGG KI Fmr1 CGG KI (C57BL/6 congenic) | B6.129P2(Cg)-Fmr1tm2Cgr/DlnJ | Bontekoe et al. (2001) | http://www.informatics.jax.org/reference/allele/MGI:2451086?typeFilter=Literature |
| Fmr1tm1Usdn | 3711215 | CGG KI, Fmr1PM | B6.129S6(Cg)-Fmr1tm1Usdn | Entezam et al. (2007) | http://www.informatics.jax.org/reference/allele/MGI:3711215?typeFilter=Literature |
| Fmr1tm1Rbd | 3840615 | Fmr1I304N Fmr1tm1(I304N)Drnl Fmr1tm1(I304N)Rbd | FVB.129-Fmr1tm1Rbd/J B6.129-Fmr1tm1Rbd/J | Zang et al. (2009) | http://www.informatics.jax.org/reference/allele/MGI:3840615?typeFilter=Literature |
| Tg(Fmr1-EGFP)HP76Gsat | 4847053 | B6;FVB-Tg(Fmr1-EGFP)HP76Gsat/Mmucd | - | - also see: http://www.informatics.jax.org/reference/allele/MGI:4847053?typeFilter=Literature |
The table shows the mouse models most commonly used in FMR1 research. Embryonic stem cell lines are not included. The majority of studies (>260) has been performed with the first mouse model, the Fmr1 KO mouse (Bakker et al., 1994), which is characterized by a complete loss of FMRP and expression of abnormal mRNA (Yan et al., 2004; Mientjes et al., 2006). To investigate a potential effect of the aberrant mRNA, another model, the Fmr1 KO2 mouse was generated in 2006 (Mientjes et al., 2006), which does not express any mRNA, but no significant differences between the two animal models were found (Gaudissard et al., 2017). By now, the KO2 animals have been employed in more than 20 studies. Along with the Fmr1 KO2 mouse model, a conditional FXS mouse was developed as well (Fmr1 CKO), but thus far, the model has only been employed in approximately 10 studies. The knock-in animals have mostly achieved attention as models of FXTAS. In addition, one model of the I304N mutation (Zang et al., 2009), which affects mRNA binding by the KH domain, has been generated. Model mice are available to researchers with generous support from the FRAXA Research Foundation: https://www.fraxa.org/fragile-x-mutant-mouse-facility/.
Taken together, these studies show that although men and mice share many features, they differ in a variety of aspects when more detailed data are included (Figure 3). It is now widely accepted that the characteristics of mice and men mostly arise from alterations in the mechanisms controlling gene expression, in particular from variations and polymorphisms of cis-elements (reviewed in Wittkopp and Kalay, 2011).
Figure 3.
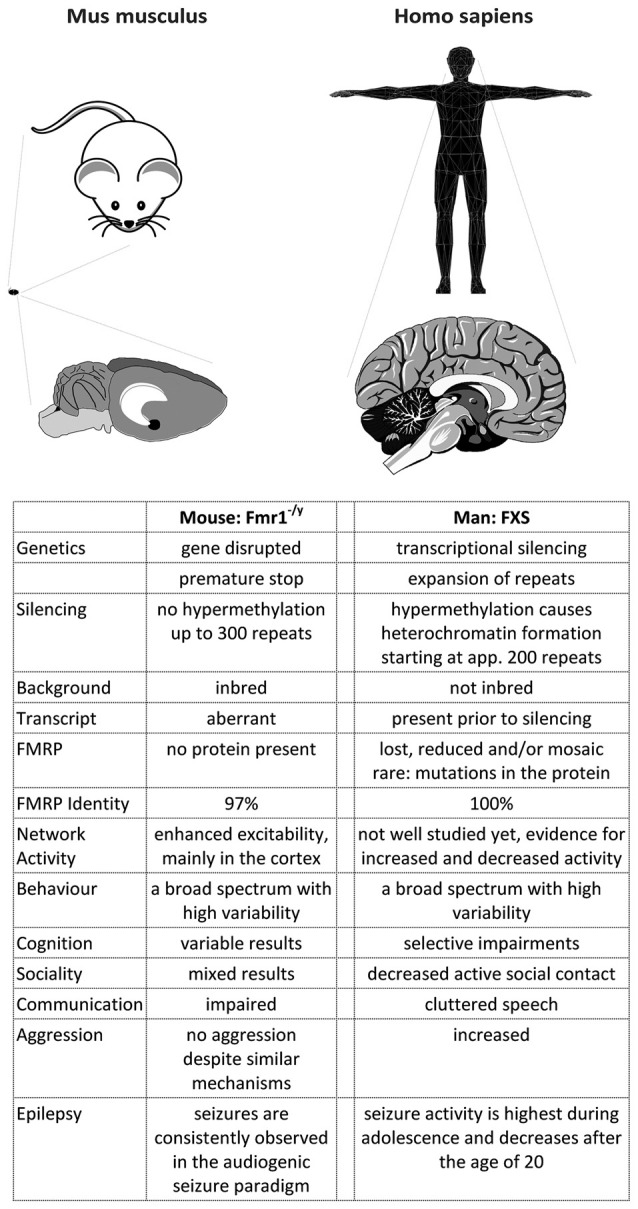
A comparison of FXS in mice and men. The figure summarizes some major differences between FXS model mice and patients. Most differences arise from the development of the cortex in primates, which caused a rewiring inside the cortex as well as between the cortex and the hippocampus (and potentially other brain regions). Consequently, the behavioral phenotype observed in men and mice does not match very well, although the mouse model recapitulates many biochemical aspects of the disease. In addition, the complex genetics of the disease cannot be modeled in mice, probably due to a more relaxed gene expression control in this species.
Genetics of the FXS Model Mouse
The fundamental difference between commonly used FXS model mice (Fmr1−/y mice8) and patients is that mice never have any FMRP, beginning with their very first moment of existence, whereas in patients, the gene is active at least until the 10th week of gestation (Devys et al., 1992; Sutcliffe et al., 1992; Suzumori et al., 1993; Iida et al., 1994; Willemsen et al., 2002). Moreover, patients display mosaic expression patterns (Kaufmann et al., 1999; Dyer-Friedman et al., 2002; Loesch et al., 2003, 2004; Govaerts et al., 2007; Pretto et al., 2014; Basuta et al., 2015) as well as residual full-length mRNA (Tassone et al., 2001), but mice don’t.
In order to overcome this dissatisfying situation, several CGG repeat knock-in mice were made to mimic the genotype found in humans (e.g., Bontekoe et al., 1997, 2001; Lavedan et al., 1997, 1998; Baskaran et al., 2002; Peier and Nelson, 2002; Fleming et al., 2003; Brouwer et al., 2007; Entezam et al., 2007; Alam et al., 2010). Similar to human pre-mutation carriers (Tassone et al., 2000a,b; Kenneson et al., 2001; Primerano et al., 2002; Ludwig et al., 2014), the knock-in mice display a direct correlation between the mRNA transcript level and the repeat length as well as an indirect correlation between the repeat length and the protein level, showing significant variation between individual animals (Ludwig et al., 2014).
In terms of pathological features, the knock-in mice reflect several biochemical, histological and behavioral symptoms of FXTAS patients (Willemsen et al., 2003; Van Dam et al., 2005; Entezam et al., 2007; Hunsaker et al., 2010, 2011; Wenzel et al., 2010; Cunningham et al., 2011) and pre-mutation transcripts were found toxic in mice (Handa et al., 2005; Hashem et al., 2009; Chen et al., 2010; Hukema et al., 2014). However, no explicit data on behavioral deficits or toxic effects were reported for the full-mutation situation (200–350 repeats; Entezam et al., 2007; Hunsaker et al., 2010, 2011; Ludwig et al., 2014) in specific, thus suggesting that contrary to humans, 350 repeats still represent a pre-mutation situation in mice.
Although some instability has been recognized in mice harboring pre-mutation alleles of about 100–260 repeats (Bontekoe et al., 2001; Peier and Nelson, 2002; Brouwer et al., 2007; Entezam et al., 2007), and based on these models, transacting mechanisms such as mismatch repair and transcript coupled repair were identified to support instability of the gene in mice (Zhao and Usdin, 2014; Zhao X. N. et al., 2015), instability is apparently not a major phenotype of the mouse (Bontekoe et al., 1997; Lavedan et al., 1997, 1998; Peier and Nelson, 2002; Fleming et al., 2003).
This situation first changed, when Baskaran and colleagues introduced the SV40 origin of replication along with their transcript to the gene (Baskaran et al., 2002) in order to exclude nucleosome formation. The transgene is driving the expression of FMR1 Exon 1 by the SV40 early promoter encoded in the SV40 origin, which excludes chromatin formation at the transgenic locus. Exon 1 contains 26 copies of the CGG repeat together with the translational FMR1 start codon. As a result, the transgene obtained an open chromatin structure compared to the normally nucleosome-flanked CGG repeats seen in other mouse models (Datta et al., 2011) and is therefore more prone to instability (cp. Oostra, 1998). Thereby, Baskaran and colleagues achieved expansions from 26 to 350 repeats within three generations only; however, the DNA remained unmethylated (Alam et al., 2010). Sadly, these results are in line with two more recent studies which also achieved significant expansions (120–230 repeats; Brouwer et al., 2007; Entezam et al., 2007), but no methylation and no inactivation of Fmr1. Given that the expression of the full-mutation mRNA did apparently not cause unusual severe FXTAS or even FXS phenotypes, and given that the full-mutation alleles were neither hypermethylated nor inactivated or significantly unstable, these data support the idea that in mice, 200–350 repeats still represent a pre-mutation situation.
Taken together, these studies further suggest that the mechanisms leading to the inactivation of FMR1 might be different in mice and humans (cp. the section “A Question of Secondary Structures?”). Indeed, Matsuo and colleagues found that CpG islands of men and mice have different properties: comparing 23 orthologous genes, they discovered that mice almost always have less pronounced islands, or even none at all. The authors speculate that the CpG islands in mice might have eroded during evolution as an adaption to the mouse’s small body mass and short life-span by allowing for a more relaxed control of gene activity (Matsuo et al., 1993). Their study is in line with an earlier report that also detected low numbers of CpG islands in mice (Aïssani and Bernardi, 1991), thus implying that mice may simply not have the capabilities to methylate genes the same way humans do, causing fully mutated Fmr1 to remain active even if humanized transgenes are employed (e.g., Lavedan et al., 1998). This hypothesis is supported by comparative in vivo footprinting analyses across several human and mouse CpG islands that demonstrated striking differences in the protein-DNA interactions of both species (Cuadrado et al., 2001, reviewed in Antequera, 2003). Furthermore, Fu and colleagues found that the murine and the human DNA methyltransferase DNMT1, which is responsible for the maintenance of methylation patterns by preferentially adding methyl groups to hemi-methylated CpG sites, differ in their processivity (Fu et al., 2012). In particular, they demonstrate a high level of processivity for human DNMT1 at FMR1, which is possibly not achieved by the murine enzyme as it has much longer non-association tracts in vivo.
Phenotypes of the Fmr1−/y Mouse
FMRP Functions to Regulate the mRNA Metabolism
Studying FMRP functions in humans is challenging. It is therefore no surprise, that most of the corresponding knowledge we acquired is derived from mouse models. However, recent advances in stem cell research contributed significantly to our understanding of the disease.
In healthy individuals, FMRP is widely expressed, yet most abundant in testes and brain, where it is present at particular high levels throughout the cerebral cortex, the hippocampus and the Purkinje cell layer as well as the granular layer of the cerebellum (Devys et al., 1993; Hinds et al., 1993; Bakker et al., 2000, also see http://mouse.brain-map.org/gene/show/14042 and http://www.gensat.org/GeneProgressTracker.jsp?gensatGeneID=339). FMRP has been detected in glial and neuronal cells (Wang et al., 2004; Gholizadeh et al., 2015), but its special importance in synaptic signaling has drawn most attention on its function in neurons. Here, FMRP is primarily located in the cytosol and the nucleus (Feng et al., 1997), but it has also been found along dendrites, axons and at synaptic sites (Weiler et al., 1997; Greenough et al., 2001; Antar et al., 2006; Akins et al., 2017). Indeed, FMRP travels between these locations through microtubules (Feng et al., 1997; Antar et al., 2005).
The main function of FMRP is to regulate the mRNA metabolism. Interacting with five different RNA-motifs (U-Pentameres, Kissing complex, SosLip, G-quartets, G-rich regions), the protein may associate with a diversity of mRNAs, approximately 4% of all mRNAs in the mammalian brain (Brown et al., 2001; Miyashiro et al., 2003; Darnell et al., 2011). Detailed biochemical studies revealed that thereby, FMRP is able to regulate not only mRNA transport (Dictenberg et al., 2008; Estes et al., 2008) and stability (Bagni and Greenough, 2005; De Rubeis and Bagni, 2010), but also mRNA translation (Ceman et al., 2003; Zalfa et al., 2003; Bechara et al., 2009). Furthermore, FMRP was found to influence the microRNA-pathway, thus gaining further control on the expression of its target proteins (reviewed in Kenny and Ceman, 2016).
Inside the nucleus, FMRP localizes to active transcription sites, where it binds to nascent mRNA (Eberhart et al., 1996; Kim et al., 2009) and may even take action in alternative splicing, since G-quartets present in the mRNA of FMRP itself were found to function as exonic splicing enhancers (Didiot et al., 2008). Studies of the transcription and splicing machinery actually revealed brain-region as well as cell type specific alterations in Fmr1−/y mice (Derlig et al., 2013) and showed that loss of FMRP results in aberrant transcriptional regulation (Korb et al., 2017). Furthermore, FMRP was found to bind to DNA and to function in DNA damage response (Alpatov et al., 2014) as well as in Heterochromatin organization (Tan et al., 2016). These findings suggest that FMRP may control every step of protein expression from DNA organization to translation.
FXS and Group 1 Metabotropic Glutamate Receptors
On the other hand, FMRP itself turned out to be under control of mGluR1/59 signaling cascades (Narayanan et al., 2008), hence allowing for an activity dependent regulation of the mRNA metabolism in various aspects by FMRP. Detailed studies on the function of mGluRs in FXS have lead to the advance of the mGluR-Theory (Huber et al., 2002; Bear et al., 2004; Dolen et al., 2007; Nakamoto et al., 2007): the theory states that FMRP normally acts as a repressor of mRNA translation downstream of group 1 mGluRs, which is released after mGluR activation and thereby induces the translation of proteins required for the expression of LTD. Hence, in the absence of FMRP, persistent and mGluR stimulation independent synthesis of LTD-proteins causes ongoing AMPAR10 internalization. The theory further posits that exaggerated mGluR-signaling, perhaps as a consequence of malfunctioning feedback inhibition, is causing many of the symptoms observed in FXS.
There is indeed good evidence for this theory: the pharmacological down-regulation of mGluR5 signaling has been shown to improve a variety of typical symptoms in Fmr1−/y mice, including aberrant neuronal morphology, hyperactivity, social behavior, seizure susceptibility and learning and memory (Yan et al., 2005; de Vrij et al., 2008; Levenga et al., 2011; Su et al., 2011; Michalon et al., 2012; Vinueza Veloz et al., 2012; Gantois et al., 2013; de Esch et al., 2015) and so has a genetic reduction of group 1 mGluRs (Dolen et al., 2007; de Esch et al., 2015). One group reported some contradictory findings (Thomas et al., 2011), but the promise of the results prompted clinical trials with mGluR antagonists such as AFQ056 (Novartis) and RO4917523 (Roche) to down-regulate the exaggerated mGluR signaling. Although patients treated with these substances were initially reported to experience some behavioral improvements (Jacquemont et al., 2011), all trials were discontinued during phases IIb/III since the studies did not show any significant improvements in abnormal behaviors compared to placebo (reviewed in Scharf et al., 2015). It has been speculated that cross-reactions with other drugs used to treat FXS patients, the long time of perpetuation in adult patients, irreversible changes during early brain development and difficulties in the outcome measures might have caused the failure, but the underlying reasons have remained unclear.
Remarkably, several targets of FMRP belong to the two major mGluR-signaling cascades controlling the expression of related proteins, the ERK11 - and the mTOR12 - pathway: ERK, PI3K13, PIKE14, GSK315 and mTOR are target mRNAs of FMRP (Darnell et al., 2011; Ascano et al., 2012). Both signaling pathways turned out to be exaggerated not only in the hippocampus of Fmr1−/y mice (ERK pathway: Hou et al., 2006; Michalon et al., 2012; mTOR pathway: Sharma et al., 2010; Liu Z. H. et al., 2012; Bhattacharya et al., 2016; Choi et al., 2016), but also in humans (Weng et al., 2008; Hoeffer et al., 2012; Wang X. et al., 2012; Kumari et al., 2014; Pellerin et al., 2016).
There has been some dispute about the status of ERK activation in FXS though (mice: Hu et al., 2008; Gross et al., 2010; Osterweil et al., 2010; patients: Yrigollen et al., 2016), but pathway-specific inhibitors of ERK-signaling constantly rescued characteristic deficits in FXS models (Chuang et al., 2005; Osterweil et al., 2010; Wang X. et al., 2012), thus supporting the idea that enhanced mGluR1/5 cascades are causative for some symptoms of the disease. Further studies found that inhibition of ERK-signaling with Metformin (Gantois et al., 2017) or Lovastatin (Osterweil et al., 2013) indeed ameliorates many deficits in Fmr1−/y mice. Strikingly though, mTOR inhibition with Rapamycin turned out to induce adverse effects on sleep and social behavior in both, control and Fmr1−/y mice (Saré et al., 2018), although positive effects of Rapamycin were reported for the BTBR T+Itpr3tf/J mouse model of autism (Burket et al., 2014). In fact, some data even suggest that mTOR inhibition with Rapamycin might cause neurodegeneration (Lin et al., 2013). The hopes are therefore now on clinical trials with Lovastatin (Caku et al., 2014; Pellerin et al., 2016) and Metformin (Dy et al., 2018).
Brain Region Specific Mechanisms in FXS
All the above mentioned strategies to amend FXS suffer from the same difficulty though; contrary to drugs, the outlined mechanisms only apply to the hippocampus. There is evidence that the signaling mechanisms of the cortical and hippocampal networks are differentially affected by the loss of FMRP. In cortical synaptosomes of Fmr1−/y mice for example, mTOR activity was found normal (Sawicka et al., 2016), whereas in the hippocampus, mTOR signaling is exaggerated (Sharma et al., 2010; Liu Z. H. et al., 2012; Bhattacharya et al., 2016; Choi et al., 2016). Cortical ERK was demonstrated to be erroneously deactivated following mGluR stimulation in Fmr1−/y mice (Kim et al., 2008), whereas it was illustrated to be normal (Osterweil et al., 2010) or even over-activated in hippocampal tissue (Hou et al., 2006; Michalon et al., 2012). Remarkably, the study of Sawicka and colleagues showed that ERK signaling in the neocortex of Fmr1−/y mice is impinging on ribosomal protein S6, which usually receives input from mTOR, though in this study, cortical ERK activity was found exaggerated.
The data on patients are mostly derived from fibroblasts (Kumari et al., 2014; Yrigollen et al., 2016) or thrombocytes (Weng et al., 2008; Pellerin et al., 2016), making conclusions on the characteristics of specific brain regions difficult. Using post-mortem tissue, one study detected no differences in ERK activation in the frontal lobe between FXS patients and controls (Hoeffer et al., 2012), while another one found increased levels of phosphorylated ERK in the frontal cortex of patients (Wang X. et al., 2012). Despite the unclear status of ERK activation in the cortex, these studies suggest that mGluR1/5 signaling pathways are functioning differently in the cortex and the hippocampus. In line with this notion, a recent study of mTOR activity and exercise demonstrated that the activation status of mTOR is depending on the brain region, the cell type (neuron or glia) and the type of exercise (sedentary, voluntary or forced; Lloyd et al., 2017).
Long term potentiation
Further support for the relevance of brain region specific mechanisms in FXS comes from a variety of studies on synaptic plasticity. Synaptic plasticity is mostly investigated by the induction of LTP16 or LTD17, two paradigms which are considered cellular models of learning and memory (reviewed in Kandel, 2001; Bliss et al., 2003; Neves et al., 2008). Both, LTP and LTD, ultimately depend on the modulation of synaptic signaling and have been studied intensively in Fmr1−/y mice using manifold induction protocols (please see Table 3 for more details).
Table 3.
LTP protocols used in different studies.
| Study | Stimulation | Recording | Study | Stimulation | Recording |
|---|---|---|---|---|---|
| Auerbach and Bear (2010) | Hippocampus: 1 s 100 Hz tetanus stimulation | Field recordings | Bostrom et al. (2015) | Hippocampus, CA1 and dentate gyrus: 4 trains of 50 pulses at 100 Hz, 30 s apart | Field recordings |
| Chen et al. (2014) | Anterior cingulate cortex: five trains of bursts with four pulses at 100 Hz and 200 ms interval; repeated five times at intervals of 10 s | MED64 probe (array) | Godfraind et al. (1996) | Hippocampus: data not available | Field recordings |
| Harlow et al. (2010) | Somatosensory cortex: pairing of 100 stimuli at 1 Hz with postsynaptic depolarization to 0 mV | Whole cell recordings | Hayashi et al. (2007) | Cortex: eight bursts (each four pulses at 100 Hz) every 200 ms | Field recordings |
| Hu et al. (2008) | Hippocampus: pairing of 200 pulses at 2 Hz at −5 mV within 5 min after formation of whole-cell configuration | Whole-cell recordings | Koga et al. (2015) | Anterior cingulate cortex: induction of pre-LTP with repetitive low-frequency stimulation at 2 Hz for 2 min | Whole-cell recordings (neurons), multielectrode array (slices) |
| Larson et al. (2005) | Anterior piriform cortex: 10 bursts at 100 Hz with four pulses repeated in 200 ms intervals, hippocampus: two pathways, one by five theta bursts, the other by 10 theta bursts | Field recordings | Lee et al. (2011) | Hippocampus: five theta burst stimuli | Field recording |
| Li et al. (2002) | Hippocampus: single tetanic train of 100 Hz, 1 s duration at maximal intensity, cortex: three tetanic trains of 200 Hz, 1 s with an interval of 10 min | Field recordings | Martin H. G. S. et al. (2016) | Prefrontal Cortex: five trains of burst with four pulses at 100 Hz and 200 ms interval, repeated four times at intervals of 10 s | Whole-cell recordings |
| Padmashri et al. (2013) | Motor cortex: chemical LTP via bath application of bicuculline (6.3 μm) for 3 min, followed by forskolin (50 μm) and the phosphodiesterase inhibitor rolipram (0.1 μm) in Mg2+-free ACSF for 15 min | Field recordings | Paradee et al. (1999) | Hippocampus: stimulation 1x every 30 s for 20 min for baseline response, followed by induction of L-LTP by three trains (10 bursts at 5 Hz, each burst consisting of a 40 ms burst at 100 Hz) of theta bursts, 1 min apart | Field recordings |
| Shang et al. (2009) | Hippocampus: stimulation intensity adjusted so that a half-maximal fEPSP was elicited | Field recording, whole-cell recording | Wilson and Cox (2007) | Neocortex: three trains of 100 Hz, 1-s duration at 5 min intervals | Field recordings |
| Xu et al. (2012a) | Prefrontal cortex: 80 pulses at 2 Hz, and then paired with postsynaptic depolarization at + 30 mV | Whole-cell recordings | Xu et al. (2012b) | Anterior cingulate cortex: 80 pulses at 2 Hz paired with postsynaptic depolarization at +30 mV | Whole-cell recordings |
| Yang et al. (2014) | Auditory cortex: three repetitions of 100-Hz stimulation of 1-s duration. | Field recordings | Zhang et al. (2009) | Hippocampus: L-LTP induced by four 1 s trains of 100 Hz with a 5 min interval | Field recordings |
| Zhao et al. (2005) | Anterior cingulate cortex: 80 pulses at 2 Hz paired with postsynaptic depolarization at +30 mV | Whole-cell recordings |
Literature providing only general information is not included. The data illustrates the variety of induction protocols used to study LTP.
While some protocols have led to the discovery of disturbances in certain forms and aspects of hippocampal LTP (Hu et al., 2008; Shang et al., 2009; Lee et al., 2011), most examinations found the expression of hippocampal LTP in Fmr1−/y mice to be normal (Godfraind et al., 1996; Paradee et al., 1999; Li et al., 2002; Larson et al., 2005; Zhang et al., 2009; Auerbach and Bear, 2010). Two of these studies also investigated cortical LTP: while they observed no abnormalities in hippocampal LTP, both detected significantly impaired LTP in the cortex of Fmr1−/y mice (Li et al., 2002; Larson et al., 2005). The result is line with several studies demonstrating defective LTP in different regions of the cortex (Zhao et al., 2005; Hayashi et al., 2007; Wilson and Cox, 2007; Harlow et al., 2010; Xu et al., 2012b; Padmashri et al., 2013; Yang et al., 2014; Koga et al., 2015).
LTP includes two distinct phases, an early phase (E-LTP), which does not require protein synthesis, and a late phase (L-LTP), which depends on protein synthesis and gene expression (Frey et al., 1993; Abel et al., 1997, reviewed in Kandel, 2001, 2009). While L-LTP is unaffected in the hippocampus of Fmr1−/y mice (Paradee et al., 1999; Zhang et al., 2009), it is blocked in the cingulate cortex (Chen et al., 2014). Since pharmacological inhibition of mGluR5 or GSK3 rescued L-LTP in the cingulate cortex of Fmr1−/y mice, these results show that exaggerated mGluR signaling is involved. Indeed, two other studies also reported rescues of cortical LTP based on mGluR1/5 antagonists (Xu et al., 2012a; Martin H. G. S. et al., 2016), but the effects of mGluR5 or GSK3 inhibition on (L-)LTP in the hippocampus were never investigated although hippocampal L-LTP is known to depend on mGluR1/5 activation (Riedel and Reymann, 1996; Francesconi et al., 2004; Neyman and Manahan-Vaughan, 2008; Fan, 2013).
The differences between the hippocampus and the cortex are further emphasized by the fact that age-related deficits in LTP were discovered specifically in the cortex (Larson et al., 2005; Martin H. G. S. et al., 2016). While Fmr1−/y mice older than 6 months displayed significant defects in the expression of cortical LTP, the mice never displayed any impairment in hippocampal LTP. In fact, Bostrom et al. (2015) even demonstrated differences within the hippocampus itself: while the loss of FMRP caused impairments in NMDAR18-dependent LTP in the dentate gyrus, NMDAR-LTP was found normal in the CA119 region of the hippocampus.
Long term depression
The most prominent and best studied plasticity model in FXS is mGluR-LTD, a type of LTD that depends on the activation of mGluR1/5, protein synthesis and the internalization of AMPA receptors. However, while numerous studies demonstrated enhanced mGluR-LTD in the hippocampus of Fmr1−/y mice (Huber et al., 2002; Hou et al., 2006; Nosyreva and Huber, 2006; Volk et al., 2007; Park et al., 2008; Ronesi and Huber, 2008; Zhang et al., 2009; Auerbach and Bear, 2010; Choi et al., 2011; Bhattacharya et al., 2012; Michalon et al., 2012; Niere et al., 2012; Costa et al., 2015; Toft et al., 2016; Thomson et al., 2017), nobody studied mGluR-LTD in the cortex yet. There is evidence though that cortical mGluR-LTD is existing (reviewed in Kang and Kaang, 2016). Using a protocol to induce spike-time-dependent plasticity (STD-LTP or STD-LTD) in the neocortex of Fmr1−/y mice, Desai and colleagues found no impairment in LTD, but a significant reduction in LTP (Desai et al., 2006). Experiments with MPEP20, a mGluR5 antagonist, revealed that cortical STD-LTP is not depending on mGluR5 activation, whereas cortical STD-LTD is. Remarkably, the application of anisomycin, an inhibitor of protein synthesis, revealed that cortical STD-LTD does not require protein synthesis, thus suggesting that FMRP is not necessary for cortical STD-LTD despite the dependence on mGluR5. Sadly though, STD-LTD has not been investigated in the hippocampus yet.
It is worth noting that the biological relevance of mGluR-LTD has recently been questioned, arguing that mGluR-LTD in the absence of previous LTP is artificial (discussed in Jones, 2017). Nonetheless, since more than 15 years of mGluR-LTD research in Fmr1−/y mice did not provide any evidence for abnormal mGluR-LTD in the cortex, it seems likely that the mechanisms underlying this form of plasticity differ among brain regions.
Keeping the balance
FXS is associated with a vast misregulation of protein expression, not only in the context of mGluR signaling, but also with respect to proteins regulating other aspects of neuronal excitability such as Calmodulin or Neuroligin for instance (Liao et al., 2008; Matic et al., 2014; Kalinowska et al., 2015; Tang et al., 2015). Although it is not clear yet whether abnormal mGluR-LTD directly impacts on the balance of excitatory and inhibitory activity in neuronal networks (E/I balance), mGluR signaling is able to alter the excitability of neurons by increasing the intrinsic conductance (Bianchi et al., 2009; Tang and Alger, 2015). Furthermore, FMRP itself may bind to ion channels such as Calcium, Slack21 and BK22 channels, thereby providing an additional level of FMRP mediated control (Brown et al., 2010; Deng et al., 2013; Ferron et al., 2014).
Deviations in the balance of excitation and inhibition have been associated with seizure activity, hypersensitivity and cognitive deficits in several ASDs and animal models (reviewed in Frye et al., 2016; Uzunova et al., 2016; Lee et al., 2017; e.g., Orekhova et al., 2008; Tebartz van Elst et al., 2014; Robertson et al., 2016), including Fmr1−/y mice (e.g., D’Hulst et al., 2006; Zhong et al., 2009; Dahlhaus and El-Husseini, 2010; Aguilar-Valles et al., 2015; Deng and Klyachko, 2016). Using these animals, in particular neocortical circuits have been shown to experience enhanced excitation (Gibson et al., 2008; Goncalves et al., 2013; Patel et al., 2013; Zhang Y. et al., 2014; Westmark et al., 2016), partially due to inhibitory deficits (Selby et al., 2007) and potentially supported by inhibitory dysfunctions in the cortico-hippocampal pathway and inhibitory defects in feed-forward circuits (Wahlstrom-Helgren and Klyachko, 2015).
Indeed, not only glutamatergic signaling has been demonstrated to be altered in Fmr1−/y mice, but also gabaergic and dopaminergic mechanisms have been found malfunctioning. Studies showed that Fmr1−/y mice experience diminished GABAa/b23 receptor expression, reduced GABA release, decreased dopamine receptor expression and malfunctioning interneurons (D’Hulst et al., 2006; Selby et al., 2007; Pacey et al., 2011b; Paluszkiewicz et al., 2011; Henderson et al., 2012; Heulens et al., 2012; Patel et al., 2013; Paul et al., 2013; Berzhanskaya et al., 2016a; Kang et al., 2017). Deficiencies in inhibitory conductance are therefore characteristic to many circuits of the murine FXS brain including circuits of the striatum, amygdala, hippocampus, subiculum and the somatosensory as well as the prefrontal cortex (Centonze et al., 2008; Curia et al., 2009; Olmos-Serrano et al., 2010; Paluszkiewicz et al., 2011; Vislay et al., 2013; Martin et al., 2014; Sabanov et al., 2016). In addition, the loss of interactions between FMRP and BK channels causes uncontrolled Glutamate release, altered action potential waveforms and exaggerated excitability (Zhang Y. et al., 2014; Myrick et al., 2015; Deng and Klyachko, 2016).
Recent research indicates that the alterations in the E/I balance may include brain region and circuit specific mechanisms. For instance, while dendrites of hippocampal neurons from Fmr1−/y mice display increased HCN1-channel24 expression and reduced input resistance (Brager et al., 2012), dendrites of cortical layer 5 neurons show the opposite (Zhang Y. et al., 2014). The intrinsic membrane excitability of cortical layer 4 excitatory neurons is exaggerated (Gibson et al., 2008), while that of excitatory hippocampal neurons is normal (Deng et al., 2013; Luque et al., 2017). Hippocampal neurons demonstrate significantly longer action potential durations and higher firing frequencies in the absence of FMRP than under normal conditions (Luque et al., 2017), whereas layer 2/3 neurons in the prefontral cortex present significantly narrower and taller action potentials in Fmr1−/y mice than in their wildtype litter mates (Routh et al., 2017). Although both alterations indicate enhanced excitability, the sharpened action potentials observed the cortex of Fmr1−/y mice are in contrast with the broadened action potentials seen in the hippocampus. Since two studies even demonstrated increased inhibition early in development (Berzhanskaya et al., 2016b; Truszkowski et al., 2016), the data show that the alterations in neuronal activity depend on the specific circuit, aspect and age.
