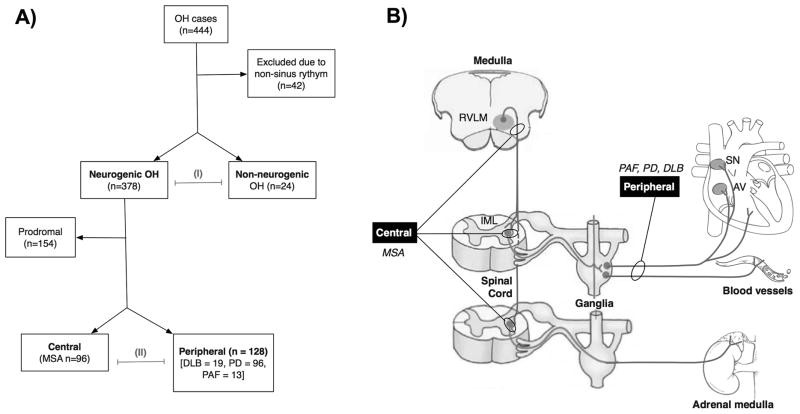
Figure 1. Patient cohort and study rationale.
A. Flow chart showing the classification of the participants. Four hundred and forty-four patients were screened. Only those in normal sinus rhythm in whom the heart rate responses could be clearly attributed to extrinsic autonomic innervation were included in the subsequent analysis. Patients were classified as having neurogenic or non-neurogenic orthostatic hypotension (OH) and both groups were compared (I). As shown in panel B, based on their neurological examination, cases of neurogenic OH were diagnosed with either probable or possible MSA, and thus classified as having central autonomic failure (due to neuronal loss in the brainstem vasomotor nuclei and intermediolateral columns of the spinal cord,49 but intact peripheral post-ganglionic sympathetic neurons innervating the heart);50 or Parkinson disease, dementia with Lewy bodies, and pure autonomic failure.22, 49, 51 The latter group was classified as having peripheral lesions, as a result of predominant involvement of peripheral postganglionic sympathetic neurons.23 Parasympathetic activity (not shown) was equally affected in patients with central and peripheral autonomic failure. The remaining patients that had autonomic failure with CNS signs, but did not meet diagnostic criteria for a defined CNS synucleinopathy were classified as having prodromal disease (see text for details). The impact of central vs. peripheral autonomic failure was compared (A II).