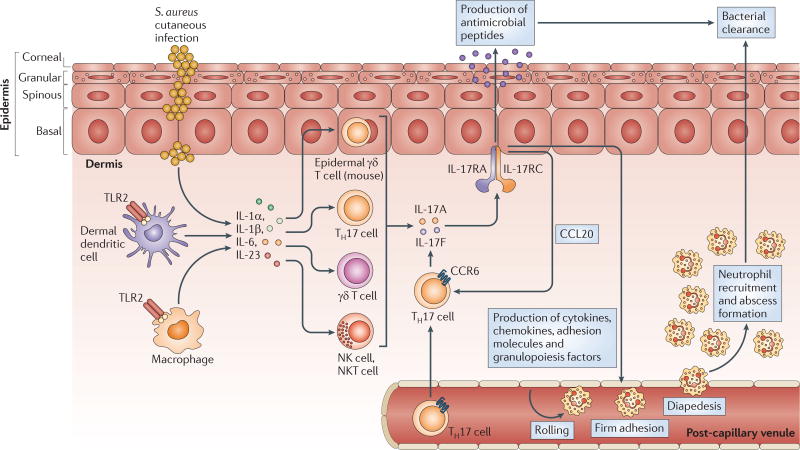
Figure 5. The IL-17-mediated cutaneous immune response against S. aureus.
Interleukin-17A (IL-17A) and IL-17F are produced by various cells in the skin, including γδ T cells in the epidermis (in mice) and T helper 17 (TH17) cells, γδ T cells, natural killer (NK) cells and NKT cells in the dermis. The production of IL-17A and IL-17F depends on the activation of Toll-like receptor 2 (TLR2) and the production of IL-1α, IL-1β, IL-6 and IL-23, which can be produced by other resident and recruited cells in the skin, such as macrophages and dendritic cells. IL-17A and IL-17F activate IL-17 receptors (IL-17RA–IL-17RC) on epidermal keratinocytes, resulting in the production of antimicrobial peptides (such as β-defensins 2 and 3, and cathelicidins) that have bacteriostatic and bactericidal activity against Staphylococcus aureus, as well as in the production of pro-inflammatory cytokines, chemokines and adhesion molecules that promote the recruitment of neutrophils from the circulation to the site of S. aureus infection in the skin. IL-17-mediated signalling also leads to the production of GM-CSF (granulocyte–macrophage colony-stimulating factor) and G-CSF, which promote neutrophil granulopoiesis in the bone marrow and perhaps locally in the skin. Neutrophils form an abscess to help control and limit the spread of the infection in the skin, and this is ultimately required for bacterial clearance. IL-17-mediated signalling also leads to the production of CC-chemokine ligand 20 (CCL20), which triggers a positive feedback loop by promoting additional recruitment from the circulation of TH17 cells that preferentially express CC-chemokine receptor 6 (CCR6).