Despite the high complexity of the system, several studies were able to rescue the aberrant neuronal activity based on restorations of mGluR1/5 signaling (Meredith et al., 2011; Ronesi et al., 2012; Westmark et al., 2016; Aloisi et al., 2017), GABA signaling (Olmos-Serrano et al., 2010, 2011; Martin B. S. et al., 2016; Kang et al., 2017) or ion channel function (Zhang Y. et al., 2014; Deng and Klyachko, 2016; Aloisi et al., 2017). In doing so, phenotypes such as epileptiform activity (Ronesi et al., 2012; Zhang Y. et al., 2014; Deng and Klyachko, 2016; Westmark et al., 2016), hyperactivity (Olmos-Serrano et al., 2011; Ronesi et al., 2012) and hypersensitivity (Zhang Y. et al., 2014) were normalized. A few studies have also investigated network oscillations in FXS model animals (Gibson et al., 2008; Goncalves et al., 2013; Rotschafer and Razak, 2013; Radwan et al., 2016; Westmark et al., 2016; Berzhanskaya et al., 2017). In these experiments, cortical neurons displayed increased synchrony in their activity as well as a threefold higher firing rate during Up states (Gibson et al., 2008; Goncalves et al., 2013; Westmark et al., 2016), increased high-frequency as well as reduced low-frequency power during rest (Berzhanskaya et al., 2017) and elevated responses to auditory stimuli (Rotschafer and Razak, 2013).
The findings support the theory that neuronal hyperexcitability is a leading cause for many symptoms of FXS and fit well with the Intense World Theory of Autism (reviewed in Markram and Markram, 2010), which posits that hyperactive micro-networks cause many of the cognitive deficits characteristic to ASDs, in particular hypersensitivity, hyperattention, hyperemotionality and seizure susceptibility. Although the studies of oscillatory dynamics in FXS patients currently available mostly confirm the idea of imbalanced circuit activity (Castrén et al., 2003; Dalton et al., 2008; Holsen et al., 2008; Van der Molen and Van der Molen, 2013; Van der Molen et al., 2014; Wang et al., 2017), not all of them are in favor of the theory: two studies detected decreased activity, one in prefrontal regions and one in the fusiform gyrus (Dalton et al., 2008; Holsen et al., 2008), while a third study found intracortical inhibition in FXS patients to be normal (Oberman et al., 2010).
From Mice to Men
Literature Summary
Most rescues reported from Fmr1−/y mice are based on investigations of the hippocampus (Table 4). Some studies included data on further brain regions or transferred approaches to cortical regions, analyzing different aspects of mGluR signaling for example; however, only 4 studies were found that focussed on the cortex in terms of their strategy and their experiments. No studies could be identified that are reporting behavioral rescues based on mechanisms characteristic to the amygdala, cerebellum, striatum or any other brain region in specific, although the available data argue for different deficits in different brain regions (see for instance Chen et al., 2014; Bostrom et al., 2015; Sawicka et al., 2016; Lloyd et al., 2017) and despite the fact that rescues of neuronal activity have been reported for the amygdala (Olmos-Serrano et al., 2010, 2011; Suvrathan et al., 2010; Martin B. S. et al., 2016). These findings show that there is a significant imbalance between the current hippocampus centered investigations and the multifarious mechanisms found in the brain of wildtype as well as FXS model animals.
Table 4.
Brain-region bias in FXS research.
| Rescue of behavior | Rescue of neuronal function only | |
|---|---|---|
| Hippocampus based strategies and/or studies | Yan et al. (2005), Dolen et al. (2007), de Vrij et al. (2008), Gross et al. (2010, 2015a), Levenga et al. (2011), Westmark et al. (2011), Bhattacharya et al. (2012), Goebel-Goody et al. (2012), Guo et al. (2012), Liu Z. H. et al. (2012), Michalon et al. (2012), Ronesi et al. (2012), Vinueza Veloz et al. (2012), Chen et al. (2013), Gantois et al. (2013), Osterweil et al. (2013), Udagawa et al. (2013), Boda et al. (2014), Franklin et al. (2014), Hébert et al. (2014), Sidhu et al. (2014), Sun et al. (2014, 2016), Tian et al. (2015), de Esch et al. (2015), Aloisi et al. (2017), Martinez and Tejada-Simon (2017), Pardo et al. (2017) and Thomson et al. (2017) total: 30 | Lauterborn et al. (2007), Nakamoto et al. (2007), Zeier et al. (2009), Choi et al. (2011), Gross et al. (2011), Meredith et al. (2011), Costa et al. (2012, 2015), Deng et al. (2013), Bostrom et al. (2015), Choi C. H. et al. (2015), Ghilan et al. (2015), Tang and Alger (2015), Zhao W. et al. (2015), Deng and Klyachko (2016), Toft et al. (2016), Westmark et al. (2016) and Yau et al. (2016) total: 18 |
| Studies including data on several brain regions | Yuskaitis et al. (2010), Liu et al. (2011), Pacey et al. (2011a), Ronesi et al. (2012), Xu et al. (2012a), Gkogkas et al. (2014), Lim et al. (2014), Braat et al. (2015), Bhattacharya et al. (2016) and Li et al. (2016) total: 10 | |
| Cortex based strategies and/or studies | Hayashi et al. (2007), Dolan et al. (2013), Gross et al. (2015c) and Yang et al. (2015) total: 4 | Henderson et al. (2012), Kim et al. (2013), Chen et al. (2014) and Lovelace et al. (2016), Westmark et al. (2016) total: 5 |
| Amygdala based strategies and/or studies | none | Olmos-Serrano et al. (2010, 2011), Suvrathan et al. (2010) and Martin B. S. et al. (2016) total: 4 |
| Brain regions not specified/studied | Veeraragavan et al. (2011), Heulens et al. (2012), Gholizadeh et al. (2014) and Pietropaolo et al. (2014) total number: 4 |
The table lists all publications that were identified on pubmed or PMC in October 2017, and found to report at least functional rescues of symptoms related to FXS using murine model systems. Studies reporting only morphological rescues were not included. The data show that there is a strong bias toward investigations of hippocampal functions in the literature.
The Cortex, the Hippocampus and FXS
Problems in translating findings from mice to men are a common phenomenon in brain research. A major difficulty arises from the development of the cerebral cortex in primates and in particular in humans. Recent research revealed that the cognitive performance of vertebrates is best reflected by a combination of the number of neurons, neuron density and axonal conduction velocity in the cortex (reviewed in Dicke and Roth, 2016). In this regard, mice are not well set, since their cerebral cortex exhibits only a relatively low density of neurons: if mice would have a brain the size of a human, their cerebral cortex would contain 2 billion neurons, whereas the human cerebral cortex does in fact have 16 billion (cp. Herculano-Houzel, 2009). However, neuron density is not the only disadvantage mice are confronted with:
the neocortex constitutes 80% of the human brain (Azevedo et al., 2009), but only 40% of a mouse brain (reviewed in Herculano-Houzel, 2009)
while mice have about 20 different cortical areas, humans have more than 200 (Kaas, 1989, 2011; Changizi and Shimojo, 2005)
most cortical areas in mice are related to sensory and motor functions, whereas the majority of the human areas function in association (reviewed in Buckner and Krienen, 2013)
some parts of the human neocortex are specifically enlarged compared to the rest of the neocortex:
-
-
the prefrontal cortex and area 10 (Semendeferi et al., 2002, 2011), which is important to higher cognitive functions,
-
-
the insula, which usually functions in sensory information processing, but has new areas in humans that are functioning in empathy and social awareness (reviewed in Keysers et al., 2010) and
-
-
the posterior parietal cortex (reviewed in Orban et al., 2006), which is important to planning, imitation and the highly skilled use of tools.
by contrast, the primary sensory and motor areas have maintained their relative sizes during the evolution from mice to men (Hill et al., 2010; Preuss, 2011)
several cell types found in the human brain do not exist in mice (reviewed in Buckner and Krienen, 2013).
In line with these findings, rodents perform relatively poor in behavioral tasks when compared to monkeys possessing similar sized brains (e.g., capybara (Macdonald, 1981) and capuchin monkey (Anderson et al., 2013; De Moraes et al., 2014; Takahashi M. et al., 2015)), thus suggesting that primate brains have properties, which are significantly different from those of rodents.
This notion is emphasized by an elegant study of Han and colleagues (Han et al., 2013), who showed that human glia cells are much more competent than murine glia cells when it comes to supporting brain functions: replacing the glia of mice with human cells, they observed that the engrafted mice were able to propagate calcium signals three times faster than allografted mice, exhibited sharply enhanced LTPs and performed excellent in cognition tests. Indeed, astrocytes are able to coordinate and modulate neural signal transmission (reviewed in Allen, 2014; Allen and Eroglu, 2017), but human astrocytes differ from their murine counterparts in that human astrocytes are larger, more complex and more diverse, have much more synaptic contacts and are more efficient in calcium signaling (Andriezen, 1893; Colombo, 1996; Colombo et al., 1997, 2000; Reisin and Colombo, 2002; Oberheim et al., 2009).
Remarkably, this is particularly true for the cerebral cortex: there are at least four morphologically distinct astrocyte classes within the primate cortex, as compared to two in rodents. The two novel classes are interlaminar astrocytes and varicose projection astrocytes (Andriezen, 1893, reviewed in Vasile et al., 2017). Varicose projection astrocytes have hitherto been observed only in cortical layers 5–6 of humans and chimpanzees, but the human cells are more complex. By contrast, interlaminar astrocytes reside in upper cortical layers and extend long processes to cortical layers 3 and 4 (Colombo, 1996; Colombo et al., 1997; Reisin and Colombo, 2002; Korzhevskii et al., 2005; Oberheim et al., 2009). Although interlaminar astrocytes are present in both, monkeys and men, humans have higher numbers of interlaminar astrocytes. Despite the fact that more than 120 years have passed since their initial description, the role of these primate-specific astrocytes is still elusive.
Nonetheless, astroglia seem to have a role in FXS: though FMRP is predominantly expressed in neurons at all ages, it is also seen in oligodendrocyte precursor cells and astrocytes. While neurons display a gradual decrease in FMRP expression during development (Davidovic et al., 2011; Bonaccorso et al., 2015), astrocytes and oligodendrocyte precursor cells mainly express FMRP during early and mid-postnatal stages of brain maturation (Wang et al., 2004; Gholizadeh et al., 2015), thus suggesting a role for glia and FMRP in development. Indeed, it was shown that FMRP deficient astrocytes cause developmental delays in dendrite maturation and synaptic protein expression of hippocampal wildtype neurons (Jacobs et al., 2010, 2016), whereas normal astrocytes prevent abnormal dendritic development in hippocampal FXS neurons (Jacobs and Doering, 2010).
Investigations on the underlying mechanisms are also still in their infancy. In line with the role of FMRP in regulating protein expression, it was recently shown that the astrocyte-secreted factors Hevin25 and SPARC26, which function to control excitatory synapse development, display abnormal expression patterns in hippocampal and cortical tissues from Fmr1−/y mice (Wallingford et al., 2017): while hippocampal Hevin expression is gradually increasing from a reduced expression at P727 to elevated levels at P21, Hevin expression in the cortex displays only a transient increase at P14. SPARC, on the other hand, shows a modest decrease at P7 and P14 in the cortex, but no abnormalities in the hippocampus. Emphasizing the relevance of this data, Cheng and colleagues were able to demonstrate that astrocyte-conditioned medium is sufficient to prevent morphological deficits in hippocampal neurons cultured from FXS model mice (Cheng et al., 2016). Furthermore, Higashimori and colleagues showed that a selective knock-out of astroglial FMRP in mice modestly increases spine density and size in cortical neurons, whereas a selective re-expression is able to attenuate the abnormal spine morphology characteristic for FXS (Higashimori et al., 2016). The group also described a normalization of the FXS-typical gain in body weight, but no data on cognitive performances were reported. Studies with human astroglia would be desirable, but are currently missing.
The expansion of neocortical areas in primates caused a profound rewiring of the cortex. As a consequence, the human association cortex lacks the strict hierarchical organization of circuits seen in rodents, although certain projections follow the canonical form (e.g., parieto-prefrontal projections), but is instead characterized by multiple, large-scale distributed and highly interwoven networks termed non-canonical circuits. These circuits are highly active during cognitive performances (reviewed in Goldman-Rakic, 1988; Buckner and Krienen, 2013; Margulies, 2017).
Notably, not only the internal pathways of the cortex changed during the evolution from mice to men, also the wiring between the cortex and the hippocampus was modified: in men, the hippocampus preferentially connects to cortical association networks, whereas in mice, it preferentially associates with sensory networks (Bergmann et al., 2016). Although there are still two conserved parallel pathways between the cortex and the hippocampus in mice and men, which transfer object and context related information (reviewed in Ranganath and Ritchey, 2012), the finding of Bergmann and colleagues is of quiet some significance since cortical-hippocampal pathways are required for important brain functions including spatial working memory (studies in rodents and humans; reviewed in Sigurdsson and Duvarci, 2016), long-term memory (studies in rodents, primates and humans; reviewed in Sigurdsson and Duvarci, 2016), motivation and emotion (studies in rodents; reviewed in Sigurdsson and Duvarci, 2016), and social recognition (studies in rodents and humans; reviewed in Bicks et al., 2015). Indeed, weaknesses in working memory performance, in particular when requiring abstract item reasoning, are characteristic to FXS patients (Munir et al., 2000; Cornish et al., 2001; Kwon et al., 2001; Ornstein et al., 2008; Baker et al., 2011; Wang et al., 2013), but not to model mice (Leach et al., 2016). While Fmr1−/y mice perform as well as their wildtype littermates even when their working memory is significantly challenged (Leach et al., 2016), individuals with FXS are unable to modulate activation of the prefrontal and parietal cortex in response to an increasing working memory load (Kwon et al., 2001), implying a lack of circuit control. Indeed, a fMRI28 study showed that decreased levels of FMRP correlate with decreases in parahippocampal activation and reduced connectivity between the hippocampus and the prefrontal cortex in patients (Wang J. M. et al., 2012).
Emotional and social difficulties are frequently observed in individuals with FXS as well (Cohen et al., 1988; Mazzocco et al., 1994; Hall et al., 2009; Cordeiro et al., 2011; Kim et al., 2014), but the data on mice are inconsistent (reviewed in Kazdoba et al., 2014). Similar to the impairments observed in working memory performance, social deficits were associated with impairments in the activation of prefrontal regions in individuals with FXS (Holsen et al., 2008). Taken together, these data demonstrate that the cortical and cortical-hippocampal circuits, which characterize the human brain, are critical to FXS and cannot be appropriately modeled in mice. Even though mice may perform the same tasks as men, it is obligatory to investigate whether they also do it in the same way.
In the hippocampus, the situation is slightly different. Current research does not support major differences in the structure and function of hippocampi from mice and men (reviewed in Clark and Squire, 2013). A study comparing human and murine spatial navigation showed that both species use the same strategies (Eilam, 2014) to solve this basic and evolutionary old task. Spatial navigation in mammals is assumed to rely on hippocampal place cells, entorhinal grid cells (reviewed in Moser et al., 2008) and hippocampal theta oscillations, albeit neuronal firing in distant brain regions such as the somatosensory or prefrontal cortex is phase-locked to hippocampal theta oscillations (reviewed in Jacobs, 2013). Interestingly, the frequencies of these theta oscillations differ among species: while rats typically display oscillations at 4–8 Hz, human theta oscillations have a frequency of approximately 1–4 Hz (reviewed in Jacobs, 2013).
In line with this data, both, Fmr1−/y mice as well as FXS patients were found to show elevated error rates in the Hebb-Williams maze (MacLeod et al., 2010), a test that analyses spatial memory performance in humans and rodents under comparable conditions. In a follow-up study, the group was able to rescue the deficit in Fmr1−/y mice using MPEP, an antagonist of mGluR5 (Gandhi et al., 2014), however, contrary to humans, mice did not show increased latencies, implying differences between FXS individuals and model mice. The authors suggest that the discrepancy might arise from differences in the presentation of the maze, that is real vs. virtual, but since the human control group faced the same difficulty, this would rather argue for a different navigation strategy in FXS individuals, a strategy, that relies more on real information, such as obtained from walking, touching or smelling for instance. Indeed, difficulties in abstract thinking are characteristic for FXS patients, but not for model mice, which do as well as their wildtype litter mates in tests employing touch screens (cp. the review of Huddleston et al., 2014 and Leach et al., 2016). Since the Hebb-Williams maze is rarely used for rodents and was not employed to measure outcomes in clinical trials, conclusions are difficult to draw, in particular in the light of the role of cortical connections in human cognition and of the mixed results obtained from mice (reviewed in Kazdoba et al., 2014). However, even under conditions clearly favoring a translation between mice and men, such as in spatial navigation paradigms, the rodent model apparently reflects the situation in humans only partially.
Alternatives
Poor translatability represents indeed a major issue in most preclinical brain research. In order to overcome this obstacle, touch screen paradigms have recently been developed for rodents, which center on the Cambridge Neuropsychological Test Automated Battery for humans (reviewed in Horner et al., 2013; Hvoslef-Eide et al., 2016; Kangas and Bergman, 2017). Although these assays analyze specific cognitive abilities known to be affected in patients and achieve a high degree of standardization as well as high throughputs, Fmr1−/y mice failed to recapitulate the working memory impairments characteristic to individuals with FXS in corresponding tests even when their cognitive performance was challenged in a non-match to position task with increasing delays (Leach et al., 2016). The reasons are elusive. It is possible that the excessive pre-training as well as the correction trials required for mice affect the interpretation of results. Also, since working memory relies on the prefrontal cortex, differences in the cognitive processing can be expected, but studies are missing. More research is required to validate the neurocognitive mechanisms underlying each behavioral paradigm in our species of interest and to identify routes as well as boundaries of translation across species.
The outlined data illustrate that the current FXS mouse models fail to mirror important genetic as well as behavioral aspects of FXS, probably due to the evolutionary distance of mice and men. To address this issue, two rat models were recently developed, Fmr1 KO29 rats (Engineer et al., 2014; Till et al., 2015; Berzhanskaya et al., 2016b; Kenkel et al., 2016) and Fmr1 exon4 KO rats (Tian et al., 2017). The investigations revealed that the new model animals indeed recapitulate many features of the murine model, including enhanced basal protein synthesis, exaggerated hippocampal mGluR-LTD, elevated dendritic spine densities and cortical hyper-excitability (Till et al., 2015; Berzhanskaya et al., 2016b; Tian et al., 2017). However and much to a surprise, the rats neither reflect the behavioral phenotype of mice very well (Till et al., 2015), nor reproduce the symptoms of FXS patients any better than the murine model: although the animals demonstrated deficits in hippocampus-dependent learning (Till et al., 2015; Tian et al., 2017), they failed to display defects in spatial reference memory and reversal learning (Till et al., 2015), thereby contrasting not only the majority of data obtained from Fmr1−/y mice (D’Hooge et al., 1997; Paradee et al., 1999; Van Dam et al., 2000; Baker et al., 2010, reviewed in Kazdoba et al., 2014), but also the weak performance of FXS patients in tasks requiring the solution of new problems (Dykens et al., 1987; Maes et al., 1994; Loesch et al., 2004; Lewis et al., 2006; Van der Molen et al., 2010). Instead, these results rather imply that there is a clade-dependent component in the behavioral phenotype observed in FXS, causing the same molecular and cellular changes to give rise to different behavioral phenotypes. Given the high number of proteins affected by the loss of FMRP, numerous options exist, through which the genetic background may impact on the symptoms of the disorder. It is indeed long known that the specific phenotype of FXS model mice varies significantly among strains (reviewed in Bernardet and Crusio, 2006; Kazdoba et al., 2014). Further studies would be needed to characterize the performance of FXS model rats in cognition as well as sociality in more detail and to explain certain discrepancies between the two rat models (see Till et al., 2015; Tian et al., 2017), but it might not be worth the effort.
Considering the evolution of cognition in primates, the logical model organism for human brain function would be a closely related primate. Although virus-mediated transgenesis (Sasaki et al., 2009; Liu et al., 2016; Park et al., 2016) or ZFN30/TALEN31-driven genome editing (Sato et al., 2016) have been used to generate primate models, the invention of Crispr-mediated genome editing and its successful employment in primates (Niu et al., 2014; Chen et al., 2015; Tu et al., 2017; Zhao et al., 2017; Zuo et al., 2017) and even in (nonviable) human embryos (Liang P. et al., 2015; Tang et al., 2017) have brought this option within much closer reach. Compared to rodents, primates have several advantages when it comes to modeling cognition (for a comprehensive review, please also see “Why primate models matter”; Phillips et al., 2014), in particular with respect to ASDs:
the cell types and circuits seen in primates are more similar to those found in humans, which is relevant to many cognitive tasks, but particularly important to spatial working memory and social recognition (see Hopkins, 2013; Frey et al., 2014; Neubert et al., 2014; Morecraft et al., 2015; Wilson et al., 2015a; and the section: “The Cortex, the Hippocampus and FXS”)
the prolonged prenatal development of the cortex, which is characteristic to humans and primates, is not present in rodents, hampering neuro-developmental studies in rodents
group living, co-operative behavior and cultural intelligence are much more sophisticated in primates (cp. the section: “The Cortex, the Hippocampus and FXS” and Decasien et al., 2017; Street et al., 2017)
the basic communication features characteristic to human language are already present in primates, including the ability to utilize symbolization, basic semantic representation, categorical representation and rudimentary grammar (Moore et al., 2003, 2005, 2006; Joly et al., 2012; Morrill et al., 2012; Ghazanfar et al., 2013; Wilson et al., 2013, 2015b)
many tests developed to analyze cognition in humans can easily be adapted for primates, e.g., eye-tracking to study abnormal gaze (Machado and Nelson, 2011; Rosati et al., 2016), a typical symptom of autism spectrum disorders, or computerized cognition tests (Spinelli et al., 2004; Harris et al., 2007; Barner et al., 2008; Diester and Nieder, 2010; Jones et al., 2010; Takemoto et al., 2011; Verrico et al., 2011; Beran et al., 2012, 2015; Brosnan et al., 2012; Evans and Beran, 2012; Basile and Hampton, 2013; Klein et al., 2013; Bramlett-Parker and Washburn, 2016; Oikonomidis et al., 2017), thereby facilitating the translation of results
Taken together, these studies show that many features characterizing human behavior and typically affected in ASDs, such as communication capabilities and social skills or abstract thinking for instance, are represented in primates. A primate model would hence facilitate investigations addressing core symptoms of the autism phenotype, which are absent or only rudimentary developed in rodents.
There is another important feature of the disease, which cannot be modeled in mice: hypermethylation. Contrary to mice, in which most CpG-islands have apparently eroded during evolution (Aïssani and Bernardi, 1991; Matsuo et al., 1993), primates show methylation patterns highly similar to those of humans. Approximately 90% of the methylation patterns are in fact conserved between men and chimpanzees (Martin et al., 2011; Molaro et al., 2011; Pai et al., 2011), in particular at CpG-islands and promoter regions (Illingworth et al., 2010; Hernando-Herraez et al., 2013, 2015; Long et al., 2013). However, when comparing those genes that are differentially methylated, human genes turned out to exhibit lower levels of promoter methylation than genes from chimpanzees (Gama-Sosa et al., 1983; Zeng et al., 2012), suggesting that gene expression control is less strict in humans. Since a disproportional high number of differentially methylated genes is associated with human diseases (Zeng et al., 2012; Fukuda et al., 2013; Hernando-Herraez et al., 2013), it seems possible that the reduced control of certain genes, which finally made us human, also makes us more susceptible to certain pathologies such as senescence and Alzheimer’s disease, disorders, which are not present in our closest relatives, the great apes (reviewed in Finch and Austad, 2015; Lowenstine et al., 2016). Notably, though some of the genes shown to be differentially methylated in humans are known for their association with ASDs, such as GABAa and GABAb receptors for instance (Zeng et al., 2012; Hernando-Herraez et al., 2013), FMR1 was not associated with human-specific methylation patterns yet.
Despite these promising premises, primate models also have some disadvantages when compared to rodent models: Working with primates, in particular with great apes, is expensive by all means, it requires a lot of training and experience, bears the risk of transmitting diseases and the longevity of great apes hampers investigations of senescence. Significant n-numbers are often hard to achieve. Hence, primate species which are small, relatively short lived and easy to keep could help to overcome these obstacles.
The evolutionary next closest alternatives to great apes are old world monkeys. Consisting of about 160 species, old world monkeys represent the largest group of primates. Among them are the macaque monkeys, which include two species, that have been used in science for a long time, the crab-eating (alias: cynomolgus; M. fascicularis) and the rhesus macaque (M. mulatta). These two species are the widest spread primates next to humans and are categorized as species with Least Concerns by the Red List. Facilitating housing and breeding, macaques live in large multi-male, multi-female groups, mature at the age of app. 3.5 years (great apes: 6–10 years) and have a gestation period of 160–180 days (great apes: 225–270 days), giving birth to one infant per parturition (reviewed in Lindburg, 1991).
Notably, crab-eating macaques have recently been used to model ASDs (Liu et al., 2016; Zhao et al., 2017). Liu and colleagues expressed human MeCP232 in the macaque brain to mimic an ASD resulting from duplications of the MECP2-containing genome segment, whereas Zhao and colleagues introduced deletions to SHANK333, which are known to cause ASD. Remarkably, both studies found striking differences compared to the corresponding mouse models: while the MECP2-overexpression model demonstrated clear autism-like behaviors in primates, but not in mice, the SHANK3-deletion model revealed significant differences in the expression pattern of Shank3, and found an impaired neurogenesis in the prefrontal cortex of macaques.
Despite these promising results, macaque models also have some disadvantages: The monkeys are carriers of Herpes B viruses and may transmit this potentially fatal disease to humans. Their long adolescence (3.5 years) hampers breeding, and their longevity (approximately 30 years in captivity) is clearly not supporting studies of senescence. Although highly developed, their social system is not in favor of ASD research as well, since macaques live in large multi-male/female groups, whereas humans live in (extended) family groups. As a result, proactive prosociality, which is believed to be based on shared infant care, is well developed in humans, but not in chimpanzees or macaques (Burkart and van Schaik, 2013).
For these reasons, marmosets have recently garnered interest as model animals for studying brain function (reviewed in Saito, 2015; Tokuno et al., 2015), for a general review on the species, please see (Schiel and Souto, 2017). Also known as zaris, these new world monkeys split from the primate lineage approximately 40 million years ago, 35 million years before humans and chimpanzees separated. Compared to great apes and macaques, marmosets have the advantage of being small, easy to handle, easy to breed and less expensive: with a life span of about 12 years in captivity, marmosets mature more quickly than great apes or macaques, starting reproduction at 18 months of age and giving birth to twins after a gestation period of 140–150 days. Contrary to macaques, marmosets do not represent a natural reservoir of Herpes B viruses.
Though lissencephalic (smooth), their brain shares many features of the human brain, and their cerebral cortex shows the neuronal architecture of all primates (Bendor and Wang, 2005; Burman et al., 2006; Elston et al., 2006; Burman and Rosa, 2009; de la Mothe et al., 2012; Chaplin et al., 2013), from which only humans differ in that neurons of their prefrontal cortex are more spiny and more complex than those of their primate relatives (Elston et al., 2006). Consequently, marmosets have the high cognitive abilities characteristic to all primates: they are not only able to perform true imitation (Bugnyar and Huber, 1997; Voelkl and Huber, 2007), transposition and generalization (Yamazaki et al., 2014) but to also solve string problems (Halsey et al., 2006; Gagne et al., 2012) and to understand physical causality (Yamazaki et al., 2011). Considering the weaknesses of FXS individuals in abstract item reasoning and in addressing new problems, the cognitive abilities of marmosets might help to develop tasks which directly translate results between the two species.
Of particular interest for the design of ASD models is the sociality of marmosets. In a convergent evolution to humans, marmosets developed a high level of group living (reviewed in Graham, 2016). At a state of sophistication not known from other mammals including most primates, marmosets demonstrate altruistic behaviors such as proactive prosociality and third-party reciprocity (Burkart et al., 2007; Burkart and van Schaik, 2013), social learning during infancy (Dell’Mour et al., 2009) as well as adulthood (Caldwell and Whiten, 2004), and behavioral adaptations to social environments (Koski and Burkart, 2015). Similar to humans, marmosets live in extended family groups, pair-bond and care for their offspring in a cooperative manner (Digby and Barreto, 1993; Sousa et al., 2005; Birnie et al., 2013; Yamamoto et al., 2014). Since parental care and in particular maternal warmth are known to influence FXS symptoms in children (Dyer-Friedman et al., 2002; Kuo et al., 2002; Glaser et al., 2003; Greenberg et al., 2012; Robinson et al., 2016; Smith et al., 2016), the latter could be useful to further investigate the role of the social environment for FXS.
Like other primates, marmosets mostly rely on vocalizations (Miller and Wang, 2006; Chen et al., 2009; Miller et al., 2010; Watson and Caldwell, 2010; Bakker et al., 2014; Kato et al., 2014; Agamaite et al., 2015) and visual cues (de Boer et al., 2013; Massen et al., 2016) for their communication, although social grooming (Lazaro-Perea et al., 2004) and scent marking (Epple, 1970; Massen et al., 2016) are present as well. Since ASDs are characterized by gaze avoidance, it is particularly interesting that marmosets are able to use a variety of facial expressions for communication (Kemp and Kaplan, 2013) and to gain information by geometrical gaze following, even from human experimenters (Burkart and Heschl, 2006). Analyzing the face scanning patterns performed by marmosets, Kotani et al. (2017) showed that these primates primarily view the eye region during contact and that this behavior can be employed to evaluate the influence of drugs.
Due to the dense vegetation of their natural habitat, vocalizations are unusual rich in marmosets, even for primates (Epple, 1968; Morrill et al., 2013; Agamaite et al., 2015). Marmoset conversations involve a cooperative vocal control and require the infants to learn when to talk and when to listen (Takahashi et al., 2013, 2016; Choi J. Y. et al., 2015; Chow et al., 2015), thereby paralleling human development. Indeed, recent research revealed that marmoset infants need to transform their babbling and crying into mature vocalizations in order to properly communicate with other group members (Margaret Elowson et al., 1998; Pistorio et al., 2006; Takahashi D. Y. et al., 2015; Ghazanfar and Zhang, 2016) and that this transformation requires social reinforcement from caregivers (Margaret Elowson et al., 1998; Takahashi et al., 2017). Given the ability of marmosets to even learn grammar (Wilson et al., 2013) and the cluttered speech observed in individuals with FXS (Hanson et al., 1986; Belser and Sudhalter, 2001; Roberts et al., 2007; Klusek et al., 2014), the high level of vocal communication in marmosets could be valuable to the development of treatments for FXS and ASD patients.
Though their sociality and their cognitive abilities make marmosets a promising model organism for FXS and ASD research, it is just this very same point, which also bears the disadvantages. The high level of communication and understanding of social interactions increases the risk that relations between researchers and experimental animals arise, which may impact on experiments (cp. Herzog, 2002), for example, if individual animals dislike or prefer being handled or cared for by a certain person and subsequent stress levels influence the outcome of an experiment. Since the n-numbers used in primate research are at the minimum, such effects might easily turn out “significant”.
Another important concern is morality. Although all mammals are able to feel pain, stress and fear in a similar way, no matter whether they are rodents, primates or of any other clade, the high cognitive capabilities and social skills of primates have raised particular ethical concerns regarding their use in biomedical research (cp. the reviews of Coors et al., 2010; Phillips et al., 2014; Zhou, 2014; Bailey and Taylor, 2016; Arnason, 2017). As a consequence, many countries have implemented policies and regulations to ensure the physiological as well as psychological well-being of all research animals (Pereira et al., 2004; Luy, 2007; Hansen et al., 2017), and the standards are particularly high for primates (see Tardif et al., 2013; Weiss and Hampshire, 2015). However, the ethical viewpoints often differ, not only within a society (cp. Buckley et al., 2011; Phillips et al., 2014; Arnason, 2017 vs. Bailey and Taylor, 2016), but also among societies (cp. Cyranoski, 2004; Zhang X. L. et al., 2014), causing the hurdles for the approval of a project to vary significantly between countries and sometimes even within countries. The same project might thus be approved within a few weeks in one country, within a few months in another, and not in years in the next.
These circumstances raise several questions:
Is it ethically justified to approve therapies developed in countries with lower animal welfare standards in countries with higher standards, considering that such approvals would torpedo all animal welfare efforts? Is it ethically justified to deny patients a therapy developed in a country, which had lower animal care standards? Is it ethically justified to have wealthy people traveling to countries offering corresponding therapies, while others cannot afford to do so?
Moreover: can cognitive abilities indeed be a measure to define welfare standards and requirements? Where is the red line? These two questions are intimately connected, since the use of cognitive capabilities as an argument for increased standards in turn causes diminished abilities to result in the opposite. Since everything goes the way of least constrains, this is the point where the seemingly high moral standards cause ethics and science to start loosing ground: is it ethically and scientifically justified to use thousands of mice in preclinical research, to enrol hundreds of patients in clinical studies, to put patients at risk, albeit the risk might be marginal, and to cause hopes and disappointments in their families, just to learn how hard it is to find out how to keep the Concorde flying from studying a biplane?
Author Contributions
RD wrote the manuscript.
Conflict of Interest Statement
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
I would like to acknowledge support by the Deutsche Forschungsgemeinschaft and the Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU) within the funding pogramme Open Access Publishing.
Footnotes
1intelligence quotient scores
2compare
3Electroencephalography
4untranslated region
55′-C-phosphate-G-3′
6single-stranded DNA
7Amyloid-Precursor-Protein
8In 2006, an inducible Fmr1−/y mouse model was generated to address aspects related to developmental or regional expression patterns, but the animals have only been used in a very few studies thus far, possibly due to limitations in the availability of appropriate Cre-lines. For more information, please refer to Table 2.
9metabotropic glutamate receptors 1 and 5, = group 1 mGluRs
10α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor
11extracellular signal-regulated kinase
12mammalian target of rapamycin
13Phosphoinositid-3-Kinase
14PI3K Enhancer
15Glycogen synthase kinase 3
16long term potentiation
17long term depression
18N-methyl-D-aspartate receptor
19Cornu Ammonis region 1
202-Methyl-6-(phenylethynyl) pyridine
21sodium-activated potassium channel Slack
22large-conductance calcium-activated potassium channels
23gamma-aminobutyric acid
24hyperpolarization-activated cyclic nucleotide-gated cation channel
25high endothelial venule protein, also known as SPARC like protein
26secreted protein, acidic and rich in cysteine
27postnatal day 7
28functional magnetic resonance imaging
29knock-out
30zinc-finger nucleases
31transcription activator-like effector nucleases
32methyl CpG binding protein 2
33SH3 and multiple ankyrin repeat domains 3, alias: proline-rich protein 2
References
- Abel T., Nguyen P. V., Barad M., Deuel T. A., Kandel E. R., Bourtchouladze R. (1997). Genetic demonstration of a role for PKA in the late phase of LTP and in hippocampus-based long-term memory. Cell 88, 615–626. 10.1016/s0092-8674(00)81904-2 [DOI] [PubMed] [Google Scholar]
- Ackerman S. (1992). Discovering the Brain. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Adams R. H., Blackmon H., Reyes-Velasco J., Schield D. R., Card D. C., Andrew A. L., et al. (2016). Microsatellite landscape evolutionary dynamics across 450 million years of vertebrate genome evolution. Genome 59, 295–310. 10.1139/gen-2015-0124 [DOI] [PubMed] [Google Scholar]
- Adihe Lokanga R., Zhao X.-N., Entezam A., Usdin K. (2014). X inactivation plays a major role in the gender bias in somatic expansion in a mouse model of the fragile X-related disorders: implications for the mechanism of repeat expansion. Hum. Mol. Genet. 23, 4985–4994. 10.1093/hmg/ddu213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agamaite J. A., Chang C. J., Osmanski M. S., Wang X. (2015). A quantitative acoustic analysis of the vocal repertoire of the common marmoset (Callithrix jacchus). J. Acoust. Soc. Am. 138, 2906–2928. 10.1121/1.4934268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aguilar-Valles A., Matta-Camacho E., Khoutorsky A., Gkogkas C., Nader K., Lacaille J. C., et al. (2015). Inhibition of group I metabotropic glutamate receptors reverses autistic-like phenotypes caused by deficiency of the translation repressor eIF4E binding protein 2. J. Neurosci. 35, 11125–11132. 10.1523/JNEUROSCI.4615-14.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aïssani B., Bernardi G. (1991). CpG islands: features and distribution in the genomes of vertebrates. Gene 106, 173–183. 10.1016/0378-1119(91)90197-j [DOI] [PubMed] [Google Scholar]
- Akins M. R., Berk-Rauch H. E., Kwan K. Y., Mitchell M. E., Shepard K. A., Korsak L. I., et al. (2017). Axonal ribosomes and mRNAs associate with fragile X granules in adult rodent and human brains. Hum. Mol. Genet. 26, 192–209. 10.1093/hmg/ddw381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alam M. P., Datta S., Majumdar S., Mehta A. K., Baskaran S., Gulati N., et al. (2010). Comparative analysis of DNA methylation in transgenic mice with unstable CGG repeats from FMR1 gene. Epigenetics 5, 241–248. 10.4161/epi.5.3.11417 [DOI] [PubMed] [Google Scholar]
- Allen N. J. (2014). Astrocyte regulation of synaptic behavior. Annu. Rev. Cell Dev. Biol. 30, 439–463. 10.1146/annurev-cellbio-100913-013053 [DOI] [PubMed] [Google Scholar]
- Allen N. J., Eroglu C. (2017). Cell biology of astrocyte-synapse interactions. Neuron 96, 697–708. 10.1016/j.neuron.2017.09.056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aloisi E., Le Corf K., Dupuis J., Zhang P., Ginger M., Labrousse V., et al. (2017). Altered surface mGluR5 dynamics provoke synaptic NMDAR dysfunction and cognitive defects in Fmr1 knockout mice. Nat. Commun. 8:1103. 10.1038/s41467-017-01191-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alpatov R., Lesch B. J., Nakamoto-Kinoshita M., Blanco A., Chen S., Stutzer A., et al. (2014). A chromatin-dependent role of the fragile X mental retardation protein FMRP in the DNA damage response. Cell 157, 869–881. 10.1016/j.cell.2014.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson J. R., Takimoto A., Kuroshima H., Fujita K. (2013). Capuchin monkeys judge third-party reciprocity. Cognition 127, 140–146. 10.1016/j.cognition.2012.12.007 [DOI] [PubMed] [Google Scholar]
- Andriezen W. L. (1893). The neuroglia elements in the human brain. Br. Med. J. 2, 227–230. 10.1136/bmj.2.1700.227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antar L. N., Dictenberg J. B., Plociniak M., Afroz R., Bassell G. J. (2005). Localization of FMRP-associated mRNA granules and requirement of microtubules for activity-dependent trafficking in hippocampal neurons. Genes Brain Behav. 4, 350–359. 10.1111/j.1601-183x.2005.00128.x [DOI] [PubMed] [Google Scholar]
- Antar L. N., Li C., Zhang H., Carroll R. C., Bassell G. J. (2006). Local functions for FMRP in axon growth cone motility and activity-dependent regulation of filopodia and spine synapses. Mol. Cell. Neurosci. 32, 37–48. 10.1016/j.mcn.2006.02.001 [DOI] [PubMed] [Google Scholar]
- Antequera F. (2003). Structure, function and evolution of CpG island promoters. Cell. Mol. Life Sci. 60, 1647–1658. 10.1007/s00018-003-3088-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnason G. (2017). The ethical justification for the use of non-human primates in research: the Weatherall report revisited. J. Med. Ethics [Epub ahead of print]. 10.1136/medethics-2016-103827 [DOI] [PubMed] [Google Scholar]
- Ascano M., Mukherjee N., Bandaru P., Miller J. B., Nusbaum J. D., Corcoran D. L., et al. (2012). FMRP targets distinct mRNA sequence elements to regulate protein expression. Nature 492, 382–386. 10.1038/nature11737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach B. D., Bear M. F. (2010). Loss of the fragile X mental retardation protein decouples metabotropic glutamate receptor dependent priming of long-term potentiation from protein synthesis. J. Neurophysiol. 104, 1047–1051. 10.1152/jn.00449.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avitzour M., Mor-Shaked H., Yanovsky-Dagan S., Aharoni S., Altarescu G., Renbaum P., et al. (2014). FMR1 epigenetic silencing commonly occurs in undifferentiated fragile X-affected embryonic stem cells. Stem Cell Rep. 3, 699–706. 10.1016/j.stemcr.2014.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azevedo F. A., Carvalho L. R., Grinberg L. T., Farfel J. M., Ferretti R. E., Leite R. E., et al. (2009). Equal numbers of neuronal and nonneuronal cells make the human brain an isometrically scaled-up primate brain. J. Comp. Neurol. 513, 532–541. 10.1002/cne.21974 [DOI] [PubMed] [Google Scholar]
- Bagni C., Greenough W. T. (2005). From mRNP trafficking to spine dysmorphogenesis: the roots of fragile X syndrome. Nat. Rev. Neurosci. 6, 376–387. 10.1038/nrn1667 [DOI] [PubMed] [Google Scholar]
- Bagshaw A. T., Horwood L. J., Fergusson D. M., Gemmell N. J., Kennedy M. A. (2017). Microsatellite polymorphisms associated with human behavioural and psychological phenotypes including a gene-environment interaction. BMC Med. Genet. 18:12. 10.1186/s12881-017-0374-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey J., Taylor K. (2016). Non-human primates in neuroscience research: the case against its scientific necessity. Altern. Lab. Anim. 44, 43–69. [DOI] [PubMed] [Google Scholar]
- Baker S., Hooper S., Skinner M., Hatton D., Schaaf J., Ornstein P., et al. (2011). Working memory subsystems and task complexity in young boys with Fragile X syndrome. J. Intellect. Disabil. Res. 55, 19–29. 10.1111/j.1365-2788.2010.01343.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker K. B., Wray S. P., Ritter R., Mason S., Lanthorn T. H., Savelieva K. V. (2010). Male and female Fmr1 knockout mice on C57 albino background exhibit spatial learning and memory impairments. Genes Brain Behav. 9, 562–574. 10.1111/j.1601-183x.2010.00585.x [DOI] [PubMed] [Google Scholar]
- Bakker C. E., De Diego Otero Y., Bontekoe C., Raghoe P., Luteijn T., Hoogeveen A. T., et al. (2000). Immunocytochemical and biochemical characterization of FMRP, FXR1P and FXR2P in the mouse. Exp. Cell Res. 258, 162–170. 10.1006/excr.2000.4932 [DOI] [PubMed] [Google Scholar]
- Bakker J., van Nijnatten T. J., Louwerse A. L., Baarends G., Arndt S. S., Langermans J. A. (2014). Evaluation of ultrasonic vocalizations in common marmosets (Callithrix jacchus) as a potential indicator of welfare. Lab Anim. (NY) 43, 313–320. 10.1038/laban.568 [DOI] [PubMed] [Google Scholar]
- Bakker C. E., Verheij C., Willemsen R., van der Helm R., Oerlemans F., Vermey M., et al. (1994). Fmr1 knockout mice: a model to study fragile X mental retardation. The Dutch-Belgian Fragile X Consortium. Cell 78, 23–33. 10.1016/0092-8674(94)90569-x [DOI] [PubMed] [Google Scholar]
- Bar-Nur O., Caspi I., Benvenisty N. (2012). Molecular analysis of FMR1 reactivation in fragile-X induced pluripotent stem cells and their neuronal derivatives. J. Mol. Cell. Biol. 4, 180–183. 10.1093/jmcb/mjs007 [DOI] [PubMed] [Google Scholar]
- Barak M. M., Lieberman D. E., Hublin J. J. (2013). Of mice, rats and men: trabecular bone architecture in mammals scales to body mass with negative allometry. J. Struct. Biol. 183, 123–131. 10.1016/j.jsb.2013.04.009 [DOI] [PubMed] [Google Scholar]
- Bardoni B., Capovilla M., Lalli E. (2017). Modeling Fragile X syndrome in neurogenesis: an unexpected phenotype and a novel tool for future therapies. Neurogenesis 4:e1270384. 10.1080/23262133.2016.1270384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barner D., Wood J., Hauser M., Carey S. (2008). Evidence for a non-linguistic distinction between singular and plural sets in rhesus monkeys. Cognition 107, 603–622. 10.1016/j.cognition.2007.11.010 [DOI] [PubMed] [Google Scholar]
- Basile B. M., Hampton R. R. (2013). Dissociation of active working memory and passive recognition in rhesus monkeys. Cognition 126, 391–396. 10.1016/j.cognition.2012.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baskaran S., Datta S., Mandal A., Gulati N., Totey S., Anand R. R., et al. (2002). Instability of CGG repeats in transgenic mice. Genomics 80, 151–157. 10.1006/geno.2002.6813 [DOI] [PubMed] [Google Scholar]
- Basuta K., Schneider A., Gane L., Polussa J., Woodruff B., Pretto D., et al. (2015). High functioning male with fragile X syndrome and fragile X-associated tremor/ataxia syndrome. Am. J. Med. Genet. A 167A, 2154–2161. 10.1002/ajmg.a.37125 [DOI] [PubMed] [Google Scholar]
- Bear M. F., Huber K. M., Warren S. T. (2004). The mGluR theory of fragile X mental retardation. Trends Neurosci. 27, 370–377. 10.1016/j.tins.2004.04.009 [DOI] [PubMed] [Google Scholar]
- Bechara E. G., Didiot M. C., Melko M., Davidovic L., Bensaid M., Martin P., et al. (2009). A novel function for fragile X mental retardation protein in translational activation. PLoS Biol. 7:e1000016. 10.1371/journal.pbio.1000016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belser R. C., Sudhalter V. (2001). Conversational characteristics of children with fragile X syndrome: repetitive speech. Am. J. Ment. Retard. 106, 28–38. [DOI] [PubMed] [Google Scholar]
- Bendor D., Wang X. (2005). The neuronal representation of pitch in primate auditory cortex. Nature 436, 1161–1165. 10.1038/nature03867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beran M. J., Evans T. A., Klein E. D., Einstein G. O. (2012). Rhesus monkeys (Macaca mulatta) and capuchin monkeys (Cebus apella) remember future responses in a computerized task. J. Exp. Psychol. Anim. Behav. Process. 38, 233–243. 10.1037/a0027796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beran M. J., Parrish A. E., Futch S. E., Evans T. A., Perdue B. M. (2015). Looking ahead? Computerized maze task performance by chimpanzees (Pan troglodytes), rhesus monkeys (Macaca mulatta), capuchin monkeys (Cebus apella), and human children (Homo sapiens). J. Comp. Psychol. 129, 160–173. 10.1037/a0038936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergmann E., Zur G., Bershadsky G., Kahn I. (2016). The organization of mouse and human cortico-hippocampal networks estimated by intrinsic functional connectivity. Cereb. Cortex 26, 4497–4512. 10.1093/cercor/bhw327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernardet M., Crusio W. E. (2006). Fmr1 KO mice as a possible model of autistic features. ScientificWorldJournal 6, 1164–1176. 10.1100/tsw.2006.220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry D., Deater-Deckard K., McCartney K., Wang Z., Petrill S. A. (2013). Gene-environment interaction between dopamine receptor D4 7-repeat polymorphism and early maternal sensitivity predicts inattention trajectories across middle childhood. Dev. Psychopathol. 25, 291–306. 10.1017/s095457941200106x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berzhanskaya J., Phillips M. A., Gorin A., Lai C., Shen J., Colonnese M. T. (2016a). Disrupted cortical state regulation in a rat model of fragile X syndrome. Cereb. Cortex 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berzhanskaya J., Phillips M. A., Shen J., Colonnese M. T. (2016b). Sensory hypo-excitability in a rat model of fetal development in Fragile X Syndrome. Sci. Rep. 6:30769. 10.1038/srep30769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berzhanskaya J., Phillips M. A., Gorin A., Lai C., Shen J., Colonnese M. T. (2017). Disrupted cortical state regulation in a rat model of fragile X syndrome. Cereb. Cortex 27, 1386–1400. 10.1093/cercor/bhv331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhattacharya A., Kaphzan H., Alvarez-Dieppa A. C., Murphy J. P., Pierre P., Klann E. (2012). Genetic removal of p70 S6 kinase 1 corrects molecular, synaptic and behavioral phenotypes in fragile X syndrome mice. Neuron 76, 325–337. 10.1016/j.neuron.2012.07.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhattacharya A., Mamcarz M., Mullins C., Choudhury A., Boyle R. G., Smith D. G., et al. (2016). Targeting translation control with p70 S6 kinase 1 inhibitors to reverse phenotypes in fragile X syndrome mice. Neuropsychopharmacology 41, 1991–2000. 10.1038/npp.2015.369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bianchi R., Chuang S. C., Zhao W., Young S. R., Wong R. K. (2009). Cellular plasticity for group I mGluR-mediated epileptogenesis. J. Neurosci. 29, 3497–3507. 10.1523/JNEUROSCI.5447-08.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bicks L. K., Koike H., Akbarian S., Morishita H. (2015). Prefrontal cortex and social cognition in mouse and man. Front. Psychol. 6:1805. 10.3389/fpsyg.2015.01805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilgin Sonay T., Carvalho T., Robinson M. D., Greminger M. P., Krützen M., Comas D., et al. (2015). Tandem repeat variation in human and great ape populations and its impact on gene expression divergence. Genome Res. 25, 1591–1599. 10.1101/gr.190868.115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birnie A. K., Taylor J. H., Cavanaugh J., French J. A. (2013). Quality of maternal and paternal care predicts later stress reactivity in the cooperatively-breeding marmoset (Callithrix geoffroyi). Psychoneuroendocrinology 38, 3003–3014. 10.1016/j.psyneuen.2013.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bliss T. V., Collingridge G. L., Morris R. G. (2003). Introduction. Long-term potentiation and structure of the issue. Philos. Trans. R. Soc. Lond. B Biol. Sci. 358, 607–611. 10.1098/rstb.2003.1282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boda B., Mendez P., Boury-Jamot B., Magara F., Muller D. (2014). Reversal of activity-mediated spine dynamics and learning impairment in a mouse model of Fragile X syndrome. Eur. J. Neurosci. 39, 1130–1137. 10.1111/ejn.12488 [DOI] [PubMed] [Google Scholar]
- Bonaccorso C. M., Spatuzza M., Di Marco B., Gloria A., Barrancotto G., Cupo A., et al. (2015). Fragile X mental retardation protein (FMRP) interacting proteins exhibit different expression patterns during development. Int. J. Dev. Neurosci. 42, 15–23. 10.1016/j.ijdevneu.2015.02.004 [DOI] [PubMed] [Google Scholar]
- Bontekoe C. J., Bakker C. E., Nieuwenhuizen I. M., van der Linde H., Lans H., de Lange D., et al. (2001). Instability of a (CGG)98 repeat in the Fmr1 promoter. Hum. Mol. Genet. 10, 1693–1699. 10.1093/hmg/10.16.1693 [DOI] [PubMed] [Google Scholar]
- Bontekoe C. J., de Graaff E., Nieuwenhuizen I. M., Willemsen R., Oostra B. A. (1997). FMR1 premutation allele (CGG)81 is stable in mice. Eur. J. Hum. Genet. 5, 293–298. [PubMed] [Google Scholar]
- Bostrom C. A., Majaess N. M., Morch K., White E., Eadie B. D., Christie B. R. (2015). Rescue of NMDAR-dependent synaptic plasticity in Fmr1 knock-out mice. Cereb. Cortex 25, 271–279. 10.1093/cercor/bht237 [DOI] [PubMed] [Google Scholar]
- Botta-Orfila T., Tartaglia G. G., Michalon A. (2016). Molecular pathophysiology of fragile X-associated tremor/ataxia syndrome and perspectives for drug development. Cerebellum 15, 599–610. 10.1007/s12311-016-0800-2 [DOI] [PubMed] [Google Scholar]
- Braat S., D’Hulst C., Heulens I., De Rubeis S., Mientjes E., Nelson D. L., et al. (2015). The GABAA receptor is an FMRP target with therapeutic potential in fragile X syndrome. Cell Cycle 14, 2985–2995. 10.4161/15384101.2014.989114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brager D. H., Akhavan A. R., Johnston D. (2012). Impaired dendritic expression and plasticity of h-channels in the fmr1−/y mouse model of fragile X syndrome. Cell Rep. 1, 225–233. 10.1016/j.celrep.2012.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bramlett-Parker J., Washburn D. A. (2016). Can rhesus monkey learn executive attention? Behav. Sci. 6:E26. 10.3390/bs6020011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brasa S., Mueller A., Jacquemont S., Hahne F., Rozenberg I., Peters T., et al. (2016). Reciprocal changes in DNA methylation and hydroxymethylation and a broad repressive epigenetic switch characterize FMR1 transcriptional silencing in fragile X syndrome. Clin. Epigenetics 8:15. 10.1186/s13148-016-0181-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brosnan S. F., Wilson B. J., Beran M. J. (2012). Old World monkeys are more similar to humans than New World monkeys when playing a coordination game. Proc. Biol. Sci. 279, 1522–1530. 10.1098/rspb.2011.1781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouwer J. R., Mientjes E. J., Bakker C. E., Nieuwenhuizen I. M., Severijnen L. A., Van der Linde H. C., et al. (2007). Elevated Fmr1 mRNA levels and reduced protein expression in a mouse model with an unmethylated Fragile X full mutation. Exp. Cell Res. 313, 244–253. 10.1016/j.yexcr.2006.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown V., Jin P., Ceman S., Darnell J. C., O’Donnell W. T., Tenenbaum S. A., et al. (2001). Microarray identification of FMRP-associated brain mRNAs and altered mRNA translational profiles in fragile X syndrome. Cell 107, 477–487. 10.1016/s0092-8674(01)00568-2 [DOI] [PubMed] [Google Scholar]
- Brown M. R., Kronengold J., Gazula V. R., Chen Y., Strumbos J. G., Sigworth F. J., et al. (2010). Fragile X mental retardation protein controls gating of the sodium-activated potassium channel Slack. Nat. Neurosci. 13, 819–821. 10.1038/nn.2563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckley L. A., Chapman K., Burns-Naas L. A., Todd M. D., Martin P. L., Lansita J. A. (2011). Considerations regarding nonhuman primate use in safety assessment of biopharmaceuticals. Int. J. Toxicol. 30, 583–590. 10.1177/1091581811415875 [DOI] [PubMed] [Google Scholar]
- Buckner R. L., Krienen F. M. (2013). The evolution of distributed association networks in the human brain. Trends Cogn. Sci. 17, 648–665. 10.1016/j.tics.2013.09.017 [DOI] [PubMed] [Google Scholar]
- Bugnyar T., Huber L. (1997). Push or pull: an experimental study on imitation in marmosets. Anim. Behav. 54, 817–831. 10.1006/anbe.1996.0497 [DOI] [PubMed] [Google Scholar]
- Burket J. A., Benson A. D., Tang A. H., Deutsch S. I. (2014). Rapamycin improves sociability in the BTBR T+Itpr3tf/J mouse model of autism spectrum disorders. Brain Res. Bull. 100, 70–75. 10.1016/j.brainresbull.2013.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burkart J. M., Fehr E., Efferson C., van Schaik C. P. (2007). Other-regarding preferences in a non-human primate: common marmosets provision food altruistically. Proc. Natl. Acad. Sci. U S A 104, 19762–19766. 10.1073/pnas.0710310104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burkart J., Heschl A. (2006). Geometrical gaze following in common marmosets (Callithrix jacchus). J. Comp. Psychol. 120, 120–130. 10.1037/0735-7036.120.2.120 [DOI] [PubMed] [Google Scholar]
- Burkart J. M., van Schaik C. (2013). Group service in macaques (Macaca fuscata), capuchins (Cebus apella) and marmosets (Callithrix jacchus): a comparative approach to identifying proactive prosocial motivations. J. Comp. Psychol. 127, 212–225. 10.1037/a0026392 [DOI] [PubMed] [Google Scholar]
- Burman K. J., Palmer S. M., Gamberini M., Rosa M. G. (2006). Cytoarchitectonic subdivisions of the dorsolateral frontal cortex of the marmoset monkey (Callithrix jacchus) and their projections to dorsal visual areas. J. Comp. Neurol. 495, 149–172. 10.1002/cne.20837 [DOI] [PubMed] [Google Scholar]
- Burman K. J., Rosa M. G. (2009). Architectural subdivisions of medial and orbital frontal cortices in the marmoset monkey (Callithrix jacchus). J. Comp. Neurol. 514, 11–29. 10.1002/cne.21976 [DOI] [PubMed] [Google Scholar]
- Buschiazzo E., Gemmell N. J. (2010). Conservation of human microsatellites across 450 million years of evolution. Genome Biol. Evol. 2, 153–165. 10.1093/gbe/evq007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caku A., Pellerin D., Bouvier P., Riou E., Corbin F. (2014). Effect of lovastatin on behavior in children and adults with fragile X syndrome: an open-label study. Am. J. Med. Genet. A 164A, 2834–2842. 10.1002/ajmg.a.36750 [DOI] [PubMed] [Google Scholar]
- Caldwell C. A., Whiten A. (2004). Testing for social learning and imitation in common marmosets, Callithrix jacchus, using an artificial fruit. Anim. Cogn. 7, 77–85. 10.1007/s10071-003-0192-9 [DOI] [PubMed] [Google Scholar]
- Castrén M., Pääkkönen A., Tarkka I. M., Ryynänen M., Partanen J. (2003). Augmentation of auditory N1 in children with fragile X syndrome. Brain Topogr. 15, 165–171. 10.1023/A:1022606200636 [DOI] [PubMed] [Google Scholar]
- Ceman S., O’Donnell W. T., Reed M., Patton S., Pohl J., Warren S. T. (2003). Phosphorylation influences the translation state of FMRP-associated polyribosomes. Hum. Mol. Genet. 12, 3295–3305. 10.1093/hmg/ddg350 [DOI] [PubMed] [Google Scholar]
- Centonze D., Rossi S., Mercaldo V., Napoli I., Ciotti M. T., De Chiara V., et al. (2008). Abnormal striatal GABA transmission in the mouse model for the fragile X syndrome. Biol. Psychiatry 63, 963–973. 10.1016/j.biopsych.2007.09.008 [DOI] [PubMed] [Google Scholar]
- Chandler S. P., Kansagra P., Hirst M. C. (2003). Fragile X (CGG)n repeats induce a transcriptional repression in cis upon a linked promoter: evidence for a chromatin mediated effect. BMC Mol. Biol. 4:3. 10.1186/1471-2199-4-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Changizi M. A., Shimojo S. (2005). Parcellation and area-area connectivity as a function of neocortex size. Brain Behav. Evol. 66, 88–98. 10.1159/000085942 [DOI] [PubMed] [Google Scholar]
- Chaplin T. A., Yu H. H., Soares J. G., Gattass R., Rosa M. G. (2013). A conserved pattern of differential expansion of cortical areas in simian primates. J. Neurosci. 33, 15120–15125. 10.1523/JNEUROSCI.2909-13.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaste P., Betancur C., Gerard-Blanluet M., Bargiacchi A., Kuzbari S., Drunat S., et al. (2012). High-functioning autism spectrum disorder and fragile X syndrome: report of two affected sisters. Mol. Autism 3:5. 10.1186/2040-2392-3-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterjee N., Lin Y., Santillan B. A., Yotnda P., Wilson J. H. (2015). Environmental stress induces trinucleotide repeat mutagenesis in human cells. Proc. Natl. Acad. Sci. U S A 112, 3764–3769. 10.1073/pnas.1421917112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chauhan A., Chauhan V. (2006). Oxidative stress in autism. Pathophysiology 13, 171–181. 10.1016/j.pathophys.2006.05.007 [DOI] [PubMed] [Google Scholar]
- Chen H. C., Kaplan G., Rogers L. J. (2009). Contact calls of common marmosets (Callithrix jacchus): influence of age of caller on antiphonal calling and other vocal responses. Am. J. Primatol. 71, 165–170. 10.1002/ajp.20636 [DOI] [PubMed] [Google Scholar]
- Chen T., Lu J. S., Song Q., Liu M. G., Koga K., Descalzi G., et al. (2014). Pharmacological rescue of cortical synaptic and network potentiation in a mouse model for fragile X syndrome. Neuropsychopharmacology 39, 1955–1967. 10.1038/npp.2014.44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X., Sun W., Pan Y., Yang Q., Cao K., Zhang J., et al. (2013). Lithium ameliorates open-field and elevated plus maze behaviors and brain phospho-glycogen synthase kinase 3-β expression in fragile X syndrome model mice. Neurosciences 18, 356–362. [PubMed] [Google Scholar]
- Chen Y., Tassone F., Berman R. F., Hagerman P. J., Hagerman R. J., Willemsen R., et al. (2010). Murine hippocampal neurons expressing Fmr1 gene premutations show early developmental deficits and late degeneration. Hum. Mol. Genet. 19, 196–208. 10.1093/hmg/ddp479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Zheng Y., Kang Y., Yang W., Niu Y., Guo X., et al. (2015). Functional disruption of the dystrophin gene in rhesus monkey using CRISPR/Cas9. Hum. Mol. Genet. 24, 3764–3774. 10.1093/hmg/ddv120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng C., Lau S. K. M., Doering L. C. (2016). Astrocyte-secreted thrombospondin-1 modulates synapse and spine defects in the fragile X mouse model. Mol. Brain 9:74. 10.1186/s13041-016-0256-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Y., Ma Z., Kim B.-H., Wu W., Cayting P., Boyle A. P., et al. (2014). Principles of regulatory information conservation between mouse and human. Nature 515, 371–375. 10.1038/nature13985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiurazzi P., Pomponi M. G., Willemsen R., Oostra B. A., Neri G. (1998). in vitro reactivation of the FMR1 gene involved in fragile X syndrome. Hum. Mol. Genet. 7, 109–113. 10.1093/hmg/7.1.109 [DOI] [PubMed] [Google Scholar]
- Choi C. H., Schoenfeld B. P., Bell A. J., Hinchey P., Kollaros M., Gertner M. J., et al. (2011). Pharmacological reversal of synaptic plasticity deficits in the mouse model of fragile X syndrome by group II mGluR antagonist or lithium treatment. Brain Res. 1380, 106–119. 10.1016/j.brainres.2010.11.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi C. H., Schoenfeld B. P., Bell A. J., Hinchey J., Rosenfelt C., Gertner M. J., et al. (2016). Multiple drug treatments that increase cAMP signaling restore long-term memory and aberrant signaling in fragile X syndrome models. Front. Behav. Neurosci. 10:136. 10.3389/fnbeh.2016.00136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi C. H., Schoenfeld B. P., Weisz E. D., Bell A. J., Chambers D. B., Hinchey J., et al. (2015). PDE-4 inhibition rescues aberrant synaptic plasticity in Drosophila and mouse models of fragile X syndrome. J. Neurosci. 35, 396–408. 10.1523/JNEUROSCI.1356-12.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi J. Y., Takahashi D. Y., Ghazanfar A. A. (2015). Cooperative vocal control in marmoset monkeys via vocal feedback. J. Neurophysiol. 114, 274–283. 10.1152/jn.00228.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow C. P., Mitchell J. F., Miller C. T. (2015). Vocal turn-taking in a non-human primate is learned during ontogeny. Proc. Biol. Sci. 282:20150069. 10.1098/rspb.2015.0069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuang S. C., Zhao W., Bauchwitz R., Yan Q., Bianchi R., Wong R. K. (2005). Prolonged epileptiform discharges induced by altered group I metabotropic glutamate receptor-mediated synaptic responses in hippocampal slices of a fragile X mouse model. J. Neurosci. 25, 8048–8055. 10.1523/JNEUROSCI.1777-05.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cilli P., Ventura I., Minoprio A., Meccia E., Martire A., Wilson S. H., et al. (2016). Oxidized dNTPs and the OGG1 and MUTYH DNA glycosylases combine to induce CAG/CTG repeat instability. Nucleic Acids Res. 44, 5190–5203. 10.1093/nar/gkw170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark R. E., Squire L. R. (2013). Similarity in form and function of the hippocampus in rodents, monkeys, and humans. Proc. Natl. Acad. Sci. U S A 110, 10365–10370. 10.1073/pnas.1301225110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffee B., Zhang F., Ceman S., Warren S. T., Reines D. (2002). Histone modifications depict an aberrantly heterochromatinized FMR1 gene in fragile x syndrome. Am. J. Hum. Genet. 71, 923–932. 10.1086/342931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffee B., Zhang F., Warren S. T., Reines D. (1999). Acetylated histones are associated with FMR1 in normal but not fragile X-syndrome cells. Nat. Genet. 22, 98–101. 10.1038/8807 [DOI] [PubMed] [Google Scholar]
- Cohen I. L., Fisch G. S., Sudhalter V., Wolf-Schein E. G., Hanson D., Hagerman R., et al. (1988). Social gaze, social avoidance, and repetitive behavior in fragile X males: a controlled study. Am. J. Ment. Retard. 92, 436–446. [PubMed] [Google Scholar]
- Colak D., Zaninovic N., Cohen M. S., Rosenwaks Z., Yang W. Y., Gerhardt J., et al. (2014). Promoter-bound trinucleotide repeat mRNA drives epigenetic silencing in fragile X syndrome. Science 343, 1002–1005. 10.1126/science.1245831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colombo J. A. (1996). Interlaminar astroglial processes in the cerebral cortex of adult monkeys but not of adult rats. Acta Anat. 155, 57–62. 10.1159/000147790 [DOI] [PubMed] [Google Scholar]
- Colombo J. A., Fuchs E., Härtig W., Marotte L. R., Puissant V. (2000). “Rodent-like” and “primate-like” types of astroglial architecture in the adult cerebral cortex of mammals: a comparative study. Anat. Embryol. 201, 111–120. 10.1007/pl00008231 [DOI] [PubMed] [Google Scholar]
- Colombo J. A., Gayol S., Yañez A., Marco P. (1997). Immunocytochemical and electron microscope observations on astroglial interlaminar processes in the primate neocortex. J. Neurosci. Res. 48, 352–357. [DOI] [PubMed] [Google Scholar]
- Coors M. E., Glover J. J., Juengst E. T., Sikela J. M. (2010). The ethics of using transgenic non-human primates to study what makes us human. Nat. Rev. Genet. 11, 658–662. 10.1038/nrg2864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordeiro L., Ballinger E., Hagerman R., Hessl D. (2011). Clinical assessment of DSM-IV anxiety disorders in fragile X syndrome: prevalence and characterization. J. Neurodev. Disord. 3, 57–67. 10.1007/s11689-010-9067-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornish K., Munir F., Wilding J. (2001). A neuropsychological and behavioural profile of attention deficits in fragile X syndrome. Rev. Neurol. 33, S24–S29. [PubMed] [Google Scholar]
- Costa L., Sardone L. M., Lacivita E., Leopoldo M., Ciranna L. (2015). Novel agonists for serotonin 5-HT7 receptors reverse metabotropic glutamate receptor-mediated long-term depression in the hippocampus of wild-type and Fmr1 KO mice, a model of fragile X syndrome. Front. Behav. Neurosci. 9:65. 10.3389/fnbeh.2015.00065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa L., Spatuzza M., D’Antoni S., Bonaccorso C. M., Trovato C., Musumeci S. A., et al. (2012). Activation of 5-HT7 serotonin receptors reverses metabotropic glutamate receptor-mediated synaptic plasticity in wild-type and Fmr1 knockout mice, a model of Fragile X syndrome. Biol. Psychiatry 72, 924–933. 10.1016/j.biopsych.2012.06.008 [DOI] [PubMed] [Google Scholar]
- Cowley B., Kirjanen S., Partanen J., Castrén M. L. (2016). Epileptic electroencephalography profile associates with attention problems in children with fragile X syndrome: review and case series. Front. Hum. Neurosci. 10:353. 10.3389/fnhum.2016.00353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuadrado M., Sacristan M., Antequera F. (2001). Species-specific organization of CpG island promoters at mammalian homologous genes. EMBO Rep. 2, 586–592. 10.1093/embo-reports/kve131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham C. L., Martínez Cerdeño V., Navarro Porras E., Prakash A. N., Angelastro J. M., Willemsen R., et al. (2011). Premutation CGG-repeat expansion of the Fmr1 gene impairs mouse neocortical development. Hum. Mol. Genet. 20, 64–79. 10.1093/hmg/ddq432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curia G., Papouin T., Seguela P., Avoli M. (2009). Downregulation of tonic GABAergic inhibition in a mouse model of fragile X syndrome. Cereb. Cortex 19, 1515–1520. 10.1093/cercor/bhn159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyranoski D. (2004). China takes steps to secure pole position in primate research. Nature 432:3. 10.1038/432003a [DOI] [PubMed] [Google Scholar]
- Dahlhaus R., El-Husseini A. (2010). Altered neuroligin expression is involved in social deficits in a mouse model of the fragile X syndrome. Behav. Brain Res. 208, 96–105. 10.1016/j.bbr.2009.11.019 [DOI] [PubMed] [Google Scholar]
- Dalton K. M., Holsen L., Abbeduto L., Davidson R. J. (2008). Brain function and gaze fixation during facial-emotion processing in fragile X and autism. Autism Res. 1, 231–239. 10.1002/aur.32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darnell J. C., Van Driesche S. J., Zhang C., Hung K. Y., Mele A., Fraser C. E., et al. (2011). FMRP stalls ribosomal translocation on mRNAs linked to synaptic function and autism. Cell 146, 247–261. 10.1016/j.cell.2011.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Datta S., Alam M. P., Majumdar S. S., Mehta A. K., Maiti S., Wadhwa N., et al. (2011). Nucleosomal occupancy and CGG repeat expansion: a comparative analysis of triplet repeat region from mouse and human fragile X mental retardation gene 1. Chromosome Res. 19, 445–455. 10.1007/s10577-011-9206-7 [DOI] [PubMed] [Google Scholar]
- Davidovic L., Navratil V., Bonaccorso C. M., Catania M. V., Bardoni B., Dumas M. E. (2011). A metabolomic and systems biology perspective on the brain of the fragile X syndrome mouse model. Genome Res. 21, 2190–2202. 10.1101/gr.116764.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Boer R. A., Overduin-de Vries A. M., Louwerse A. L., Sterck E. H. (2013). The behavioral context of visual displays in common marmosets (Callithrix jacchus). Am. J. Primatol. 75, 1084–1095. 10.1002/ajp.22167 [DOI] [PubMed] [Google Scholar]
- Decasien A. R., Williams S. A., Higham J. P. (2017). Primate brain size is predicted by diet but not sociality. Nat. Ecol. Evol. 1:112. 10.1038/s41559-017-0112 [DOI] [PubMed] [Google Scholar]
- de Esch C. E., Ghazvini M., Loos F., Schelling-Kazaryan N., Widagdo W., Munshi S. T., et al. (2014). Epigenetic characterization of the FMR1 promoter in induced pluripotent stem cells from human fibroblasts carrying an unmethylated full mutation. Stem Cell Rep. 3, 548–555. 10.1016/j.stemcr.2014.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Esch C. E., van Den Berg W. E., Buijsen R. A., Jaafar I. A., Nieuwenhuizen-Bakker I. M., Gasparini F., et al. (2015). Fragile X mice have robust mGluR5-dependent alterations of social behaviour in the Automated Tube Test. Neurobiol. Dis. 75, 31–39. 10.1016/j.nbd.2014.12.021 [DOI] [PubMed] [Google Scholar]
- de la Mothe L. A., Blumell S., Kajikawa Y., Hackett T. A. (2012). Cortical connections of auditory cortex in marmoset monkeys: lateral belt and parabelt regions. Anat. Rec. Hoboken 295, 800–821. 10.1002/ar.22451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Moraes B. L., Da Silva Souto A., Schiel N. (2014). Adaptability in stone tool use by wild capuchin monkeys (Sapajus libidinosus). Am. J. Primatol. 76, 967–977. 10.1002/ajp.22286 [DOI] [PubMed] [Google Scholar]
- De Rubeis S., Bagni C. (2010). Fragile X mental retardation protein control of neuronal mRNA metabolism: insights into mRNA stability. Mol. Cell. Neurosci. 43, 43–50. 10.1016/j.mcn.2009.09.013 [DOI] [PubMed] [Google Scholar]
- de Vries B. B., Wiegers A. M., Smits A. P., Mohkamsing S., Duivenvoorden H. J., Fryns J. P., et al. (1996). Mental status of females with an FMR1 gene full mutation. Am. J. Hum. Genet. 58, 1025–1032. [PMC free article] [PubMed] [Google Scholar]
- de Vrij F. M., Levenga J., van der Linde H. C., Koekkoek S. K., De Zeeuw C. I., Nelson D. L., et al. (2008). Rescue of behavioral phenotype and neuronal protrusion morphology in Fmr1 KO mice. Neurobiol. Dis. 31, 127–132. 10.1016/j.nbd.2008.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dell’Mour V., Range F., Huber L. (2009). Social learning and mother’s behavior in manipulative tasks in infant marmosets. Am. J. Primatol. 71, 503–509. 10.1002/ajp.20682 [DOI] [PubMed] [Google Scholar]
- Demetrius L. (2006). Aging in mouse and human systems: a comparative study. Ann. N Y Acad. Sci. 1067, 66–82. 10.1196/annals.1354.010 [DOI] [PubMed] [Google Scholar]
- Deng P. Y., Klyachko V. A. (2016). Genetic upregulation of BK channel activity normalizes multiple synaptic and circuit defects in a mouse model of fragile X syndrome. J. Physiol. 594, 83–97. 10.1113/JP271031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng P. Y., Rotman Z., Blundon J. A., Cho Y., Cui J., Cavalli V., et al. (2013). FMRP regulates neurotransmitter release and synaptic information transmission by modulating action potential duration via BK channels. Neuron 77, 696–711. 10.1016/j.neuron.2013.03.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennery P. A. (2007). Effects of oxidative stress on embryonic development. Birth Defects Res. C Embryo Today 81, 155–162. 10.1002/bdrc.20098 [DOI] [PubMed] [Google Scholar]
- Derlig K., Gießl A., Brandstätter J. H., Enz R., Dahlhaus R. (2013). Identification and characterisation of simiate, a novel protein linked to the fragile X syndrome. PLoS One 8:e83007. 10.1371/journal.pone.0083007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derreumaux S., Chaoui M., Tevanian G., Fermandjian S. (2001). Impact of CpG methylation on structure, dynamics and solvation of cAMP DNA responsive element. Nucleic Acids Res. 29, 2314–2326. 10.1093/nar/29.11.2314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desai N. S., Casimiro T. M., Gruber S. M., Vanderklish P. W. (2006). Early postnatal plasticity in neocortex of Fmr1 knockout mice. J. Neurophysiol. 96, 1734–1745. 10.1152/jn.00221.2006 [DOI] [PubMed] [Google Scholar]
- Devys D., Biancalana V., Rousseau F., Boué J., Mandel J. L., Oberlé I. (1992). Analysis of full fragile X mutations in fetal tissues and monozygotic twins indicate that abnormal methylation and somatic heterogeneity are established early in development. Am. J. Med. Genet. 43, 208–216. 10.1002/ajmg.1320430134 [DOI] [PubMed] [Google Scholar]
- Devys D., Lutz Y., Rouyer N., Bellocq J. P., Mandel J. L. (1993). The FMR-1 protein is cytoplasmic, most abundant in neurons and appears normal in carriers of a fragile X premutation. Nat. Genet. 4, 335–340. 10.1038/ng0893-335 [DOI] [PubMed] [Google Scholar]
- D’Hooge R., Nagels G., Franck F., Bakker C. E., Reyniers E., Storm K., et al. (1997). Mildly impaired water maze performance in male Fmr1 knockout mice. Neuroscience 76, 367–376. 10.1016/s0306-4522(96)00224-2 [DOI] [PubMed] [Google Scholar]
- D’Hulst C., De Geest N., Reeve S. P., Van Dam D., De Deyn P. P., Hassan B. A., et al. (2006). Decreased expression of the GABAA receptor in fragile X syndrome. Brain Res. 22, 238–245. 10.1016/j.brainres.2006.08.115 [DOI] [PubMed] [Google Scholar]
- Dicke U., Roth G. (2016). Neuronal factors determining high intelligence. Philos. Trans. R. Soc. Lond. B Biol. Sci. 371:20150180. 10.1098/rstb.2015.0180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dictenberg J. B., Swanger S. A., Antar L. N., Singer R. H., Bassell G. J. (2008). A direct role for FMRP in activity-dependent dendritic mRNA transport links filopodial-spine morphogenesis to fragile X syndrome. Dev. Cell 14, 926–939. 10.1016/j.devcel.2008.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Didiot M. C., Tian Z. X., Schaeffer C., Subramanian M., Mandel J. L., Moine H. (2008). The G-quartet containing FMRP binding site in FMR1 mRNA is a potent exonic splicing enhancer. Nucleic Acids Res. 36, 4902–4912. 10.1093/nar/gkn472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diester I., Nieder A. (2010). Numerical values leave a semantic imprint on associated signs in monkeys. J. Cogn. Neurosci. 22, 174–183. 10.1162/jocn.2009.21193 [DOI] [PubMed] [Google Scholar]
- Digby L. J., Barreto C. E. (1993). Social organization in a wild population of Callithrix jacchus. I. Group composition and dynamics. Folia Primatol. 61, 123–134. 10.1159/000156739 [DOI] [PubMed] [Google Scholar]
- Doers M. E., Musser M. T., Nichol R., Berndt E. R., Baker M., Gomez T. M., et al. (2014). iPSC-derived forebrain neurons from FXS individuals show defects in initial neurite outgrowth. Stem Cells Dev. 23, 1777–1787. 10.1089/scd.2014.0030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolan B. M., Duron S. G., Campbell D. A., Vollrath B., Shankaranarayana Rao B. S., Ko H. Y., et al. (2013). Rescue of fragile X syndrome phenotypes in Fmr1 KO mice by the small-molecule PAK inhibitor FRAX486. Proc. Natl. Acad. Sci. U S A 110, 5671–5676. 10.1073/pnas.1219383110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolen G., Osterweil E., Rao B. S., Smith G. B., Auerbach B. D., Chattarji S., et al. (2007). Correction of fragile X syndrome in mice. Neuron 56, 955–962. 10.1016/j.neuron.2007.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolenšek J., Rupnik M. S., Stožer A. (2015). Structural similarities and differences between the human and the mouse pancreas. Islets 7:e1024405. 10.1080/19382014.2015.1024405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolskiy A. A., Pustylnyak V. O., Yarushkin A. A., Lemskaya N. A., Yudkin D. V. (2017). Inhibitors of histone deacetylases are weak activators of the FMR1 gene in fragile X syndrome cell lines. Biomed Res. Int. 2017:3582601. 10.1155/2017/3582601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dombrowski C., Levesque S., Morel M. L., Rouillard P., Morgan K., Rousseau F. (2002). Premutation and intermediate-size FMR1 alleles in 10572 males from the general population: loss of an AGG interruption is a late event in the generation of fragile X syndrome alleles. Hum. Mol. Genet. 11, 371–378. 10.1093/hmg/11.4.371 [DOI] [PubMed] [Google Scholar]
- Donohoue P. D., Barrangou R., May A. P. (2017). Advances in industrial biotechnology using CRISPR-cas systems. Trends Biotechnol. 36, 134–146. 10.1016/j.tibtech.2017.07.007 [DOI] [PubMed] [Google Scholar]
- Du X., Cui J., Wang C., Huo X., Lu J., Li Y., et al. (2013). Detected microsatellite polymorphisms in genetically altered inbred mouse strains. Mol. Genet. Genomics 288, 309–316. 10.1007/s00438-013-0751-y [DOI] [PubMed] [Google Scholar]
- Durdiaková J., Lakatošová S., Kubranská A., Laznibatová J., Ficek A., Ostatniková D., et al. (2013). Mental rotation in intellectually gifted boys is affected by the androgen receptor CAG repeat polymorphism. Neuropsychologia 51, 1693–1698. 10.1016/j.neuropsychologia.2013.05.016 [DOI] [PubMed] [Google Scholar]
- Dutta S., Sengupta P. (2016). Men and mice: relating their ages. Life Sci. 152, 244–248. 10.1016/j.lfs.2015.10.025 [DOI] [PubMed] [Google Scholar]
- Dy A. B. C., Tassone F., Eldeeb M., Salcedo-Arellano M. J., Tartaglia N., Hagerman R. (2018). Metformin as targeted treatment in fragile X syndrome. Clin. Genet. 93, 216–222. 10.1007/978-3-642-21649-7_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyer-Friedman J., Glaser B., Hessl D., Johnston C., Huffman L. C., Taylor A., et al. (2002). Genetic and environmental influences on the cognitive outcomes of children with fragile X syndrome. J. Am. Acad. Child Adolesc. Psychiatry 41, 237–244. 10.1097/00004583-200203000-00002 [DOI] [PubMed] [Google Scholar]
- Dykens E. M., Hodapp R. M., Leckman J. F. (1987). Strengths and weaknesses in the intellectual functioning of males with fragile X syndrome. Am. J. Ment. Defic. 92, 234–236. [PubMed] [Google Scholar]
- Eberhart D. E., Malter H. E., Feng Y., Warren S. T. (1996). The fragile X mental retardation protein is a ribonucleoprotein containing both nuclear localization and nuclear export signals. Hum. Mol. Genet. 5, 1083–1091. 10.1093/hmg/5.8.1083 [DOI] [PubMed] [Google Scholar]
- Eichler E. E., Holden J. J., Popovich B. W., Reiss A. L., Snow K., Thibodeau S. N., et al. (1994). Length of uninterrupted CGG repeats determines instability in the FMR1 gene. Nat. Genet. 8, 88–94. 10.1038/ng0994-88 [DOI] [PubMed] [Google Scholar]
- Eiges R., Urbach A., Malcov M., Frumkin T., Schwartz T., Amit A., et al. (2007). Developmental study of fragile X syndrome using human embryonic stem cells derived from preimplantation genetically diagnosed embryos. Cell Stem Cell 1, 568–577. 10.1016/j.stem.2007.09.001 [DOI] [PubMed] [Google Scholar]
- Eilam D. (2014). Of mice and men: building blocks in cognitive mapping. Neurosci. Biobehav. Rev. 47, 393–409. 10.1016/j.neubiorev.2014.09.010 [DOI] [PubMed] [Google Scholar]
- Elefteriou F., Yang X. (2011). Genetic mouse models for bone studies—strengths and limitations. Bone 49, 1242–1254. 10.1016/j.bone.2011.08.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elston G. N., Benavides-Piccione R., Elston A., Zietsch B., Defelipe J., Manger P., et al. (2006). Specializations of the granular prefrontal cortex of primates: implications for cognitive processing. Anat. Rec. A Discov. Mol. Cell. Evol. Biol. 288, 26–35. 10.1002/ar.a.20278 [DOI] [PubMed] [Google Scholar]
- Engineer C. T., Centanni T. M., Im K. W., Rahebi K. C., Buell E. P., Kilgard M. P. (2014). Degraded speech sound processing in a rat model of fragile X syndrome. Brain Res. 20, 72–84. 10.1016/j.brainres.2014.03.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Entezam A., Biacsi R., Orrison B., Saha T., Hoffman G. E., Grabczyk E., et al. (2007). Regional FMRP deficits and large repeat expansions into the full mutation range in a new Fragile X premutation mouse model. Gene 395, 125–134. 10.1016/j.gene.2007.02.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epple G. (1968). Comparative studies on vocalization in marmoset monkeys (Hapalidae). Folia Primatol. 8, 1–40. 10.1159/000155129 [DOI] [PubMed] [Google Scholar]
- Epple G. (1970). Quantitative studies on scent marking in the marmoset (Callithrix jacchus). Folia Primatol. 13, 48–62. 10.1159/000155308 [DOI] [PubMed] [Google Scholar]
- Estes P. S., O’Shea M., Clasen S., Zarnescu D. C. (2008). Fragile X protein controls the efficacy of mRNA transport in Drosophila neurons. Mol. Cell. Neurosci. 39, 170–179. 10.1016/j.mcn.2008.06.012 [DOI] [PubMed] [Google Scholar]
- European Commission (2010). Seventh Report on the Statistics on the Number of Animals Used for Experimental and Other Scientific Purposes in the Member States of the European Union SEC(2010) 1107/final 2. Brussels: European Commission; Available online at: http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=SWD:2013:0497:FIN:EN:PDF [Google Scholar]
- Evans T. A., Beran M. J. (2012). Monkeys exhibit prospective memory in a computerized task. Cognition 125, 131–140. 10.1016/j.cognition.2012.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan W. (2013). Group I metabotropic glutamate receptors modulate late phase long-term potentiation in hippocampal CA1 pyramidal neurons: comparison of apical and basal dendrites. Neurosci. Lett. 553, 132–137. 10.1016/j.neulet.2013.08.030 [DOI] [PubMed] [Google Scholar]
- Feng Y., Gutekunst C. A., Eberhart D. E., Yi H., Warren S. T., Hersch S. M. (1997). Fragile X mental retardation protein: nucleocytoplasmic shuttling and association with somatodendritic ribosomes. J. Neurosci. 17, 1539–1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferron L., Nieto-Rostro M., Cassidy J. S., Dolphin A. C. (2014). Fragile X mental retardation protein controls synaptic vesicle exocytosis by modulating N-type calcium channel density. Nat. Commun. 5:3628. 10.1038/ncomms4628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch C. E., Austad S. N. (2015). Commentary: is Alzheimer’s disease uniquely human? Neurobiol. Aging 36, 553–555. 10.1016/j.neurobiolaging.2014.10.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkel T., Holbrook N. J. (2000). Oxidants, oxidative stress and the biology of ageing. Nature 408, 239–247. 10.1038/35041687 [DOI] [PubMed] [Google Scholar]
- Fleming K., Riser D. K., Kumari D., Usdin K. (2003). Instability of the fragile X syndrome repeat in mice: the effect of age, diet and mutations in genes that affect DNA replication, recombination and repair proficiency. Cytogenet Genome Res. 100, 140–146. 10.1159/000072848 [DOI] [PubMed] [Google Scholar]
- Francesconi W., Cammalleri M., Sanna P. (2004). The metabotropic glutamate receptor 5 is necessary for late-phase long-term potentiation in the hippocampal CA1 region. Brain Res. 1022, 12–18. 10.1016/j.brainres.2004.06.060 [DOI] [PubMed] [Google Scholar]
- Franklin A. V., King M. K., Palomo V., Martinez A., McMahon L. L., Jope R. S. (2014). Glycogen synthase kinase-3 inhibitors reverse deficits in long-term potentiation and cognition in fragile X mice. Biol. Psychiatry 75, 198–206. 10.1016/j.biopsych.2013.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freudenreich C. H., Stavenhagen J. B., Zakian V. A. (1997). Stability of a CTG/CAG trinucleotide repeat in yeast is dependent on its orientation in the genome. Mol. Cell. Biol. 17, 2090–2098. 10.1128/mcb.17.4.2090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freund L. S., Reiss A. L., Abrams M. T. (1993). Psychiatric disorders associated with fragile X in the young female. Pediatrics 91, 321–329. [PubMed] [Google Scholar]
- Frey U., Huang Y. Y., Kandel E. R. (1993). Effects of cAMP simulate a late stage of LTP in hippocampal CA1 neurons. Science 260, 1661–1664. 10.1126/science.8389057 [DOI] [PubMed] [Google Scholar]
- Frey S., Mackey S., Petrides M. (2014). Cortico-cortical connections of areas 44 and 45B in the macaque monkey. Brain Lang. 131, 36–55. 10.1016/j.bandl.2013.05.005 [DOI] [PubMed] [Google Scholar]
- Fry M., Loeb L. A. (1994). The fragile X syndrome d(CGG)n nucleotide repeats form a stable tetrahelical structure. Proc. Natl. Acad. Sci. U S A 91, 4950–4954. 10.1073/pnas.91.11.4950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frye R. E., Casanova M. F., Fatemi S. H., Folsom T. D., Reutiman T. J., Brown G. L., et al. (2016). Neuropathological mechanisms of seizures in autism spectrum disorder. Front. Neurosci. 10:192. 10.3389/fnins.2016.00192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu A. Q., Genereux D. P., Stoger R., Burden A. F., Laird C. D., Stephens M. (2012). Statistical inference of in vivo properties of human DNA methyltransferases from double-stranded methylation patterns. PLoS One 7:19. 10.1371/journal.pone.0032225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu Y. H., Kuhl D. P., Pizzuti A., Pieretti M., Sutcliffe J. S., Richards S., et al. (1991). Variation of the CGG repeat at the fragile X site results in genetic instability: resolution of the Sherman paradox. Cell 67, 1047–1058. 10.1016/0092-8674(91)90283-5 [DOI] [PubMed] [Google Scholar]
- Fukuda H., Katahira M., Tanaka E., Enokizono Y., Tsuchiya N., Higuchi K., et al. (2005). Unfolding of higher DNA structures formed by the d(CGG) triplet repeat by UP1 protein. Genes Cells 10, 953–962. 10.1111/j.1365-2443.2005.00896.x [DOI] [PubMed] [Google Scholar]
- Fukuda K., Ichiyanagi K., Yamada Y., Go Y., Udono T., Wada S., et al. (2013). Regional DNA methylation differences between humans and chimpanzees are associated with genetic changes, transcriptional divergence and disease genes. J. Hum. Genet. 58, 446–454. 10.1038/jhg.2013.55 [DOI] [PubMed] [Google Scholar]
- Gagne M., Levesque K., Nutile L., Locurto C. (2012). Performance on patterned string problems by common marmosets (Callithrix jacchus). Anim. Cogn. 15, 1021–1030. 10.1007/s10071-012-0511-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gama-Sosa M. A., Midgett R. M., Slagel V. A., Githens S., Kuo K. C., Gehrke C. W., et al. (1983). Tissue-specific differences in DNA methylation in various mammals. Biochim. Biophys. Acta 740, 212–219. 10.1016/0167-4781(83)90079-9 [DOI] [PubMed] [Google Scholar]
- Gandhi R. M., Kogan C. S., Messier C. (2014). 2-Methyl-6-(phenylethynyl) pyridine (MPEP) reverses maze learning and PSD-95 deficits in Fmr1 knock-out mice. Front. Cell. Neurosci. 8:70. 10.3389/fncel.2014.00070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gantois I., Khoutorsky A., Popic J., Aguilar-Valles A., Freemantle E., Cao R., et al. (2017). Metformin ameliorates core deficits in a mouse model of fragile X syndrome. Nat. Med. 23, 674–677. 10.1038/nm.4335 [DOI] [PubMed] [Google Scholar]
- Gantois I., Pop A. S., de Esch C. E., Buijsen R. A., Pooters T., Gomez-Mancilla B., et al. (2013). Chronic administration of AFQ056/Mavoglurant restores social behaviour in Fmr1 knockout mice. Behav. Brain Res. 239, 72–79. 10.1016/j.bbr.2012.10.059 [DOI] [PubMed] [Google Scholar]
- Gaudissard J., Ginger M., Premoli M., Memo M., Frick A., Pietropaolo S. (2017). Behavioral abnormalities in the Fmr1-KO2 mouse model of fragile X syndrome: the relevance of early life phases. Autism Res. 10, 1584–1596. 10.1002/aur.1814 [DOI] [PubMed] [Google Scholar]
- Geahigan K. B., Meints G. A., Hatcher M. E., Orban J., Drobny G. P. (2000). The dynamic impact of CpG methylation in DNA. Biochemistry 39, 4939–4946. 10.1021/bi9917636 [DOI] [PubMed] [Google Scholar]
- Gentry M., Meyer P. (2013). An 11bp region with stem formation potential is essential for de novo DNA methylation of the RPS element. PLoS One 8:e63652. 10.1371/journal.pone.0063652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerhardt J. (2017). Epigenetic modifications in human fragile X pluripotent stem cells; Implications in fragile X syndrome modeling. Brain Res. 1656, 55–62. 10.1016/j.brainres.2015.10.004 [DOI] [PubMed] [Google Scholar]
- Gerra G., Garofano L., Pellegrini C., Bosari S., Zaimovic A., Moi G., et al. (2005). Allelic association of a dopamine transporter gene polymorphism with antisocial behaviour in heroin-dependent patients. Addict. Biol. 10, 275–281. 10.1080/13556210500223769 [DOI] [PubMed] [Google Scholar]
- Gharib S. A., Nguyen E., Altemeier W. A., Shaffer S. A., Doneanu C. E., Goodlett D. R., et al. (2010). Of mice and men: comparative proteomics of bronchoalveolar fluid. Eur. Respir. J. 35, 1388–1395. 10.1183/09031936.00089409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghazanfar A. A., Morrill R. J., Kayser C. (2013). Monkeys are perceptually tuned to facial expressions that exhibit a theta-like speech rhythm. Proc. Natl. Acad. Sci. U S A 110, 1959–1963. 10.1073/pnas.1214956110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghazanfar A. A., Zhang Y. S. (2016). The autonomic nervous system is the engine for vocal development through social feedback. Curr. Opin. Neurobiol. 40, 155–160. 10.1016/j.conb.2016.07.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghilan M., Hryciw B. N., Brocardo P. S., Bostrom C. A., Gil-Mohapel J., Christie B. R. (2015). Enhanced corticosteroid signaling alters synaptic plasticity in the dentate gyrus in mice lacking the fragile X mental retardation protein. Neurobiol. Dis. 77, 26–34. 10.1016/j.nbd.2015.01.008 [DOI] [PubMed] [Google Scholar]
- Gholizadeh S., Arsenault J., Xuan I. C., Pacey L. K., Hampson D. R. (2014). Reduced phenotypic severity following adeno-associated virus-mediated Fmr1 gene delivery in fragile X mice. Neuropsychopharmacology 39, 3100–3111. 10.1038/npp.2014.167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gholizadeh S., Halder S. K., Hampson D. R. (2015). Expression of fragile X mental retardation protein in neurons and glia of the developing and adult mouse brain. Brain Res. 30, 22–30. 10.1016/j.brainres.2014.11.023 [DOI] [PubMed] [Google Scholar]
- Gibson J. R., Bartley A. F., Hays S. A., Huber K. M. (2008). Imbalance of neocortical excitation and inhibition and altered UP states reflect network hyperexcitability in the mouse model of fragile X syndrome. J. Neurophysiol. 100, 2615–2626. 10.1152/jn.90752.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginno P. A., Lim Y. W., Lott P. L., Korf I., Chedin F. (2013). GC skew at the 5′ and 3′ ends of human genes links R-loop formation to epigenetic regulation and transcription termination. Genome Res. 23, 1590–1600. 10.1101/gr.158436.113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginno P. A., Lott P. L., Christensen H. C., Korf I., Chedin F. (2012). R-loop formation is a distinctive characteristic of unmethylated human CpG island promoters. Mol. Cell 45, 814–825. 10.1016/j.molcel.2012.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gkogkas C. G., Khoutorsky A., Cao R., Jafarnejad S. M., Prager-Khoutorsky M., Giannakas N., et al. (2014). Pharmacogenetic inhibition of eIF4E-dependent Mmp9 mRNA translation reverses fragile X syndrome-like phenotypes. Cell Rep. 9, 1742–1755. 10.1016/j.celrep.2014.10.064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaser B., Hessl D., Dyer-Friedman J., Johnston C., Wisbeck J., Taylor A., et al. (2003). Biological and environmental contributions to adaptive behavior in fragile X syndrome. Am. J. Med. Genet. A 15, 21–29. 10.1002/ajmg.a.10549 [DOI] [PubMed] [Google Scholar]
- Gläser D., Wöhrle D., Salat U., Vogel W., Steinbach P. (1999). Mitotic behavior of expanded CGG repeats studied on cultured cells: further evidence for methylation-mediated triplet repeat stability in fragile X syndrome. Am. J. Med. Genet. 84, 226–228. [DOI] [PubMed] [Google Scholar]
- Godfraind J. M., Reyniers E., De Boulle K., D’Hooge R., De Deyn P. P., Bakker C. E., et al. (1996). Long-term potentiation in the hippocampus of fragile X knockout mice. Am. J. Med. Genet. 64, 246–251. [DOI] [PubMed] [Google Scholar]
- Goebel-Goody S. M., Wilson-Wallis E. D., Royston S., Tagliatela S. M., Naegele J. R., Lombroso P. J. (2012). Genetic manipulation of STEP reverses behavioral abnormalities in a fragile X syndrome mouse model. Genes Brain Behav. 11, 586–600. 10.1111/j.1601-183x.2012.00781.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman-Rakic P. S. (1988). Topography of cognition: parallel distributed networks in primate association cortex. Annu. Rev. Neurosci. 11, 137–156. 10.1146/annurev.neuro.11.1.137 [DOI] [PubMed] [Google Scholar]
- Goncalves J. T., Anstey J. E., Golshani P., Portera-Cailliau C. (2013). Circuit level defects in the developing neocortex of Fragile X mice. Nat. Neurosci. 16, 903–909. 10.1038/nn.3415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman J., Chandna A., Roe K. (2015). Trends in animal use at US research facilities. J. Med. Ethics 41, 567–569. 10.1136/medethics-2014-102404 [DOI] [PubMed] [Google Scholar]
- Govaerts L. C., Smit A. E., Saris J. J., Vanderwerf F., Willemsen R., Bakker C. E., et al. (2007). Exceptional good cognitive and phenotypic profile in a male carrying a mosaic mutation in the FMR1 gene. Clin. Genet. 72, 138–144. 10.1111/j.1399-0004.2007.00829.x [DOI] [PubMed] [Google Scholar]
- Graham D. M. (2016). Exploring social cognition with marmosets. Lab Anim. (NY) 45:249. 10.1038/laban.1049 [DOI] [PubMed] [Google Scholar]
- Greenberg J., Seltzer M., Baker J., Smith L., Warren S. F., Brady N., et al. (2012). Family environment and behavior problems in children, adolescents, and adults with fragile X syndrome. Am. J. Intellect. Dev. Disabil. 117, 331–346. 10.1352/1944-7558-117.4.331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenough W. T., Klintsova A. Y., Irwin S. A., Galvez R., Bates K. E., Weiler I. J. (2001). Synaptic regulation of protein synthesis and the fragile X protein. Proc. Natl. Acad. Sci. U S A 98, 7101–7106. 10.1073/pnas.141145998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groh M., Lufino M. M., Wade-Martins R., Gromak N. (2014). R-loops associated with triplet repeat expansions promote gene silencing in Friedreich ataxia and fragile X syndrome. PLoS Genet. 10:e1004318. 10.1371/journal.pgen.1004318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross C., Chang C. W., Kelly S. M., Bhattacharya A., McBride S. M., Danielson S. W., et al. (2015a). Increased expression of the PI3K enhancer PIKE mediates deficits in synaptic plasticity and behavior in fragile X syndrome. Cell Rep. 11, 727–736. 10.1016/j.celrep.2015.03.060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross C., Hoffmann A., Bassell G. J., Berry-Kravis E. M. (2015b). Therapeutic strategies in fragile X syndrome: from bench to bedside and back. Neurotherapeutics 12, 584–608. 10.1007/s13311-015-0355-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross C., Raj N., Molinaro G., Allen A. G., Whyte A. J., Gibson J. R., et al. (2015c). Selective role of the catalytic PI3K subunit p110β in impaired higher order cognition in fragile X syndrome. Cell Rep. 11, 681–688. 10.1016/j.celrep.2015.03.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross C., Nakamoto M., Yao X., Chan C. B., Yim S. Y., Ye K., et al. (2010). Excess phosphoinositide 3-kinase subunit synthesis and activity as a novel therapeutic target in fragile X syndrome. J. Neurosci. 30, 10624–10638. 10.1523/JNEUROSCI.0402-10.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross C., Yao X., Pong D. L., Jeromin A., Bassell G. J. (2011). Fragile X mental retardation protein regulates protein expression and mRNA translation of the potassium channel Kv4.2. J. Neurosci. 31, 5693–5698. 10.1523/JNEUROSCI.6661-10.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunter C., Paradee W., Crawford D. C., Meadows K. A., Newman J., Kunst C. B., et al. (1998). Re-examination of factors associated with expansion of CGG repeats using a single nucleotide polymorphism in FMR1. Hum. Mol. Genet. 7, 1935–1946. 10.1093/hmg/7.12.1935 [DOI] [PubMed] [Google Scholar]
- Guo W., Murthy A. C., Zhang L., Johnson E. B., Schaller E. G., Allan A. M., et al. (2012). Inhibition of GSK3β improves hippocampus-dependent learning and rescues neurogenesis in a mouse model of fragile X syndrome. Hum. Mol. Genet. 21, 681–691. 10.1093/hmg/ddr501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagerman R. J., Hagerman P. (2016). Fragile X-associated tremor/ataxia syndrome—features, mechanisms and management. Nat. Rev. Neurol. 12, 403–412. 10.1038/nrneurol.2016.82 [DOI] [PubMed] [Google Scholar]
- Hagerman R., Hoem G., Hagerman P. (2010). Fragile X and autism: intertwined at the molecular level leading to targeted treatments. Mol. Autism 1:12. 10.1186/2040-2392-1-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagerman R. J., Jackson C., Amiri K., Silverman A. C., O’Connor R., Sobesky W. (1992). Girls with fragile X syndrome: physical and neurocognitive status and outcome. Pediatrics 89, 395–400. [PubMed] [Google Scholar]
- Halder K., Wieland M., Hartig J. S. (2009). Predictable suppression of gene expression by 5′-UTR-based RNA quadruplexes. Nucleic Acids Res. 37, 6811–6817. 10.1093/nar/gkp696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall S. S., Lightbody A. A., Huffman L. C., Lazzeroni L. C., Reiss A. L. (2009). Physiological correlates of social avoidance behavior in children and adolescents with fragile X syndrome. J. Am. Acad. Child Adolesc. Psychiatry 48, 320–329. 10.1097/CHI.0b013e318195bd15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halsey L. G., Bezerra B. M., Souto A. S. (2006). Can wild common marmosets (Callithrix jacchus) solve the parallel strings task? Anim. Cogn. 9, 229–233. 10.1007/s10071-006-0016-9 [DOI] [PubMed] [Google Scholar]
- Hammock E. A., Young L. J. (2005). Microsatellite instability generates diversity in brain and sociobehavioral traits. Science 308, 1630–1634. 10.1126/science.1111427 [DOI] [PubMed] [Google Scholar]
- Han X., Chen M., Wang F., Windrem M., Wang S., Shanz S., et al. (2013). Forebrain engraftment by human glial progenitor cells enhances synaptic plasticity and learning in adult mice. Cell Stem Cell 12, 342–353. 10.1016/j.stem.2012.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handa V., Goldwater D., Stiles D., Cam M., Poy G., Kumari D., et al. (2005). Long CGG-repeat tracts are toxic to human cells: implications for carriers of Fragile X premutation alleles. FEBS Lett. 579, 2702–2708. 10.1016/j.febslet.2005.04.004 [DOI] [PubMed] [Google Scholar]
- Handa V., Saha T., Usdin K. (2003). The fragile X syndrome repeats form RNA hairpins that do not activate the interferon-inducible protein kinase, PKR, but are cut by Dicer. Nucleic Acids Res. 31, 6243–6248. 10.1093/nar/gkg818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handt M., Epplen A., Hoffjan S., Mese K., Epplen J. T., Dekomien G. (2014). Point mutation frequency in the FMR1 gene as revealed by fragile X syndrome screening. Mol. Cell. Probes 28, 279–283. 10.1016/j.mcp.2014.08.003 [DOI] [PubMed] [Google Scholar]
- Hannan A. J. (2012). Tandem repeat polymorphisms: mediators of genetic plasticity, modulators of biological diversity and dynamic sources of disease susceptibility. Adv. Exp. Med. Biol. 769, 1–9. 10.1007/978-1-4614-5434-2_1 [DOI] [PubMed] [Google Scholar]
- Hansen B. C., Gografe S., Pritt S., Jen K. C., McWhirter C. A., Barman S. M., et al. (2017). Ensuring due process in the IACUC and animal welfare setting: considerations in developing noncompliance policies and procedures for institutional animal care and use committees and institutional officials. FASEB J. 31, 4216–4225. 10.1096/fj.201601250R [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen R. S., Gartler S. M., Scott C. R., Chen S. H., Laird C. D. (1992). Methylation analysis of CGG sites in the CpG island of the human FMR1 gene. Hum. Mol. Genet. 1, 571–578. 10.1093/hmg/1.8.571 [DOI] [PubMed] [Google Scholar]
- Hanson D. M., Jackson A. W., III., Hagerman R. J. (1986). Speech disturbances (cluttering) in mildly impaired males with the Martin-Bell/fragile X syndrome. Am. J. Med. Genet. 23, 195–206. 10.1002/ajmg.1320230114 [DOI] [PubMed] [Google Scholar]
- Harlow E. G., Till S. M., Russell T. A., Wijetunge L. S., Kind P., Contractor A. (2010). Critical period plasticity is disrupted in the barrel cortex of FMR1 knockout mice. Neuron 65, 385–398. 10.1016/j.neuron.2010.01.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris E. H., Washburn D. A., Beran M. J., Sevcik R. A. (2007). Rhesus monkeys (Macaca mulatta) select Arabic numerals or visual quantities corresponding to a number of sequentially completed maze trials. Learn. Behav. 35, 53–59. 10.3758/bf03196074 [DOI] [PubMed] [Google Scholar]
- Hartley S. L., Seltzer M. M., Raspa M., Olmstead M., Bishop E., Bailey D. B. (2011). Exploring the adult life of men and women with fragile X syndrome: results from a national survey. Am. J. Intellect. Dev. Disabil. 116, 16–35. 10.1352/1944-7558-116.1.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hashem V., Galloway J. N., Mori M., Willemsen R., Oostra B. A., Paylor R., et al. (2009). Ectopic expression of CGG containing mRNA is neurotoxic in mammals. Hum. Mol. Genet. 18, 2443–2451. 10.1093/hmg/ddp182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi M. L., Rao B. S., Seo J. S., Choi H. S., Dolan B. M., Choi S. Y., et al. (2007). Inhibition of p21-activated kinase rescues symptoms of fragile X syndrome in mice. Proc. Natl. Acad. Sci. U S A 104, 11489–11494. 10.1073/pnas.0705003104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hébert B., Pietropaolo S., Même S., Laudier B., Laugeray A., Doisne N., et al. (2014). Rescue of fragile X syndrome phenotypes in Fmr1 KO mice by a BKCa channel opener molecule. Orphanet J. Rare Dis. 9:124. 10.1186/s13023-014-0124-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heitz D., Devys D., Imbert G., Kretz C., Mandel J. L. (1992). Inheritance of the fragile X syndrome: size of the fragile X premutation is a major determinant of the transition to full mutation. J. Med. Genet. 29, 794–801. 10.1136/jmg.29.11.794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson G. I., Chen J. J., Schenker S. (1999). Ethanol, oxidative stress, reactive aldehydes, and the fetus. Front. Biosci. 15, D541–D550. 10.2741/henderson [DOI] [PubMed] [Google Scholar]
- Henderson C., Wijetunge L., Kinoshita M. N., Shumway M., Hammond R. S., Postma F. R., et al. (2012). Reversal of disease-related pathologies in the fragile X mouse model by selective activation of GABAB receptors with arbaclofen. Sci. Transl. Med. 4:152ra128. 10.1126/scitranslmed.3004218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herculano-Houzel S. (2009). The human brain in numbers: a linearly scaled-up primate brain. Front. Hum. Neurosci. 3:31. 10.3389/neuro.09.031.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernández J. A., López-Sánchez R. C., Rendón-Ramírez A. (2016). Lipids and oxidative stress associated with ethanol-induced neurological damage. Oxid. Med. Cell. Longev. 2016:1543809. 10.1155/2016/1543809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernando-Herraez I., Heyn H., Fernandez-Callejo M., Vidal E., Fernandez-Bellon H., Prado-Martinez J., et al. (2015). The interplay between DNA methylation and sequence divergence in recent human evolution. Nucleic Acids Res. 43, 8204–8214. 10.1093/nar/gkv693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernando-Herraez I., Prado-Martinez J., Garg P., Fernandez-Callejo M., Heyn H., Hvilsom C., et al. (2013). Dynamics of DNA methylation in recent human and great ape evolution. PLoS Genet. 9:e1003763. 10.1371/journal.pgen.1003763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herzog H. (2002). Ethical aspects of relationships between humans and research animals. ILAR J. 43, 27–32. 10.1093/ilar.43.1.27 [DOI] [PubMed] [Google Scholar]
- Heulens I., D’Hulst C., Van Dam D., De Deyn P. P., Kooy R. F. (2012). Pharmacological treatment of fragile X syndrome with GABAergic drugs in a knockout mouse model. Behav. Brain Res. 229, 244–249. 10.1016/j.bbr.2012.01.031 [DOI] [PubMed] [Google Scholar]
- Heyer D. B., Meredith R. M. (2017). Environmental toxicology: sensitive periods of development and neurodevelopmental disorders. Neurotoxicology 58, 23–41. 10.1016/j.neuro.2016.10.017 [DOI] [PubMed] [Google Scholar]
- Higashimori H., Schin C. S., Chiang M. S., Morel L., Shoneye T. A., Nelson D. L., et al. (2016). Selective deletion of astroglial FMRP dysregulates glutamate transporter GLT1 and contributes to fragile X syndrome phenotypes in vivo. J. Neurosci. 36, 7079–7094. 10.1523/JNEUROSCI.1069-16.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill J., Inder T., Neil J., Dierker D., Harwell J., Van Essen D. (2010). Similar patterns of cortical expansion during human development and evolution. Proc. Natl. Acad. Sci. U S A 107, 13135–13140. 10.1073/pnas.1001229107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinds H. L., Ashley C. T., Sutcliffe J. S., Nelson D. L., Warren S. T., Housman D. E., et al. (1993). Tissue specific expression of FMR-1 provides evidence for a functional role in fragile X syndrome. Nat. Genet. 3, 36–43. 10.1038/ng0193-36 [DOI] [PubMed] [Google Scholar]
- Hinton V. J., Brown W. T., Wisniewski K., Rudelli R. D. (1991). Analysis of neocortex in three males with the fragile X syndrome. Am. J. Med. Genet. 41, 289–294. 10.1002/ajmg.1320410306 [DOI] [PubMed] [Google Scholar]
- Hirst M. C., White P. J. (1998). Cloned human FMR1 trinucleotide repeats exhibit a length- and orientation-dependent instability suggestive of in vivo lagging strand secondary structure. Nucleic Acids Res. 26, 2353–2358. 10.1093/nar/26.10.2353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoeffer C. A., Sanchez E., Hagerman R. J., Mu Y., Nguyen D. V., Wong H., et al. (2012). Altered mTOR signaling and enhanced CYFIP2 expression levels in subjects with fragile X syndrome. Genes Brain Behav. 11, 332–341. 10.1111/j.1601-183x.2012.00768.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoehndorf R., Hiebert T., Hardy N. W., Schofield P. N., Gkoutos G. V., Dumontier M. (2014). Mouse model phenotypes provide information about human drug targets. Bioinformatics 30, 719–725. 10.1093/bioinformatics/btt613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holsen L. M., Dalton K. M., Johnstone T., Davidson R. J. (2008). Prefrontal social cognition network dysfunction underlying face encoding and social anxiety in fragile X syndrome. Neuroimage 43, 592–604. 10.1016/j.neuroimage.2008.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopkins W. D. (2013). Neuroanatomical asymmetries and handedness in chimpanzees (Pan troglodytes): a case for continuity in the evolution of hemispheric specialization. Ann. N Y Acad. Sci. 1288, 17–35. 10.1111/nyas.12109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horner A. E., Heath C. J., Hvoslef-Eide M., Kent B. A., Kim C. H., Nilsson S. R., et al. (2013). The touchscreen operant platform for testing learning and memory in rats and mice. Nat. Protoc. 8, 1961–1984. 10.1038/nprot.2013.122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornstra I. K., Nelson D. L., Warren S. T., Yang T. P. (1993). High resolution methylation analysis of the FMR1 gene trinucleotide repeat region in fragile X syndrome. Hum. Mol. Genet. 2, 1659–1665. 10.1093/hmg/2.10.1659 [DOI] [PubMed] [Google Scholar]
- Hou L., Antion M. D., Hu D., Spencer C. M., Paylor R., Klann E. (2006). Dynamic translational and proteasomal regulation of fragile X mental retardation protein controls mGluR-dependent long-term depression. Neuron 51, 441–454. 10.1016/j.neuron.2006.07.005 [DOI] [PubMed] [Google Scholar]
- Hu H., Qin Y., Bochorishvili G., Zhu Y., van Aelst L., Zhu J. J. (2008). Ras signaling mechanisms underlying impaired GluR1-dependent plasticity associated with fragile X syndrome. J. Neurosci. 28, 7847–7862. 10.1523/JNEUROSCI.1496-08.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang J., Wang Y., Zhao J. (2017). CRISPR editing in biological and biomedical investigation. J. Cell. Physiol. [Epub ahead of print]. 10.1002/jcp.26141 [DOI] [PubMed] [Google Scholar]
- Huber K. M., Gallagher S. M., Warren S. T., Bear M. F. (2002). Altered synaptic plasticity in a mouse model of fragile X mental retardation. Proc. Natl. Acad. Sci. U S A 99, 7746–7750. 10.1073/pnas.122205699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huddleston L. B., Visootsak J., Sherman S. L. (2014). Cognitive aspects of fragile X syndrome. Wiley Interdiscip. Rev. Cogn. Sci. 5, 501–508. 10.1002/wcs.1296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hukema R. K., Buijsen R. A., Raske C., Severijnen L. A., Nieuwenhuizen-Bakker I., Minneboo M., et al. (2014). Induced expression of expanded CGG RNA causes mitochondrial dysfunction in vivo. Cell Cycle 13, 2600–2608. 10.4161/15384101.2014.943112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulbert A. J. (2005). On the importance of fatty acid composition of membranes for aging. J. Theor. Biol. 234, 277–288. 10.1016/j.jtbi.2004.11.024 [DOI] [PubMed] [Google Scholar]
- Hunsaker M. R., Goodrich-Hunsaker N. J., Willemsen R., Berman R. F. (2010). Temporal ordering deficits in female CGG KI mice heterozygous for the fragile X premutation. Behav. Brain Res. 213, 263–268. 10.1016/j.bbr.2010.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunsaker M. R., von Leden R. E., Ta B. T., Goodrich-Hunsaker N. J., Arque G., Kim K., et al. (2011). Motor deficits on a ladder rung task in male and female adolescent and adult CGG knock-in mice. Behav. Brain Res. 222, 117–121. 10.1016/j.bbr.2011.03.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter J., Rivero-Arias O., Angelov A., Kim E., Fotheringham I., Leal J. (2014). Epidemiology of fragile X syndrome: a systematic review and meta-analysis. Am. J. Med. Genet. A 164A, 1648–1658. 10.1002/ajmg.a.36511 [DOI] [PubMed] [Google Scholar]
- Hvoslef-Eide M., Nilsson S. R., Saksida L. M., Bussey T. J. (2016). Cognitive translation using the rodent touchscreen testing approach. Curr. Top. Behav. Neurosci. 28, 423–447. 10.1007/7854_2015_5007 [DOI] [PubMed] [Google Scholar]
- Iida T., Nakahori Y., Tsutsumi O., Taketani Y., Nakagome Y. (1994). The CpG island of the FMR-1 gene is methylated differently among embryonic tissues: implication for prenatal diagnosis. Hum. Reprod. 9, 1471–1473. 10.1093/oxfordjournals.humrep.a138732 [DOI] [PubMed] [Google Scholar]
- Illingworth R. S., Gruenewald-Schneider U., Webb S., Kerr A. R., James K. D., Turner D. J., et al. (2010). Orphan CpG islands identify numerous conserved promoters in the mammalian genome. PLoS Genet. 6:1001134. 10.1371/journal.pgen.1001134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin S. A., Patel B., Idupulapati M., Harris J. B., Crisostomo R. A., Larsen B. P., et al. (2001). Abnormal dendritic spine characteristics in the temporal and visual cortices of patients with fragile-X syndrome: a quantitative examination. Am. J. Med. Genet. 98, 161–167. [DOI] [PubMed] [Google Scholar]
- Jacobs J. (2013). Hippocampal theta oscillations are slower in humans than in rodents: implications for models of spatial navigation and memory. Philos. Trans. R. Soc. Lond. B Biol. Sci. 369:20130304. 10.1098/rstb.2013.0304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs S., Cheng C., Doering L. C. (2016). Hippocampal neuronal subtypes develop abnormal dendritic arbors in the presence of Fragile X astrocytes. Neuroscience 324, 202–217. 10.1016/j.neuroscience.2016.03.011 [DOI] [PubMed] [Google Scholar]
- Jacobs R. A., Díaz V., Meinild A.-K., Gassmann M., Lundby C. (2013). The C57Bl/6 mouse serves as a suitable model of human skeletal muscle mitochondrial function. Exp. Physiol. 98, 908–921. 10.1113/expphysiol.2012.070037 [DOI] [PubMed] [Google Scholar]
- Jacobs S., Doering L. C. (2010). Astrocytes prevent abnormal neuronal development in the fragile x mouse. J. Neurosci. 30, 4508–4514. 10.1523/JNEUROSCI.5027-09.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs S., Nathwani M., Doering L. C. (2010). Fragile X astrocytes induce developmental delays in dendrite maturation and synaptic protein expression. BMC Neurosci. 11:132. 10.1186/1471-2202-11-132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacquemont S., Curie A., Des Portes V., Torrioli M. G., Berry-Kravis E., Hagerman R. J., et al. (2011). Epigenetic modification of the FMR1 gene in fragile X syndrome is associated with differential response to the mGluR5 antagonist AFQ056. Sci. Transl. Med. 3:64ra1. 10.1126/scitranslmed.3001708 [DOI] [PubMed] [Google Scholar]
- Jarem D. A., Huckaby L. V., Delaney S. (2010). AGG interruptions in (CGG)n DNA repeat tracts modulate the structure and thermodynamics of non-B conformations in vitro. Biochemistry 49, 6826–6837. 10.1021/bi1007782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joly O., Pallier C., Ramus F., Pressnitzer D., Vanduffel W., Orban G. A. (2012). Processing of vocalizations in humans and monkeys: a comparative fMRI study. Neuroimage 62, 1376–1389. 10.1016/j.neuroimage.2012.05.070 [DOI] [PubMed] [Google Scholar]
- Jones O. D. (2017). Do group I metabotropic glutamate receptors mediate LTD? Neurobiol. Learn. Mem. 138, 85–97. 10.1016/j.nlm.2016.08.010 [DOI] [PubMed] [Google Scholar]
- Jones S. M., Cantlon J. F., Merritt D. J., Brannon E. M. (2010). Context affects the numerical semantic congruity effect in rhesus monkeys (Macaca mulatta). Behav. Processes 83, 191–196. 10.1016/j.beproc.2009.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaas J. H. (1989). Why does the brain have so many visual areas? J. Cogn. Neurosci. 1, 121–135. 10.1162/jocn.1989.1.2.121 [DOI] [PubMed] [Google Scholar]
- Kaas J. H. (2011). Reconstructing the areal organization of the neocortex of the first mammals. Brain Behav. Evol. 78, 7–21. 10.1159/000327316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalinowska M., Castillo C., Francesconi A. (2015). Quantitative profiling of brain lipid raft proteome in a mouse model of fragile X syndrome. PLoS One 10:e0121464. 10.1371/journal.pone.0121464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandel E. R. (2001). The molecular biology of memory storage: a dialogue between genes and synapses. Science 294, 1030–1038. 10.1126/science.1067020 [DOI] [PubMed] [Google Scholar]
- Kandel E. R. (2009). The biology of memory: a forty-year perspective. J. Neurosci. 29, 12748–12756. 10.1523/JNEUROSCI.3958-09.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang J. Y., Chadchankar J., Vien T. N., Mighdoll M. I., Hyde T. M., Mather R. J., et al. (2017). Deficits in the activity of presynaptic γ-aminobutyric acid type B receptors contribute to altered neuronal excitability in fragile X syndrome. J. Biol. Chem. 292, 6621–6632. 10.1074/jbc.M116.772541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang S. J., Kaang B. K. (2016). Metabotropic glutamate receptor dependent long-term depression in the cortex. Korean J. Physiol. Pharmacol. 20, 557–564. 10.4196/kjpp.2016.20.6.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kangas B. D., Bergman J. (2017). Touchscreen technology in the study of cognition-related behavior. Behav. Pharmacol. 28, 623–629. 10.1097/FBP.0000000000000356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashi Y., King D. G. (2006). Simple sequence repeats as advantageous mutators in evolution. Trends Genet. 22, 253–259. 10.1016/j.tig.2006.03.005 [DOI] [PubMed] [Google Scholar]
- Kato Y., Gokan H., Oh-Nishi A., Suhara T., Watanabe S., Minamimoto T. (2014). Vocalizations associated with anxiety and fear in the common marmoset (Callithrix jacchus). Behav. Brain Res. 275, 43–52. 10.1016/j.bbr.2014.08.047 [DOI] [PubMed] [Google Scholar]
- Kaufmann W. E., Abrams M. T., Chen W., Reiss A. L. (1999). Genotype, molecular phenotype and cognitive phenotype: correlations in fragile X syndrome. Am. J. Med. Genet. 83, 286–295. [DOI] [PubMed] [Google Scholar]
- Kazdoba T. M., Leach P. T., Silverman J. L., Crawley J. N. (2014). Modeling fragile X syndrome in the Fmr1 knockout mouse. Intractable Rare Dis. Res. 3, 118–133. 10.5582/irdr.2014.01024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp C., Kaplan G. (2013). Facial expressions in common marmosets (Callithrix jacchus) and their use by conspecifics. Anim. Cogn. 16, 773–788. 10.1007/s10071-013-0611-5 [DOI] [PubMed] [Google Scholar]
- Kenkel W. M., Yee J. R., Moore K., Madularu D., Kulkarni P., Gamber K., et al. (2016). Functional magnetic resonance imaging in awake transgenic fragile X rats: evidence of dysregulation in reward processing in the mesolimbic/habenular neural circuit. Transl. Psychiatry 22:e763. 10.1038/tp.2016.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenneson A., Zhang F., Hagedorn C. H., Warren S. T. (2001). Reduced FMRP and increased FMR1 transcription is proportionally associated with CGG repeat number in intermediate-length and premutation carriers. Hum. Mol. Genet. 10, 1449–1454. 10.1093/hmg/10.14.1449 [DOI] [PubMed] [Google Scholar]
- Kenny P., Ceman S. (2016). RNA secondary structure modulates FMRP’s bi-functional role in the MicroRNA pathway. Int. J. Mol. Sci. 17:E985. 10.3390/ijms17060985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kettani A., Kumara R. A., Patel J. D. (1995). Solution structure of a DNA quadruplex containing the fragile X syndrome triplet repeat. J. Mol. Biol. 254, 638–656. 10.1006/jmbi.1995.0644 [DOI] [PubMed] [Google Scholar]
- Keysers C., Kaas J. H., Gazzola V. (2010). Somatosensation in social perception. Nat. Rev. Neurosci. 11, 417–428. 10.1038/nrn2833 [DOI] [PubMed] [Google Scholar]
- Khalfallah O., Jarjat M., Davidovic L., Nottet N., Cestele S., Mantegazza M., et al. (2017). Depletion of the fragile X mental retardation protein in embryonic stem cells alters the kinetics of neurogenesis. Stem Cells 35, 374–385. 10.1002/stem.2505 [DOI] [PubMed] [Google Scholar]
- Khateb S., Weisman-Shomer P., Hershco-Shani I., Ludwig A. L., Fry M. (2007). The tetraplex (CGG)n destabilizing proteins hnRNP A2 and CBF-A enhance the in vivo translation of fragile X premutation mRNA. Nucleic Acids Res. 35, 5775–5788. 10.1093/nar/gkm636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim M., Bellini M., Ceman S. (2009). Fragile X mental retardation protein FMRP binds mRNAs in the nucleus. Mol. Cell. Biol. 29, 214–228. 10.1128/MCB.01377-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S. Y., Burris J., Bassal F., Koldewyn K., Chattarji S., Tassone F., et al. (2014). Fear-specific amygdala function in children and adolescents on the fragile X spectrum: a dosage response of the FMR1 gene. Cereb. Cortex 24, 600–613. 10.1093/cercor/bhs341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H., Gibboni R., Kirkhart C., Bao S. (2013). Impaired critical period plasticity in primary auditory cortex of fragile X model mice. J. Neurosci. 33, 15686–15692. 10.1523/JNEUROSCI.3246-12.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S. H., Markham J. A., Weiler I. J., Greenough W. T. (2008). Aberrant early-phase ERK inactivation impedes neuronal function in fragile X syndrome. Proc. Natl. Acad. Sci. U S A 105, 4429–4434. 10.1073/pnas.0800257105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein E. D., Evans T. A., Schultz N. B., Beran M. J. (2013). Learning how to “make a deal”: human (Homo sapiens) and monkey (Macaca mulatta) performance when repeatedly faced with the Monty Hall Dilemma. J. Comp. Psychol. 127, 103–108. 10.1037/a0029057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klusek J., Martin G. E., Losh M. (2014). A comparison of pragmatic language in boys with autism and fragile X syndrome. J. Speech Lang. Hear. Res. 57, 1692–1707. 10.1044/2014_JSLHR-L-13-0064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koekkoek S. K., Yamaguchi K., Milojkovic B. A., Dortland B. R., Ruigrok T. J., Maex R., et al. (2005). Deletion of FMR1 in Purkinje cells enhances parallel fiber LTD, enlarges spines and attenuates cerebellar eyelid conditioning in Fragile X syndrome. Neuron 47, 339–352. 10.1016/j.neuron.2005.07.005 [DOI] [PubMed] [Google Scholar]
- Koga K., Liu M. G., Qiu S., Song Q., O’Den G., Chen T., et al. (2015). Impaired presynaptic long-term potentiation in the anterior cingulate cortex of Fmr1 knock-out mice. J. Neurosci. 35, 2033–2043. 10.1523/JNEUROSCI.2644-14.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kogan C. S., Turk J., Hagerman R. J., Cornish K. M. (2008). Impact of the Fragile X mental retardation 1 (FMR1) gene premutation on neuropsychiatric functioning in adult males without fragile X-associated Tremor/Ataxia syndrome: a controlled study. Am. J. Med. Genet. B Neuropsychiatr. Genet. 5, 859–872. 10.1002/ajmg.b.30685 [DOI] [PubMed] [Google Scholar]
- Korb E., Herre M., Zucker-Scharff I., Gresack J., Allis C. D., Darnell R. B. (2017). Excess translation of epigenetic regulators contributes to fragile X syndrome and is alleviated by Brd4 inhibition. Cell 170, 1209.e20–1223.e20. 10.1016/j.cell.2017.07.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korzhevskii D. E., Otellin V. A., Grigor’ev I. P. (2005). Glial fibrillary acidic protein in astrocytes in the human neocortex. Neurosci. Behav. Physiol. 35, 789–792. 10.1007/s11055-005-0125-y [DOI] [PubMed] [Google Scholar]
- Koski S. E., Burkart J. M. (2015). Common marmosets show social plasticity and group-level similarity in personality. Sci. Rep. 5:8878. 10.1038/srep08878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotani M., Shimono K., Yoneyama T., Nakako T., Matsumoto K., Ogi Y., et al. (2017). An eye tracking system for monitoring face scanning patterns reveals the enhancing effect of oxytocin on eye contact in common marmosets. Psychoneuroendocrinology 83, 42–48. 10.1016/j.psyneuen.2017.05.009 [DOI] [PubMed] [Google Scholar]
- Ku H.-H., Brunk U. T., Sohal R. S. (1993). Relationship between mitochondrial superoxide and hydrogen peroxide production and longevity of mammalian species. Free Radic. Biol. Med. 15, 621–627. 10.1016/0891-5849(93)90165-q [DOI] [PubMed] [Google Scholar]
- Kumari D., Bhattacharya A., Nadel J., Moulton K., Zeak N. M., Glicksman A., et al. (2014). Identification of fragile X syndrome specific molecular markers in human fibroblasts: a useful model to test the efficacy of therapeutic drugs. Hum. Mutat. 35, 1485–1494. 10.1002/humu.22699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumari D., Usdin K. (2010). The distribution of repressive histone modifications on silenced FMR1 alleles provides clues to the mechanism of gene silencing in fragile X syndrome. Hum. Mol. Genet. 19, 4634–4642. 10.1093/hmg/ddq394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumari D., Usdin K. (2016). Sustained expression of FMR1 mRNA from reactivated fragile X syndrome alleles after treatment with small molecules that prevent trimethylation of H3K27. Hum. Mol. Genet. 25, 3689–3698. 10.1093/hmg/ddw215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo A. Y., Reiss A. L., Freund L. S., Huffman L. C. (2002). Family environment and cognitive abilities in girls with fragile-X syndrome. J. Intellect. Disabil. Res. 46, 328–339. 10.1046/j.1365-2788.2002.00396.x [DOI] [PubMed] [Google Scholar]
- Kwon H., Menon V., Eliez S., Warsofsky I. S., White C. D., Dyer-Friedman J., et al. (2001). Functional neuroanatomy of visuospatial working memory in fragile X syndrome: relation to behavioral and molecular measures. Am. J. Psychiatry 158, 1040–1051. 10.1176/appi.ajp.158.7.1040 [DOI] [PubMed] [Google Scholar]
- La Fata G., Gärtner A., Domínguez-Iturza N., Dresselaers T., Dawitz J., Poorthuis R. B., et al. (2014). FMRP regulates multipolar to bipolar transition affecting neuronal migration and cortical circuitry. Nat. Neurosci. 17, 1693–1700. 10.1038/nn.3870 [DOI] [PubMed] [Google Scholar]
- Lai Y., Xu M., Zhang Z., Liu Y. (2013). Instability of CTG repeats is governed by the position of a DNA base lesion through base excision repair. PLoS One 8:e56960. 10.1371/journal.pone.0056960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lalanne L., Weiner L., Trojak B., Berna F., Bertschy G. (2015). Substance-use disorder in high-functioning autism: clinical and neurocognitive insights from two case reports. BMC Psychiatry 15:149. 10.1186/s12888-015-0541-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landrigan P. J. (2010). What causes autism? Exploring the environmental contribution. Curr. Opin. Pediatr. 22, 219–225. 10.1097/mop.0b013e328336eb9a [DOI] [PubMed] [Google Scholar]
- Larsen L. A., Armstrong J. S., Grønskov K., Hjalgrim H., Macpherson J. N., Brøndum-Nielsen K., et al. (2000). Haplotype and AGG-interspersion analysis of FMR1 (CGG)n alleles in the Danish population: implications for multiple mutational pathways towards fragile X alleles. Am. J. Med. Genet. 93, 99–106. [DOI] [PubMed] [Google Scholar]
- Larsen H., van der Zwaluw C. S., Overbeek G., Granic I., Franke B., Engels R. C. (2010). A variable-number-of-tandem-repeats polymorphism in the dopamine D4 receptor gene affects social adaptation of alcohol use: investigation of a gene-environment interaction. Psychol. Sci. 21, 1064–1068. 10.1177/0956797610376654 [DOI] [PubMed] [Google Scholar]
- Larson J., Jessen R. E., Kim D., Fine A. K., Du Hoffmann J. (2005). Age-dependent and selective impairment of long-term potentiation in the anterior piriform cortex of mice lacking the fragile X mental retardation protein. J. Neurosci. 25, 9460–9469. 10.1523/JNEUROSCI.2638-05.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauterborn J. C., Rex C. S., Kramár E., Chen L. Y., Pandyarajan V., Lynch G., et al. (2007). Brain-derived neurotrophic factor rescues synaptic plasticity in a mouse model of fragile X syndrome. J. Neurosci. 27, 10685–10694. 10.1523/JNEUROSCI.2624-07.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavedan C. N., Garrett L., Nussbaum R. L. (1997). Trinucleotide repeats (CGG)22TGG(CGG)43TGG(CGG)21 from the fragile X gene remain stable in transgenic mice. Hum. Genet. 100, 407–414. 10.1007/s004390050525 [DOI] [PubMed] [Google Scholar]
- Lavedan C., Grabczyk E., Usdin K., Nussbaum R. L. (1998). Long uninterrupted CGG repeats within the first exon of the human FMR1 gene are not intrinsically unstable in transgenic mice. Genomics 50, 229–240. 10.1006/geno.1998.5299 [DOI] [PubMed] [Google Scholar]
- Lazaro-Perea C., de Fátima Arruda M., Snowdon C. T. (2004). Grooming as a reward? Social function of grooming between females in cooperatively breeding marmosets. Anim. Behav. 67, 627–636. 10.1016/j.anbehav.2003.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leach P. T., Hayes J., Pride M., Silverman J. L., Crawley J. N. (2016). Normal performance of Fmr1 mice on a touchscreen delayed nonmatching to position working memory task. eNeuro 3:ENEURO.0143-15.2016. 10.1523/ENEURO.0143-15.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H. Y., Ge W. P., Huang W., He Y., Wang G. X., Rowson-Baldwin A., et al. (2011). Bidirectional regulation of dendritic voltage-gated potassium channels by the fragile X mental retardation protein. Neuron 72, 630–642. 10.1016/j.neuron.2011.09.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee E., Lee J., Kim E. (2017). Excitation/inhibition imbalance in animal models of autism spectrum disorders. Biol. Psychiatry 81, 838–847. 10.1016/j.biopsych.2016.05.011 [DOI] [PubMed] [Google Scholar]
- Levenga J., Hayashi S., de Vrij F. M., Koekkoek S. K., van der Linde H. C., Nieuwenhuizen I., et al. (2011). AFQ056, a new mGluR5 antagonist for treatment of fragile X syndrome. Neurobiol. Dis. 42, 311–317. 10.1016/j.nbd.2011.01.022 [DOI] [PubMed] [Google Scholar]
- Lewis P., Abbeduto L., Murphy M., Richmond E., Giles N., Bruno L., et al. (2006). Cognitive, language and social-cognitive skills of individuals with fragile X syndrome with and without autism. J. Intellect. Disabil. Res. 50, 532–545. 10.1111/j.1365-2788.2006.00803.x [DOI] [PubMed] [Google Scholar]
- Li J., Pelletier M. R., Perez Velazquez J.-L., Carlen P. L. (2002). Reduced cortical synaptic plasticity and GluR1 expression associated with fragile X mental retardation protein deficiency. Mol. Cell. Neurosci. 19, 138–151. 10.1006/mcne.2001.1085 [DOI] [PubMed] [Google Scholar]
- Li Y., Stockton M. E., Bhuiyan I., Eisinger B. E., Gao Y., Miller J. L., et al. (2016). MDM2 inhibition rescues neurogenic and cognitive deficits in a mouse model of fragile X syndrome. Sci. Transl. Med. 8:336ra61. 10.1126/scitranslmed.aad9370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang K. C., Tseng J. T., Tsai S. J., Sun H. S. (2015). Characterization and distribution of repetitive elements in association with genes in the human genome. Comput. Biol. Chem. 57, 29–38. 10.1016/j.compbiolchem.2015.02.007 [DOI] [PubMed] [Google Scholar]
- Liang P., Xu Y., Zhang X., Ding C., Huang R., Zhang Z., et al. (2015). CRISPR/Cas9-mediated gene editing in human tripronuclear zygotes. Protein Cell 6, 363–372. 10.1007/s13238-015-0153-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao L. J., Park S. K., Xu T., Vanderklish P., Yates J. R. (2008). Quantitative proteomic analysis of primary neurons reveals diverse changes in synaptic protein content in fmr1 knockout mice. Proc. Natl. Acad. Sci. U S A 105, 15281–15286. 10.1073/pnas.0804678105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ligsay A., Hagerman R. J. (2016). Review of targeted treatments in fragile X syndrome. Intractable Rare Dis. Res. 5, 158–167. 10.5582/irdr.2016.01045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim C. S., Hoang E. T., Viar K. E., Stornetta R. L., Scott M. M., Zhu J. J. (2014). Pharmacological rescue of Ras signaling, GluA1-dependent synaptic plasticity and learning deficits in a fragile X model. Genes Dev. 28, 273–289. 10.1101/gad.232470.113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y., Tang C., He H., Duan R. (2013). Activation of mTOR ameliorates fragile X premutation rCGG repeat-mediated neurodegeneration. PLoS One 8:e62572. 10.1371/journal.pone.0062572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindburg D. G. (1991). Ecological requirements of macaques. Lab Anim. Sci. 41, 315–322. [PubMed] [Google Scholar]
- Linderkamp O., Janus L., Linder R., Skoruppa D. B. (2009). Time table of normal foetal brain development. Int. J. Prenat. Perinat. Psychol. Med. 21, 4–16. [Google Scholar]
- Liu Z. H., Chuang D. M., Smith C. B. (2011). Lithium ameliorates phenotypic deficits in a mouse model of fragile X syndrome. Int. J. Neuropsychopharmacol. 14, 618–630. 10.1017/s1461145710000520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z. H., Huang T., Smith C. B. (2012). Lithium reverses increased rates of cerebral protein synthesis in a mouse model of fragile X syndrome. Neurobiol. Dis. 45, 1145–1152. 10.1016/j.nbd.2011.12.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z., Li X., Zhang J. T., Cai Y. J., Cheng T. L., Cheng C., et al. (2016). Autism-like behaviours and germline transmission in transgenic monkeys overexpressing MeCP2. Nature 530, 98–102. 10.1038/nature16533 [DOI] [PubMed] [Google Scholar]
- Liu H., Yin J., Xiao M., Gao C., Mason A. S., Zhao Z., et al. (2012). Characterization and evolution of 5’ and 3’ untranslated regions in eukaryotes. Gene 507, 106–111. 10.1016/j.gene.2012.07.034 [DOI] [PubMed] [Google Scholar]
- Lloyd B. A., Hake H. S., Ishiwata T., Farmer C. E., Loetz E. C., Fleshner M., et al. (2017). Exercise increases mTOR signaling in brain regions involved in cognition and emotional behavior. Behav. Brain Res. 323, 56–67. 10.1016/j.bbr.2017.01.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loesch D. Z., Huggins R. M., Bui Q. M., Taylor A. K., Pratt C., Epstein J., et al. (2003). Effect of fragile X status categories and FMRP deficits on cognitive profiles estimated by robust pedigree analysis. Am. J. Med. Genet. A 15, 13–23. 10.1002/ajmg.a.20214 [DOI] [PubMed] [Google Scholar]
- Loesch D. Z., Huggins R. M., Hagerman R. J. (2004). Phenotypic variation and FMRP levels in fragile X. Ment. Retard. Dev. Disabil. Res. Rev. 10, 31–41. 10.1002/mrdd.20006 [DOI] [PubMed] [Google Scholar]
- Loesch D. Z., Sherwell S., Kinsella G., Tassone F., Taylor A., Amor D., et al. (2012). Fragile X-associated tremor/ataxia phenotype in a male carrier of unmethylated full mutation in the FMR1 gene. Clin. Genet. 82, 88–92. 10.1111/j.1399-0004.2011.01675.x [DOI] [PubMed] [Google Scholar]
- Long H. K., Sims D., Heger A., Blackledge N. P., Kutter C., Wright M. L., et al. (2013). Epigenetic conservation at gene regulatory elements revealed by non-methylated DNA profiling in seven vertebrates. Elife 26:e00348. 10.7554/eLife.00348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loomis E. W., Sanz L. A., Chedin F., Hagerman P. J. (2014). Transcription-associated R-loop formation across the human FMR1 CGG-repeat region. PLoS Genet. 10:e1004294. 10.1371/journal.pgen.1004294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovelace J. W., Wen T. H., Reinhard S., Hsu M. S., Sidhu H., Ethell I. M., et al. (2016). Matrix metalloproteinase-9 deletion rescues auditory evoked potential habituation deficit in a mouse model of Fragile X Syndrome. Neurobiol. Dis. 89, 126–135. 10.1016/j.nbd.2016.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowenstine L. J., McManamon R., Terio K. A. (2016). Comparative pathology of aging great apes: bonobos, chimpanzees, gorillas and orangutans. Vet. Pathol. 53, 250–276. 10.1177/0300985815612154 [DOI] [PubMed] [Google Scholar]
- Lubojemska A., Borejko M., Czapiewski P., Dziadziuszko R., Biernat W. (2016). Of mice and men: olfactory neuroblastoma among animals and humans. Vet. Comp. Oncol. 14, e70–e82. 10.1111/vco.12102 [DOI] [PubMed] [Google Scholar]
- Lucarelli M., Visalberghi E., Adriani W., Addessi E., Pierandrei S., Manciocco A., et al. (2017). Polymorphism of the 3’-UTR of the dopamine transporter gene (DAT) in New World monkeys. Primates 58, 169–178. 10.1007/s10329-016-0560-0 [DOI] [PubMed] [Google Scholar]
- Ludwig A. L., Espinal G. M., Pretto D. I., Jamal A. L., Arque G., Tassone F., et al. (2014). CNS expression of murine fragile X protein (FMRP) as a function of CGG-repeat size. Hum. Mol. Genet. 23, 3228–3238. 10.1093/hmg/ddu032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luecke R. H., Wosilait W. D., Young J. F. (1999). Mathematical modeling of human embryonic and fetal growth rates. Growth Dev. Aging 63, 49–59. [PubMed] [Google Scholar]
- Luque M. A., Beltran-Matas P., Marin M. C., Torres B., Herrero L. (2017). Excitability is increased in hippocampal CA1 pyramidal cells of Fmr1 knockout mice. PLoS One 12:e0185067. 10.1371/journal.pone.0185067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luy J. (2007). Ethical and legal aspects of animal experiments on non-human primates. Dtsch. Tierarztl. Wochenschr. 114, 81–85. [PubMed] [Google Scholar]
- Macdonald D. W. (1981). Dwindling resources and the social behaviour of Capybaras, (Hydrochoerus hydrochaeris) (Mammalia). J. Zool. 194, 371–391. 10.1111/j.1469-7998.1981.tb04588.x [DOI] [Google Scholar]
- Machado C. J., Nelson E. E. (2011). Eye-tracking with nonhuman primates is now more accessible than ever before. Am. J. Primatol. 73, 562–569. 10.1002/ajp.20928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLeod L. S., Kogan C. S., Collin C. A., Berry-Kravis E., Messier C., Gandhi R. (2010). A comparative study of the performance of individuals with fragile X syndrome and Fmr1 knockout mice on Hebb-Williams mazes. Genes Brain Behav. 9, 53–64. 10.1111/j.1601-183x.2009.00534.x [DOI] [PubMed] [Google Scholar]
- Maes B., Fryns J. P., Van Walleghem M., Van Den Berghe H. (1994). Cognitive functioning and information processing of adult mentally retarded men with fragile-X syndrome. Am. J. Med. Genet. 50, 190–200. 10.1002/ajmg.1320500211 [DOI] [PubMed] [Google Scholar]
- Malgowska M., Gudanis D., Kierzek R., Wyszko E., Gabelica V., Gdaniec Z. (2014). Distinctive structural motifs of RNA G-quadruplexes composed of AGG, CGG and UGG trinucleotide repeats. Nucleic Acids Res. 42, 10196–10207. 10.1093/nar/gku710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margaret Elowson A., Snowdon C. T., Lazaro-Perea C. (1998). ‘Babbling’ and social context in infant monkeys: parallels to human infants. Trends Cogn. Sci. 2, 31–37. 10.1016/s1364-6613(97)01115-7 [DOI] [PubMed] [Google Scholar]
- Margulies D. S. (2017). Unraveling the complex tapestry of association networks. Neuron 95, 239–241. 10.1016/j.neuron.2017.07.006 [DOI] [PubMed] [Google Scholar]
- Markram K., Markram H. (2010). The intense world theory–a unifying theory of the neurobiology of autism. Front. Hum. Neurosci. 4:224. 10.3389/fnhum.2010.00224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin B. S., Corbin J. G., Huntsman M. M. (2014). Deficient tonic GABAergic conductance and synaptic balance in the fragile X syndrome amygdala. J. Neurophysiol. 112, 890–902. 10.1152/jn.00597.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin H. G. S., Lassalle O., Brown J. T., Manzoni O. J. (2016). Age-dependent long-term potentiation deficits in the prefrontal cortex of the Fmr1 knockout mouse model of fragile X syndrome. Cereb. Cortex 26, 2084–2092. 10.1093/cercor/bhv031 [DOI] [PubMed] [Google Scholar]
- Martin B. S., Martinez-Botella G., Loya C. M., Salituro F. G., Robichaud A. J., Huntsman M. M., et al. (2016). Rescue of deficient amygdala tonic γ-aminobutyric acidergic currents in the Fmr-/y mouse model of fragile X syndrome by a novel γ-aminobutyric acid type A receptor-positive allosteric modulator. J. Neurosci. Res. 94, 568–578. 10.1002/jnr.23632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin D. I., Singer M., Dhahbi J., Mao G., Zhang L., Schroth G. P., et al. (2011). Phyloepigenomic comparison of great apes reveals a correlation between somatic and germline methylation states. Genome Res. 21, 2049–2057. 10.1101/gr.122721.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez L. A., Tejada-Simon M. V. (2017). Pharmacological rescue of hippocampal fear learning deficits in fragile X syndrome. Mol. Neurobiol. [Epub ahead of print]. 10.1007/s12035-017-0819-5 [DOI] [PubMed] [Google Scholar]
- Massen J. J., Šlipogor V., Gallup A. C. (2016). An observational investigation of behavioral contagion in common marmosets (Callithrix jacchus): indications for contagious scent-marking. Front. Psychol. 7:1190. 10.3389/fpsyg.2016.01190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matic K., Eninger T., Bardoni B., Davidovic L., Macek B. (2014). Quantitative phosphoproteomics of murine Fmr1-KO cell lines provides new insights into FMRP-dependent signal transduction mechanisms. J. Proteome Res. 13, 4388–4397. 10.1021/pr5006372 [DOI] [PubMed] [Google Scholar]
- Matsuo K., Clay O., Takahashi T., Silke J., Schaffner W. (1993). Evidence for erosion of mouse CpG islands during mammalian evolution. Somat. Cell Mol. Genet. 19, 543–555. 10.1007/bf01233381 [DOI] [PubMed] [Google Scholar]
- Mazzocco M. M., Pennington B. F., Hagerman R. J. (1994). Social cognition skills among females with fragile X. J. Autism Dev. Disord. 24, 473–485. 10.1007/bf02172129 [DOI] [PubMed] [Google Scholar]
- Meredith R. M., de Jong R., Mansvelder H. D. (2011). Functional rescue of excitatory synaptic transmission in the developing hippocampus in Fmr1-KO mouse. Neurobiol. Dis. 41, 104–110. 10.1016/j.nbd.2010.08.026 [DOI] [PubMed] [Google Scholar]
- Mestas J., Hughes C. C. (2004). Of mice and not men: differences between mouse and human immunology. J. Immunol. 172, 2731–2738. 10.4049/jimmunol.172.5.2731 [DOI] [PubMed] [Google Scholar]
- Michalon A., Sidorov M., Ballard T. M., Ozmen L., Spooren W., Wettstein J. G., et al. (2012). Chronic pharmacological mGlu5 inhibition corrects fragile X in adult mice. Neuron 74, 49–56. 10.1016/j.neuron.2012.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mientjes E. J., Nieuwenhuizen I., Kirkpatrick L., Zu T., Hoogeveen-Westerveld M., Severijnen L., et al. (2006). The generation of a conditional Fmr1 knock out mouse model to study Fmrp function in vivo. Neurobiol. Dis. 21, 549–555. 10.1016/j.nbd.2005.08.019 [DOI] [PubMed] [Google Scholar]
- Miller C. T., Mandel K., Wang X. (2010). The communicative content of the common marmoset phee call during antiphonal calling. Am. J. Primatol. 72, 974–980. 10.1002/ajp.20854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller C. T., Wang X. (2006). Sensory-motor interactions modulate a primate vocal behavior: antiphonal calling in common marmosets. J. Comp. Physiol. A Neuroethol. Sens. Neural Behav. Physiol. 192, 27–38. 10.1007/s00359-005-0043-z [DOI] [PubMed] [Google Scholar]
- Ming X., Johnson W. G., Stenroos E. S., Mars A., Lambert G. H., Buyske S. (2010). Genetic variant of glutathione peroxidase 1 in autism. Brain Dev. 32, 105–109. 10.1016/j.braindev.2008.12.017 [DOI] [PubMed] [Google Scholar]
- Mitas M., Yu A., Dill J., Haworth S. I. (1995). The trinucleotide repeat sequence d(CGG)15 forms a heat-stable hairpin containing Gsyn. Ganti base pairs. Biochemistry 34, 12803–12811. 10.1021/bi00039a041 [DOI] [PubMed] [Google Scholar]
- Miyashiro K. Y., Beckel-Mitchener A., Purk T. P., Becker K. G., Barret T., Liu L., et al. (2003). RNA cargoes associating with FMRP reveal deficits in cellular functioning in Fmr1 null mice. Neuron 37, 417–431. 10.1016/s0896-6273(03)00034-5 [DOI] [PubMed] [Google Scholar]
- Mohammadparast S., Bayat H., Biglarian A., Ohadi M. (2014). Exceptional expansion and conservation of a CT-repeat complex in the core promoter of PAXBP1 in primates. Am. J. Primatol. 76, 747–756. 10.1002/ajp.22266 [DOI] [PubMed] [Google Scholar]
- Molaro A., Hodges E., Fang F., Song Q., Mccombie W. R., Hannon G. J., et al. (2011). Sperm methylation profiles reveal features of epigenetic inheritance and evolution in primates. Cell 146, 1029–1041. 10.1016/j.cell.2011.08.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore T. L., Killiany R. J., Herndon J. G., Rosene D. L., Moss M. B. (2003). Impairment in abstraction and set shifting in aged rhesus monkeys. Neurobiol. Aging 24, 125–134. 10.1016/s0197-4580(02)00054-4 [DOI] [PubMed] [Google Scholar]
- Moore T. L., Killiany R. J., Herndon J. G., Rosene D. L., Moss M. B. (2005). A non-human primate test of abstraction and set shifting: an automated adaptation of the Wisconsin Card Sorting Test. J. Neurosci. Methods 146, 165–173. 10.1016/j.jneumeth.2005.02.005 [DOI] [PubMed] [Google Scholar]
- Moore T. L., Killiany R. J., Herndon J. G., Rosene D. L., Moss M. B. (2006). Executive system dysfunction occurs as early as middle-age in the rhesus monkey. Neurobiol. Aging 27, 1484–1493. 10.1016/j.neurobiolaging.2005.08.004 [DOI] [PubMed] [Google Scholar]
- Morecraft R. J., Stilwell-Morecraft K. S., Ge J., Cipolloni P. B., Pandya D. N. (2015). Cytoarchitecture and cortical connections of the anterior insula and adjacent frontal motor fields in the rhesus monkey. Brain Res. Bull. 119, 52–72. 10.1016/j.brainresbull.2015.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mornet E., Chateau C., Taillandier A., Simon-Bouy B., Serre J. L. (1996). Recurrent and unexpected segregation of the FMR1 CGG repeat in a family with fragile X syndrome. Hum. Genet. 97, 512–515. 10.1007/s004390050083 [DOI] [PubMed] [Google Scholar]
- Morrill R. J., Paukner A., Ferrari P. F., Ghazanfar A. A. (2012). Monkey lipsmacking develops like the human speech rhythm. Dev. Sci. 15, 557–568. 10.1111/j.1467-7687.2012.01149.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrill R. J., Thomas A. W., Schiel N., Souto A., Miller C. T. (2013). The effect of habitat acoustics on common marmoset vocal signal transmission. Am. J. Primatol. 75, 904–916. 10.1002/ajp.22152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor-Shaked H., Eiges R. (2016). Modeling fragile X syndrome using human pluripotent stem cells. Genes 7:E77. 10.3390/genes7100077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor-Shaked H., Eiges R. (2018). Reevaluation of FMR1 hypermethylation timing in fragile X syndrome. Front. Mol. Neurosci. 11:31 10.3389/fnmol.2018.00031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moser E. I., Kropff E., Moser M. B. (2008). Place cells, grid cells and the brain’s spatial representation system. Annu. Rev. Neurosci. 31, 69–89. 10.1146/annurev.neuro.31.061307.090723 [DOI] [PubMed] [Google Scholar]
- Mulvihill D. J., Nichol Edamura K., Hagerman K. A., Pearson C. E., Wang Y. H. (2005). Effect of CAT or AGG interruptions and CpG methylation on nucleosome assembly upon trinucleotide repeats on spinocerebellar ataxia, type 1 and fragile X syndrome. J. Biol. Chem. 280, 4498–4503. 10.1074/jbc.M413239200 [DOI] [PubMed] [Google Scholar]
- Munir F., Cornish K. M., Wilding J. (2000). A neuropsychological profile of attention deficits in young males with fragile X syndrome. Neuropsychologia 38, 1261–1270. 10.1016/s0028-3932(00)00036-1 [DOI] [PubMed] [Google Scholar]
- Murphy M. M., Abbeduto L. (2007). Gender differences in repetitive language in fragile X syndrome. J. Intellect. Disabil. Res. 51, 387–400. 10.1111/j.1365-2788.2006.00888.x [DOI] [PubMed] [Google Scholar]
- Muzar Z., Adams P. E., Schneider A., Hagerman R. J., Lozano R. (2014). Addictive substances may induce a rapid neurological deterioration in fragile X-associated tremor ataxia syndrome: a report of two cases. Intractable Rare Dis. Res. 3, 162–165. 10.5582/irdr.2014.01023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myrick L. K., Deng P. Y., Hashimoto H., Oh Y. M., Cho Y., Poidevin M. J., et al. (2015). Independent role for presynaptic FMRP revealed by an FMR1 missense mutation associated with intellectual disability and seizures. Proc. Natl. Acad. Sci. U S A 112, 949–956. 10.1073/pnas.1423094112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myrick L. K., Nakamoto-Kinoshita M., Lindor N. M., Kirmani S., Cheng X., Warren S. T. (2014). Fragile X syndrome due to a missense mutation. Eur. J. Hum. Genet. 22, 1185–1189. 10.1038/ejhg.2013.311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadel Y., Weisman-Shomer P., Fry M. (1995). The fragile X syndrome single strand d(CGG)n nucleotide repeats readily fold back to form unimolecular hairpin structures. J. Biol. Chem. 270, 28970–28977. 10.1074/jbc.270.48.28970 [DOI] [PubMed] [Google Scholar]
- Nakamoto M., Nalavadi V., Epstein M. P., Narayanan U., Bassell G. J., Warren S. T. (2007). Fragile X mental retardation protein deficiency leads to excessive mGluR5-dependent internalization of AMPA receptors. Proc. Natl. Acad. Sci. U S A 104, 15537–15542. 10.1073/pnas.0707484104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Namdar-Aligoodarzi P., Mohammadparast S., Zaker-Kandjani B., Talebi Kakroodi S., Jafari Vesiehsari M., Ohadi M. (2015). Exceptionally long 5’ UTR short tandem repeats specifically linked to primates. Gene 569, 88–94. 10.1016/j.gene.2015.05.053 [DOI] [PubMed] [Google Scholar]
- Napierala M., Michalowski D., de Mezer M., Krzyzosiak W. J. (2005). Facile FMR1 mRNA structure regulation by interruptions in CGG repeats. Nucleic Acids Res. 33, 451–463. 10.1093/nar/gki186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narayanan U., Nalavadi V., Nakamoto M., Thomas G., Ceman S., Bassell G. J., et al. (2008). S6K1 phosphorylates and regulates fragile X mental retardation protein (FMRP) with the neuronal protein synthesis-dependent mammalian target of rapamycin (mTOR) signaling cascade. J. Biol. Chem. 283, 18478–18482. 10.1074/jbc.C800055200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson D. L., Orr H. T., Warren S. T. (2013). The unstable repeats–three evolving faces of neurological disease. Neuron 77, 825–843. 10.1016/j.neuron.2013.02.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neubert F. X., Mars R. B., Thomas A. G., Sallet J., Rushworth M. F. (2014). Comparison of human ventral frontal cortex areas for cognitive control and language with areas in monkey frontal cortex. Neuron 81, 700–713. 10.1016/j.neuron.2013.11.012 [DOI] [PubMed] [Google Scholar]
- Neves G., Cooke S. F., Bliss T. V. (2008). Synaptic plasticity, memory and the hippocampus: a neural network approach to causality. Nat. Rev. Neurosci. 9, 65–75. 10.1038/nrn2303 [DOI] [PubMed] [Google Scholar]
- Neyman S., Manahan-Vaughan D. (2008). Metabotropic glutamate receptor 1 (mGluR1) and 5 (mGluR5) regulate late phases of LTP and LTD in the hippocampal CA1 region in vitro. Eur. J. Neurosci. 27, 1345–1352. 10.1111/j.1460-9568.2008.06109.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nichol Edamura K., Leonard M. R., Pearson C. E. (2005). Role of replication and CpG methylation in fragile X syndrome CGG deletions in primate cells. Am. J. Hum. Genet. 76, 302–311. 10.1086/427928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niere F., Wilkerson J. R., Huber K. M. (2012). Evidence for a fragile X mental retardation protein-mediated translational switch in metabotropic glutamate receptor-triggered Arc translation and long-term depression. J. Neurosci. 32, 5924–5936. 10.1523/JNEUROSCI.4650-11.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niu Y., Shen B., Cui Y., Chen Y., Wang J., Wang L., et al. (2014). Generation of gene-modified cynomolgus monkey via Cas9/RNA-mediated gene targeting in one-cell embryos. Cell 156, 836–843. 10.1016/j.cell.2014.01.027 [DOI] [PubMed] [Google Scholar]
- Nolin S. L., Brown W. T., Glicksman A., Houck G. E., Jr., Gargano A. D., Sullivan A., et al. (2003). Expansion of the fragile X CGG repeat in females with premutation or intermediate alleles. Am. J. Hum. Genet. 72, 454–464. 10.1086/367713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolin S. L., Glicksman A., Ersalesi N., Dobkin C., Brown W. T., Cao R., et al. (2015). Fragile X full mutation expansions are inhibited by one or more AGG interruptions in premutation carriers. Genet. Med. 17, 358–364. 10.1038/gim.2014.106 [DOI] [PubMed] [Google Scholar]
- Nolin S. L., Houck G. E., Jr., Gargano A. D., Blumstein H., Dobkin C. S., Brown W. T. (1999). FMR1 CGG-repeat instability in single sperm and lymphocytes of fragile-X premutation males. Am. J. Hum. Genet. 65, 680–688. 10.1086/302543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolin S. L., Lewis F. A., III., Ye L. L., Houck G. E., Jr., Glicksman A. E., Limprasert P., et al. (1996). Familial transmission of the FMR1 CGG repeat. Am. J. Hum. Genet. 59, 1252–1261. [PMC free article] [PubMed] [Google Scholar]
- Nolin S. L., Sah S., Glicksman A., Sherman S. L., Allen E., Berry-Kravis E., et al. (2013). Fragile X AGG analysis provides new risk predictions for 45–69 repeat alleles. Am. J. Med. Genet. A 4, 771–778. 10.1002/ajmg.a.35833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nosyreva E. D., Huber K. M. (2006). Metabotropic receptor-dependent long-term depression persists in the absence of protein synthesis in the mouse model of fragile X syndrome. J. Neurophysiol. 95, 3291–3295. 10.1152/jn.01316.2005 [DOI] [PubMed] [Google Scholar]
- Oberheim N. A., Takano T., Han X., He W., Lin J. H., Wang F., et al. (2009). Uniquely hominid features of adult human astrocytes. J. Neurosci. 29, 3276–3287. 10.1523/JNEUROSCI.4707-08.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oberlé I., Rousseau F., Heitz D., Kretz C., Devys D., Hanauer A., et al. (1991). Instability of a 550-base pair DNA segment and abnormal methylation in fragile X syndrome. Science 252, 1097–1102. 10.1126/science.252.5009.1097 [DOI] [PubMed] [Google Scholar]
- Oberman L., Ifert-Miller F., Najib U., Bashir S., Woollacott I., Gonzalez-Heydrich J., et al. (2010). Transcranial magnetic stimulation provides means to assess cortical plasticity and excitability in humans with fragile x syndrome and autism spectrum disorder. Front. Synaptic Neurosci. 2:26. 10.3389/fnsyn.2010.00026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohadi M., Valipour E., Ghadimi-Haddadan S., Namdar-Aligoodarzi P., Bagheri A., Kowsari A., et al. (2015). Core promoter short tandem repeats as evolutionary switch codes for primate speciation. Am. J. Primatol. 77, 34–43. 10.1002/ajp.22308 [DOI] [PubMed] [Google Scholar]
- Oikonomidis L., Santangelo A. M., Shiba Y., Clarke F. H., Robbins T. W., Roberts A. C. (2017). A dimensional approach to modeling symptoms of neuropsychiatric disorders in the marmoset monkey. Dev. Neurobiol. 77, 328–353. 10.1002/dneu.22446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olmos-Serrano J. L., Corbin J. G., Burns M. P. (2011). The GABAA receptor agonist THIP ameliorates specific behavioral deficits in the mouse model of fragile X syndrome. Dev. Neurosci. 33, 395–403. 10.1159/000332884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olmos-Serrano J. L., Paluszkiewicz S. M., Martin B. S., Kaufmann W. E., Corbin J. G., Huntsman M. M. (2010). Defective GABAergic neurotransmission and pharmacological rescue of neuronal hyperexcitability in the amygdala in a mouse model of fragile X syndrome. J. Neurosci. 30, 9929–9938. 10.1523/JNEUROSCI.1714-10.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oostra B. A. (1998). “Instability of triplet repeats: factors and mechanisms,” in Trinucleotide Diseases and Instability, eds Wells R. D., Bacolla A., Bowater R. P. (Berlin, Heidelberg: Springer-Verlag; ), 133–165. [DOI] [PubMed] [Google Scholar]
- Orban G. A., Claeys K., Nelissen K., Smans R., Sunaert S., Todd J. T., et al. (2006). Mapping the parietal cortex of human and non-human primates. Neuropsychologia 44, 2647–2667. 10.1016/j.neuropsychologia.2005.11.001 [DOI] [PubMed] [Google Scholar]
- Orekhova E. V., Stroganova T. A., Prokofyev A. O., Nygren G., Gillberg C., Elam M. (2008). Sensory gating in young children with autism: relation to age, IQ and EEG γ oscillations. Neurosci. Lett. 434, 218–223. 10.1016/j.neulet.2008.01.066 [DOI] [PubMed] [Google Scholar]
- Ornstein P. A., Schaaf J. M., Hooper S. R., Hatton D. D., Mirrett P., Bailey D. B., Jr. (2008). Memory skills of boys with fragile X syndrome. Am. J. Ment. Retard. 113, 453–465. 10.1352/2008.113:453-465 [DOI] [PubMed] [Google Scholar]
- Osterweil E. K., Chuang S. C., Chubykin A. A., Sidorov M., Bianchi R., Wong R. K., et al. (2013). Lovastatin corrects excess protein synthesis and prevents epileptogenesis in a mouse model of fragile X syndrome. Neuron 77, 243–250. 10.1016/j.neuron.2012.01.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osterweil E. K., Krueger D. D., Reinhold K., Bear M. F. (2010). Hypersensitivity to mGluR5 and ERK1/2 leads to excessive protein synthesis in the hippocampus of a mouse model of fragile X syndrome. J. Neurosci. 30, 15616–15627. 10.1523/JNEUROSCI.3888-10.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacey L. K., Doss L., Cifelli C., van der Kooy D., Heximer S. P., Hampson D. R. (2011a). Genetic deletion of regulator of G-protein signaling 4 (RGS4) rescues a subset of fragile X related phenotypes in the FMR1 knockout mouse. Mol. Cell. Neurosci. 46, 563–572. 10.1016/j.mcn.2010.12.005 [DOI] [PubMed] [Google Scholar]
- Pacey L. K., Tharmalingam S., Hampson D. R. (2011b). Subchronic administration and combination metabotropic glutamate and GABAB receptor drug therapy in fragile X syndrome. J. Pharmacol. Exp. Ther. 338, 897–905. 10.1124/jpet.111.183327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padmashri R., Reiner B. C., Suresh A., Spartz E., Dunaevsky A. (2013). Altered structural and functional synaptic plasticity with motor skill learning in a mouse model of fragile X syndrome. J. Neurosci. 33, 19715–19723. 10.1523/JNEUROSCI.2514-13.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pai A. A., Bell J. T., Marioni J. C., Pritchard J. K., Gilad Y. (2011). A genome-wide study of DNA methylation patterns and gene expression levels in multiple human and chimpanzee tissues. PLoS Genet. 7:24. 10.1371/journal.pgen.1001316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paigen K. (2003). One hundred years of mouse genetics: an intellectual history. I. The classical period (1902–1980). Genetics 163, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paluszkiewicz S. M., Olmos-Serrano J. L., Corbin J. G., Huntsman M. M. (2011). Impaired inhibitory control of cortical synchronization in fragile X syndrome. J. Neurophysiol. 106, 2264–2272. 10.1152/jn.00421.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paoloni-Giacobino A., D’Aiuto L., Cirio M. C., Reinhart B., Chaillet J. R. (2007). Conserved features of imprinted differentially methylated domains. Gene 399, 33–45. 10.1016/j.gene.2007.04.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paradee W., Melikian H. E., Rasmussen D. L., Kenneson A., Conn P. J., Warren S. T. (1999). Fragile X mouse: strain effects of knockout phenotype and evidence suggesting deficient amygdala function. Neuroscience 94, 185–192. 10.1016/s0306-4522(99)00285-7 [DOI] [PubMed] [Google Scholar]
- Pardo M., Beurel E., Jope R. S. (2017). Cotinine administration improves impaired cognition in the mouse model of Fragile X syndrome. Eur. J. Neurosci. 45, 490–498. 10.1111/ejn.13446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park C. Y., Halevy T., Lee D. R., Sung J. J., Lee J. S., Yanuka O., et al. (2015). Reversion of FMR1 methylation and silencing by editing the triplet repeats in fragile X iPSC-derived neurons. Cell Rep. 13, 234–241. 10.1016/j.celrep.2015.08.084 [DOI] [PubMed] [Google Scholar]
- Park S., Park J. M., Kim S., Kim J. A., Shepherd J. D., Smith-Hicks C. L., et al. (2008). Elongation factor 2 and fragile X mental retardation protein control the dynamic translation of Arc/Arg3.1 essential for mGluR-LTD. Neuron 59, 70–83. 10.1016/j.neuron.2008.05.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park J. E., Zhang X. F., Choi S. H., Okahara J., Sasaki E., Silva A. C. (2016). Generation of transgenic marmosets expressing genetically encoded calcium indicators. Sci. Rep. 6:34931. 10.1038/srep34931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel P. K., Bhavesh N. S., Hosur R. V. (2000). Cation-dependent conformational switches in d-TGGCGGC containing two triplet repeats of Fragile X Syndrome: NMR observations. Biochem. Biophys. Res. Commun. 278, 833–838. 10.1006/bbrc.2000.3878 [DOI] [PubMed] [Google Scholar]
- Patel A. B., Hays S. A., Bureau I., Huber K. M., Gibson J. R. (2013). A target cell-specific role for presynaptic Fmr1 in regulating glutamate release onto neocortical fast-spiking inhibitory neurons. J. Neurosci. 33, 2593–2604. 10.1523/JNEUROSCI.2447-12.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul K., Venkitaramani D. V., Cox C. L. (2013). Dampened dopamine-mediated neuromodulation in prefrontal cortex of fragile X mice. J. Physiol. 591, 1133–1143. 10.1113/jphysiol.2012.241067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peier A. M., Nelson D. L. (2002). Instability of a premutation-sized CGG repeat in FMR1 YAC transgenic mice. Genomics 80, 423–432. 10.1006/geno.2002.6849 [DOI] [PubMed] [Google Scholar]
- Pellerin D., Çaku A., Fradet M., Bouvier P., Dubé J., Corbin F. (2016). Lovastatin corrects ERK pathway hyperactivation in fragile X syndrome: potential of platelet’s signaling cascades as new outcome measures in clinical trials. Biomarkers 21, 497–508. 10.3109/1354750x.2016.1160289 [DOI] [PubMed] [Google Scholar]
- Pereira S., Veeraraghavan P., Ghosh S., Gandhi M. (2004). Animal experimentation and ethics in India: the CPCSEA makes a difference. Altern. Lab. Anim. 32, 411–415. [DOI] [PubMed] [Google Scholar]
- Petersen B. (2017). Basics of genome editing technology and its application in livestock species. Reprod. Domest. Anim. 3, 4–13. 10.1111/rda.13012 [DOI] [PubMed] [Google Scholar]
- Pezer Z., Brajković J., Feliciello I., Ugarkovć D. (2012). Satellite DNA-mediated effects on genome regulation. Genome Dyn. 7, 153–169. 10.1159/000337116 [DOI] [PubMed] [Google Scholar]
- Phillips K. A., Bales K. L., Capitanio J. P., Conley A., Czoty P. W., ‘t Hart B. A., et al. (2014). Why primate models matter. Am. J. Primatol. 76, 801–827. 10.1002/ajp.22281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieretti M., Zhang F. P., Fu Y. H., Warren S. T., Oostra B. A., Caskey C. T., et al. (1991). Absence of expression of the FMR-1 gene in fragile X syndrome. Cell 66, 817–822. 10.1016/0092-8674(91)90125-i [DOI] [PubMed] [Google Scholar]
- Pietrobono R., Tabolacci E., Zalfa F., Zito I., Terracciano A., Moscato U., et al. (2005). Molecular dissection of the events leading to inactivation of the FMR1 gene. Hum. Mol. Genet. 14, 267–277. 10.1093/hmg/ddi024 [DOI] [PubMed] [Google Scholar]
- Pietropaolo S., Goubran M. G., Joffre C., Aubert A., Lemaire-Mayo V., Crusio W. E., et al. (2014). Dietary supplementation of omega-3 fatty acids rescues fragile X phenotypes in Fmr1-Ko mice. Psychoneuroendocrinology 49, 119–129. 10.1016/j.psyneuen.2014.07.002 [DOI] [PubMed] [Google Scholar]
- Pistorio A. L., Vintch B., Wang X. (2006). Acoustic analysis of vocal development in a New World primate, the common marmoset (Callithrix jacchus). J. Acoust. Soc. Am. 120, 1655–1670. 10.1121/1.2225899 [DOI] [PubMed] [Google Scholar]
- Plohl M., Meštrović N., Mravinac B. (2012). Satellite DNA evolution. Genome Dyn. 7, 126–152. 10.1159/000337122 [DOI] [PubMed] [Google Scholar]
- Powell W. T., Coulson R. L., Gonzales M. L., Crary F. K., Wong S. S., Adams S., et al. (2013). R-loop formation at Snord116 mediates topotecan inhibition of Ube3a-antisense and allele-specific chromatin decondensation. Proc. Natl. Acad. Sci. U S A 110, 13938–13943. 10.1073/pnas.1305426110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pretto D., Yrigollen C. M., Tang H. T., Williamson J., Espinal G., Iwahashi C. K., et al. (2014). Clinical and molecular implications of mosaicism in FMR1 full mutations. Front. Genet. 5:318. 10.3389/fgene.2014.00318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preuss T. M. (2011). The human brain: rewired and running hot. Ann. N Y Acad. Sci. 1225, E182–E191. 10.1111/j.1749-6632.2011.06001.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primerano B., Tassone F., Hagerman R. J., Hagerman P., Amaldi F., Bagni C. (2002). Reduced FMR1 mRNA translation efficiency in fragile X patients with premutations. RNA 8, 1482–1488. [PMC free article] [PubMed] [Google Scholar]
- Quartier A., Poquet H., Gilbert-Dussardier B., Rossi M., Casteleyn A. S., Portes V. D., et al. (2017). Intragenic FMR1 disease-causing variants: a significant mutational mechanism leading to Fragile-X syndrome. Eur. J. Hum. Genet. 25, 423–431. 10.1038/ejhg.2016.204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quilez J., Guilmatre A., Garg P., Highnam G., Gymrek M., Erlich Y., et al. (2016). Polymorphic tandem repeats within gene promoters act as modifiers of gene expression and DNA methylation in humans. Nucleic Acids Res. 44, 3750–3762. 10.1093/nar/gkw219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radwan B., Dvorak D., Fenton A. A. (2016). Impaired cognitive discrimination and discoordination of coupled theta-γ oscillations in Fmr1 knockout mice. Neurobiol. Dis. 88, 125–138. 10.1016/j.nbd.2016.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajan-Babu I. S., Chong S. S. (2016). Molecular correlates and recent advancements in the diagnosis and screening of FMR1-related disorders. Genes (Basel) 7:E87. 10.3390/genes7100087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranganath C., Ritchey M. (2012). Two cortical systems for memory-guided behaviour. Nat. Rev. Neurosci. 13, 713–726. 10.1038/nrn3338 [DOI] [PubMed] [Google Scholar]
- Reisin H. D., Colombo J. A. (2002). Astroglial interlaminar processes in human cerebral cortex: variations in cytoskeletal profiles. Brain Res. 937, 51–57. 10.1016/s0006-8993(02)02464-2 [DOI] [PubMed] [Google Scholar]
- Reyniers E., Martin J.-J., Cras P., Van Marck E., Handig I., Jorens H. Z. J., et al. (1999). Postmortem examination of two fragile X brothers with an FMR1 full mutation. Am. J. Med. Genet. 84, 245–249. [DOI] [PubMed] [Google Scholar]
- Reyniers E., Vits L., De Boulle K., Roy B. V., Velzen D. V., de Graaff E., et al. (1993). The full mutation in the FMR-1 gene of male fragile X patients is absent in their sperm. Nat. Genet. 4, 143–146. 10.1038/ng0693-143 [DOI] [PubMed] [Google Scholar]
- Rezazadeh M., Gharesouran J., Mirabzadeh A., Khorram Khorshid H. R., Biglarian A., Ohadi M. (2015). A primate-specific functional GTTT-repeat in the core promoter of CYTH4 is linked to bipolar disorder in human. Prog. Neuropsychopharmacol. Biol. Psychiatry 56, 161–167. 10.1016/j.pnpbp.2014.09.001 [DOI] [PubMed] [Google Scholar]
- Riedel G., Reymann K. G. (1996). Metabotropic glutamate receptors in hippocampal long-term potentiation and learning and memory. Acta Physiol. Scand. 157, 1–19. 10.1046/j.1365-201x.1996.484231000.x [DOI] [PubMed] [Google Scholar]
- Riley D. E., Krieger J. N. (2009). Embryonic nervous system genes predominate in searches for dinucleotide simple sequence repeats flanked by conserved sequences. Gene 429, 74–79. 10.1016/j.gene.2008.09.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts J. E., Hennon E. A., Price J. R., Dear E., Anderson K., Vandergrift N. A. (2007). Expressive language during conversational speech in boys with fragile X syndrome. Am. J. Ment. Retard. 112, 1–17. 10.1352/0895-8017(2007)112[1:eldcsi]2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- Robertson C. E., Ratai E. M., Kanwisher N. (2016). Reduced GABAergic action in the autistic brain. Curr. Biol. 26, 80–85. 10.1016/j.cub.2015.11.019 [DOI] [PubMed] [Google Scholar]
- Robinson A. N., Roberts J. E., Brady N. C., McQuillin S. D., Warren S. F. (2016). Physiological correlates of maternal responsivity in mothers of preschoolers with fragile X syndrome. Am. J. Intellect. Dev. Disabil. 121, 111–120. 10.1352/1944-7558-121.2.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronesi J. A., Collins K. A., Hays S. A., Tsai N.-P., Guo W., Birnbaum S. G., et al. (2012). Disrupted mGluR5-Homer scaffolds mediate abnormal mGluR5 signaling, circuit function and behavior in a mouse model of Fragile X Syndrome. Nat. Neurosci. 15:S431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronesi J. A., Huber K. M. (2008). Homer interactions are necessary for metabotropic glutamate receptor-induced long-term depression and translational activation. J. Neurosci. 28, 543–547. 10.1523/JNEUROSCI.5019-07.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosati A. G., Arre A. M., Platt M. L., Santos L. R. (2016). Rhesus monkeys show human-like changes in gaze following across the lifespan. Proc. Biol. Sci. 283:20160376. 10.1098/rspb.2016.0376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotschafer S., Razak K. (2013). Altered auditory processing in a mouse model of fragile X syndrome. Brain Res. 19, 12–24. 10.1016/j.brainres.2013.02.038 [DOI] [PubMed] [Google Scholar]
- Routh B. N., Rathour R. K., Baumgardner M. E., Kalmbach B. E., Johnston D., Brager D. H. (2017). Increased transient Na+ conductance and action potential output in layer 2/3 prefrontal cortex neurons of the fmr1-/y mouse. J. Physiol. 595, 4431–4448. 10.1113/JP274258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabanov V., Braat S., D’Andrea L., Willemsen R., Zeidler S., Rooms L., et al. (2016). Impaired GABAergic inhibition in the hippocampus of Fmr1 knockout mice. Neuropharmacology 116, 71–81. 10.1016/j.neuropharm.2016.12.010 [DOI] [PubMed] [Google Scholar]
- Sabaratnam M., Vroegop P. G., Gangadharan S. K. (2001). Epilepsy and EEG findings in 18 males with fragile X syndrome. Seizure 10, 60–63. 10.1053/seiz.2000.0492 [DOI] [PubMed] [Google Scholar]
- Sabino F. C., Ribeiro A. O., Tufik S., Torres L. B., Oliveira J. A., Mello L. E., et al. (2014). Evolutionary history of the PER3 variable number of tandem repeats (VNTR): idiosyncratic aspect of primate molecular circadian clock. PLoS One 9:e107198. 10.1371/journal.pone.0107198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saffary R., Xie Z. (2011). FMRP regulates the transition from radial glial cells to intermediate progenitor cells during neocortical development. J. Neurosci. 31, 1427–1439. 10.1523/JNEUROSCI.4854-10.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saito A. (2015). The marmoset as a model for the study of primate parental behavior. Neurosci. Res. 93, 99–109. 10.1016/j.neures.2014.12.011 [DOI] [PubMed] [Google Scholar]
- Salcedo-Arellano M. J., Lozano R., Tassone F., Hagerman R. J., Saldarriaga W. (2016). Alcohol use dependence in fragile X syndrome. Intractable Rare Dis. Res. 5, 207–213. 10.5582/irdr.2016.01046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saldarriaga W., Tassone F., González-Teshima L. Y., Forero-Forero J. V., Ayala-Zapata S., Hagerman R. (2014). Fragile X syndrome. Colomb. Med. 45, 190–198. [PMC free article] [PubMed] [Google Scholar]
- Santa Maria L., Pugin A., Alliende M. A., Aliaga S., Curotto B., Aravena T., et al. (2014). FXTAS in an unmethylated mosaic male with fragile X syndrome from Chile. Clin. Genet. 86, 378–382. 10.1111/cge.12278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saré R. M., Song A., Loutaev I., Cook A., Maita I., Lemons A., et al. (2018). Negative effects of chronic rapamycin treatment on behavior in a mouse model of fragile X syndrome. Front. Mol. Neurosci. 10:452. 10.3389/fnmol.2017.00452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasaki E., Suemizu H., Shimada A., Hanazawa K., Oiwa R., Kamioka M., et al. (2009). Generation of transgenic non-human primates with germline transmission. Nature 459, 523–527. 10.1038/nature08090 [DOI] [PubMed] [Google Scholar]
- Sato K., Oiwa R., Kumita W., Henry R., Sakuma T., Ito R., et al. (2016). Generation of a nonhuman primate model of severe combined immunodeficiency using highly efficient genome editing. Cell Stem Cell 19, 127–138. 10.1016/j.stem.2016.06.003 [DOI] [PubMed] [Google Scholar]
- Sawaya S., Bagshaw A., Buschiazzo E., Kumar P., Chowdhury S., Black M. A., et al. (2013). Microsatellite tandem repeats are abundant in human promoters and are associated with regulatory elements. PLoS One 8:e54710. 10.1371/journal.pone.0054710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawaya S. M., Bagshaw A. T., Buschiazzo E., Gemmell N. J. (2012). Promoter microsatellites as modulators of human gene expression. Adv. Exp. Med. Biol. 769, 41–54. 10.1007/978-1-4614-5434-2_4 [DOI] [PubMed] [Google Scholar]
- Sawicka K., Pyronneau A., Chao M., Bennett M. V., Zukin R. S. (2016). Elevated ERK/p90 ribosomal S6 kinase activity underlies audiogenic seizure susceptibility in fragile X mice. Proc. Natl. Acad. Sci. U S A 113, E6290–E6297. 10.1073/pnas.1610812113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scharf S. H., Jaeschke G., Wettstein J. G., Lindemann L. (2015). Metabotropic glutamate receptor 5 as drug target for Fragile X syndrome. Curr. Opin. Pharmacol. 20, 124–134. 10.1016/j.coph.2014.11.004 [DOI] [PubMed] [Google Scholar]
- Schibler L., Roig A., Mahe M. F., Laurent P., Hayes H., Rodolphe F., et al. (2006). High-resolution comparative mapping among man, cattle and mouse suggests a role for repeat sequences in mammalian genome evolution. BMC Genomics 7:194. 10.1186/1471-2164-7-194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiel N., Souto A. (2017). The common marmoset: an overview of its natural history, ecology and behavior. Dev. Neurobiol. 77, 244–262. 10.1002/dneu.22458 [DOI] [PubMed] [Google Scholar]
- Schmidt A., Morales-Prieto D. M., Pastuschek J., Fröhlich K., Markert U. R. (2015). Only humans have human placentas: molecular differences between mice and humans. J. Reprod. Immunol. 108, 65–71. 10.1016/j.jri.2015.03.001 [DOI] [PubMed] [Google Scholar]
- Selby L., Zhang C., Sun Q. Q. (2007). Major defects in neocortical GABAergic inhibitory circuits in mice lacking the fragile X mental retardation protein. Neurosci. Lett. 412, 227–232. 10.1016/j.neulet.2006.11.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semendeferi K., Lu A., Schenker N., Damasio H. (2002). Humans and great apes share a large frontal cortex. Nat. Neurosci. 5, 272–276. 10.1038/nn814 [DOI] [PubMed] [Google Scholar]
- Semendeferi K., Teffer K., Buxhoeveden D. P., Park M. S., Bludau S., Amunts K., et al. (2011). Spatial organization of neurons in the frontal pole sets humans apart from great apes. Cereb. Cortex 21, 1485–1497. 10.1093/cercor/bhQ211 [DOI] [PubMed] [Google Scholar]
- Shang Y., Wang H., Mercaldo V., Li X., Chen T., Zhuo M. (2009). Fragile X mental retardation protein is required for chemically-induced long-term potentiation of the hippocampus in adult mice. J. Neurochem. 111, 635–646. 10.1111/j.1471-4159.2009.06314.x [DOI] [PubMed] [Google Scholar]
- Sharma A., Hoeffer C. A., Takayasu Y., Miyawaki T., McBride S. M., Klann E., et al. (2010). Dysregulation of mTOR signaling in fragile X syndrome. J. Neurosci. 30, 694–702. 10.1523/JNEUROSCI.3696-09.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheridan S. D., Theriault K. M., Reis S. A., Zhou F., Madison J. M., Daheron L., et al. (2011). Epigenetic characterization of the FMR1 gene and aberrant neurodevelopment in human induced pluripotent stem cell models of fragile X syndrome. PLoS One 6:e26203. 10.1371/journal.pone.0026203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidhu H., Dansie L. E., Hickmott P. W., Ethell D. W., Ethell I. M. (2014). Genetic removal of matrix metalloproteinase 9 rescues the symptoms of fragile X syndrome in a mouse model. J. Neurosci. 34, 9867–9879. 10.1523/JNEUROSCI.1162-14.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sigurdsson T., Duvarci S. (2016). Hippocampal-prefrontal interactions in cognition, behavior and psychiatric disease. Front. Syst. Neurosci. 9:190. 10.3389/fnsys.2015.00190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons Z. L., Roney J. R. (2011). Variation in CAG repeat length of the androgen receptor gene predicts variables associated with intrasexual competitiveness in human males. Horm. Behav. 60, 306–312. 10.1016/j.yhbeh.2011.06.006 [DOI] [PubMed] [Google Scholar]
- Siomi H., Choi M., Siomi M. C., Nussbaum R. L., Dreyfuss G. (1994). Essential role for KH domains in RNA binding: impaired RNA binding by a mutation in the KH domain of FMR1 that causes fragile X syndrome. Cell 77, 33–39. 10.1016/0092-8674(94)90232-1 [DOI] [PubMed] [Google Scholar]
- Smeets H. J., Smits A. P., Verheij C. E., Theelen J. P., Willemsen R., van de Burgt I., et al. (1995). Normal phenotype in two brothers with a full FMR1 mutation. Hum. Mol. Genet. 4, 2103–2108. 10.1093/hmg/4.11.2103 [DOI] [PubMed] [Google Scholar]
- Smith L. E., Hong J., Greenberg J. S., Mailick M. R. (2016). Change in the behavioral phenotype of adolescents and adults with FXS: role of the family environment. J. Autism Dev. Disord. 46, 1824–1833. 10.1007/s10803-016-2714-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smrzka O. W., Faé I., Stöger R., Kurzbauer R., Fischer G. F., Henn T., et al. (1995). Conservation of a maternal-specific methylation signal at the human IGF2R locus. Hum. Mol. Genet. 4, 1945–1952. 10.1093/hmg/4.10.1945 [DOI] [PubMed] [Google Scholar]
- Sousa M. B., Albuquerque A. C., Albuquerque Fda S., Araujo A., Yamamoto M. E., Arruda Mde F. (2005). Behavioral strategies and hormonal profiles of dominant and subordinate common marmoset (Callithrix jacchus) females in wild monogamous groups. Am. J. Primatol. 67, 37–50. 10.1002/ajp.20168 [DOI] [PubMed] [Google Scholar]
- Spinelli S., Pennanen L., Dettling A. C., Feldon J., Higgins G. A., Pryce C. R. (2004). Performance of the marmoset monkey on computerized tasks of attention and working memory. Cogn. Brain Res. 19, 123–137. 10.1016/j.cogbrainres.2003.11.007 [DOI] [PubMed] [Google Scholar]
- Street S. E., Navarrete A. F., Reader S. M., Laland K. N. (2017). Coevolution of cultural intelligence, extended life history, sociality and brain size in primates. Proc. Natl. Acad. Sci. U S A 24:1620734114. 10.1073/pnas.1620734114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuber E. F., Baumgartner C., Dingemanse N. J., Kempenaers B., Mueller J. C. (2016). Genetic correlates of individual differences in sleep behavior of free-living great tits (Parus major). G3 (Bethesda) 6, 599–607. 10.1534/g3.115.024216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su T., Fan H. X., Jiang T., Sun W. W., Den W. Y., Gao M. M., et al. (2011). Early continuous inhibition of group 1 mGlu signaling partially rescues dendritic spine abnormalities in the Fmr1 knockout mouse model for fragile X syndrome. Psychopharmacology 215, 291–300. 10.1007/s00213-010-2130-2 [DOI] [PubMed] [Google Scholar]
- Subramanian P. S., Nelson D. L., Chinault A. C. (1996). Large domains of apparent delayed replication timing associated with triplet repeat expansion at FRAXA and FRAXE. Am. J. Hum. Genet. 59, 407–416. [PMC free article] [PubMed] [Google Scholar]
- Sun M. K., Hongpaisan J., Alkon D. L. (2016). Rescue of synaptic phenotypes and spatial memory in young fragile X mice. J. Pharmacol. Exp. Ther. 357, 300–310. 10.1124/jpet.115.231100 [DOI] [PubMed] [Google Scholar]
- Sun M. K., Hongpaisan J., Lim C. S., Alkon D. L. (2014). Bryostatin-1 restores hippocampal synapses and spatial learning and memory in adult fragile x mice. J. Pharmacol. Exp. Ther. 349, 393–401. 10.1124/jpet.114.214098 [DOI] [PubMed] [Google Scholar]
- Sutcliffe J. S., Nelson D. L., Zhang F., Pieretti M., Caskey C. T., Saxe D., et al. (1992). DNA methylation represses FMR-1 transcription in fragile X syndrome. Hum. Mol. Genet. 1, 397–400. 10.1093/hmg/1.6.397 [DOI] [PubMed] [Google Scholar]
- Suvrathan A., Hoeffer C. A., Wong H., Klann E., Chattarji S. (2010). Characterization and reversal of synaptic defects in the amygdala in a mouse model of fragile X syndrome. Proc. Natl. Acad. Sci. U S A 107, 11591–11596. 10.1073/pnas.1002262107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzumori K., Yamauchi M., Seki N., Kondo I., Hori T. (1993). Prenatal diagnosis of a hypermethylated full fragile X mutation in chorionic villi of a male fetus. J. Med. Genet. 30, 785–787. 10.1136/jmg.30.9.785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Symonds E. L., Peiris M., Page A. J., Chia B., Dogra H., Masding A., et al. (2015). Mechanisms of activation of mouse and human enteroendocrine cells by nutrients. Gut 64, 618–626. 10.1136/gutjnl-2014-306834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabata H., Yoshinaga S., Nakajima K. (2012). Cytoarchitecture of mouse and human subventricular zone in developing cerebral neocortex. Exp. Brain Res. 216, 161–168. 10.1007/s00221-011-2933-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabolacci E., Mancano G., Lanni S., Palumbo F., Goracci M., Ferre F., et al. (2016a). Genome-wide methylation analysis demonstrates that 5-aza-2-deoxycytidine treatment does not cause random DNA demethylation in fragile X syndrome cells. Epigenetics Chromatin 9, 016–0060. 10.1186/s13072-016-0060-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabolacci E., Palumbo F., Nobile V., Neri G. (2016b). Transcriptional reactivation of the FMR1 gene. A possible approach to the treatment of the fragile X syndrome. Genes 7:E49. 10.3390/genes7080049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabolacci E., Moscato U., Zalfa F., Bagni C., Chiurazzi P., Neri G. (2008). Epigenetic analysis reveals a euchromatic configuration in the FMR1 unmethylated full mutations. Eur. J. Hum. Genet. 16, 1487–1498. 10.1038/ejhg.2008.130 [DOI] [PubMed] [Google Scholar]
- Tabolacci E., Pietrobono R., Moscato U., Oostra B. A., Chiurazzi P., Neri G. (2005). Differential epigenetic modifications in the FMR1 gene of the fragile X syndrome after reactivating pharmacological treatments. Eur. J. Hum. Genet. 13, 641–648. 10.1038/sj.ejhg.5201393 [DOI] [PubMed] [Google Scholar]
- Takahashi D. Y., Fenley A. R., Ghazanfar A. A. (2016). Early development of turn-taking with parents shapes vocal acoustics in infant marmoset monkeys. Philos. Trans. R. Soc. Lond. B Biol. Sci. 371:20150370. 10.1098/rstb.2015.0370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi D. Y., Fenley A. R., Teramoto Y., Narayanan D. Z., Borjon J. I., Holmes P., et al. (2015). LANGUAGE DEVELOPMENT. The developmental dynamics of marmoset monkey vocal production. Science 349, 734–738. 10.1126/science.aab1058 [DOI] [PubMed] [Google Scholar]
- Takahashi D. Y., Liao D. A., Ghazanfar A. A. (2017). Vocal learning via social reinforcement by infant marmoset monkeys. Curr. Biol. 27, 1844–1852. 10.1016/j.cub.2017.05.004 [DOI] [PubMed] [Google Scholar]
- Takahashi D. Y., Narayanan D. Z., Ghazanfar A. A. (2013). Coupled oscillator dynamics of vocal turn-taking in monkeys. Curr. Biol. 23, 2162–2168. 10.1016/j.cub.2013.09.005 [DOI] [PubMed] [Google Scholar]
- Takahashi M., Ueno Y., Fujita K. (2015). Inference in a social context: a comparative study of capuchin monkeys (Cebus apella), tree shrews (Tupaia belangeri), hamsters (Mesocricetus auratus), and rats (Rattus norvegicus). J. Comp. Psychol. 129, 402–411. 10.1037/a0039732 [DOI] [PubMed] [Google Scholar]
- Takemoto A., Izumi A., Miwa M., Nakamura K. (2011). Development of a compact and general-purpose experimental apparatus with a touch-sensitive screen for use in evaluating cognitive functions in common marmosets. J. Neurosci. Methods 199, 82–86. 10.1016/j.jneumeth.2011.04.029 [DOI] [PubMed] [Google Scholar]
- Tan W., Schauder C., Naryshkina T., Minakhina S., Steward R. (2016). Zfrp8 forms a complex with fragile-X mental retardation protein and regulates its localization and function. Dev. Biol. 410, 202–212. 10.1016/j.ydbio.2015.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang A. H., Alger B. E. (2015). Homer protein-metabotropic glutamate receptor binding regulates endocannabinoid signaling and affects hyperexcitability in a mouse model of fragile X syndrome. J. Neurosci. 35, 3938–3945. 10.1523/JNEUROSCI.4499-14.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang B., Wang T., Wan H., Han L., Qin X., Zhang Y., et al. (2015). Fmr1 deficiency promotes age-dependent alterations in the cortical synaptic proteome. Proc. Natl. Acad. Sci. U S A 112, E4697–E4706. 10.1073/pnas.1502258112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang L., Zeng Y., Du H., Gong M., Peng J., Zhang B., et al. (2017). CRISPR/Cas9-mediated gene editing in human zygotes using Cas9 protein. Mol. Genet. Genomics 292, 525–533. 10.1007/s00438-017-1299-z [DOI] [PubMed] [Google Scholar]
- Taqi M. M., Wärmländer S. K. T. S., Yamskova O., Madani F., Bazov I., Luo J., et al. (2012). Conformation effects of CpG methylation on single-stranded DNA oligonucleotides: analysis of the opioid peptide dynorphin-coding sequences. PLoS One 7:e39605. 10.1371/journal.pone.0039605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tardif S. D., Coleman K., Hobbs T. R., Lutz C. (2013). IACUC review of nonhuman primate research. ILAR J. 54, 234–245. 10.1093/ilar/ilt040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tassone F., Hagerman R. J., Loesch D. Z., Lachiewicz A., Taylor A. K., Hagerman P. J. (2000a). Fragile X males with unmethylated, full mutation trinucleotide repeat expansions have elevated levels of FMR1 messenger RNA. Am. J. Med. Genet. 94, 232–236. [DOI] [PubMed] [Google Scholar]
- Tassone F., Hagerman R. J., Taylor A. K., Gane L. W., Godfrey T. E., Hagerman P. J. (2000b). Elevated levels of FMR1 mRNA in carrier males: a new mechanism of involvement in the fragile-X syndrome. Am. J. Hum. Genet. 66, 6–15. 10.1086/302720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tassone F., Hagerman R. J., Taylor A. K., Hagerman P. J. (2001). A majority of fragile X males with methylated, full mutation alleles have significant levels of FMR1 messenger RNA. J. Med. Genet. 38, 453–456. 10.1136/jmg.38.7.453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor A. K., Tassone F., Dyer P. N., Hersch S. M., Harris J. B., Greenough W. T., et al. (1999). Tissue heterogeneity of the FMR1 mutation in a high-functioning male with fragile X syndrome. Am. J. Med. Genet. 84, 233–239. [DOI] [PubMed] [Google Scholar]
- Tebartz van Elst L., Maier S., Fangmeier T., Endres D., Mueller G. T., Nickel K., et al. (2014). Disturbed cingulate glutamate metabolism in adults with high-functioning autism spectrum disorder: evidence in support of the excitatory/inhibitory imbalance hypothesis. Mol. Psychiatry 19, 1314–1325. 10.1038/mp.2014.62 [DOI] [PubMed] [Google Scholar]
- Tecott L. H. (2003). The genes and brains of mice and men. Am. J. Psychiatry 160, 646–656. 10.1176/appi.ajp.160.4.646 [DOI] [PubMed] [Google Scholar]
- Telias M., Segal M., Ben-Yosef D. (2013). Neural differentiation of Fragile X human Embryonic Stem Cells reveals abnormal patterns of development despite successful neurogenesis. Dev. Biol. 374, 32–45. 10.1016/j.ydbio.2012.11.031 [DOI] [PubMed] [Google Scholar]
- Thomas A. M., Bui N., Graham D., Perkins J. R., Yuva-Paylor L. A., Paylor R. (2011). Genetic reduction of group 1 metabotropic glutamate receptors alters select behaviors in a mouse model for fragile X syndrome. Behav. Brain Res. 223, 310–321. 10.1016/j.bbr.2011.04.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson S. R., Seo S. S., Barnes S. A., Louros S. R., Muscas M., Dando O., et al. (2017). Cell-type-specific translation profiling reveals a novel strategy for treating fragile X syndrome. Neuron 95, 550–563. 10.1016/j.neuron.2017.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian M., Zeng Y., Hu Y., Yuan X., Liu S., Li J., et al. (2015). 7, 8-Dihydroxyflavone induces synapse expression of AMPA GluA1 and ameliorates cognitive and spine abnormalities in a mouse model of fragile X syndrome. Neuropharmacology 89, 43–53. 10.1016/j.neuropharm.2014.09.006 [DOI] [PubMed] [Google Scholar]
- Tian Y., Yang C., Shang S., Cai Y., Deng X., Zhang J., et al. (2017). Loss of FMRP impaired hippocampal long-term plasticity and spatial learning in rats. Front. Mol. Neurosci. 10:269. 10.3389/fnmol.2017.00269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Till S. M., Asiminas A., Jackson A. D., Katsanevaki D., Barnes S. A., Osterweil E. K., et al. (2015). Conserved hippocampal cellular pathophysiology but distinct behavioural deficits in a new rat model of FXS. Hum. Mol. Genet. 24, 5977–5984. 10.1093/hmg/ddv299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Todd P. K., Oh S. Y., Krans A., He F., Sellier C., Frazer M., et al. (2013). CGG repeat-associated translation mediates neurodegeneration in fragile X tremor ataxia syndrome. Neuron 78, 440–455. 10.1016/j.neuron.2013.03.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toft A. K., Lundbye C. J., Banke T. G. (2016). Dysregulated NMDA-receptor signaling inhibits long-term depression in a mouse model of fragile X syndrome. J. Neurosci. 36, 9817–9827. 10.1523/JNEUROSCI.3038-15.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tokuno H., Watson C., Roberts A., Sasaki E., Okano H. (2015). Marmoset neuroscience. Neurosci. Res. 93, 1–2. 10.1016/j.neures.2015.03.001 [DOI] [PubMed] [Google Scholar]
- Truszkowski T. L., James E. J., Hasan M., Wishard T. J., Liu Z., Pratt K. G., et al. (2016). Fragile X mental retardation protein knockdown in the developing Xenopus tadpole optic tectum results in enhanced feedforward inhibition and behavioral deficits. Neural. Dev. 11:14. 10.1186/s13064-016-0069-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tu Z., Yang W., Yan S., Yin A., Gao J., Liu X., et al. (2017). Promoting Cas9 degradation reduces mosaic mutations in non-human primate embryos. Sci. Rep. 7:42081. 10.1038/srep42081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tzschach A., Ropers H.-H. (2007). Genetik der mentalen Retardierung. Dtsch Arztebl Int. 104, 1400–1405. Available online at: https://www.aerzteblatt.de/archiv/55715/Genetik-der-mentalen-Retardierung [Google Scholar]
- Udagawa T., Farny N. G., Jakovcevski M., Kaphzan H., Alarcon J. M., Anilkumar S., et al. (2013). Genetic and acute CPEB1 depletion ameliorate fragile X pathophysiology. Nat. Med. 19, 1473–1477. 10.1038/nm.3353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urbach A., Bar-Nur O., Daley G. Q., Benvenisty N. (2010). Differential modeling of fragile X syndrome by human embryonic stem cells and induced pluripotent stem cells. Cell Stem Cell 6, 407–411. 10.1016/j.stem.2010.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usdin K., Kumari D. (2015). Repeat-mediated epigenetic dysregulation of the FMR1 gene in the fragile X-related disorders. Front. Genet. 6:192. 10.3389/fgene.2015.00192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usdin K., Woodford K. J. (1995). CGG repeats associated with DNA instability and chromosome fragility form structures that block DNA synthesis in vitro. Nucleic Acids Res. 23, 4202–4209. 10.1093/nar/23.20.4202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uzunova G., Pallanti S., Hollander E. (2016). Excitatory/inhibitory imbalance in autism spectrum disorders: implications for interventions and therapeutics. World J. Biol. Psychiatry 17, 174–186. 10.3109/15622975.2015.1085597 [DOI] [PubMed] [Google Scholar]
- Valomon A., Holst S. C., Bachmann V., Viola A. U., Schmidt C., Zürcher J., et al. (2014). Genetic polymorphisms of DAT1 and COMT differentially associate with actigraphy-derived sleep-wake cycles in young adults. Chronobiol. Int. 31, 705–714. 10.3109/07420528.2014.896376 [DOI] [PubMed] [Google Scholar]
- Van Dam D., D’Hooge R., Hauben E., Reyniers E., Gantois I., Bakker C. E., et al. (2000). Spatial learning, contextual fear conditioning and conditioned emotional response in Fmr1 knockout mice. Behav. Brain Res. 117, 127–136. 10.1016/s0166-4328(00)00296-5 [DOI] [PubMed] [Google Scholar]
- Van Dam D., Errijgers V., Kooy R. F., Willemsen R., Mientjes E., Oostra B. A., et al. (2005). Cognitive decline, neuromotor and behavioural disturbances in a mouse model for fragile-X-associated tremor/ataxia syndrome (FXTAS). Behav. Brain Res. 162, 233–239. 10.1016/j.bbr.2005.03.007 [DOI] [PubMed] [Google Scholar]
- Van der Molen M. J., Huizinga M., Huizenga H. M., Ridderinkhof K. R., Van der Molen M. W., Hamel B. J., et al. (2010). Profiling Fragile X Syndrome in males: strengths and weaknesses in cognitive abilities. Res. Dev. Disabil. 31, 426–439. 10.1016/j.ridd.2009.10.013 [DOI] [PubMed] [Google Scholar]
- Van der Molen M. J., Stam C. J., Van der Molen M. W. (2014). Resting-state EEG oscillatory dynamics in fragile X syndrome: abnormal functional connectivity and brain network organization. PLoS One 9:e88451. 10.1371/journal.pone.0088451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Molen M. J., Van der Molen M. W. (2013). Reduced α and exaggerated theta power during the resting-state EEG in fragile X syndrome. Biol. Psychol. 92, 216–219. 10.1016/j.biopsycho.2012.11.013 [DOI] [PubMed] [Google Scholar]
- Van der Weyden L., Adams D. J. (2013). Cancer of mice and men: old twists and new tails. J. Pathol. 230, 4–16. 10.1002/path.4184 [DOI] [PubMed] [Google Scholar]
- Vandamme T. F. (2014). Use of rodents as models of human diseases. J. Pharm. Bioallied Sci. 6, 2–9. 10.4103/0975-7406.124301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasile F., Dossi E., Rouach N. (2017). Human astrocytes: structure and functions in the healthy brain. Brain Struct. Funct. 222, 2017–2029. 10.1007/s00429-017-1383-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veeraragavan S., Bui N., Perkins J. R., Yuva-Paylor L. A., Paylor R. (2011). The modulation of fragile X behaviors by the muscarinic M4 antagonist, tropicamide. Behav. Neurosci. 125, 783–790. 10.1037/a0025202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verkerk A. J. M. H., Pieretti M., Sutcliffe J. S., Fu Y.-H., Kuhl D. P. A., Pizzuti A., et al. (1991). Identification of a gene (FMR-1) containing a CGG repeat coincident with a breakpoint cluster region exhibiting length variation in fragile X syndrome. Cell 65, 905–914. 10.1016/0092-8674(91)90397-H [DOI] [PubMed] [Google Scholar]
- Verrico C. D., Liu S., Asafu-Adjei J. K., Sampson A. R., Bradberry C. W., Lewis D. A. (2011). Acquisition and baseline performance of working memory tasks by adolescent rhesus monkeys. Brain Res. 10, 91–104. 10.1016/j.brainres.2010.12.081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinces M. D., Legendre M., Caldara M., Hagihara M., Verstrepen K. J. (2009). Unstable tandem repeats in promoters confer transcriptional evolvability. Science 324, 1213–1216. 10.1126/science.1170097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinueza Veloz M. F., Buijsen R. A., Willemsen R., Cupido A., Bosman L. W., Koekkoek S. K., et al. (2012). The effect of an mGluR5 inhibitor on procedural memory and avoidance discrimination impairments in Fmr1 KO mice. Genes Brain Behav. 11, 325–331. 10.1111/j.1601-183X.2012.00763.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vislay R. L., Martin B. S., Olmos-Serrano J. L., Kratovac S., Nelson D. L., Corbin J. G., et al. (2013). Homeostatic responses fail to correct defective amygdala inhibitory circuit maturation in fragile X syndrome. J. Neurosci. 33, 7548–7558. 10.1523/JNEUROSCI.2764-12.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voelkl B., Huber L. (2007). Imitation as faithful copying of a novel technique in marmoset monkeys. PLoS One 2:e611. 10.1371/journal.pone.0000611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volk L. J., Pfeiffer B. E., Gibson J. R., Huber K. M. (2007). Multiple Gq-coupled receptors converge on a common protein synthesis-dependent long-term depression that is affected in fragile X syndrome mental retardation. J. Neurosci. 27, 11624–11634. 10.1523/JNEUROSCI.2266-07.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volle C. B., Delaney S. (2013). AGG/CCT interruptions affect nucleosome formation and positioning of healthy-length CGG/CCG triplet repeats. BMC Biochem. 14:33. 10.1186/1471-2091-14-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Votinov M., Pripfl J., Windischberger C., Moser E., Sailer U., Lamm C. (2015). A functional polymorphism in the prodynorphin gene affects cognitive flexibility and brain activation during reversal learning. Front. Behav. Neurosci. 9:172. 10.3389/fnbeh.2015.00172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahlstrom-Helgren S., Klyachko V. A. (2015). GABAB receptor-mediated feed-forward circuit dysfunction in the mouse model of fragile X syndrome. J. Physiol. 593, 5009–5024. 10.1113/JP271190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallingford J., Scott A. L., Rodrigues K., Doering L. C. (2017). Altered developmental expression of the astrocyte-secreted factors hevin and sparc in the fragile X mouse model. Front. Mol. Neurosci. 10:268. 10.3389/fnmol.2017.00268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Ethridge L. E., Mosconi M. W., White S. P., Binder D. K., Pedapati E. V., et al. (2017). A resting EEG study of neocortical hyperexcitability and altered functional connectivity in fragile X syndrome. J. Neurodev. Disord. 9:11. 10.1186/s11689-017-9191-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J. Y., Hessl D., Iwahashi C., Cheung K., Schneider A., Hagerman R. J., et al. (2013). Influence of the fragile X mental retardation (FMR1) gene on the brain and working memory in men with normal FMR1 alleles. Neuroimage 65, 288–298. 10.1016/j.neuroimage.2012.09.075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J. M., Koldewyn K., Hashimoto R., Schneider A., Le L., Tassone F., et al. (2012). Male carriers of the FMR1 premutation show altered hippocampal-prefrontal function during memory encoding. Front. Hum. Neurosci. 6:297. 10.3389/fnhum.2012.00297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H., Ku L., Osterhout D. J., Li W., Ahmadian A., Liang Z., et al. (2004). Developmentally-programmed FMRP expression in oligodendrocytes: a potential role of FMRP in regulating translation in oligodendroglia progenitors. Hum. Mol. Genet. 13, 79–89. 10.1093/hmg/ddh009 [DOI] [PubMed] [Google Scholar]
- Wang X., Snape M., Klann E., Stone J. G., Singh A., Petersen R. B., et al. (2012). Activation of the extracellular signal-regulated kinase pathway contributes to the behavioral deficit of fragile X-syndrome. J. Neurochem. 121, 672–679. 10.1111/j.1471-4159.2012.07722.x [DOI] [PubMed] [Google Scholar]
- Waterston R. H., Lindblad-Toh K., Birney E., Rogers J., Abril J. F., Agarwal P., et al. (2002). Initial sequencing and comparative analysis of the mouse genome. Nature 420, 520–562. 10.1038/nature01262 [DOI] [PubMed] [Google Scholar]
- Watson C. F., Caldwell C. A. (2010). Neighbor effects in marmosets: social contagion of agonism and affiliation in captive Callithrix jacchus. Am. J. Primatol. 72, 549–558. 10.1002/ajp.20805 [DOI] [PubMed] [Google Scholar]
- Weiler I. J., Irwin S. A., Klintsova A. Y., Spencer C. M., Brazelton A. D., Miyashiro K., et al. (1997). Fragile X mental retardation protein is translated near synapses in response to neurotransmitter activation. Proc. Natl. Acad. Sci. U S A 94, 5395–5400. 10.1073/pnas.94.10.5395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisman-Shomer P., Cohen E., Fry M. (2000). Interruption of the fragile X syndrome expanded sequence d(CGG)(n) by interspersed d(AGG) trinucleotides diminishes the formation and stability of d(CGG)(n) tetrahelical structures. Nucleic Acids Res. 28, 1535–1541. 10.1093/nar/28.7.1535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss D., Hampshire V. (2015). Primate wellness exams. Lab Anim. (NY) 44, 342–344. 10.1038/laban.835 [DOI] [PubMed] [Google Scholar]
- Weiss K., Orr-Urtreger A., Kaplan Ber I., Naiman T., Shomrat R., Bardugu E., et al. (2014). Ethnic effect on FMR1 carrier rate and AGG repeat interruptions among Ashkenazi women. Genet. Med. 16, 940–944. 10.1038/gim.2014.64 [DOI] [PubMed] [Google Scholar]
- Weitzmann M. N., Woodford K. J., Usdin K. (1997). DNA secondary structures and the evolution of hypervariable tandem arrays. J. Biol. Chem. 272, 9517–9523. 10.1074/jbc.272.14.9517 [DOI] [PubMed] [Google Scholar]
- Wells P. G., Bhatia S., Drake D. M., Miller-Pinsler L. (2016). Fetal oxidative stress mechanisms of neurodevelopmental deficits and exacerbation by ethanol and methamphetamine. Birth Defects Res. C Embryo Today 108, 108–130. 10.1002/bdrc.21134 [DOI] [PubMed] [Google Scholar]
- Weng N., Weiler I., Sumis A., Berry-Kravis E., Greenough W. (2008). Early-phase ERK activation as a biomarker for metabolic status in fragile X syndrome. Am. J. Med. Genet. B Neuropsychiatr. Genet. 147B, 1253–1257. 10.1002/ajmg.b.30765 [DOI] [PubMed] [Google Scholar]
- Wenzel H. J., Hunsaker M. R., Greco C. M., Willemsen R., Berman R. F. (2010). Ubiquitin-positive intranuclear inclusions in neuronal and glial cells in a mouse model of the fragile X premutation. Brain Res. 8, 155–166. 10.1016/j.brainres.2009.12.077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westmark C. J. (2017). Commentary: depletion of the fragile X mental retardation protein in embryonic stem cells alters the kinetics of neurogenesis. Front. Mol. Neurosci. 10:29. 10.3389/fnmol.2017.00029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westmark C. J., Chuang S. C., Hays S. A., Filon M. J., Ray B. C., Westmark P. R., et al. (2016). APP causes hyperexcitability in fragile X mice. Front. Mol. Neurosci. 9:147. 10.3389/fnmol.2016.00147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westmark C. J., Westmark P. R., O’Riordan K. J., Ray B. C., Hervey C. M., Salamat M. S., et al. (2011). Reversal of fragile X phenotypes by manipulation of AβPP/Aβ levels in Fmr1KO mice. PLoS One 6:e26549. 10.1371/journal.pone.0026549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willemsen R., Bontekoe C. J., Severijnen L. A., Oostra B. A. (2002). Timing of the absence of FMR1 expression in full mutation chorionic villi. Hum. Genet. 110, 601–605. 10.1007/s00439-002-0723-5 [DOI] [PubMed] [Google Scholar]
- Willemsen R., Hoogeveen-Westerveld M., Reis S., Holstege J., Severijnen L. A., Nieuwenhuizen I. M., et al. (2003). The FMR1 CGG repeat mouse displays ubiquitin-positive intranuclear neuronal inclusions; implications for the cerebellar tremor/ataxia syndrome. Hum. Mol. Genet. 12, 949–959. 10.1093/hmg/ddg114 [DOI] [PubMed] [Google Scholar]
- Wilson B. M., Cox C. L. (2007). Absence of metabotropic glutamate receptor-mediated plasticity in the neocortex of fragile X mice. Proc. Natl. Acad. Sci. U S A 104, 2454–2459. 10.1073/pnas.0610875104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson B., Kikuchi Y., Sun L., Hunter D., Dick F., Smith K., et al. (2015a). Auditory sequence processing reveals evolutionarily conserved regions of frontal cortex in macaques and humans. Nat. Commun. 6:8901. 10.1038/ncomms9901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson B., Smith K., Petkov C. I. (2015b). Mixed-complexity artificial grammar learning in humans and macaque monkeys: evaluating learning strategies. Eur. J. Neurosci. 41, 568–578. 10.1111/ejn.12834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson B., Slater H., Kikuchi Y., Milne A. E., Marslen-Wilson W. D., Smith K., et al. (2013). Auditory artificial grammar learning in macaque and marmoset monkeys. J. Neurosci. 33, 18825–18835. 10.1523/jneurosci.2414-13.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittkopp P. J., Kalay G. (2011). Cis-regulatory elements: molecular mechanisms and evolutionary processes underlying divergence. Nat. Rev. Genet. 13, 59–69. 10.1038/nrg3095 [DOI] [PubMed] [Google Scholar]
- Wöhrle D., Hennig I., Vogel W., Steinbach P. (1993). Mitotic stability of fragile X mutations in differentiated cells indicates early post-conceptional trinucleotide repeat expansion. Nat. Genet. 4, 140–142. 10.1038/ng0693-140 [DOI] [PubMed] [Google Scholar]
- Wöhrle D., Salat U., Hameister H., Vogel W., Steinbach P. (2001). Demethylation, reactivation and destabilization of human fragile X full-mutation alleles in mouse embryocarcinoma cells. Am. J. Hum. Genet. 69, 504–515. 10.1086/322739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu C. L., Huang L. Y., Chang C. L. (2017). Linking arsenite- and cadmium-generated oxidative stress to microsatellite instability in vitro and in vivo. Free Radic. Biol. Med. 112, 12–23. 10.1016/j.freeradbiomed.2017.07.006 [DOI] [PubMed] [Google Scholar]
- Wu D., Zhai Q., Shi X. (2006). Alcohol-induced oxidative stress and cell responses. J. Gastroenterol. Hepatol. 21, S26–S29. 10.1111/j.1440-1746.2006.04589.x [DOI] [PubMed] [Google Scholar]
- Xu H., Rosales-Reynoso M. A., Barros-Núñez P., Peprah E. (2013). DNA repair/replication transcripts are down regulated in patients with fragile X syndrome. BMC Res. Notes 6:90. 10.1186/1756-0500-6-90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Z. H., Yang Q., Feng B., Liu S. B., Zhang N., Xing J. H., et al. (2012a). Group I mGluR antagonist rescues the deficit of D1-induced LTP in a mouse model of fragile X syndrome. Mol. Neurodegener. 7:24. 10.1186/1750-1326-7-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Z. H., Yang Q., Ma L., Liu S. B., Chen G. S., Wu Y. M., et al. (2012b). Deficits in LTP induction by 5-HT2A receptor antagonist in a mouse model for fragile X syndrome. PLoS One 7:e48741. 10.1371/journal.pone.0048741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto M. E., Araujo A., Arruda Mde F., Lima A. K., Siqueira Jde O., Hattori W. T. (2014). Male and female breeding strategies in a cooperative primate. Behav. Processes 109, 27–33. 10.1016/j.beproc.2014.06.009 [DOI] [PubMed] [Google Scholar]
- Yamazaki Y., Iriki A., Watanabe S. (2011). Modulation of physical understanding by common marmosets (Callithrix jacchus). Anim. Cogn. 14, 175–186. 10.1007/s10071-010-0351-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamazaki Y., Saiki M., Inada M., Iriki A., Watanabe S. (2014). Transposition and its generalization in common marmosets. J. Exp. Psychol. Anim. Learn. Cogn. 40, 317–326. 10.1037/xan0000027 [DOI] [PubMed] [Google Scholar]
- Yan Q. J., Asafo-Adjei P. K., Arnold H. M., Brown R. E., Bauchwitz R. P. (2004). A phenotypic and molecular characterization of the fmr1-tm1Cgr fragile X mouse. Genes Brain Behav. 3, 337–359. 10.1111/j.1601-183x.2004.00087.x [DOI] [PubMed] [Google Scholar]
- Yan Q. J., Rammal M., Tranfaglia M., Bauchwitz R. P. (2005). Suppression of two major Fragile X Syndrome mouse model phenotypes by the mGluR5 antagonist MPEP. Neuropharmacology 49, 1053–1066. 10.1016/j.neuropharm.2005.06.004 [DOI] [PubMed] [Google Scholar]
- Yang Q., Yang L., Zhang K., Guo Y. Y., Liu S. B., Wu Y. M., et al. (2015). Increased coupling of caveolin-1 and estrogen receptor α contributes to the fragile X syndrome. Ann. Neurol. 77, 618–636. 10.1002/ana.24358 [DOI] [PubMed] [Google Scholar]
- Yang S., Park J. S., Kirkwood A., Bao S. (2014). Failed stabilization for long-term potentiation in the auditory cortex of FMR1 knockout mice. PLoS One 9:e104691. 10.1371/journal.pone.0104691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yau S. Y., Bostrom C. A., Chiu J., Fontaine C. J., Sawchuk S., Meconi A., et al. (2016). Impaired bidirectional NMDA receptor dependent synaptic plasticity in the dentate gyrus of adult female Fmr1 heterozygous knockout mice. Neurobiol. Dis. 96, 261–270. 10.1016/j.nbd.2016.09.012 [DOI] [PubMed] [Google Scholar]
- Yrigollen C. M., Durbin-Johnson B., Gane L., Nelson D. L., Hagerman R., Hagerman P. J., et al. (2012). AGG interruptions within the maternal FMR1 gene reduce the risk of offspring with fragile X syndrome. Genet. Med. 14, 729–736. 10.1038/gim.2012.34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yrigollen C. M., Martorell L., Durbin-Johnson B., Naudo M., Genoves J., Murgia A., et al. (2014). AGG interruptions and maternal age affect FMR1 CGG repeat allele stability during transmission. J. Neurodev. Disord. 6:24. 10.1186/1866-1955-6-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yrigollen C. M., Mendoza-Morales G., Hagerman R., Tassone F. (2013). Transmission of an FMR1 premutation allele in a large family identified through newborn screening: the role of AGG interruptions. J. Hum. Genet. 58, 553–559. 10.1038/jhg.2013.50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yrigollen C. M., Pacini L., Nobile V., Lozano R., Hagerman R. J., Bagni C., et al. (2016). Clinical and molecular assessment in a female with fragile X syndrome and tuberous sclerosis. J. Genet. Disord. Genet. Rep. 5:139. 10.4172/2327-5790.1000139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yue F., Cheng Y., Breschi A., Vierstra J., Wu W., Ryba T., et al. (2014). A comparative encyclopedia of DNA elements in the mouse genome. Nature 515, 355–364. 10.1038/nature13992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu S., Mulley J., Loesch D., Turner G., Donnelly A., Gedeon A., et al. (1992). Fragile-X syndrome: unique genetics of the heritable unstable element. Am. J. Hum. Genet. 50, 968–980. [PMC free article] [PubMed] [Google Scholar]
- Yuskaitis C. J., Mines M. A., King M. K., Sweatt J. D., Miller C. A., Jope R. S. (2010). Lithium ameliorates altered glycogen synthase kinase-3 and behavior in a mouse model of fragile X syndrome. Biochem. Pharmacol. 79, 632–646. 10.1016/j.bcp.2009.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalfa F., Giorgi M., Primerano B., Moro A., Di Penta A., Reis S., et al. (2003). The fragile X syndrome protein FMRP associates with BC1 RNA and regulates the translation of specific mRNAs at synapses. Cell 112, 317–327. 10.1016/s0092-8674(03)00079-5 [DOI] [PubMed] [Google Scholar]
- Zang J. B., Nosyreva E. D., Spencer C. M., Volk L. J., Musunuru K., Zhong R., et al. (2009). A mouse model of the human fragile X syndrome I304N mutation. PLoS Genet. 5:e1000758. 10.1371/journal.pgen.1000758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeier Z., Kumar A., Bodhinathan K., Feller J. A., Foster T. C., Bloom D. C. (2009). Fragile X mental retardation protein replacement restores hippocampal synaptic function in a mouse model of fragile X syndrome. Gene Ther. 16, 1122–1129. 10.1038/gt.2009.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng J., Konopka G., Hunt B. G., Preuss T. M., Geschwind D., Yi S. V. (2012). Divergent whole-genome methylation maps of human and chimpanzee brains reveal epigenetic basis of human regulatory evolution. Am. J. Hum. Genet. 91, 455–465. 10.1016/j.ajhg.2012.07.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang N., Ashizawa T. (2017). RNA toxicity and foci formation in microsatellite expansion diseases. Curr. Opin. Genet. Dev. 44, 17–29. 10.1016/j.gde.2017.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Bonnan A., Bony G., Ferezou I., Pietropaolo S., Ginger M., et al. (2014). Dendritic channelopathies contribute to neocortical and sensory hyperexcitability in Fmr1−/y mice. Nat. Neurosci. 17, 1701–1709. 10.1038/nn.3864 [DOI] [PubMed] [Google Scholar]
- Zhang J., Hou L., Klann E., Nelson D. L. (2009). Altered hippocampal synaptic plasticity in the FMR1 gene family knockout mouse models. J. Neurophysiol. 101, 2572–2580. 10.1152/jn.90558.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y. W., Luo H. R., Ryder O. A., Zhang Y. P. (2004). Evolution of the tandem repeats in thymidylate synthase enhancer region (TSER) in primates. Gene 338, 47–54. 10.1016/j.gene.2004.05.018 [DOI] [PubMed] [Google Scholar]
- Zhang X. L., Pang W., Hu X. T., Li J. L., Yao Y. G., Zheng Y. T. (2014). Experimental primates and non-human primate (NHP) models of human diseases in China: current status and progress. Dongwuxue Yanjiu 35, 447–464. 10.13918/j.issn.2095-8137.2014.6.447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao W., Chuang S. C., Young S. R., Bianchi R., Wong R. K. (2015). Extracellular glutamate exposure facilitates group I mGluR-mediated epileptogenesis in the hippocampus. J. Neurosci. 35, 308–315. 10.1523/jneurosci.1944-14.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao X. N., Kumari D., Gupta S., Wu D., Evanitsky M., Yang W., et al. (2015). Mutsbeta generates both expansions and contractions in a mouse model of the Fragile X-associated disorders. Hum. Mol. Genet. 24, 7087–7096. 10.1093/hmg/ddv408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao M. G., Toyoda H., Ko S. W., Ding H. K., Wu L. J., Zhuo M. (2005). Deficits in trace fear memory and long-term potentiation in a mouse model for fragile X syndrome. J. Neurosci. 25, 7385–7392. 10.1523/jneurosci.1520-05.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao H., Tu Z., Xu H., Yan S., Yan H., Zheng Y., et al. (2017). Altered neurogenesis and disrupted expression of synaptic proteins in prefrontal cortex of SHANK3-deficient non-human primate. Cell Res. 27, 1293–1297. 10.1038/cr.2017.95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao X. N., Usdin K. (2014). Gender and cell-type-specific effects of the transcription-coupled repair protein, ERCC6/CSB, on repeat expansion in a mouse model of the fragile X-related disorders. Hum. Mutat. 35, 341–349. 10.1002/humu.22495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong J., Chuang S. C., Bianchi R., Zhao W., Lee H., Fenton A. A., et al. (2009). BC1 regulation of metabotropic glutamate receptor-mediated neuronal excitability. J. Neurosci. 29, 9977–9986. 10.1523/jneurosci.3893-08.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Q. (2014). Balancing the welfare: the use of non-human primates in research. Trends Genet. 30, 476–478. 10.1016/j.tig.2014.09.005 [DOI] [PubMed] [Google Scholar]
- Zhou Y., Kumari D., Sciascia N., Usdin K. (2016). CGG-repeat dynamics and FMR1 gene silencing in fragile X syndrome stem cells and stem cell-derived neurons. Mol. Autism 7:42. 10.1186/s13229-016-0105-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zumwalt M., Ludwig A., Hagerman P. J., Dieckmann T. (2007). Secondary structure and dynamics of the r(CGG) repeat in the mRNA of the fragile X mental retardation 1 (FMR1) gene. RNA Biol. 4, 93–100. 10.4161/rna.4.2.5039 [DOI] [PubMed] [Google Scholar]
- Zuo E., Cai Y. J., Li K., Wei Y., Wang B. A., Sun Y., et al. (2017). One-step generation of complete gene knockout mice and monkeys by CRISPR/Cas9-mediated gene editing with multiple sgRNAs. Cell Res. 27, 933–945. 10.1038/cr.2017.81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuo B., Du X., Zhao J., Yang H., Wang C., Wu Y., et al. (2012). Analysis of microsatellite polymorphism in inbred knockout mice. PLoS One 7:e34555. 10.1371/journal.pone.0034555 [DOI] [PMC free article] [PubMed] [Google Scholar]